Hypokinesia
Hypokinesia is an extraordinary condition of the human body, in which there is a lack of motor activity, which is manifested by a decrease in pace and limitation of movements.
A decrease in motor activity can occur against the background of mental and neurological disorders, such as Parkinson's disease and other extrapyramidal syndromes, various stupors - catatonic, depressive and apathetic. In addition, hypokinesia may be the result of a sedentary lifestyle or the nature of work.
Monotonous work with a fixed posture, which reduces the work of muscles or uses only a certain group of them, is often accompanied not only by physical inactivity, but also by hypokinesia. The risk group includes programmers, accountants, operators, cashiers and other professionals whose activities involve monotonous work.
The degree of hypokinesia is determined based on a person’s energy expenditure on muscle activity in a certain period of time. The degree of development of hypokinesia varies from slight to complete cessation of motor activity.
Life on the move
Between 25 and 40 percent of our body weight is muscle. And the ancient Greek scientist Hippocrates called physical activity “food for life.” The key to the normal functioning of all organs and systems of our body is the active work of all muscles. Man as a biological system is created for active activity.
But our age of rapid technology and information space increasingly takes up our time and leaves no opportunity for the development of muscle activity. The concept of “hypodynamia” (from the Greek words hypo - “below”, “under” and dynamikos - “strong”) is known to everyone today. It means a decrease in physical activity. Along with it, a term is often used that characterizes a general decrease in the tempo and range of movements. This is hypokinesia (from the Greek words hypo - “from below” and kinesis - “movement”). And if the first concept refers to a general decrease in activity, then hypokinesia is characterized by a decrease in the amplitude and strength of movements.
Thus, hypokinesia, like physical inactivity, has a complex effect on our body, leading to decreased performance, fatigue, nervousness, headaches and insomnia.
The effect of hypokinesia on the human body
A sedentary lifestyle or the consequences of diseases, as a result of which reduced activity develops, have a negative impact on the human body, on the optimal functionality of all its organs and systems. The influence of hypokinesia on the human body can be traced in a decrease in resistance and endurance to irritating environmental factors and physical activity.
As a result of the effect of hypokinesia on the human body, cardiovascular activity is disrupted - the heart rate decreases, lung ventilation decreases, and stagnation occurs in small veins and capillaries.
As a consequence, swelling occurs, intestinal absorption is impaired, and congestion occurs in the liver.
With hypokinesia, due to a decrease in the volume of joint fluid, the functioning of the joints is disrupted and their mobility is lost.
Muscle atrophy is observed as a result of their lack of demand by the body and a decrease in their contractile abilities. In addition, there is a disruption of blood supply and replacement of muscle tissue with fat and loss of protein.
With reduced motor activity, the tendon-ligament apparatus is weakened, flat feet develop and posture changes.
Hypokinesia leads to loss of intercentral connections in the central nervous system, disruption of the mental and emotional spheres.
In addition, hypotension develops, reducing a person’s mental and physical activity.
Maximum pulmonary ventilation decreases, the volume and depth of breathing is impaired.
Hypokinesia causes atrophy of the heart muscle, worsening the nutrition of the heart and disrupting blood flow from the lower extremities to the myocardium. The volume of the heart decreases and the period of blood circulation increases.
According to statistics, almost half of the world's population suffers from hypokinesia, and in the northern regions and in economically more developed countries this figure is higher.
What is the sequence of deformities in fetal akinesia/hypokinesia syndrome?
The deformity sequence of fetal akinesia includes the type of akinesia that causes a combination of pathologies in the womb as the baby develops. Examples of such symptoms:
- Various contractures;
- Facial abnormalities;
- Intrauterine growth restriction;
- Hypoplasia (underdevelopment) of the lungs.
Approximately 30% of children with fetal akinesia deformity sequence are stillborn. Others cannot live long due to problems associated with pulmonary hypoplasia.
Types of hypokinesia
The types of hypokinesia are determined from the speed of voluntary or automatic movements, their amplitude, volume and etiology.
Physiological hypokinesia occurs as a result of hereditary preconditions, abnormal development of the body and motor “debility.”
Common everyday types of hypokinesia include conditions caused by a decrease in motor initiative, a sedentary lifestyle, a comfortable lifestyle and a reluctance to engage in physical activity.
Occupational hypokinesia occurs as a result of professional activity caused by production circumstances.
There is clinical hypokinesia caused by the need for prolonged immobilization. It develops when the patient is kept in bed as a result of any illness or injury.
Currently, many students suffer from a form of school physical inactivity and hypokinesia. This is due to improper distribution of school workloads, rest schedules, and lack of time for physical education and sports.
Climatogeographic hypokinesia also often occurs, when a person’s physical activity decreases due to weather and climatic conditions. Quite often it occurs among residents of the Far North.
Based on the form of motor activity disorder, bradykinesia and akinesia are distinguished.
Bradykinesia is determined by the predominance of slow movements. With akinesia, the amplitude and range of movements are limited.
Hypokinesia is. Description, consequences, prevention, types and treatment
Scientific and technological progress has brought many useful things into our lives and has largely freed us from hard physical labor. But he also awarded the person with many serious problems. These are hypokinesia, physical inactivity, chronic fatigue syndrome, stress. According to experts, insufficient physical activity today has become the scourge of civilization and a factor contributing to general degradation. The statistics are inexorable: physical inactivity and hypokinesia take leading positions in the ranking of causes that cause obesity, coronary heart disease, myocardial infarction, and atherosclerosis.
Treatment of hypokinesia
Treatment is based on the severity of hypokinesia.
If the disease does not have pronounced consequences and the degree of decrease in activity is not high, then it is enough just to change living conditions and vigorously engage in dynamic activities - sports, walking, hiking and other active activities.
If hypokinesia is expressed as a consequence of any disease and the decrease in motor activity is more significant, then, first of all, the treatment of hypokinesia should include measures to exclude the cause of its occurrence.
Most often, treatment of hypokinesia is carried out in a combination of drug therapy and physical activity, using physical therapy.
Neurotransmitter level drugs are prescribed that regulate muscle tone and increase neuromuscular conduction.
For preventive purposes, in order to avoid such serious consequences as myocardial infarction, stroke, diabetes mellitus and diseases of the joints and bones, it is necessary to drink properly, avoid overeating and fatty foods, and lead an active lifestyle. And if working or living conditions limit your activity, you need to reconsider your attitude towards work and rest, change them to ones that are more active and necessary for your health.
Analysis of local contractility of the left ventricle
State Healthcare Institution "Lipetsk Regional Clinical Hospital"
Analysis of local contractility of the left ventricle
Informational and methodological letter
functional and ultrasound diagnostic doctors, cardiologists, therapists
– Head of the Department of Functional Diagnostics, State Healthcare Institution “Lipetsk Regional Clinical Hospital”, Ph.D.;
– Doctor of Ultrasound Diagnostics, Department of Functional Diagnostics, Lipetsk Regional Clinical Hospital;
– Ultrasound diagnostics doctor at the functional diagnostics department of the Lipetsk Regional Clinical Hospital.
– Chief Physician of the Lipetsk Regional Clinical Hospital, Ph.D., Honored Doctor of the Russian Federation
Approved for publication by the coordinating council for the implementation of the State Health Institution "LOKB"
Purpose
This information and methodological letter is to standardize and unify echocardiographic reports, bringing them to a single standard, which should lead to improved mutual understanding both between specialists working in echocardiography and specialists who referred the patient for research.
Echocardiography (EchoCG) is an ultrasound examination of the heart.
The examination is carried out with the patient lying on his left side with the upper half of the body elevated. Parasternal and apical approaches are mandatory; suprasternal and subxiphoidal approaches are optional.
• The most common indication for echocardiography is coronary artery disease. It is used both for diagnosing coronary heart disease and for determining myocardial contractility and valve function in coronary artery disease, complications of myocardial infarction, and prognosis.
• Echocardiography from parasternal, apical and sometimes subcostal approaches can visualize all segments of the left ventricle. For the analysis of local contractility, a 17-segment model of the left ventricle is recommended.
Etiology of local contractility disorders
• Myocardial infarction, post-infarction cardiosclerosis.
• Transient myocardial ischemia (stunned myocardium - contractility improves after taking nitroglycerin or independently).
• Constant (chronic) myocardial ischemia (dormant myocardium - viable, but not contracting).
• Myocardial damage of non-ischemic origin.
Types of local contractility disorders
• Hypokinesia—decreased range of motion and thickening of the myocardium in the area under study.
• Akinesia - lack of movement and thickening of the myocardium of the area under study.
• Dyskinesia - movement of the area under study in the direction opposite to normal.
• Hyperkinesia - an increase in the amplitude of movement and thickening of the myocardium of the area under study (usually the intact myocardium).
Syndrome of local disturbance of myocardial contractility
During ultrasound examination of the heart, verification of zones of local hypo- or akinesis of the left ventricular myocardium always sets the attending physician the task of establishing the cause of this echocardiographic phenomenon. In most cases, this does not present any particular difficulties, since, for example, if the patient has suffered an acute myocardial infarction, the patient will have an appropriate medical history, supported by a discharge summary and electrocardiograms. In addition, sometimes provoking local hypokinesis is the target of diagnosis (stress echocardiography). However, there are situations when the detection of zones of local disturbance of myocardial contractility is an accidental finding during an echocardiography study. Moreover, such a patient can be both subjectively healthy and, for example, have clinical signs of heart failure.
When abstracting from a specific clinical situation, there are primarily three diseases that can be complicated by local impairment of myocardial contractility:
— myocardial infarction
within the framework of IBS,
Myocardial infarction
against the background of stenotic atherosclerosis of the coronary arteries, it is certainly the leading cause of local hypo- or akinesis syndrome. It accounts for at least 90% of all cases.
Myocarditis
, as a cause of decreased local contractility, should always be suspected in myocardial infarction “on pure coronary arteries.” Interestingly, in different patients the clinical debut of such myocarditis can be polar. In one case, it does not differ from acute myocardial infarction: typical acute anginal pain with characteristic ECG dynamics. In another case, the disease manifests itself with symptoms of heart failure - ultrasound of the heart reveals local hypoakinesis or diffuse hypokinesis. They have one thing in common: with coronary angiography, the arteries are intact.
It should be noted that there are rare cases when thrombotic occlusion of the distal segment of the coronary artery is difficult to visualize due to the small diameter of the artery. We have seen this more than once in the hospital. In this case, repeated examination of coronary angiograms, including collegial examination, helps to establish the location of thrombosis. So, theoretically, there is a small chance of error. However, I repeat, myocardial infarction “on clean arteries” in the vast majority of cases indicates one thing: there is no atherosclerosis of the coronary arteries.
Heart bruise
as a cause of local contractility impairment is very rare. As a rule, in case of cardiac contusion, ECG changes are limited to “fine-focal changes within the T wave,” and according to echocardiographic criteria, the kinesis of the walls of the left ventricle remains correct. However, hypothetically anything is possible. Obviously, a relevant history (chest trauma) must be mandatory. Almost always, only the anterior wall of the left ventricle is injured.
I will outline a few more clinical cases that can manifest themselves as local hypokinesis in “clean arteries”:
- arrhythmogenic dysplasia of the right ventricle with transition to the left ventricle,
- myocardial infarction due to abnormal development of the coronary arteries,
The diseases listed above are united by one important clinical and morphological phenomenon: local myocardial dysfunction is caused by gross degenerative processes in cardiomyocytes: from irreversible (necrosis during myocardial infarction), to potentially reversible (with alcoholic cardiomyopathy) or transient (with Takotsubo cardiomyopathy). In other words, local impairment of myocardial contractility is caused by objective changes in histochemical processes in it.
Another group of causes of local hypoakinesis syndrome of the left ventricular myocardium includes clinical situations when impaired contractility is caused not by cardiomyocyte dysfunction, but by other reasons. Let's talk about them.
1. Severe hypertrophy of the interventricular septum
within the framework of asymmetric hypertrophic cardiomyopathy. With subaortic stenosis, the thicker the IVS, the higher the likelihood of impaired contractility. This phenomenon is not due to the death of cardiomyocytes, but to a gross disruption of the normal architecture of the myocardial syncytium and an increased specific gravity of connective tissue. As a result, the contractile function of the IVS is significantly affected. The ECG may even show infarct-like changes like a pathological Q wave, reflecting the “loss” of the IVS from the electrical systole of the left ventricle. To make it clearer, watch this video.
2. Left bundle branch block
is a common cause of local hypoakinesis of the left ventricular myocardium. It is mainly the contractile function of the IVS that suffers. The rule is this: the wider the QRS complex during LBP blockade, the higher the likelihood of detecting a violation of IVS contractility during ECHO. Impaired contractility of the IVS during LBP blockade can vary from hypoakinesis to dyskinesis. A consequence of the disruption of the propagation of the electrical impulse during LBP blockade is premature contraction of the IVS (at the end of the ejection period - that is, when the aortic valve is closed), when the rest of the left ventricular myocardium has not yet contracted. In addition, the asynchrony of contraction of the IVS segments and the rest of the left ventricle leads to IVS stretching, which does not contribute to full systole. The bulk of the left ventricle contracts at a time when the IVS is already relaxed.
Echocardiography for dummies, part 3. Local contractility disorders
Continuation of the article.
Echocardiography – what is it? Explanation for non-cardiologists. I am continuing my series of publications that I hope will help non-cardiology physicians gain a general understanding of echocardiography. We have already discussed what sizes of heart chambers are considered pathological, and how left ventricular ejection fraction is measured. Now I would like to talk about how the heart changes after myocardial infarction.
How can you determine if a patient has had a heart attack using echocardiography? We all remember that myocardial cells contract during systole and lengthen during diastole. But if some of these cells receive insufficient nutrition or die altogether, then the area of the myocardium loses the ability to contract as well as its neighbors. If he still moves at the very least, then this is called “hypokinesia”. If he is motionless at all, then “akinesia”. If a section of the myocardium has turned into an ugly fibrous scar, which not only does not contract when it should, but also moves out of phase with the rest of the sections, then this is “dyskinesia.”
A heart attack cannot happen wherever he pleases. To understand the principle by which local contractility disorders develop, an anatomical certificate is needed. The heart is supplied with blood by two arteries – the left coronary artery (LCA) and the right coronary artery (RCA). Both have many branches, the most important of which are the large branches of the LMCA: the anterior interventricular branch (LAD; also called the anterior descending artery, LAD) and the circumflex branch (OB). Options are possible, but in the classic scenario, the LAD supplies blood to the apex of the left ventricle and the interventricular septum, the OB - its lateral and posterior sections, and the RCA - the posterior and inferior sections, as well as the right ventricle. This is a very approximate diagram; I have attached a more detailed diagram to the publication in the form of a picture. It is useful to have it in mind if your patient had a coronary angiography: for example, if the conclusion says that the patient has an occlusion of the LAD, and all other vessels are clean, then don’t go to a fortune teller, he had a heart attack in the apex.
In principle, a regular ECG can be used for the same purposes. That’s why diagnosticians require that the patient have an ECG on hand - so that it is clear where to look for the scar. This approach, of course, helps, but not always: if the patient’s endocardium is poorly visible, but there are changes on the ECG, then you involuntarily want to write to him, just in case, something that you really can’t see, just to be on the safe side. All these favorite phrases by us, diagnosticians, like “the impression is created of...”, “under conditions of non-optimal visualization it is determined...”, etc., in fact, show that we are not at all confident in our words, so we do not want to answer for them . It’s easier for me in this regard - I work in cardiac surgery, the patient goes for surgery in any case, so I can, in theory, write any nonsense Smiley “smile”. But if, let’s say, a patient who is not complaining about anything came from the street to get an echocardiogram for the sake of laughter, then his future fate depends on the conclusion of the diagnostician. Therefore, I want to give some practical tips on interpreting the conclusion:
— The most important advice regarding not only heart attacks, but also all cardiology: collect anamnesis! If a patient’s report states that everything is bad, but he himself is in full health and runs 10 kilometers every day, then there is a high probability of a diagnostic error. And vice versa, if the echocardiography results are ideal, and the patient cannot scratch his nose without shortness of breath, then you need to think hard about whether everything is really so good.
— When analyzing echocardiography, the left ventricle is usually divided into segments. Some people select 16 segments, others 17. Now they recommend using a 17-segment model, but that’s not the point. So, we can talk about a scar if there is a violation of contractility in at least two adjacent segments, with the exception of small infarcts in the area of the apex and basal sections of the interventricular septum. If you see in the conclusion, say, “hypokinesia of the middle lower and apical septal segments,” i.e., two completely unrelated sections of the myocardium (we remember that the lower sections are supplied by the RCA, and the apex by the LAD!), then there is a high probability that there is an error in the conclusion. Of course, anything can happen. For example, this is possible in cases of stab wounds to the heart or certain systemic diseases. But, as the very good book “The House of God” says, if we see hoof prints on the ground, then we should think about a horse, not a zebra... unless we are in Africa, of course.
— Strongly recommend that your patients take old reports with them, and require that diagnosticians evaluate the dynamics. We often see how scars miraculously migrate and dissolve in the same person who has had an echocardiogram in different places.
— Another big problem is that everyone tries to call the walls of the heart in their own way. Some have a lower wall, some have a diaphragmatic wall; some even believe that “basal segments” is the name of the wall. Diagnosticians working in the same institution often call the walls differently! It would be nice if everyone spoke the same language.
— Disturbances of local contractility are nothing without tests with physical activity. If the patient seems to have decent systolic function and has no complaints, but there are contractility disorders, then you can’t just shake your head, say “you’ve had a heart attack!”, prescribe him bisoprolol and calm down at that. It is necessary to invite a cardiologist to determine whether the patient has indications for coronary angiography. This is determined using stress tests - treadmill, bicycle ergometer, stress echocardiography... there are many options! The most important thing is not to miss the moment when the patient can still be helped.
Myocardial contractility: concept, norm and disorder, treatment of decreased
All materials are published under the authorship or editorship of medical professionals (about the authors), but are not a prescription for treatment. Contact the specialists!
© Use of site materials only in agreement with the administration.
Author: Sazykina Oksana Yurievna, cardiologist
The heart muscle is the most resilient in the human body. The high performance of the myocardium is due to a number of properties of myocardial cells – cardiomyocytes. These properties include automaticity (the ability to independently generate electricity), conductivity (the ability to transmit electrical impulses to nearby muscle fibers in the heart) and contractility - the ability to contract synchronously in response to electrical stimulation.
In a more global concept, contractility refers to the ability of the heart muscle as a whole to contract in order to push blood into the large main arteries - the aorta and the pulmonary trunk. They usually talk about the contractility of the left ventricular myocardium, since it is the one that does the most work of pushing out blood, and this work is assessed by the ejection fraction and stroke volume, that is, by the amount of blood that is ejected into the aorta with each cardiac cycle.
Treatment
Hypertrophy of the heart muscle can be treated with medication or surgery. The main goal of therapeutic intervention is to bring the volume of the myocardium to a normal state or prevent its further growth. The treatment process will depend on the cause of the pathology.
Medicines
- Since hypertrophy is most often caused by hypertension, it is necessary to take antihypertensive drugs.
- Another group of drugs are medications necessary to maintain the functioning of the heart muscle and improve myocardial nutrition.
- Symptomatic remedies. They are needed to eliminate unpleasant symptoms: shortness of breath, arrhythmia, pain, swelling.
Surgical intervention
- Excision of part of the myocardium located between the ventricles (the procedure is called the Morrow operation).
- Correction or replacement of valves (mitral, aortic).
- Removal of adhesions blocking the entrance to the aorta (commissurotomy).
- Artificial expansion of the arterial lumen by introducing an implant (stent).
- Implantation of a pacemaker.
In addition to the listed treatment methods, lifestyle correction, proper nutrition, physical therapy, and weight loss are necessary.
Left ventricular myocardial hypertrophy does not pose a particular threat if the changes are moderate and detected in a timely manner. In some cases, you can even do without treatment. It is enough to follow the doctor’s recommendations regarding nutrition, physical activity, and maintaining a stable emotional background.
However, this diagnosis cannot be ignored. Severe progression of the pathological process without taking adequate measures can lead to serious consequences (left ventricular failure), including death (myocardial infarction).
Bioelectrical basis of myocardial contractility
heart contraction cycle
The contractility of the entire myocardium depends on the biochemical characteristics in each individual muscle fiber. The cardiomyocyte, like any cell, has a membrane and internal structures, mainly consisting of contractile proteins. These proteins (actin and myosin) can contract, but only if calcium ions enter the cell through the membrane. This is followed by a cascade of biochemical reactions, and as a result, the protein molecules in the cell contract like springs, causing contraction of the cardiomyocyte itself. In turn, the entry of calcium into the cell through special ion channels is possible only in the case of repolarization and depolarization processes, that is, sodium and potassium ion currents through the membrane.
With each incoming electrical impulse, the cardiomyocyte membrane is excited, and the flow of ions into and out of the cell is activated. Such bioelectric processes in the myocardium do not occur simultaneously in all parts of the heart, but one by one - first the atria are excited and contracted, then the ventricles themselves and the interventricular septum. The result of all processes is a synchronous, regular contraction of the heart with the ejection of a certain volume of blood into the aorta and further throughout the body. Thus, the myocardium performs its contractile function.
Video: more about the biochemistry of myocardial contractility
Why do you need to know about myocardial contractility?
Cardiac contractility is the most important ability that indicates the health of the heart itself and the entire body as a whole. In the case when a person’s myocardial contractility is within normal limits, he has nothing to worry about, since in the complete absence of cardiac complaints, we can confidently say that at the moment everything is in order with his cardiovascular system.
If the doctor suspects and confirms through examination that the patient has impaired or reduced myocardial contractility, he needs to be further examined as soon as possible and begin treatment if he has a serious myocardial disease. What diseases can cause impaired myocardial contractility will be discussed below.
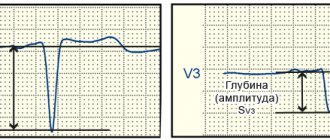
Myocardial contractility according to ECG
The contractility of the heart muscle can be assessed already by performing an electrocardiogram (ECG), since this research method allows you to record the electrical activity of the myocardium. With normal contractility, the heart rhythm on the cardiogram is sinus and regular, and the complexes reflecting contractions of the atria and ventricles (PQRST) have the correct appearance, without changes in individual teeth. The nature of the PQRST complexes in different leads (standard or chest) is also assessed, and with changes in different leads, one can judge the impairment of contractility of the corresponding sections of the left ventricle (lower wall, high-lateral sections, anterior, septal, apical-lateral walls of the LV). Due to its high information content and ease of use, an ECG is a routine research method that allows timely identification of certain disorders in the contractility of the heart muscle.
Myocardial contractility by echocardiography
EchoCG (echocardioscopy), or ultrasound of the heart, is the gold standard in the study of the heart and its contractility due to good visualization of cardiac structures. Myocardial contractility using cardiac ultrasound is assessed based on the quality of reflection of ultrasonic waves, which are converted into a graphic image using special equipment.
photo: assessment of myocardial contractility on EchoCG with load
Cardiac ultrasound mainly assesses the contractility of the left ventricular myocardium. In order to find out whether the myocardium is contracting completely or partially, it is necessary to calculate a number of indicators. Thus, the total wall mobility index is calculated (based on the analysis of each segment of the LV wall) - WMSI. LV wall mobility is determined based on the percentage by which the LV wall thickness increases during cardiac contraction (during LV systole). The greater the thickness of the LV wall during systole, the better the contractility of this segment. Each segment, based on the thickness of the walls of the LV myocardium, is assigned a certain number of points - for normokinesis 1 point, for hypokinesia - 2 points, for severe hypokinesia (up to akinesia) - 3 points, for dyskinesia - 4 points, for aneurysm - 5 points. The total index is calculated as the ratio of the sum of points for the segments under study to the number of visualized segments.
A total index equal to 1 is considered normal. That is, if the doctor “looked” at three segments using ultrasound, and each of them had normal contractility (each segment had 1 point), then the total index = 1 (normal, and myocardial contractility is satisfactory ). If, of the three visualized segments, at least one has impaired contractility and is rated 2-3 points, then the total index = 5/3 = 1.66 (myocardial contractility is reduced). Thus, the total index should be no more than 1.
sections of the heart muscle on echocardiography
In cases where myocardial contractility according to cardiac ultrasound is within normal limits, but the patient has a number of cardiac complaints (pain, shortness of breath, swelling, etc.), the patient is advised to undergo stress ECHO-CG, that is, ultrasound of the heart performed after physical exercise. loads (walking on a treadmill - treadmill, bicycle ergometry, 6-minute walk test). In the case of myocardial pathology, contractility after exercise will be impaired.
About other possible anomalies
The myocardium of the left ventricle can undergo diffuse and focal changes of different nature:
- Inflammatory process. Develops under the influence of infectious diseases.
- Dysmetabolic metamorphoses in cardiomyocytes. Disturbed metabolic processes lead to dystrophic modifications of the muscular layer of the heart.
- Tissue necrosis. It can be caused by a heart attack, advanced stage of myocardial dystrophy or myocarditis, ischemia and other cardiac pathologies.
- Extracardiac factors (poor nutrition, hormone imbalance, disease). They cause nonspecific changes in the myocardium of the left ventricle, which in most cases are not dangerous and are easily reversible. Such anomalies are associated with impaired repolarization (restoration of the initial charge of myocardiocytes during cardiac diastole).
Each of these conditions requires its own approach to treatment. Moderate metabolic disorders are considered the most correctable. To restore the altered cell structure, drug therapy is not always necessary. The most dangerous are sclerotic processes, as a result of which areas of the myocardium are replaced by scar tissue that is not capable of contraction.
Minor changes in the myocardium on the part of the left ventricle may not manifest themselves for a long time. The only way to detect them in this case is to do an ECG or ultrasound of the heart. Often such deviations can be a variant of the norm. For example, due to age-related changes in a child or a mature person, as well as during pregnancy.
Hypertrophic and other disorders of the myocardial structure should be a reason for close attention. This also applies to nonspecific deviations. Especially if they concern the left ventricle. This chamber is very significant and wears out faster than others, as it is subject to maximum load during cardiac activity. Even if the diagnosis made on the basis of a cardiogram does not affect the person’s well-being, you should not lose sight of it. In this case, the condition of the heart must be constantly monitored, because there is always a risk of minor changes turning into a more dangerous form. In such a situation, the prognosis of the disease can no longer be called favorable.
Normal cardiac contractility and abnormal myocardial contractility
Whether the patient has preserved contractility of the heart muscle or not can be reliably judged only after an ultrasound of the heart. Thus, based on the calculation of the total wall mobility index, as well as determining the thickness of the LV wall during systole, it is possible to identify a normal type of contractility or deviations from the norm. Thickening of the studied myocardial segments of more than 40% is considered normal. An increase in myocardial thickness by 10-30% indicates hypokinesia, and a thickening of less than 10% of the original thickness indicates severe hypokinesia.
Based on this, the following concepts can be distinguished:
- Normal type of contractility - all segments of the LV contract in full force, regularly and synchronously, myocardial contractility is preserved,
- Hypokinesia – decreased local contractility of the LV,
- Akinesia is the complete absence of contraction of a given segment of the LV,
- Dyskinesia – myocardial contraction in the segment under study is incorrect,
- An aneurysm is a “protrusion” of the left ventricular wall, consisting of scar tissue, completely lacking the ability to contract.
In addition to this classification, disorders of global or local contractility are distinguished. In the first case, the myocardium of all parts of the heart is not able to contract with such force to achieve a full cardiac output. In case of disturbance of local myocardial contractility, the activity of those segments that are directly susceptible to pathological processes and in which signs of dys-, hypo- or akinesia are visualized decreases.
Signs and consequences of infarction of the anterior wall of the left ventricle
To begin with, I will try to briefly outline the essence of the problem.
Acute myocardial infarction is one of the variants of coronary heart disease (CHD). The basis of the pathology remains a critical discrepancy between the needs of the heart muscle for oxygen and nutrients.
Simply put, certain areas of the myocardium are simply not supplied with blood, which leads to the death of first isolated cells (cardiomyocytes), and then entire areas of muscle tissue.
My patients often ask me what can happen to cause the vessel that supplies the heart with blood to close. In 70-80% of cases, the basis of the problem is atherosclerosis. The disease is accompanied by the deposition of fat on the surface of the vascular wall and inflammation of the cells of its inner layer.
Over time, these elements form a tubercle, after which the lumen of the artery narrows. The result may be plaque rupture with the formation of a blood clot and complete blockage of the vessel. Acute myocardial infarction of the anterior wall of the left ventricle occurs in my practice more often than other forms.
This is due to the anatomical features of the blood supply to the heart.
According to modern views of cardiologists on the causes of myocardial infarction, it is worth highlighting the following key factors contributing to the progression of the pathology:
- Poor nutrition. I mean excessive consumption of foods rich in fast carbohydrates and fats (fast food, various sweets, energy drinks, alcohol).
- Obesity. Excess body weight indicates an active process of fat deposition in the wall of blood vessels. You can determine your body mass index by clicking on the link.
- Smoking. Nicotine promotes additional spasm of the coronary arteries.
- Physical inactivity. The less you move, the higher the chance of developing obesity with further progression of atherosclerosis.
- High blood pressure (BP). The chance of developing anterior, lateral or inferior myocardial infarction in hypertensive patients is higher than in patients with normal blood pressure.
- Stress. Emotional stress leads to vasospasm, which, given the presence of plaques, increases the risk of their rupture with the development of acute thrombosis and artery blockage.
- Age, gender Men over 50 occupy a leading place among patients with heart attacks of various locations.
Genetic predisposition also plays a role in the development of the disease. If you have close relatives who have suffered or died from a heart attack, you should be more attentive to risk factors and visit the doctor more often.
Symptoms
An infarction of the anterior wall of the heart (as well as another localization) is accompanied by the appearance of characteristic clinical signs that allow one to immediately suspect the disease.
Typical signs
When talking with patients suffering from hypertension or other heart diseases, I always pay attention to signs that may indicate the onset of acute infarction of the anterior wall of the left ventricle:
- Burning, pressing pain in the region of the heart. Many of my patients have described the symptom as “being squeezed in a vice” or “an elephant stepping on the chest.” A feature of a heart attack is the irradiation (spread) of pain to the left arm, neck, jaw or under the shoulder blade.
- The duration of the attack may exceed 30 minutes.
- Ineffectiveness of the tablets used. My patients always keep antihypertensive medications at home, Nitroglycerin and Validol. In case of a heart attack, these drugs will not bring relief.
Most of my patients can clearly indicate the moment of pain. The attack is often associated with a stressful situation or excessive physical activity. However, in my practice there have often been patients in whom a heart attack developed in the absence of any provoking factors.
Atypical manifestations
The clinical picture described above remains classic. It is characteristic mainly of anterior infarction. However, plaque rupture with thrombosis can also occur in arteries that supply blood to other parts of the heart.
In case of myocardial infarction of the inferior wall of the left ventricle, the following atypical signs come to the fore:
- Nausea, vomiting. One patient told me how he ate a heavy meal and his abdominal discomfort suddenly began to increase. Before seeking help, he took 4 tablets of drugs to improve digestion. The ambulance team diagnosed an inferior infarction.
- Isolated shortness of breath with a tendency to increase the intensity of the symptom. In this case we are talking about a disease.
- Weakness with episodes of dizziness. Patients lose consciousness extremely rarely.
- Painless form of ischemia. A relatively rare variant of the development of the disease. The patient may only notice weakness and a desire to rest.
I always tell my patients that if at least one of the symptoms described above occurs, they should consult a specialist. It is quite easy to miss a heart attack that develops in the lower wall of the left ventricle. However, it is not easy to treat it after losing precious time.
Diagnostics
Inferior, posterior or anterior myocardial infarction is diagnosed in the same way. First, I always collect a medical history and evaluate the patient's complaints. Most often, chest pain alone is enough to raise suspicions.
To confirm my guess, I use auxiliary instrumental and laboratory examinations.
Instrumental methods
The basis for diagnosing any myocardial infarction is an ECG. It is impossible to overestimate the importance of the electrocardiogram in ischemic heart disease. The technique allows you to see on paper or a screen the slightest deviations in the electrical function of the heart, which always occur when the supply of certain areas of the myocardium with blood is disrupted.
Possible changes on the film:
- elevation (rise) or depression (subsidence) of the ST segment relative to the isoline;
- inversion (change of polarity to the opposite) of the T wave;
- formation of a deep and wide (pathological) Q wave.
There are indirect signs on the ECG that may indicate an anterior infarction or damage to the other wall of the left ventricle.
To clarify the location and extent of damage to the heart muscle, I always additionally prescribe the following studies:
- Angiography of the coronary vessels. After contrast is injected into the coronary arteries, I see the blockage site on the monitor screen, which allows me to quickly restore the patency of the vessel using stenting.
- Echocardiography (Echo-CG). Ultrasound examination of the heart allows you to see a decrease or complete absence of contractions of the affected area of the myocardium (hypo- or akinesia).
In 98% of cases, the instrumental methods described above are sufficient to make a final diagnosis.
Laboratory methods
Laboratory tests are excellent assistants in the early stage of disease verification. The most reliable blood test remains for troponin I. The latter is a protein found in cardiomyocytes. When myocardial cells die, troponin enters the blood, where it can be fixed. For more information on how it is made, read the article at the link.
Additional laboratory tests:
- General blood analysis. During a heart attack, the number of leukocytes may increase and the erythrocyte sedimentation rate (ESR) may increase.
- Blood chemistry. The amount of C-reactive peptide, AST, and ALT may increase.
- Coagulogram. The analysis demonstrates the function of blood clotting. In heart attack patients it is often too pronounced.
Among laboratory tests, I, like the vast majority of cardiologists, first of all do a troponin test. Other tests are of secondary importance.
Consequences and possible complications
The prognosis for a patient with a heart attack always depends on timely consultation with a doctor.
When providing qualified assistance to the patient within the first 2 hours after the onset of the attack, it is likely to prevent the development of necrosis of the heart muscle.
A similar prognosis is possible thanks to rapid thrombolysis and stenting. However, people often endure pain and hope that it will “go away on its own,” thereby wasting precious minutes and increasing the affected area.
The most common complications of the disease that I often encounter:
- Deterioration of the contractile function of the heart with the development of failure.
- Various types of rhythm and conduction disorders.
- Chronic cardiac aneurysm. Due to the thinning of the affected myocardium, a protrusion forms in the wall, in which blood clots can form.
The most severe consequence of a heart attack is death. However, with adequate therapy and a successful combination of circumstances, patients can live well for decades even after suffering a heart attack. You can read about what medications and for how long to take after discharge from the hospital.
My advice to patients is quite simple:
- quit smoking;
- be less nervous about trifles;
- rationalize nutrition: there is no need to give up your favorite dishes, the main thing is moderation;
- undergo regular preventive medical examinations;
- move more and do as much physical exercise as possible.
It is almost impossible to completely protect yourself from a heart attack. However, thanks to the basic points mentioned above, you can not only improve your well-being, but also prevent the progression of more than two dozen internal diseases.
A 49-year-old man was admitted to our clinic with severe pressing pain behind the sternum, which radiated to the left arm. The patient attributes the symptoms to stress due to a quarrel with his wife.
It took 2 hours from the moment the symptom appeared to seeking help. On the cardiogram, ST segment elevation in V1-V4 and the formation of a pathological Q wave in I, aVL, V1-V4. During bedside echo-CG, no zones of hypokinesia were identified.
The troponin test is positive. Blood pressure – 130/90 mm Hg. Art.
The patient was sent for urgent coronary angiography. Total occlusion of the anterior descending branch of the left coronary artery was discovered. Stenting was performed with the placement of a metal stent.
As a result, a diagnosis was made: anteroseptal myocardial infarction.
On the third day after stenting and taking appropriate drug therapy, the patient notes an almost complete normalization of his condition.
Source: https://cardiograf.com/ibs/nekroz/infarkt-perednej-stenki.html
What diseases cause myocardial contractility disorders?
graphs of changes in myocardial contractility in various situations
Disturbances in global or local myocardial contractility can be caused by diseases characterized by the presence of inflammatory or necrotic processes in the heart muscle, as well as the formation of scar tissue instead of normal muscle fibers. The category of pathological processes that provoke a violation of local myocardial contractility includes the following:
- Myocardial hypoxia in coronary heart disease,
- Necrosis (death) of cardiomyocytes during acute myocardial infarction,
- Scar formation in post-infarction cardiosclerosis and LV aneurysm,
- Acute myocarditis is an inflammation of the heart muscle caused by infectious agents (bacteria, viruses, fungi) or autoimmune processes (systemic lupus erythematosus, rheumatoid arthritis, etc.),
- Postmyocardial cardiosclerosis,
- Dilated, hypertrophic and restrictive types of cardiomyopathy.
In addition to pathology of the heart muscle itself, pathological processes in the pericardial cavity (in the outer lining of the heart, or in the heart sac) can lead to disruption of global myocardial contractility, which prevent the myocardium from fully contracting and relaxing - pericarditis, cardiac tamponade.
In acute stroke and brain injury, a short-term decrease in the contractility of cardiomyocytes is also possible.
More harmless causes of decreased myocardial contractility include vitamin deficiency, myocardial dystrophy (with general exhaustion of the body, dystrophy, anemia), as well as acute infectious diseases.
Risk factors for akinesia
Parkinson's disease
- a disease in which there is a decrease in the production of dopamine in the brain, which affects a person’s ability to control their muscles.
Drug-induced parkinsonism
- develops as a result of the fact that a person takes too many drugs that inhibit dopamine.
Progressive supranuclear palsy
is a condition that gradually damages the brain, initially affecting balance while walking.
Hormones – Hypothyroidism or low thyroid hormone levels can lead to akinesia.
In people with Parkinson's disease, men are more likely to experience akinesia than women.
Other risk factors:
- bradykinesia or slow muscle movement;
- Parkinson's disease that lasts for a long time;
- postural instability;
- problems with muscle stiffness.
Are clinical manifestations of impaired contractility possible?
Changes in myocardial contractility are not isolated, and, as a rule, are accompanied by one or another myocardial pathology. Therefore, among the patient’s clinical symptoms, those that are characteristic of a specific pathology are noted. Thus, with acute myocardial infarction, intense pain in the heart region is observed, with myocarditis and cardiosclerosis - shortness of breath, and with increasing systolic dysfunction of the LV - edema. Heart rhythm disturbances (usually atrial fibrillation and ventricular extrasystole) are common, as well as syncope (fainting) conditions caused by low cardiac output and, as a consequence, low blood flow to the brain.
Phoenix Heart
Currently, it is not possible to completely restore muscle tissue and eliminate cardiac hypokinesia. It is important not to let the process worsen and prevent complications from developing.
Treatment of cardiac hypokinesia is carried out by a cardiology doctor. The main goals of therapy are as follows:
- eliminate the root cause of hypokinesia;
- eliminate factors that may aggravate the problem in the future;
- support cardiac activity;
- prevent the development of complications;
- if possible, improve the patient’s quality of life.
Treatment of patients with cardiac hypokinesia is carried out taking into account the degree of damage to the organ, as well as taking into account the existing symptoms.
The following groups of drugs are most often prescribed:
- ACE inhibitors;
- glycoside cardiotonic drugs;
- β-adrenergic receptor blockers;
- aldosterone receptor blockers;
- diuretics.
Prescribing a treatment regimen based on the listed drugs allows you to stabilize cardiac activity and normalize the load on the heart muscle. All appointments are carried out exclusively by a cardiologist. Self-administration of medications is unacceptable.
| Dosage and method of administration | Side effects | special instructions | |
| Captopril | Take 6.25-50 mg, up to 3 times a day, with a maximum daily dose of 150 mg. | Dizziness, orthostatic decrease in blood pressure, changes in taste sensations. | Captopril is an ACE inhibitor. It reduces the load on the myocardium and lowers blood pressure. |
| Bisoprolol | Take 1.25-10 mg once a day. | Facial redness (hot flashes), dizziness, bradycardia. | Bisoprolol normalizes cardiac activity and reduces hypoxia. |
| Furosemide | Take from 20 to 500 mg per day, on an empty stomach. | Nausea, itching, temporary hearing loss, headache, depression, dry mouth. | Furosemide eliminates edema, reduces stress and facilitates heart function. |
| Digoxin | Take 0.125 mg up to 2 times a day, with a maximum daily dose of 0.25 mg. | Dyspepsia, feeling tired, headaches, heart rhythm disturbances. | Digoxin is a cardiac glycoside, but it is prescribed only for a short time - only to relieve symptoms. |
| Spironolactone | Take 25-50 mg per day, in the morning or afternoon, in 1-2 doses. | Dyspepsia, drowsiness, lethargy, menstrual dysfunction in women and erectile dysfunction in men. | Spironolactone improves cardiac compensation. It is an aldosterone antagonist. |
In case of cardiac hypokinesia, vitamins must be prescribed - complex preparations with a mandatory content of B vitamins are especially useful. The drugs of choice may be Angiovit, Centrum, Neurobeks, Vitrum Centuri: these vitamin supplements can improve nerve conduction and prevent complications from the cardiovascular system.
Physiotherapeutic treatment
For various heart disorders - for example, with cardiosclerosis or myocardial hypokinesia, doctors advise practicing balneotherapy using carbon dioxide, sodium chloride, iodine-bromine baths. If there is no arrhythmia, then it is also possible to use baths with hydrogen sulfide.
To improve immune defense, inductothermy is used with an effect on the adrenal glands.
If the cause of hypokinesia is atherosclerosis (cardiosclerosis), then the doctor may prescribe electrophoresis procedures with novocaine to Zakharyin Ged’s zones. The duration of one session is from six to 15 minutes, the frequency is every day or every other day. One course may require from 8 to 20 sessions. Such procedures will improve blood circulation and the functional ability of the myocardium.
For mild forms of hypokinesia, patients are advised to undergo sanatorium-resort treatment.
Traditional treatment
With cardiac hypokinesia, you cannot do without traditional methods of treatment. There are many known remedies and medicinal plants that help alleviate the patient’s condition by improving the functioning of the cardiovascular system. For example, you should pay attention to such recipes.
- Mix 1 tbsp. l. chopped hawthorn rhizome and 1 tsp. caraway seeds, brew in a thermos in 300 ml of boiling water overnight. In the morning, the infusion is filtered and drunk throughout the day.
- Prepare a kind of cocktail from two raw chicken proteins, 2 tsp. sour cream and 1 tsp. honey This cocktail should be drunk every morning on an empty stomach.
- You should eat 150 g of fresh homemade cottage cheese every day.
- Juice or compote is prepared from rowan berries (both red and chokeberry). You can also use the rhizome of the plant.
- Prepare a two-hour infusion of buckwheat flowers (1 tablespoon of flowers per 500 ml of boiling water). Drink 100-150 ml infusion 3-4 times a day.
- Every morning they eat one lemon, crushed in a meat grinder and mixed with honey and sugar.
For cardiac hypokinesia, berries and leaves of currants, blackberries, cranberries, as well as bird cherry flowers and garlic will be beneficial.
Herbal treatment
- Prepare a mixture of crushed herbs: 1 tbsp. l. yarrow, one and a half spoons each of hawthorn, mistletoe and periwinkle foliage. Pour 1 tbsp. l. the resulting mixture 300 ml of boiling water, leave for about an hour. Drink the resulting infusion throughout the day.
- A herbal mixture is prepared from 20 g of lemon balm, 10 g of lily of the valley, 30 g of cinquefoil and the same amount of rue. One tablespoon of the resulting mixture is poured into 200 ml of boiling water and filtered after an hour. Drink 1 tbsp three times a day. l. before meals.
To strengthen the heart, you can use more complex herbal mixtures. The ingredients usually used are sage, peppermint, drop cap, clover, calendula, chicory blossom, lingonberry leaves, oregano, and sweet clover.
Depending on the indications, after consulting a doctor, infusions based on valerian rhizome and motherwort are used - such drugs are especially relevant in the presence of spasms and cardioneurosis.
Homeopathy
There are reviews about the positive effect of homeopathic medicines on the well-being of patients with cardiac hypokinesia. What drugs are we talking about, and when can they be taken?
- Arnica 3x, 3 – when the heart muscle is overloaded;
- Aurum – if hypokinesia is caused by hypertension or atherosclerosis;
- Barita carbonica in dilutions of 3, 6, 12 – if cardiac hypokinesia is provoked by age-related cardiosclerosis;
- Phosphorus 6, 12 – for hypokinesia caused by myocardial dystrophy;
- Calcarea arsenicosis 3, 6 – with hypokinesia due to cardiosclerosis;
- Graphite 6, 12 – for dystrophy of the heart muscle;
- Crategus 0.2x – for arrhythmia against the background of cardiac hypokinesia;
- Adonis 0.2x – for heart rhythm disturbances, shortness of breath and swelling;
- Ammonicum carbonicum 6 – for cardiac hypokinesia, with symptoms such as blue discoloration of the nasolabial triangle, cough and shortness of breath during exercise.
Homeopathic remedies are used along with drug therapy as an auxiliary type of treatment. These drugs are harmless and quite effective if properly selected by a qualified homeopathic doctor.
Surgery
Surgical intervention for cardiac hypokinesia is a cardinal type of treatment and is carried out only in severe and life-threatening situations for the patient. In this case, the most effective way to eliminate painful signs and restore adequate trophism is a heart transplant.
Typically, transplantation is recommended for diffuse myocardial damage, or for severe cardiac failure due to deep myocarditis. In cases of relatively mild cardiac hypokinesia, transplantation is considered inappropriate: drug therapy is sufficient.
Transplantation is prescribed:
- when cardiac output decreases to less than 20% of normal levels;
- patients under 65 years of age;
- in the absence of effectiveness of conservative treatment.
Surgery is not prescribed unless the true cause of hypokinesia is established.
In addition to transplantation, palliative surgical treatment may be used in some cases:
- Coronary bypass surgery is performed when coronary circulation is impaired and the vascular lumen is narrowed.
- Corrective surgery for an aneurysm involves removing the damaged section of the vessel or strengthening it.
- Installation of a pacemaker - used for severe heart rhythm disturbances.
Source: ilive.com.ua
Do contractility disorders need to be treated?
Treatment of impaired contractility of the heart muscle is mandatory. However, when diagnosing such a condition, it is necessary to establish the cause that led to impaired contractility and treat this disease. Against the background of timely, adequate treatment of the causative disease, myocardial contractility returns to normal levels. For example, in the treatment of acute myocardial infarction, areas subject to akinesia or hypokinesia begin to normally perform their contractile function 4-6 weeks after the onset of the infarction.
Are there possible consequences?
If we talk about the consequences of this condition, then you should know that possible complications are caused by the underlying disease. They can be represented by sudden cardiac death, pulmonary edema, cardiogenic shock during a heart attack, acute heart failure during myocarditis, etc. Regarding the prognosis of impaired local contractility, it should be noted that zones of akinesia in the area of necrosis worsen the prognosis in acute cardiac pathology and increase the risk of sudden later cardiac death. Timely treatment of the causative disease significantly improves the prognosis, and patient survival increases.
Preventing the development of the disorder
Preventive measures are based on following the rules of a healthy diet and regular physical activity. It is recommended to take walks and engage in acceptable sports. You don’t have to use an elevator, get to work on foot, etc. All this will have a beneficial effect on the body.
It is important for people with sedentary jobs to take breaks and do at least a minimal warm-up. You should carefully consider improving your workplace, for example, purchasing a chair with a fixed back.