Today, coronary heart disease refers to a whole complex of diseases. All of them are characterized by unstable blood flow in the arteries responsible for ensuring the functioning of the myocardium. Insufficient blood supply in this case may be caused by narrowing of the coronary vessels.
Such a pathology can manifest itself under the influence of both external and internal factors. How is ischemia determined on an ECG, is it possible to protect yourself from such a disease, and what does the course of treatment include? We will try to understand these questions in this review.
Causes
Coronary heart disease can lead to disability and even death. According to the World Health Organization, this disease causes the death of 7 million people every year. The death rate could double by 2020. Men aged 40 to 62 years are at risk.
However, the risk of disease increases significantly when exposed to the following negative factors:
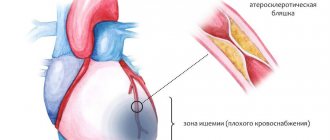
- Atherosclerosis is a disease that affects the arteries located in close proximity to the heart muscle. As a result, the walls of blood vessels become denser and lose their elasticity. The lumen can also narrow due to plaques formed by calcium and fat.
- Spasm of the coronary vessels - such an ailment is caused by the development of atherosclerosis, but can form without it. May appear as a result of stress. Spasm has a negative effect on the functioning of the arteries. With hypertension, the heart has to fight high pressure in the aorta. This can impair circulation, causing angina and heart attack.
- Thrombosis. As a result of plaque disintegration, a blood clot may form in the coronary artery. The vessel can also be blocked by a blood clot formed in another part of the circulatory system.
- Congenital and acquired defects.
Consequences
A person who wants to live a long time must take care of his health, because a pathological complication in the form of myocardial infarction has many consequences.
Complications to be aware of:
- Transmural (extensive) infarction, affecting the entire thickness of the myocardium, can lead to rupture and even immediate death.
- With pathology that has developed in the left ventricle of the heart, fibrillation may begin, which is also a serious complication, often leading to death.
- A posterolateral infarction affecting a large area of the heart can result in protrusion of the anterior wall of the cardiac chamber. Thinning caused by pathology leads to the development of an acute aneurysm. Recovery of a patient with such a complication takes a lot of time.
Thromboembolism is a complication consisting of blockage of a coronary vessel by a blood clot (thrombus), leading to impaired cerebral circulation, lung damage, and problems in the diaphragmatic region of the gastrointestinal tract. Rehabilitation of such a patient takes a very long time.
Risk factors
Why does myocardial ischemia occur? On the ECG, the first signs of this disease can usually be seen after 40 years. In this case, a factor such as heredity is of great importance. If the parents suffered from coronary artery disease, then the children will most likely have a similar disease.
Negative factors also include:
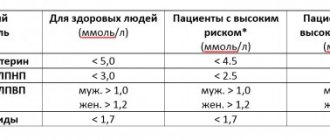
- increased blood cholesterol levels;
- disorders of fat metabolism;
- obesity of any degree;
- diabetes;
- sedentary lifestyle;
- frequent disorders and character traits;
- gender: among men, coronary heart disease is more common;
- poor nutrition.
When and how often to do it
An ECG is included in the list of mandatory tests when passing a medical commission. Therefore, once a year, a healthy adult should have a cardiogram. This is important because heart problems do not always show symptoms.
If a person has already been diagnosed with myocardial ischemia, he needs to undergo an ECG at least once every 1-3 months, and if his condition worsens, immediately during an attack. Only in this case is it possible to avoid the development of a heart attack. With the same frequency, it is necessary to check the condition of the heart in diseases that are provoking factors of ischemia:
- diabetes;
- hypertension;
- severe toxicosis in pregnant women;
- systemic pathologies;
- disorders of the thyroid gland.
Cardiography should be done a little more often in elderly people and people whose profession is associated with a high risk of developing coronary artery disease.
Important information: How to treat chronic (cerebral) ischemia of cerebral vessels with folk remedies in adults and what are the symptoms of ischemic head disease of 1 (2) degree
Classification
What is she like? Experts identify several forms of coronary heart disease:
- Primary cardiac arrest.
- Acute coronary insufficiency.
- Angina pectoris is a form of coronary artery disease characterized by squeezing and pressing discomfort.
Typically, such manifestations are mainly localized behind the sternum. Painful sensations and discomfort may also radiate to the left arm, epigastric region, and jaw. This pathology usually develops as a result of physical activity. There are several forms: primary, progressive, vasospastic.
How often should a cardiogram be done for a patient with coronary artery disease?
The diagnosis of IHD is established only on the basis of a detailed survey, examination, description of an ECG at rest and taken during an attack, with physical activity and, if necessary, echocardiography and coronary angiography.
Often in the early stages of coronary artery disease, ischemic signs are not detected on an ECG taken during the interictal period. Pathology is found when performing functional exercise tests or Holter monitoring. These methods help to identify hidden areas of damage and register a silent form of ischemia, which is more dangerous.
According to the rules of medical examination, patients with stable coronary artery disease undergo an ECG annually.
In patients with a newly established diagnosis, for whom adequate therapy is being selected, a cardiogram is performed more often.
An unscheduled ECG is indicated when:
- pain attacks that are atypical for a particular patient;
- prolonged episodes of angina pectoris;
- the occurrence of rhythm disturbances.
Additionally, an ECG for myocardial ischemia is indicated before performing bicycle ergometry, coronary angiography, stenting and coronary artery bypass grafting.
Consequences and complications
Coronary heart disease, in the absence of the required therapy, can lead to the formation of progressive heart failure. Muscle contractility weakens. As a result, the heart stops providing the body with the required amount of blood. Patients with cardiac ischemia become fatigued quickly and experience constant fatigue. If no measures are taken to treat the disease, the matter may result in disability or even death.
Information on ECG results
An ECG for coronary heart disease may contain the following information depending on the form of the disease:
- Coronary sharp teeth on the graphic tape with a large amplitude and symmetrical arrangement, which indicates hypoxia of the heart tissues, which do not receive a sufficient volume of blood. The teeth themselves can be positive or negative, which is determined by the location of the affected area.
- Ischemic injuries are characterized by a shift of the ST region above or below the isoline. The permissible deviations of this indicator are no more than 0.5 mm.
- The development of myocardial infarction is indicated by the detection of Q waves of the electrocardiogram, which exceed standard values against the background of a gradual increase in the amplitude for R waves.
- If acute myocardial infarction occurs, the ECG results indicate a shift in the ST region with T-waves for up to half an hour, although this may be a symptom of other ailments.
- Another characteristic sign of ECG results for coronary artery disease is the so-called reverse changes. First of all, a rise in the ST region is noted in conjunction with a clear decline in this zone, which is recorded by electrodes located on the other side of the heart.
First signs
Of course, subendocardial ischemia is immediately noticeable on the ECG. But there are symptoms that will help identify coronary insufficiency in the early stages, even without additional examinations. They can appear individually or in combination. Here everything largely depends on the form of the disease. There is a direct connection between the development of pain localized in the heart area and physical activity.
Also, unpleasant sensations can appear under unfavorable conditions and after a heavy meal. With ischemic heart disease, patients usually experience pressing pain. It seems to a person that he feels a lack of air, and heaviness increases in the chest. The pain is usually localized along the left edge of the sternum. Unpleasant sensations can spread to the arm, shoulder and shoulder blade. As a rule, attacks of pain last no more than 10 minutes. After taking nitrates, they gradually subside.
Other symptoms include:
If the patient does not seek medical help, swelling of the lower extremities will also be added to the symptoms listed above.
Causes of myocardial ischemia
Myocardial ischemia can be associated with many factors. Predisposing factors that increase the risk of developing myocardial ischemia are male gender and age over forty-five years.
In women, cardiovascular diseases develop less frequently, more often after menopause (an increased risk of developing pathologies of the cardiovascular system in the postmenopausal period is associated with a decrease in estrogen levels).
In patients under eighteen years of age, circulatory disorders are most often associated with congenital anomalies of the coronary arteries, viral coronaritis, dilated and hypertrophic cardiomyopathies, congenital malformations of the cardiovascular system, etc.
The development of severe dyslipoproteinemia not only increases the risk of development and rapid progression of atherosclerotic vascular damage, but also contributes to the disruption of metabolic processes in myocardial cells.
How to diagnose the disease?
Many people believe that IHD can be determined by an ECG. Signs of myocardial ischemia can also be established by performing the following examinations:
- Anamnesis collection. For this purpose, the doctor must ask the patient in detail about the nature of the pain, discomfort, and its location. The doctor will also find out whether the patient feels weak and has trouble breathing.
- Examination by a cardiologist. At this stage, the doctor should listen to the heartbeat for the presence of wheezing and murmurs. Also during the examination, the doctor measures your blood pressure level.
- General blood analysis. Allows you to identify the possible cause of ischemia. Experts evaluate indicators such as triglyceride and cholesterol levels. This is especially important for assessing the risk of vascular atherosclerosis. The level of troponins in the blood is also considered an important indicator. When heart muscle cells are destroyed, specific enzymes are released into the blood.
- Coagulogram. With coronary heart disease, blood clotting increases significantly.
- Electrocardiography. Allows you to identify excess size of the left ventricle and other specific characteristics. A doctor can easily identify signs of ischemia on an ECG.
- Echo ECG. With this type of examination, the structure and size of the organ are assessed, and the blood flow inside the heart, the functioning of the valves and the degree of vascular damage are also studied.
- Daily monitoring. With this method of examination, special equipment reads the electrocardiogram within 24-72 hours. This procedure allows you to objectively assess the patient’s condition and accurately determine the causes of symptoms of coronary heart disease.
- Radiography. Used to detect left ventricular dilatation. This pathology may be a consequence of aortic dissection. This type of examination also allows us to identify other complications.
What to do if cardiac ischemia was detected on the ECG? As a rule, to make an accurate diagnosis, the doctor uses a whole list of additional examinations. These include stress tests, X-ray contrast examination, computed tomography, Doppler sonography, electrophysiological examination, etc.
Electrocardiographic signs of ischemic heart disease
Changes in the ECG in coronary heart disease are caused by oxygen deficiency resulting from pathology of the coronary vessels and energy disturbances in cardiomyocytes.
Techniques for detecting ischemia:
- Simple 12-lead ECG.
- With additional leads - for diagnosing certain localizations of ischemia that are not recorded with a regular ECG.
- Holter monitoring (cardiogram recording for 24-48 hours).
- ECG with physical activity (stress test) - to determine hidden pathology.
- With medicinal samples.
50% of patients with coronary artery disease at rest have no signs of ischemia on the ECG. Therefore, the “gold standard” in the outpatient diagnosis of such a disease is an exercise test. This procedure solves several problems simultaneously:
- identification of hidden coronary insufficiency;
- registration of fleeting rhythm disturbances;
- designation of the threshold of tolerance to physical activity.
Photo 1. Bicycle ergometry.
The most commonly used are bicycle ergometry or treadmill test (treadmill). In a person with healthy vessels, such a load causes dilatation of the coronary arteries and an increase in myocardial contractility, necessary to ensure adequate blood flow. In the case of coronary artery disease, the coronary arteries are already in an expanded state before the load and do not compensate for the need. As a result, angina pectoris occurs and ischemia is recorded on the ECG.
Bicycle ergometry is done on a special exercise bike. ECG sensors and a tonometer cuff are fixed on the patient to monitor hemodynamic parameters. The procedure lasts 15-20 minutes. During this time, the load gradually increases from 25 to 50 W. Patients with severe cardiac diseases are allowed to take short breaks.
The test is stopped if:
- changes in the ST segment on the ECG;
- attack of chest pain;
- drop in blood pressure;
- increase in blood pressure more than 200 mm Hg. Art.;
- achieving the threshold heart rate for a given age;
- severe shortness of breath;
- serious rhythm disturbances;
- dizziness, severe weakness, nausea;
- patient refusal.
Photo 2. Treadmill test.
The treadmill test differs from bicycle ergometry only in that the patient performs physical activity on a treadmill with a varying inclination angle.
Load tests are contraindicated if:
- acute coronary syndrome;
- unstable course of angina pectoris;
- severe circulatory failure;
- stroke;
- thrombophlebitis;
- hypertensive crisis;
- severe arrhythmias;
- decompensated heart defects;
- severe pain in diseases of the musculoskeletal system.
Ischemia slows down the repolarization processes in the cardiomyocyte or changes the direction of the electrical wave. On an ECG with coronary artery disease, these disturbances correspond to widening, depression and changes in the configuration of the ST segment. In acute coronary syndrome, the main pathological changes are observed in the QRS complex and the ST segment.
The degree of changes in the ECG is directly related to the extent of the process and the duration of ischemia. With stable angina, signs of coronary insufficiency may not be detected on a cardiogram taken in the interictal period. And in the case of MI, disorders are recorded both in the acute phase and after several years.
One of the early signs of insufficiency of coronary blood flow is the appearance of a distinct sharp border between the transition of the ST segment to the T wave. Further growth of the atherosclerotic plaque aggravates ST depression below the isoline.
Types of ST interval depression in coronary artery disease:
| Offset type | ST interval | T wave |
| Horizontal | Parallel and below the isoline | Positive (+), negative (-) or biphasic |
| Oblique descending | The degree of ST depression increases with distance from the ORS complex | +/-, smoothed |
| Arched, rounded upward | The degree of displacement varies throughout, in the shape of an arc | Any kind |
| Oblique ascending | The greatest ST depression is located immediately after the QRS | Positive, smoothed |
| Trough-shaped | Arc shape with a convexity, apex down | Any kind |
| Elevation of the ST segment above the isoline | Rounded, arc with apex downwards | Positive, smoothed |
Changes in the ST segment in coronary artery disease are most clearly visible in the leads:
- V4-V6;
- II, III;
- aVF, I, aVL.
Unlike acute coronary syndrome with ischemic heart disease, ST changes are stable over months and even years.
ST segment depression is present when:
- ventricular hypertrophy;
- myocarditis;
- pericarditis;
- therapy with Digitalis;
- hypokalemia;
- myocardial dystrophy;
- bundle branch block, WPW syndrome;
- acute pancreatitis, cholecystitis, cholelithiasis, diaphragmatic hernia (reflex reaction);
- pulmonary failure;
- pulmonary embolism;
- nicotine poisoning;
- Prinzmetal's angina;
- vegetative-vascular dystonia.
The greatest stability in ischemic heart disease is associated with changes in the T wave (the so-called “coronary”). This is a negative, symmetrical T wave with an amplitude of more than 5 mm, which signals serious ischemic damage to the myocardium. A rounded and irregularly shaped tooth indicates less pronounced changes in the heart muscle.
The farther the electrode is installed from the place that is supplied by the damaged vessel, the less pronounced the signs of ischemia on the ECG.
Changes in T waves are recorded in:
- left chest leads;
- I;
- aVL;
- III;
- aVF.
But similar changes in T waves are also observed with:
- pulmonary embolism;
- myxoma;
- myocarditis;
- constrictive pericarditis;
- ventricular hypertrophy;
- cardiac conduction blockades;
- electrolyte imbalance;
- excessive smoking;
- hypokalemia;
- dishormonal processes;
- stress;
- use of certain medications.
With a long course of coronary artery disease, the ECG shows a widening of the P wave. This is an unfavorable prognostic sign regarding the risk of acute coronary syndrome and atrial fibrillation.
Slowing of electrical conduction during ventricular systole (QT) is also observed. The heart, under conditions of oxygen starvation, which is caused by atherosclerotic cardiosclerosis, needs more and more time to contract.
Due to a decrease in coronary blood flow, arrhythmias and blockades occur:
- extrasystoles;
- sinus tachycardia, bradycardia;
- atrial flutter;
- paroxysmal tachycardia;
- atrioventricular block;
- Hiss bundle branch block.
The extreme degree of ischemia of the heart muscle is myocardial infarction. If necrosis involves all layers of the muscle, there is a high probability of fatal arrhythmia, cardiac arrest, rupture of the papillary muscles, thromboembolism, ventricular aneurysm, acute circulatory failure and cardiogenic pulmonary edema.
Using a standard ECG, reliable data regarding the location and area of the lesion are obtained already at the prehospital stage.
It is very difficult to diagnose posterior and basal MI when the left ventricle is affected at the site of contact with the diaphragm. In such cases, additional leads V7-V9 and dorsal along the Palate are required.
Determination of coronary artery disease by ECG
What is it? Using an ECG, the following forms of the disease can be detected:
- A silent form in which a person does not feel pain.
- Angina pectoris, characterized by significant pain in the sternum.
- Acute circulatory disorder resulting from thrombosis.
- Pathology of myocardial contractions.
All these degrees of cardiac muscle ischemia can be determined using a cardiogram. This method is based on the principle of recording cardiac impulses.
Causes
The number of true reasons that lead to the fact that the patient’s heart or atria begins to be insufficiently supplied with oxygen is large. Among them:
- increased cholesterol levels caused by obesity or poor diet, leading to the formation of cholesterol plaques on the walls of blood vessels;
- persistent hypertension, causing rapid myocardial depletion;
- bad habits (tobacco smoking, excessive alcohol consumption), leading to oxygen starvation of the body and IVS of the heart (hypertrophy of the interventricular septum);
- lack of exercise, leading to blood stagnation;
- age criteria (over the years, vascular walls lose flexibility, which leads to poor supply of blood and oxygen to the heart).
- Cardiac pathology of the posterior wall of the myocardium in its manifestation differs little from other types of infarction. The patient feels severe pain in the chest area. The pain may radiate to the left limb, subscapular region. The attack is often accompanied by the following symptoms:
- arrhythmia, expressed in disruption of the heart;
- sticky cold sweat suddenly appearing on the face;
- trembling in the limbs;
- low blood pressure;
- general weakness of the body.
An analysis of the condition of many patients showed that with posterobasal pathology, the characteristic symptoms are blurred, and the course of an acute attack is not accompanied by pain.
Diagnosing such a pathology is somewhat difficult even when using an ECG; due to atypical symptoms, the disease is often confused with a stomach disease such as gastritis.
How is the procedure performed?
An electrocardiogram is a safe and accurate method for determining ischemia of the heart muscle. All necessary operating parameters will be recorded within 10 minutes.
The procedure is carried out in the following order:
- The patient removes clothing from the chest and frees the leg area from the knee to the foot.
- The specialist conducting the examination lubricates the necessary areas with a special gel and secures the electrodes.
- The data will be transmitted through the electrodes to the sensor.
- The device displays the transmitted information on paper in the form of graphs.
- The specialist interprets the results obtained.
What is ischemia and how does it affect the myocardium?
Ischemia is a decrease in blood supply to an organ or tissue due to insufficient arterial blood flow. Short-term current limitation does not lead to irreversible damage, long-term limitation causes consequences in the form of tissue death (necrosis) of the area supplied by the diseased vessel.
The organs with a high level of oxygen consumption (heart and brain) are most sensitive to insufficient blood flow.
IHD is an acute or persistent discrepancy between the oxygen needs of cardiomyocytes and the ability of the circulatory system to provide its delivery due to diseases of the coronary arteries. In ischemia, decreased blood flow occurs due to a combination of vessel stenosis and impaired wall tone caused by endothelial dysfunction (the inner lining of the arterioles).
In most patients with coronary artery disease, the main pathological process in the coronary vessels is atherosclerosis. A specific symptom of the disease is pain in the chest during physical and emotional stress, which goes away with rest or after taking a Nitroglycerin tablet.
Myocardial ischemia develops when the lumen of the coronary artery is blocked by a cholesterol plaque by 70% or more. In such cases, even the maximum expansion of small vessels does not provide cardiomyocytes with blood in sufficient quantities and signs of oxygen starvation develop during physical or emotional stress. Arteries narrowed by 90% do not supply the heart with oxygen even at rest.
Drawing. Causes of narrowing of the lumen of the coronary vessels.
The process is aggravated by impaired microcirculation due to increased blood clotting and the formation of small blood clots in the branches of the coronary artery.
Ischemic damage to cardiomyocytes causes:
- Disturbances in the energy supply of cardiomyocytes.
- Changes in the properties and structure of cell membranes, enzyme activity and electrolyte imbalance.
- Failures of the genetic program of myocardial cells.
- Disorders of the autonomic innervation of cardiac activity.
- Myocardial remodeling (disordered growth of cardiomyocytes, increase in connective tissue mass).
Such changes lead to a progressive decrease in myocardial contractility, limitation of its functionality and the development of heart failure.
Ischemia does not persist for long. Either adequate blood flow in the organ is restored, or muscle fibers are damaged. The most vulnerable is the subendocardial (inner) layer of the myocardium, which is less well supplied with blood and is subject to pressure load.
Classification of IHD according to ICD-10:
- Angina:
- Stable.
- Unstable.
- With vasospasm.
- Unspecified.
- Acute myocardial infarction (MI):
- Transmural.
- Subendocardial.
- Repeated.
- Complications of MI.
- Other forms:
- Silent ischemia.
- Coronary thrombosis.
- Acute ischemic heart disease.
- Dressler's syndrome.
What does an ECG help determine?
An electrocardiogram allows you to identify pathologies in the cardiac cycle. Also, using such an examination, you can determine the signs of myocardial infarction and pathological changes in the heart muscle. Thus, the ECG helps to find out which area was most damaged. This type of examination is also used when symptoms appear in attacks.
Myocardial ischemia on the ECG looks like this:
Advantages of ECG for ischemic heart disease
Today, there is no better method for recording ischemic changes in heart tissue than an ECG. Therefore, it is the electrocardiogram that remains the main diagnostic technique that provides differentiated results. Its main advantages are as follows:
- Based on the results of the data recorded by the electrocardiograph, specialists get a complete picture of the state of the heart muscle and its possible damage, thanks to which it is possible to differentiate ischemia from damage to heart tissue and necrosis.
- Depending on the cardiogram, a general picture of the degree of damage to the heart muscle and its size is drawn up, and the exact location of the areas involved is determined.
Based on the cardiogram, a general picture of the degree of damage to the heart muscle and its size is formed
- The technique makes it possible to obtain many data regarding the pathological process occurring in the tissues of the heart, including its duration, based on which the most appropriate tactics for treating the disease are selected.
Decoding a graphic cardiogram demonstrates a complete picture of pathological processes, including the phenomena of depolarization and repolarization.
The main changes against the background of the patient's coronary artery disease are observed in the gastric complex, which is reflected in the monophasic QS and QRS curves.
Usually, with little involvement of the heart wall in the pathological process, the appearance of the QS complex is noted, and the myocardium continues its characteristic electrical signals. In cases where an interruption of the impulse is recorded, more significant damage is indicated; in this case, deviations appear in the QRS curve.
Treatment
The entire course of treatment for coronary heart disease is based on several principles.
These include:
- Regular cardio training (walking, swimming, gymnastics). The amount and duration of training should be determined by a doctor.
- Special diet. A patient suffering from coronary heart disease should not eat salty or fatty foods.
- Emotional peace.
Also, the patient’s condition can be maintained through the use of pharmacological drugs.
Myocardial ischemia - Main symptoms and methods of treatment of ischemia, advice from doctors
Diseases of the cardiovascular system are the leading cause of death in the world today.
More than 50% of people die due to vascular problems and heart failure.
The question of what is cardiac ischemia is asked by more than one person every day. The phrase “myocardial ischemia” means insufficient oxygen supply to the heart muscle.
Ischemia on the ECG is manifested by a characteristic set of symptoms and pathological changes that cannot be confused with another disease.
Etiology and pathogenesis of myocardial ischemia
The main cause of the disease is a decrease in the supply of arterial blood rich in oxygen to the myocardium.
Pathological processes causing myocardial ischemia:
- atherosclerotic narrowing of the heart arteries due to the formation of plaques in the stroma of the vessel. Each plaque consists of low- and very low-density lipoproteins, as well as platelets. When a plaque ruptures, acute ischemic injury of the myocardium is formed, otherwise known as a heart attack;
- inflammatory changes in the vascular wall: vasculitis, arteritis, systemic connective tissue diseases lead to impaired vascular permeability;
- viral and bacterial agents that multiply in the intima of blood vessels;
- toxic damage to the coronary vessels, causing their spasm. Can be formed due to excessive consumption of alcohol, nicotine, poisoning with heavy metals and mercury salts;
- a stressful situation that causes a massive release of adrenaline into the blood leads to a narrowing of the vascular lumen.
- hormone-dependent tumors of various organs and tissues.
As a result of malnutrition of the heart muscle, vasospasm develops, impaired oxidation of free fatty acids, accumulation of under-oxidized protein breakdown products, and lipid peroxidation is activated.
These changes lead to disruption of the nutrition of mitochondria, the main sources of energy production in cells.
Due to mitochondrial dysfunction, ion channels in the cardiac tissue do not function, and an imbalance of ions develops, which leads to impaired contractile function of the heart.
Types of myocardial ischemia
Depending on the location of the area of the heart that does not receive blood, ischemia of the entire myocardium is divided into subepicardial and subendocardial forms.
Subepicardial myocardial ischemia is localized directly under the outer layer of the heart muscle - under the epicardium. The damage zone is of sufficient size and extent from the epicardium to the endocardium, affecting all layers of the anterior and posterior walls.
With subendocardial ischemia, the inner part of the heart muscle, the endocardium, is damaged. The endocardium contains a large number of small capillaries and blood vessels that provide nutrition to the heart, so damage to it is particularly difficult.
Clinical picture of the disease
Typical ischemia of the entire myocardium consists of the following manifestations: pressing, burning pain behind the sternum with irradiation to the jaw, scapula or shoulder; feeling of lack of air and shortness of breath, weakness, cold sweat and pale skin.
The pain is accompanied by fear of death and goes away within 15-20 minutes after taking nitroglycerin.
In the abdominal form, the disease begins with nausea and vomiting, possibly diarrhea and abdominal pain.
After a few minutes, chest pain, rapid breathing and palpitations are added to these unpleasant sensations. Symptoms disappear within a few minutes after taking nitro-containing medications.
If the disease manifests itself in the form of an asthmatic attack, there is a high probability of confusing myocardial ischemia with an attack of suffocation. In the asthmatic form, a sharp lack of air initially develops, accompanied by chest pain, impaired sweating and pale skin.
After some time, the discomfort in the chest goes away, and only breathing problems remain. The most severe form for diagnosis is non-painful myocardial ischemia. It is practically asymptomatic for the patient, leaving necrotic changes in the affected vessels.
For the painless form, the most typical occurrence is the appearance of myocardial infarction at the end of the disease.
The cerebrovascular form occurs as an acute cerebrovascular accident and is characterized by loss of consciousness, impaired spinal reflexes, and loss of the ability to read and write for a short period of time.
After the attack ends, the patient may experience the following symptoms: dizziness, headache, nausea and weakness.
The peripheral form of ischemia begins with pain in the arms or legs, gradually moving to the heart area.
The limbs become cold and pale, wet to the touch. The pulse quickens, the frequency of respiratory movements gradually increases. Symptoms of damage to the cardiovascular system appear after a few hours.
Diagnostic measures
To diagnose this disease, many reliable laboratory and instrumental techniques are used. Most hospitals use a primary medical examination and patient interview, which allows one to suspect ischemic changes in the heart and identify specific symptoms and symptomatic complexes.
When listening to the patient's chest, rhythm and conduction disturbances can be detected, indicating a pathological process occurring in the body.
To confirm the diagnosis, the following laboratory methods are used:
- a general analysis of urine and blood with determination of the number of platelets allows us to judge disorders in the hematopoietic system and bone marrow pathology;
- biochemical analyzes provide information about the main markers of myocardial necrosis: troponins, myoglobin, creatine phosphokinase fraction. You also need to measure the main indicators of the liver and observe them over time;
- A coagulogram and hemostasiogram are used to determine blood clotting time and diagnose disorders in the blood coagulation system.
Of the instrumental methods, electrocardiographic examination of the heart is most widely used.
An ECG is taken at the time of an attack, with the participation of stress tests (pharmacological tests, cold and heat tests, stress test, through esophageal stimulation of the ventricles, bicycle ergometry), and 24-hour ECG monitoring, otherwise called Holter, is also very informative.
Myocardial ischemia on the ECG is manifested by ST segment elevation above the isoline.
X-ray examination of the chest in both projections reveals an increase in the size of the ventricles, which indicates a functional overload of certain parts of the heart. You can also see changes in the aorta: this vessel is most susceptible to changes.
On phonocardiography, you can see changes in heart sounds, the appearance of pathological noises, indicating rhythm and conduction disturbances, as well as indicating heart defects.
An echocardiogram of the heart or ultrasound allows you to see the size of the heart cavities, the thickness of the walls, determine the location and nature of the location of necrosis, and pathological changes in the myocardium.
It is a highly sensitive research method that minimizes the risk of making an incorrect diagnosis with these initial data.
Treatment of ischemia
If cardiac ischemia is detected, treatment should lead to the development of the body's compensatory capabilities and normalization of blood flow. To achieve positive results, the patient must change his lifestyle: eat rationally, avoid stress, give up bad habits, play sports (swimming, skiing, running, cycling are especially useful).
Doctors prescribe medications and physiotherapeutic procedures to patients. If they do not produce results, then surgery is recommended.
Drug treatment
In drug therapy, several groups of drugs are mainly used:
- nitrates (nitroglycerin and its derivatives) – relieve spasms, promote dilation of coronary vessels and facilitate the flow of blood and oxygen to the myocardium;
- beta-blockers (atenolol, metoprolol) – reduce heart rate and reduce myocardial oxygen demand;
- calcium antagonists (nifidipine, verapamil) – lower blood pressure and promote better exercise tolerance;
- thrombolytics (aspirin, heparin, cardiomagnyl, streptokinase) - reduce blood clotting, dissolve blood clots, restore vascular patency.
The doctor may also prescribe medications that reduce the concentration of cholesterol in the blood, increase the metabolic rate and remove lipids from the body.
It is recommended to consume vitamins P, E and ascorbic acid.
Physiotherapeutic methods
Physiotherapy gives excellent results: balneotherapy (iodine-bromine, chloride, radon, carbon dioxide baths), the use of a galvanic collar, laser therapy, electrophoresis, electrosleep, massage, physical therapy.
Treatment with traditional methods
For patients diagnosed with cardiac ischemia, treatment with folk remedies in combination with traditional therapy can provide effective results. It is recommended to take decoctions and infusions of motherwort, birch, valerian, eleutherococcus, horsetail, sweet clover, immortelle, yarrow, arnica, lemon balm, elecampane root, oats, hawthorn, rose hips, viburnum. Herbal preparations will be especially useful. They have a diuretic and calming effect, improve blood circulation.
Manifestations of ischemia on the electrocardiogram
It is quite difficult to answer unequivocally what the ECG results for IHD will look like on film. When hypoxia of the heart muscle occurs, the movement of electrical potentials slows down slightly, potassium ions leave the cells, which negatively affects resting potentials. At the same time, compensatory processes are launched, the heart begins to overstrain, pressing pain develops behind the sternum, and the patient is disturbed by an unpleasant feeling of lack of air.
Characteristic ECG signs in chronic ischemic heart disease and oxygen starvation of cardiac tissues are:
- Oblique or horizontal depression of the ST segment.
- Reduction of the T wave, or its movement below the horizontal line.
- Widening of the T wave due to slower ventricular repolarization.
- The appearance of a pathological Q wave with the development of large-focal necrosis.
- The dynamics of changes in the electrocardiogram, which is a sign of the “freshness” of the pathological process.
ECG signs of ischemic heart disease should not be ignored. Additionally, the image may show signs of arrhythmias and blockades, which arise as a complication of ischemic processes. In most cases, with the development of ischemia of the heart muscle on the ECG, the QRS complex retains its normal shape, since oxygen deficiency primarily affects the restoration (repolarization) of the ventricles, which completes the cardiac cycle within normal limits.
Clinical recommendations for ischemic heart disease will be given below.
Research methodology
The first ECG devices were introduced into the practice of medical workers in the 20s of the last century. The pioneers in the development of a method for diagnosing myocardial lesions based on the level of electrical conductivity were the Dutch doctor Einthoven and the Russian scientist Samoilov. Over time, the examination technique and the devices themselves have changed a lot.
Modern electrocardiographs are designed on the principle of voltage meters. To conduct a full ECG study, special electrodes are used that make it possible to record conduction disturbances in the heart muscle in 12 leads. This includes three standard leads, six chest leads and three unipolar leads, when signals are taken from the patient's limbs. In rare cases, it is necessary to resort to the use of additional electrodes to fix a larger number of leads, for example, esophageal ones.
The number of leads involved in the study depends on the design of the ECG apparatus, the place where the film removal process takes place, and the urgency of obtaining data on disorders in the myocardium. Ambulance teams are usually equipped with portable devices that can detect only gross pathology, but this is often enough to initiate intensive care in a timely manner.
Cardiology departments and centers are provided with more powerful equipment, which allows them to obtain a complete picture of the catastrophe in the patient’s heart. In difficult cases, ECG comes to the aid of cardiac ultrasound, coronary angiography and other, more complex methods for diagnosing cardiac pathology.
We recommend reading the article about laboratory tests to confirm a heart attack. From it you will learn how, based on diagnosis, the stage and severity of necrosis of the heart muscle is established.
Cardiogram for myocardial infarction
During a heart attack, sections of the myocardium die due to insufficient blood supply. The heart tissues become deficient in oxygen and nutrients and cease to perform their function. The heart attack itself consists of three zones:
- ischemia (initial degree, repolarization processes are disrupted);
- zone of damage (deeper disturbances, depolarization and repolarization processes are disrupted);
- necrosis (tissues begin to die, the processes of repolarization and depolarization are completely absent).
Experts note several types of necrosis:
- subendocardial (on the inside);
- subepicardial (outside, in contact with the outer membrane)
- intramural (inside the ventricular wall, not in contact with the membranes);
- transmural (throughout the entire volume of the wall).
ECG signs of myocardial infarction:
- the frequency of contractions of the heart muscle increases;
- The ST segment rises, its stable depression is observed;
- QRS duration increases;
- The R wave changes.
Common “failures” in the functioning of the heart and changes in the ECG associated with the development of necrosis:
| Graphic image on a cardiogram | The pathology that caused the change | Characteristic signs |
| Normal heart function | The ST segment and waves are normal. | |
| Subendocardial ischemia | Repolarization disorder – high pointed T wave. | |
| Subepicardial ischemia | T wave negative | |
| Transmural ischemia | Deep negative T wave | |
| Subendocardial damage | The ST segment changes - either rises or falls (depression) | |
| Subepicardial damage | ST segment elevation | |
| Subepicardial ischemia + subendocardial injury | ST segment depression and negative T wave | |
| Subepicardial injury + subepicardial ischemia | ST segment elevation and negative T wave | |
| Transmural damage | The elevation of the ST segment is more noticeable than with subepicardial damage, reaches the T wave in height and is combined with it in one line. The complex is popularly called “cat’s back”. It is registered at the initial stages of pathology, in its most acute stage. | |
| Transmural infarction | There is no depolarization or repolarization. Only the Q wave is recorded under the electrode - deep and combined with the S wave, therefore it is also called the QS wave | |
| Nontransmural infarction | “Irregular” Q wave, almost equal in size to the R wave (it is not high, because only part of the wall is repolarized) | |
| Non-transmural infarction + subepicardial ischemia | Pathological Q, reduced R wave, negative T. Normal ST segment | |
| Subendocardial infarction (non-Q) + subendocardial injury | Necrosis does not penetrate into the myocardium (a thin strip lies under the endocardium). The R wave is reduced, the ST segment is depressed |
Important! Intramural infarction (not Q) occurs within the myocardial wall. Depolarization bypasses it on both sides, so the Q wave is usually not recorded.
How does ischemia occur?
Ischemia occurs predominantly in older people. This is explained by the irreversible changes that a worn-out body undergoes. With age, degenerative processes are observed in the vessels, and material metabolism deteriorates. Other causes of ischemia include:
- genetic predisposition;
- physical inactivity;
- cardiac aneurysms;
- passion for alcohol or smoking;
- the presence of concomitant diseases such as obesity, diabetes, hypertension;
- lipid spectrum disorder.
It is worth noting that representatives of the fair sex are less susceptible to coronary disease than men, which is due to the hormonal characteristics of the female body. Estrogens, which have protective properties and prevent the development of atherosclerosis, help delay the encounter with this disease. But with the onset of menopause, the hormonal picture changes radically. Therefore, this disease is often diagnosed in women after 60 years of age.
Coronary artery disease is caused by impaired blood supply to the myocardium. To make an accurate diagnosis, the patient needs to have an electrocardiogram. An ECG during ischemia allows you to determine changes occurring in the work of the heart.