What if the condition does not improve? And if it is easier, then how many people can lie there?
ARO (anesthesiology-resuscitation department) or ICU (resuscitation and intensive care unit) is available in every hospital, ranging from the central district hospital (central district hospital in rural areas) to large clinics.
Patients with severe somatic pathology are treated there: acute period of myocardial infarction with complications: rhythm disturbances, pulmonary edema, cardiogenic shock), stroke, severe pneumonia with respiratory failure, diabetic comas, patients in the early postoperative period before recovery from anesthesia, severe polytrauma in an accident , high-altitude polytrauma, acute poisoning and many more severe pathologies.
In short: there are people with impaired vital functions; to maintain life, they need round-the-clock monitoring and mechanical ventilation (artificial ventilation).
The length of stay depends on the pathology with which the person is there. When the condition stabilizes (the average time spent in the ICU is from 2-3 days to 10 days ), the patient is transferred to a specialized department for further treatment.
Treatment is carried out by a resuscitator, attending physician or head of a specialized department, and consultations with related specialists are carried out.
It also happens that the patient remains in intensive care until the end of his days and dies there.
Depending on who it is, but still, almost all patients are brought out in a stable condition.
The word “reanimation”, which frightens and alarms the average person, is translated as “revival”. This is where the real struggle for human life takes place. In this department, the day is not divided into day and night: medical workers attend to patients every minute. The intensive care unit is a closed area of the hospital. This is a forced measure that is necessary so that no one and nothing distracts doctors from saving human life. After all, some of the patients will never be able to leave the cold walls of the intensive care unit.
Relatives of such patients are worried because they do not know how long they have been in intensive care. How resuscitation treatment is carried out, what factors are associated with the length of a patient’s stay in the “rescue” department, you will learn from our article.
Specifics of the resuscitation state
Resuscitation is a department of a hospital where emergency actions are carried out to eliminate violations of the vital functions of the body. No one can answer how many days the patient will spend between life and death. Recovery time is always individual and depends on the type of injury, the patient’s condition and the presence of concomitant complications that appeared after the injury.
For example, after the operation, blood flow and spontaneous breathing were restored. However, at this stage a complication is diagnosed: cerebral edema or infection. Therefore, monitoring the patient’s condition in the intensive care unit will continue until all complications are eliminated. After this, the patient will be transferred to a regular ward.
It is important to understand that relatives, acquaintances and friends cannot visit the patient in the intensive care unit. This rule applies to all visitors with rare exceptions. Let's tell you why.
All visitors bring a lot of bacteria and viruses on their clothes, bodies and hands. They are absolutely safe for a healthy person. But for patients in serious condition, they will cause a complex infection. Moreover, patients themselves can infect visitors.
There are several patients in the general intensive care unit. Their location does not depend on gender: patients are undressed and connected to numerous equipment. Not everyone will be able to calmly react to such an appearance of people close to them. Therefore, people who are worried about the condition of their relatives need to wait until the patients are transferred to therapy. There it will be possible to communicate normally, regularly visiting friends and relatives.
Let us consider the features of resuscitation treatment in patients whose critical health condition is associated with the most common pathologies: stroke and heart attack.
Stroke
A stroke is a dangerous change in the blood circulation of the brain. He spares neither women nor men at any age. Moreover, 80% of stroke cases are characterized by ischemic pathology and only 20% by the hemorrhagic type. It is impossible to predict when the cerebral hemorrhage itself will occur: the course of the pathology is unique for each patient. Therefore, each patient spends a different time in intensive care after a stroke.
How long a stroke will keep a person in the hospital depends on several factors:
- Localization and size of brain tissue damage;
- Severity of symptoms;
- Presence or absence of coma;
- Functioning of systems and organs: breathing, heartbeat, swallowing and others;
- Possibility of relapse;
- Presence of concomitant diseases.
As you can see, the patient will stay in the intensive care unit as long as his condition requires. Patients in the department are carefully examined every day, making a verdict on their further stay in the hospital.
It should be noted that in case of pathological changes in the brain, the patient is required to stay in intensive care for 3 weeks. This time is needed for the doctor so that he can track possible relapses and prevent them.
General standardization of stroke treatment involves a month. This period is approved by the Ministry of Health for the complete recovery of the patient. However, on an individual basis, the period of therapy is extended if it is determined that the patient needs further treatment and rehabilitation.
Stroke therapy includes 3 stages.
The first therapeutic course consists of basic treatment measures:
- Improve the functioning of the respiratory system;
- Adjust hemodynamics;
- Eliminate elevated body temperature and psychomotor disorders;
- Fight cerebral edema;
- Provide proper nutrition and care to the patient.
Read more Decision of the Arbitration Court of the Sverdlovsk Region
After restoration of the primary functions of the body, differentiated treatment follows. It depends on the type of stroke and the patient's condition.
- Eliminate cerebral edema;
- Adjust intracranial and blood pressure indicators;
- Assess the need for surgical intervention.
- Restore good blood circulation in brain tissue;
- Improve metabolism;
- Eliminate manifestations of hypoxia.
The larger the affected area in the brain tissue, the more time the patient will need to recover.
Also, relatives should know what happens to the patient when he falls into a coma. This dangerous complication occurs only in 10% of cases. A comatose state occurs due to instantaneous dissection of the brain vessels. No one knows how long it will last. Therefore, in this situation, it is important to quickly provide qualified emergency care and ensure regular monitoring of the patient’s condition.
Diagnostic and corrective therapy for comatose state consists of the following actions:
- Using constant hardware monitoring, the functioning of vital human organs and systems is monitored;
- Measures against pressure ulcers are used;
- The patient is fed through a feeding tube;
- The food is ground and heated.
If the patient is in an extremely serious condition, he may be placed in an induced coma. This is necessary to perform emergency brain surgery.
After the patient comes to his senses, therapy is aimed at combating the consequences of the attack: restoring speech and motor activity.
The reason for transfer to a general ward is the following improvements in the patient’s well-being:
- Stable pulse and blood pressure readings within an hour of diagnosis;
- Having the ability to breathe independently;
- Full awareness of the speech addressed to him, the opportunity to contact the attending physician;
- Complete exclusion of relapse.
Treatment is carried out in the neurological department. Therapy consists of taking medications and rehabilitation exercises aimed at developing motor activity.
Heart attack
The most dangerous consequence of heart disease is myocardial infarction. Severe pathology requires constant medical supervision, the timing of which depends on the severity and criticality of the condition.
As a rule, a heart attack and all other heart ailments require rehabilitation measures within 3 days from the onset of the attack. Then rehabilitation therapy begins in the general ward.
Treatment of heart problems occurs in 2 stages.
7 days after an attack is the most critical and dangerous time for the patient’s life. Therefore, it is extremely important for him to stay in the hospital for several weeks in order to completely eliminate the possible negative consequences of the attack.
An acute attack of a heart attack requires resuscitation. They are aimed at providing the myocardium with oxygen to maintain its viability. The patient is prescribed the following treatment:
- Complete rest;
- Analgesics;
- Hypnotic;
- Medicines that reduce heart rate.
The first day of resuscitation is important for further treatment. On this day, the need to use the following types of surgical intervention is decided:
- Installation of a catheter in the heart;
- Expansion or narrowing of an injured vessel;
- Coronary artery bypass grafting (helps restore blood flow).
The administration of drugs that stop the formation of blood clots is necessarily indicated.
After restoration of the necessary functioning of the heart muscle, the patient is transferred to the cardiology department for further therapy. Then the attending physician will provide a plan of rehabilitation actions, with the help of which cardiac activity will resume in a natural manner.
The duration of the recovery period depends on the following factors:
- Timeliness of emergency assistance during an attack;
- Age category (persons over 70 years of age suffer a more severe heart attack);
- The presence or absence of complications;
- Type of heart attack;
- Possibility of complications.
The patient is discharged from the hospital only if the patient’s condition meets the following indicators:
- Complete restoration of heart rhythm;
- No complications were identified.
The recovery period after rehabilitation treatment continues even after discharge from the hospital. The patient must change his lifestyle, correctly alternating periods of rest and physical activity. It is important to completely reconsider nutrition issues and give up bad habits. It is better to continue the rehabilitation period in a sanatorium-resort treatment setting.
“How many days do they stay in intensive care?” - this is the question I am often asked by people whose relatives are in intensive care for various reasons. So I’ll say right away that there is no clear answer to this question. Everything is very individual. A person can spend from a day to several months in intensive care, and this will depend on many factors:
- the patient's condition;
- reasons for entry;
- concomitant diseases;
- age, weight, individual characteristics.
The word “resuscitation” itself is scary, this is due to superficial knowledge of various fields of medicine (which is absolutely normal for an ordinary person), and also to the fact that our respected media very often intimidate people even more by distorting medical facts, either out of ignorance, either by his journalistic “calling”.
My specialty is anesthesiology and resuscitation, I am the doctor by whose decision the patient is transferred to the intensive care unit and the one who subsequently monitors the patient there and makes the decision on discharge. Therefore, I will tell you first-hand what and how it works there, why and why we transfer patients there, what kind of care there is and what prognosis can be given if your relative is admitted to the intensive care unit.
“In Russia, doctors do not turn off the ventilator. This is murder"
– Why is an artificial coma needed when the patient is specially put into such a state?
– I’ll say right away that doctors do not put patients into a coma. Patients are given deep medicinal sedation and put into deep sleep. And why did this term “artificial coma” appear? It was such a copy of translation. Several years ago, barbiturates were actively used to make the patient sleep, and in English the use of large doses was called “barbituric coma.” And so it happened.
– If a person finds himself in a vegetative state, what do they do with him? Are there special departments for such patients?
– Such patients are in the neurological department, in the intensive care unit, in the neurosurgical department, and then a consultation is held and their rehabilitation potential is determined. If it is high, the person is transferred to the rehabilitation department. If it is low, they are transferred to a palliative center for decent care and feeding.
– If a person has been in a vegetative state for a long time, is connected to a ventilator, but there is no hope, what happens? Are they turning off the ventilator?
– In Russia, doctors do not turn off the ventilator. Because this is euthanasia, murder. Euthanasia is prohibited in our country.
– Well, if suddenly there are 100 people on ventilators, will they be constantly supported?
– This case will be paid for by compulsory medical insurance and the state. The whole question is that we wean these patients in a vegetative state from mechanical ventilation; modern devices allow dosing. Yes, there are cases when the machine breathes 100% for the patient, and modern intelligent modes allow this load to be transferred. There is a term “weaning from ventilation” - this is a whole protocol for such patients. One of the tasks is to bring a patient in a vegetative state to spontaneous spontaneous breathing and then transfer him to a specialized department.
RIA Novosti/Vladimir Smirnov
But there is still a point. Unfortunately, during the vegetative state, many functions are weakened. And patients often die from secondary purulent-septic changes. First of all - from pneumonia.
– In your practice, have there been patients who were in a vegetative state and came out of it?
- Yes, they went out, but with disability. They learned to breathe on their own and began to fix their gaze. It seemed that they began to recognize loved ones. At this stage, we transferred them from intensive care, and I no longer observed their fate.
Why are patients transferred to intensive care?
Severe patients are transferred to the intensive care unit in agreement with the head of the department.
Read more Devices for measuring temperature in a boiler room
Reasons for translation:
- underlying disease (worsening condition - respiratory failure, critical circulatory disorder, confusion or loss of consciousness).
- condition after surgery (if an anesthesiologist-resuscitator notices that after surgery a person has not fully recovered vital functions, a decision may be made to transfer to intensive care, this minimizes risks, and the patient is under observation.
- emergency conditions - people from the ambulance can also be admitted to the intensive care unit (the criteria are the same) - acute heart attack, stroke, trauma, burns, frostbite, drowning.
Stages of treatment
Drug treatment in a hospital
Therapy is divided into 3 stages:
- intensive care unit therapy;
- hospital treatment;
- ambulatory treatment.
They stay in intensive care for up to 3 weeks. Treatment in a hospital lasts more than 3 months. Outpatient recovery can take place over 4 months. Temporary indicators depend on the severity of the disease. If recovery is slow, the time frame increases. But the treatment period cannot be reduced, otherwise the affected areas will not recover or the attack will cause more serious disorders.
How many people can stay in intensive care?
In order for you to understand how individual everything is, I will tell you several cases from my practice - you will find out how and why people ended up in intensive care and what happened then.
There are standard periods for a patient to remain in intensive care: Orders, Orders of the Ministry of Health. But in reality this is not always the case. All these documents are a pretty picture, but real life is a little different. It is not always possible for a hospital to keep a patient, for example, with a stroke for a whole month - there simply is not enough staff.
Case from practice: I worked in one of the cities near Moscow. It’s a small hospital, where the intensive care unit is designed for only two people. A husband and wife came to my duty after an accident (they crashed into a tree). I am one anesthesiologist-resuscitator, there is no one to replace me. The man had a ruptured spleen, an emergency operation was performed, the second patient (a woman) was in a coma and was placed in intensive care and transferred to mechanical breathing. They were under my supervision for two days; there was simply no one to replace me. On the first day it was somehow still possible to work, but on the second day I couldn’t even sit, then they sent a team and transferred the patients to the nearest larger hospital, after which I was able to complete my shift. What is shown in the movies is beautiful and interesting, but in real life everything is different.
Transfer to intensive care for pneumonia
Not everyone and not always are admitted to intensive care with pneumonia. If the condition is satisfactory, treatment in a hospital is possible. We will consider a case of severe pneumonia, in which transfer of the patient to the intensive care unit is directly indicated, because by all indications there was a serious threat to the patient’s life.
Case from practice. I was called to the therapy department, where a patient was admitted with suspected pneumonia. The patient is a man, 42 years old. On examination - shortness of breath (30-40 breaths per minute), pulse approximately 120, blood pressure 80/40, cyanosis of the nail plates and nasolabial triangle, acrocyanosis.
I assess the condition as extremely serious - I transfer the patient to intensive care, and immediately begin resuscitation measures. We insert the subclavian vein (in this case on the right), and begin anesthesia.
Tracheal intubation is performed, the patient is transferred to mechanical ventilation. In addition, be sure to place a catheter in the bladder.
A catheter is placed in the bladder to control diuresis (urine volume). Normally, it should be at least 30 ml/hour, and the doctor also evaluates the color of the urine. Kidney function is extremely important!
We also take other tests, ECG, chest x-ray. All this is done to clarify the diagnosis. We make sure to check that the endotracheal tube is positioned correctly. A little later we put in a gastric tube for feeding (this is not so urgent). The initial diagnosis was confirmed. The condition was stabilized. The patient spent 5 days in intensive care, during which time the underlying disease was treated as prescribed by the therapist + what the resuscitator prescribed.
On the 6th day, extubation was performed, the patient regained consciousness, and it took about two days to recover. After complete restoration of consciousness and vital functions, the patient was transferred to the ward and subsequently discharged.
That is why be vigilant, monitor your health and seek medical help in a timely manner.
Resuscitation after caesarean section
Normally, a caesarean section operation lasts about 30 minutes. It can be performed under general anesthesia or spinal (epidural) anesthesia. It depends on the wishes of the woman in labor, her individual characteristics and other factors.
In what cases may resuscitation be required after a caesarean section? This may be if the patient’s condition raises concerns among doctors, if something went wrong during the operation or if some complication occurred.
Again, a case from my medical practice. Maternity hospital, 9.30, 29-year-old woman, taken to the operating room for a planned caesarean section. Operation was successfully completed. The child’s condition is good, the mother is conscious, but her condition causes me concern (pale skin color, weakness). At this moment, labor begins in the next department, they call me there. I leave this patient under the supervision of a nurse anesthetist. Everything is fine in that department, they urgently call me back (to the first patient).
The woman is pale, rolls her eyes, loses consciousness. The blood pressure is not determined, the pulse is 140, I put the subclavian in place, and we begin anesthesia. An operation is being carried out, donors are invited for a warm blood transfusion. 00.30 - completion of the operation. The result is removal of the uterus, the patient is alive.
The reason for the sharp deterioration of the condition is DIC syndrome (disseminated intravascular coagulation - in other words, this is a very rare, dynamic process when a large number of blood clots form in the vessels in combination with blood incoagulability, which leads to numerous hemorrhages).
No one could have predicted such an outcome, so I want each of us to understand that doctors are not Gods. And we cannot predict anything, each organism is individual and it is simply impossible to predict how it will behave with any, even small, intervention. But our task is to do everything possible to save the patient’s life!
Resuscitation after stroke, heart attack
Stroke patients can stay in intensive care for up to 21 days. With stable hemodynamics and sufficient breathing, they are transferred to a specialized department.
Read more Check the cadastral registration of the house
If their condition is stable, then they are discharged home, and their relatives take care of them.
In case of an acute heart attack, if less than 6 hours have passed since the attack, patients are taken urgently to the operating room in the radiology department for angioplasty and stenting. After the operation, such patients can be discharged home after 3-4 days.
Duration of sick leave for myocardial infarction
After discharge, the patient is given a sick leave, which is drawn up by the attending physician. If it is necessary to extend its validity, a special medical commission is appointed. The specific duration of sick leave for incapacity for work after a heart attack depends on the severity of the pathology:
- small focal infarction without complications – 60 days;
- extensive large-focal and transmural – 60-90 days;
- complicated heart attack – 3-4 months.
If the following conditions are present, the patient is referred to a medical and rehabilitation expert commission to determine the fact of permanent disability:
- repeated (recurrent) heart attack;
- the presence of severe heart rhythm disturbances;
- chronic heart failure.
The commission determines the severity of the patient's condition and assigns him to one of the functional classes. Depending on the class, doctors decide the future fate of the patient - extend his sick leave, or give him a disability group.
There are four functional classes:
- I – ability to work is preserved, but patients are removed from night shifts, additional workloads, and business trips. In this case, it is recommended to change heavy physical work to lighter work;
- II – only light work is allowed, without significant physical exertion;
- III – patients are recognized as disabled if their activities are associated with physical work or psycho-emotional stress;
- IV – patients are considered absolutely unable to work, they are given a disability group.
Further rehabilitation
A heart attack is not a diagnosis, but a way of life. After the patient leaves the hospital bed, he will have a long period of rehabilitation, during which he will restore his health and performance.
A specific program is prescribed by a cardiologist and physiotherapist. In addition to drug therapy, it includes:
- Spa treatment;
- physical therapy – in accordance with the functional class of the disease;
- dieting and weight control - avoidance of flour and fatty foods, split meals;
- quitting smoking and alcohol, which can significantly reduce the risk of relapse;
- avoiding stress, including psychological training or meditation;
- constant independent monitoring of blood pressure and pulse.
It is also necessary to periodically undergo preventive examinations according to the following scheme:
- first month - every week;
- the first six months - once every two weeks;
- the next six months - once a month;
- in the future – once a quarter.
Why is anesthesia administered in intensive care?
You can often hear on TV or radio: “the patient has been placed in an induced coma.” This is not entirely true - the patient is under anesthesia, but not in an “induced coma”. Why do we give anesthesia? Firstly, if you or your relative end up in intensive care, it is not at all necessary that he will be there under anesthesia, but for seriously ill patients - yes, we really do provide anesthesia.
The goal is to help the patient cope with all disorders in the body, because in order to be conscious he needs to consume a lot of energy. In this case, it is simply a medical procedure. This is a guided medical intervention that makes breathing muscles and other organs easier to work with. This state can be maintained for as long as desired.
After extensive operations (for example, on the heart, lungs, with massive injuries), patients are definitely transferred for further treatment to prolonged mechanical ventilation. After relatively short and simple operations (up to an hour), it doesn’t matter if the anesthesiologist sees that at the end of the operation there is no restoration of elements of consciousness, attempts to breathe, interruptions in cardiac activity, pressure drops are observed, also for confidence and safety, the anesthesiologist transfers the patient to intensive care .
Do not be alarmed if, after surgery, a person is transferred to intensive care - there the patient is under the strict control of doctors and monitoring systems, and there is very good care there.
Doctors' actions
Resuscitation for a heart attack involves intensive therapy aimed at maintaining basic vital functions and stabilizing the condition. To achieve results, certain prohibitions and recommendations are introduced. This:
- exclusion of physical activity;
- preventing the patient from contacting friends and relatives;
- strict adherence to bed rest;
- 24-hour monitoring by doctors;
- regular examination.
In case of cardiac arrest, cardiopulmonary resuscitation methods are used. You cannot spend time with them, so it is advisable that people nearby provide assistance (indirect cardiac massage and artificial respiration) to the patient. The arriving team of specialists will continue manipulations to preserve vital functions, preventing the death of brain cells. This condition occurs due to the cessation of cardiac function and respiratory function against the background of extensive necrotic lesions. The duration of resuscitation is usually approximately half an hour. The patient's chance of survival increases significantly when assistance is provided in the first five minutes after the attack.
The actions of doctors directly depend on the severity of the lesions, so the diagnosis is carried out:
- Magnetic resonance imaging;
- electrocardiography;
- cardiac catheterization;
- echocardiography;
- lab tests.
Based on its results, it will become clear what to do in intensive care during a heart attack. In most cases, the patient is prescribed intravenous medications to stabilize the heart, prevent the formation of blood clots and dilute them. In severe cases, surgery is recommended:
- stenting;
- coronary artery bypass grafting;
- excision of aneurysm;
- installation of an artificial pacemaker.
Why aren't relatives allowed there?
They are allowed, but very rarely. Basically, doctors are really against relatives coming there.
Firstly, this is a very difficult sight for an unprepared person and we don’t know how he will behave there.
In the department (in one room) there are different patients, of varying severity, without clothes, equipment, sensors, alarming sounds all around. This is not a place where you need to come, sit, communicate. (even though this is how they usually show it in films). The doctor must always be ready - after all, at any moment a situation may arise when it is necessary to urgently resuscitate a patient who is there, no one needs the presence of strangers,
Secondly, there is the risk of infection. Yours will be even higher than the patients there.
Disability
Myocardial infarction often leaves irreversible consequences. They are the reason for assigning a disability group:
| Group | Description |
| I | Even after discharge from the clinic, the patient continues to experience attacks of chest pain (angina). They are difficult to control with medications. There are pronounced symptoms of heart failure. |
| II | Sometimes angina appears after exercise. There are signs of cardiac dysfunction. |
| III | Assigned in case of minor disruptions in cardiac activity that prevent one from returning to their previous place of work. |
The sick leave certificate after a heart attack indicates how many days the person will remain unable to work. It should be given upon discharge from the hospital. Recovery time is affected by complications, age and the presence of other pathologies. Some professions that require special attention will become completely unavailable, since a person may endanger himself and others if the attack recurs. On average, the duration of the incapacity period varies from 3 to 6 months.
Sometimes it is possible to reduce the duration of sick leave after a heart attack to 2 months thanks to the MSEC (medical and social expert commission). They will assess the degree of disability of the patient, focusing on generally accepted standards, and render their verdict.
If you are admitted to intensive care
If you have received approval to go to see your relative who is in serious condition in intensive care, then try to follow some rules; I can’t call them simple, because... I understand that for an ordinary person this is a stressful situation.
- Prepare mentally and tune in to what you will see there (think several times whether it’s really worth going there - are you ready to see your loved one in a completely different form).
- If you are impressionable, you should avoid visiting;
- Do not bring anything from home (medicines, food) - this can be fatal for the patient;
- Communicate quietly, you are not alone in the department;
- Be polite to medical staff and try to listen to their advice.
Drug therapy at home
While at home, a person will have to follow a drug therapy regimen drawn up by a specialist for a long time:
- Statins (Atomax, Crestor) are prescribed to reduce inflammation in blood vessels and the concentration of bad cholesterol in the blood. This effect helps prevent the formation of fatty plaques. They must be taken while following a diet.
- Antiplatelet agents (Aspirin, Aklotin) prevent blood clotting by reducing its viscosity. Taking them significantly reduces the likelihood of blood clots.
- Sartans (Losartan, Valsartan) and ACE inhibitors (Captopril, Quinapril) prevent angiotensin II from exerting its effect, which makes it possible to stabilize blood pressure and heart rate
- Nitrates (“Nitroglycerin”, “Nitrocor”) are used to quickly dilate blood vessels, relieve hypertension and relieve pain. They reduce the load on the heart and improve its nutrition.
- Beta-adrenergic receptor blockers (Anaprilin, Timolol) prevent adrenaline from exerting its effect on the heart muscle. With long-term use, it is possible to reduce the frequency and severity of heartbeats, reduce blood pressure and reduce the myocardial need for oxygen.
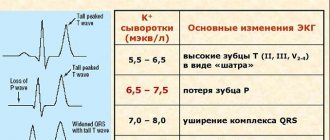
- Tablets rich in magnesium and potassium (Orokomag, Magnestad) are necessary to improve heart regulation, stabilize neuromuscular transmission and maintain normal vascular tone.
Care of patients in intensive care
The intensive care unit has pretty good care (of course, there are cases when it is not always possible to carry out everything in full and the reason is trivial - lack of staff).
- prevention of bedsores is carried out (massage of the back and other protruding places, where bedsores often begin), nurses must turn the patient over at certain intervals;
- postural drainage is done (this is a complex of actions - tapping, stroking, etc. to remove stagnant fluid (mucus, sputum) from the respiratory tract;
- tube feeding for those who cannot swallow on their own;
- Intravenous infusion of solutions, vitamins;
- Patients have their nails cut, their face and body wiped, and in general all necessary hygiene procedures are carried out.
Medical staff in the ward
The table below lists the number of medical personnel required to care for patients in the intensive care unit.
| Job title | Number of workers per ICU with 6 beds |
| Anesthesiologist-resuscitator | 2 people to provide 24-hour patient care |
| Nurse anesthetist | 15 people with a shift work schedule |
| Junior nurse caring for a patient | 5 people |
| Orderly | 5 people |
The number of medical personnel indicated in the table above provides 24-hour care for seriously ill patients in the intensive care unit. If the patient's condition worsens, immediate response measures are taken.
Severity of patients in intensive care
In any case, the definition of a condition is a rather subjective assessment of the doctor, but it is customary to distinguish the following conditions by severity:
- Satisfactory condition - in this case the patient is not transferred to intensive care, and if he was there, he is discharged and observed in a regular ward. The patient's life is not in danger. The disease occurs in a mild form, or the process of recovery begins.
- Moderate severity - in this case, the signs of the disease appear quite pronounced, a decision may be made to transfer to intensive care for more careful monitoring of vital signs. There may be fever, weakness, and pallor, but the person is conscious.
- Severe - the condition is defined as severe if there is depression of consciousness, sometimes the person may become delirious, fever, pale skin, cyanosis, the person cannot care for himself. If you are told that your condition is stable and serious, what does this mean? This means that the patient is not showing signs of improvement.
- Extremely severe - a life-threatening condition, the person is unconscious, pale skin, cold sweat is possible.
That's probably all on this topic, if you still have questions, you can ask me in the form below. Be healthy.
I created this project to tell you in simple language about anesthesia and anesthesia. If you received an answer to your question and the site was useful to you, I will be glad to receive support; it will help further develop the project and compensate for the costs of its maintenance.
“The brain feels bad, we don’t want to remember bad things - a person falls into a coma”
– What is a coma? Why do people fall into this state?
– Why does the patient fall into a coma? It seems to me that there are two points here. Firstly, damage to the brain substance and the second point (I am sure of this) is a defensive reaction. The brain feels bad, the body feels bad, we don’t want to remember the bad, we block it to the point of unconsciousness - the person falls into a coma. Of course, the physiology is much deeper in terms of neural connections and the genesis of coma, but this is a pathological protective reaction to damage to the brain substance.
– How long can you stay in a coma and then come to your senses and return to normal life?
– You can come out of a coma quickly, in stages. People always come out of a coma in stages. However, some stages pass very quickly, and it happens that at one stage the patient withdraws and then the so-called “locked-in” syndrome occurs, when the person has not achieved clear consciousness (a state in which the patient is conscious, but has no facial expressions, movements , speech). Locked-in syndrome is one of the stages of recovery from a coma. How long can you go out like this? There are rare cases described when a person came out of a coma after decades. I have not encountered such cases.
– If a person is stuck at some intermediate stage, what do they do with him?
– There are specialized rehabilitation centers, where they feed such patients, give them water, exercise them, and try to activate them. In general, early activation is exactly what has appeared over the past 15 years, early rehabilitation of the patient is also a breakthrough. And after planned operations. There is such an English term fast track - accelerated rehabilitation. If previously a patient was operated on - and that’s it, he lies at rest... Now we force patients to get back on their feet after preparation, a special program, anesthesia, a major operation.
RIA Novosti/Sergei Pyatakov
Help during a stroke
If a person experiences an increase in upper pressure, nausea, vomiting, dizziness, or problems with coordination of movements and speech, then action is needed. First of all, call the ambulance service. Most often, doctors quickly respond to a call, but when they see a conscious person, they are in no hurry to resuscitate. They prescribe basic medications to the patient that can lower blood pressure. But this is a big mistake. Even if all the symptoms of a stroke have subsided in a person and the attack is more like a sharp headache, it is necessary to insist on hospitalization and examination in a hospital.
Resuscitation is extremely necessary for the victim both during and after a stroke. At the hospital he will undergo a full examination, which will show the results of his health. The patient will be connected to sensors that will monitor breathing and pulse, as well as blood pressure. Acute circulatory disorders can occur against the background of ischemic stroke (more than 80% of cases) or hemorrhagic. In the first situation, the death of nerve cells, necrotic tissue changes occur, and blood stagnation occurs. A hemorrhagic stroke is characterized by rupture of a blood vessel and bleeding into the brain. This is the most severe version of the disease, which most often develops into a coma if measures are not taken in time.