The principle of differential diagnosis
Carrying out differential diagnosis of arterial hypertension allows you to obtain the most accurate data. For this purpose, cardiologists examine heart sounds in strict accordance with the plan. It is divided into two parts. This allows you to eliminate some errors that may occur during the determination of the disease.
- Analysis of clinical symptoms.
- Conducting an assessment of the functional state.
How is hypertension diagnosed? First of all, the clinic examines the patient and collects anamnesis. The data that was obtained is required by cardiologists to clarify the diagnosis and prescribe subsequent drug treatment. Thus, examination is a prerequisite for starting therapeutic actions to normalize the patient’s condition.
Differential diagnosis of primary arterial hypertension
Differential diagnosis of arterial hypertension should be based on a carefully collected medical history and a comprehensive examination of the patient using a set of necessary clinical, laboratory and instrumental methods.
When studying your medical history, you should pay attention to the age at which the initial manifestations of the disease were first discovered. A persistent increase in blood pressure in young children, especially under 10 years of age, is more typical of symptomatic hypertension. It should be borne in mind that puberty can contribute to the manifestation of previously hidden symptomatic hypertension. In this case, a high level of systolic and diastolic pressure, which is slightly reduced under the influence of antihypertensive drugs, has diagnostic value.
In a hospital, a patient with arterial hypertension is systematically measured blood pressure in the upper and lower extremities, basal pressure, blood and urine tests are done, urinary sediment is re-examined according to Kakovsky-Addis, Amburge, Nechiporenko, a bacteriological examination of urine is performed, Zimnitsky's test is performed, and creatinine clearance is determined. , filtration and renal blood flow, sodium and potassium content in blood serum and red blood cells, blood sugar, chest radiography, electro- and mechanocardiography are used. According to indications, intravenous excretory urography, isotope renography are performed, the level of catecholamines and their metabolites (vanillylmandelic acid), 17-OX, plasma renin activity, and aldosterone are determined. The child is examined by a neurologist, ophthalmologist, otolaryngologist, and, if necessary, an endocrinologist or urologist. If there are indications, the patient is sent to a specialized medical institution for angiographic examination and the final stage of differential diagnosis.
Among the diseases that a pediatrician must think about at the bedside of a patient with secondary hypertension, it is necessary to point out chronic nephritis, fibromuscular dysplasia of the renal arteries, pubertal juvenile basophilism syndrome, cystic kidney, hydronephrosis. renal hypoplasia, congenital aneurysm of the renal artery, pheochromocytoma. primary aldosteronism.
Diagnosis of nephrogenic hypertension (the most common form of symptomatic hypertension) is facilitated by the detection of urinary syndrome, as well as extrarenal manifestations of nephropathy: edema, signs of impaired nitrogen excretory function of the kidneys, hypoproteinemia, etc. In children with chronic glomerulonephritis, edematous and urinary syndromes may be mildly expressed. The diagnosis is confirmed by the results of blood tests, kidney function, and fundus. Hypertension is relatively common in secondary chronic pyelonephritis. complicating congenital. kidney anomalies, and therefore X-ray and urological examinations are mandatory in these patients. Persistent hypertension occurs in chronic renal failure. With a stable nature of hypertension with an increase in predominantly diastolic pressure, the presence of a systolic murmur over the renal artery, and high plasma renin activity, renovascular hypertension can be assumed.
Pubertal juvenile basophilism syndrome is diagnosed by such external signs as obesity of varying degrees, a round, full, sometimes moon-shaped face with a bright blush, crimson lips and delicate skin, pink stretch marks on the skin (striae). Girls experience premature puberty, and boys sometimes experience short-term delayed puberty, true gynecomastia. Arterial hypertension is often systolic in nature.
An undulating course of the disease with a paroxysmal increase in blood pressure, accompanied by pallor of the skin, dizziness, sweating, trembling, nervous excitement, shortness of breath, pain in the heart and epigastric region is observed with pheochromocytoma.
To clarify the diagnosis, laboratory and instrumental studies are used. It should be noted that negative data from oxysuprarenography do not exclude pheochromocytoma, which can develop in accumulations of chromaffin tissue located along large vessels.
The most conclusive evidence is the identification of hypercatecholuria in such patients. If the levels of urine catecholamines are normal, it is tested for their metabolite - vanillylmandelic acid, the content of which steadily increases.
Severe muscle weakness, polydipsia, polyuria, hyposthenuria, hypokalemia and increased blood pressure are typical symptoms of primary hyperaldosteronism (Conn syndrome).
Laboratory examination of patients reveals a slight increase in sodium content and a decrease in potassium content in the blood serum. At the same time, there is an increased excretion of potassium and chlorine in the urine. A sharp alkaline reaction of urine is detected, which cannot be eliminated even with the administration of ammonium chloride. Characterized by a significant increase in the content of aldosterone in the urine.
Well-developed muscles of the upper half of the body, absence or weakening of the pulse in the femoral vessels, low or undetectable pressure in the lower extremities, displacement of the borders of the heart to the left, abnormalities of the III-IV ribs in the posterior sections during X-ray examination are characteristic of hypertension with coarctation of the aorta.
Hemodynamic indicators recorded using mechanocardiography also have differential diagnostic significance. In patients with symptomatic hypertension, in contrast to primary hypertension, there is a pronounced increase in pressure (systolic, diastolic, lateral, average dynamic), peripheral resistance, the speed of propagation of the pulse wave through elastic and muscular vessels, a decrease in stroke and minute blood volumes, cardiac index .
A typical clinical picture, skin biopsy results, fundus examination data, and the absence of a clear and rapid effect from the therapy are taken into account.
Women's magazine www.BlackPantera.ru: Dmitry Krivcheni
Analysis of clinical symptoms of arterial hypertension
Diagnosis of arterial hypertension is a necessity. The disease is developing at a catastrophic speed, which is why consultation with a specialist will most likely be disappointing. If a patient experiences primary symptoms of arterial hypertension, he should immediately consult a doctor. Only timely help will allow you to avoid sad consequences.
As a result of analyzing detailed data, the specialist receives a differential diagnosis. He is able to confirm the presence of hypertension. Experts never tire of reminding that there are a large number of types of hypertension, which is why it will not be possible to obtain an accurate diagnosis at the initial stage of the examination. After the examination is completed, the next diagnostic stage begins, which provides the specialist with additional information.
Assessing the functional state of a patient with arterial hypertension
Differential diagnosis of arterial hypertension at the second stage is carried out in order to identify concomitant manifestations of the disease. Routine tests are not carried out at this stage, because all the results were obtained at the previous stage of the examination. Practice shows that experts most often rely on averaged data, which does not always allow an accurate assessment of a person’s condition.
At the second stage of diagnosis, the doctor checks the patient’s functional state. Hypertension is characterized by serious changes that are not superficial symptoms. Most often, treatment for this disease is carried out in a hospital setting. This allows the specialist to observe changes in the patient's condition over time.
Diff. Diagnosis of arterial hypertension allows us to identify what type it belongs to.
How is differential diagnosis performed?
Differential diagnosis of secondary arterial hypertension is carried out in 2 stages:
- Analysis of clinical manifestations, anamnesis and course of the disease, physical examination, mandatory instrumental and laboratory tests.
- Diagnostic measures aimed at assessing the functional state of organs and the changes present in them.
The first stage of differential diagnosis is carried out as follows:
- The anamnesis is studied and the clinical manifestations of the disease are analyzed. In this case, the collection of anamnesis should include information about medications taken by patients that can cause an increase in blood pressure. Diseases the patient has suffered in the past that could cause secondary hypertension (gout, pyelonephritis, tuberculosis, rheumatism, etc.) are also studied.
- A physical examination involves examining the major arteries and measuring pressure in the arms and legs. The abdomen is palpated for enlarged kidneys. A systolic murmur is heard over the renal arteries.
- Laboratory tests include a urine test (urinary sediment is examined according to Amburge, Kakovsky-Addis, Nechiporenko, a Zimnitsky test is taken, a bacteriological examination is carried out), as well as a general and biochemical blood test (the possibility of anemia is studied, signs of inflammation are examined).
Anamnesis collection includes information about medications taken by the patient that can cause an increase in blood pressure.
A physical examination involves measuring blood pressure.
The abdomen is palpated for enlarged kidneys.
The patient must also submit blood and urine tests.
When manifestations corresponding to any secondary form of arterial hypertension are identified, the second stage of diagnosis begins, aimed at identifying the causes and diseases leading to increased blood pressure.
Types of hypertension
For any type of hypertension, examination requires identification of the type of disease. This helps the doctor to take into account some nuances that make it possible to make a diagnosis in a short time. It is worth noting that in this case the diagnosis will be as accurate as possible. This will allow you to prepare a course of therapy using certain medications. There are several types of arterial hypertension (the differential diagnosis is based on this):
- Renal.
- Hemodynamic.
- Focal.
- Endocrine.
The formulation of the diagnosis includes not only hypertension, but also its secondary manifestations. This is due to the fact that they are more dangerous than the disease itself. Related to this is the need for detailed justification. The question that constantly arises is how to identify symptoms. If this is not done in a timely manner, it will not be possible to begin effective therapy in a clinical setting. Accordingly, the consequences will not be long in coming. Statistics show a large number of deaths caused by minor delays in treatment.
To exclude this, differential diagnosis of arterial hypertension is carried out.
Treatment
To select the optimal treatment option, the doctor must study the medical history and identify the disease or pathologies that led to the occurrence of symptomatic arterial hypertension.
For endocrine pathologies, a correction of the medication course is prescribed (if the increase in blood pressure is caused by therapy with corticosteroids or iodothyronines), replacement therapy (for menopause) or drugs that suppress hormone synthesis (for hyperthyroidism, Itsenko-Cushing syndrome). Neoplasia in the adrenal medulla and cortex requires surgical treatment.
Surgical treatment of renovascular hypertension can be of three types: angioplasty of the renal arteries, stenting of the affected vessels and placement of an aortic-renal shunt. In rare cases, surgical revascularization of the kidney is performed.
Therapy for neurogenic and hemodynamic hypertension is aimed at eliminating and relieving symptoms of brain and vascular damage. For strokes, intensive antihypertensive treatment is prescribed only after the patient's condition has stabilized.
Symptomatic treatment is recommended in almost all cases of secondary hypertension, in most of them as a pre- and postoperative course or in addition to drug therapy for the underlying disease. A persistent increase in lower pressure is considered a more dangerous factor requiring complex treatment.
Before prescribing a course of certain pharmaceuticals, it is important to consider contraindications and the patient’s individual intolerance to individual components. Ideally, the selection of competent treatment should be the result of joint efforts of competent specialists in the field of neurology, endocrinology and cardiology.
Renal manifestations
Hypertension can be complemented by renal manifestations, which significantly affect the patient’s body. Quite often in such cases, renal failure develops, which is why a prerequisite is a timely assessment of the patient’s condition and initiation of treatment. If there is insufficient blood flow, then you should immediately think about the possible consequences. After all, it will no longer be possible to eliminate them.
Secondary manifestations of a renal nature develop over a period of time. There are examples when, due to a chronic lack of oxygen, internal organs begin to malfunction. This involves a thorough check of each patient. Quite often, against the background of the underlying disease, some symptoms go unnoticed by the patient himself, but the specialist is able to take into account all the subtleties, even minor ones.
What else could be the differential diagnosis of arterial hypertension?
Endocrine
As we have already noted, the formulation of any type of arterial hypertension involves indicating secondary manifestations. The effect on the endocrine system is quite serious. It provides protection against infections and regulates the activity of the body as a whole, so you should not allow its functionality to be impaired.
However, finding endocrine manifestations is quite difficult. This will require careful examination. It can complement the description of the patient’s condition, which allows one to cope with the process of functional restoration. In such cases, drug therapy is pointless. If the disease is advanced, doctors will not even try to eliminate it; all treatment will be purely symptomatic.
Differential diagnosis of hypertension can determine the hemodynamic signs of pathology.
Differential diagnosis of hypertension table
Published on: 12/22/2018 adminComment: 0
Differential diagnosis of hypertension is based on a detailed medical history of the patient and a comprehensive examination using a complex of all instrumental and laboratory methods necessary for this. Its goal is to identify secondary forms of arterial hypertension and establish their etiology.
Differential diagnosis of hypertension reveals secondary forms of arterial hypertension and establishes their etiology.
How is differential diagnosis performed?
Differential diagnosis of secondary arterial hypertension is carried out in 2 stages:
- Analysis of clinical manifestations, anamnesis and course of the disease, physical examination, mandatory instrumental and laboratory tests.
- Diagnostic measures aimed at assessing the functional state of organs and the changes present in them.
This stepwise method (from simple to complex measures) allows you to exclude unnecessary examinations and make a differential diagnosis between hypertension itself and secondary forms of arterial hypertension.
The first stage of differential diagnosis is carried out as follows:
- The anamnesis is studied and the clinical manifestations of the disease are analyzed. In this case, the collection of anamnesis should include information about medications taken by patients that can cause an increase in blood pressure. Diseases the patient has suffered in the past that could cause secondary hypertension (gout, pyelonephritis, tuberculosis, rheumatism, etc.) are also studied.
- A physical examination involves examining the major arteries and measuring pressure in the arms and legs. The abdomen is palpated for enlarged kidneys. A systolic murmur is heard over the renal arteries.
- Laboratory tests include a urine test (urinary sediment is examined according to Amburge, Kakovsky-Addis, Nechiporenko, a Zimnitsky test is taken, a bacteriological examination is carried out), as well as a general and biochemical blood test (the possibility of anemia is studied, signs of inflammation are examined).
When manifestations corresponding to any secondary form of arterial hypertension are identified, the second stage of diagnosis begins, aimed at identifying the causes and diseases leading to increased blood pressure.
Diagnosis of secondary hypertension
It is quite difficult to identify secondary hypertension - only in 10%-25% of all cases is secondary hypertension diagnosed.
Secondary arterial hypertension is classified depending on the influence of certain organs on the process of increasing blood pressure:
- Endocrine;
- Renal (renovascular, parenchymal);
- Hemodynamic (mechanical, cardiovascular);
- Centrogenic (brain lesions);
- Other.
Differential diagnosis of hypertension is given in the table listing possible diseases leading to secondary hypertension.
| Classification of hypertension | Diagnostics | Additional diagnostic methods |
| Renal arterial hypertension: 1) Chronic diffuse glomerulonephritis2) Chronic pyelonephritis3) Polycystic kidney disease4) Vasorenal hypertension5) Nephroptosis | The history often contains indications of kidney pathology. There are changes in the urine (proteinuria, hematuria). Blood pressure is never high, most often stable, crises are rare. The history contains indications of cystitis, prostate adenoma, and an increase in blood pressure. In the urine - increased ESR, bacteriuria, pyuria. Appearance: swelling of the eyelids, puffiness of the face. A congenital anomaly, in which the size of the kidneys is often increased. Frequent thirst and polyuria are characteristic. Characteristic signs: high, rapidly progressing blood pressure, vascular noise in the region of the renal artery. It often develops at a young age, hypertension occurs with severe headaches, crises, and pronounced autonomic disorders. | Nechiporenko's tests, Zimnitsky's tests, excretory urography. Palpation, excretory urography. Radioisotope renography, scanning, excretory urography, aortography. Excretory urography, aortography. |
| Endocrine arterial hypertension 1) Ishchenko-Cushing's disease 2) Pheochromocytoma 3) Conn's syndrome | Moon-shaped face with a purple coloration, in women - the appearance of facial hair, increased acne formation, atrophy of the mammary glands, limbs, and the appearance of fatty deposits. A sudden instant increase in blood pressure (up to 300 mm Hg), a feeling of fear, tachycardia, pale skin. In the urine - leukocytosis, hyperglycemia, increased ESR. Muscle weakness, paroxysmal paralysis of the legs, polyuria, nocturia. In the blood - hypernatremia, hypokalemia, alkalosis. | Diagnosis is helped by identifying the concentrations of norepinephrine and adrenaline in the urine, and examining the adrenal glands using echography. ECG, blood test for sodium and potassium concentration. |
| Hemodynamic arterial hypertension 1) Coarctation of the aorta 2) Takayasu syndrome (pulseless disease) | Diagnosed on the basis of two main syndromes: syndrome of increased blood supply to the upper body (plethora of the neck and face, increased blood pressure in both arms, aortic dilatation, systolic murmur in the heart), syndrome of reduced blood supply to the lower body (convulsions, muscle weakness, low or no undetectable blood pressure, muscle hypertrophy of the lower extremities). Prolonged low-grade fever (reminiscent of allergic reactions or a feverish state), ischemia of the limbs and cerebral vessels (fainting, headaches, weakness in the arms, fainting). Low blood pressure in the arms; blood pressure is always higher in the legs. | The main method is aortography. Aortography, urine test for increased ESR. Find out your level of risk of heart attack or stroke Take a free online test from experienced cardiologists Test time no more than 2 minutes 7 simple questions 94% test accuracy 10 thousand successful tests |
| Centrogenic arterial hypertension: tumors, encephalitis, ischemia, hemorrhage, skull trauma, etc. | Constantly elevated blood pressure, dizziness, severe headaches, tachycardia, vasomotor and pilomotor reactions. | ECG |
Other arterial hypertension includes symptomatic hypertension in patients with carcinoid syndrome, polycythemia, increased blood pressure due to thallium or lead poisoning, or with an overdose of catecholamines, prednisolone, ephedrine. This also includes arterial hypertension that occurs in women when taking hormonal contraceptives and with late toxicosis in pregnant women.
Differential diagnosis of hypertension
Lesson 5. Diagnosis of hypertension
Differential diagnosis of hypertension should be carried out on the basis of the main clinical manifestations of the diseases given above, but when making a diagnosis, one should not forget that the listed symptoms may be mild (and some may be completely absent), because All cases of disease are purely individual.
Source: ProGipertoniyu.ru
Source: https://feedjc.org/differentnyj-diagnoz-gipertonicheskoj-bolezni-tablica/
Hemodynamic
This type of manifestation is based on impaired blood circulation. An example of such a manifestation is a loss of blood pressure stability and a temporary stop of the pulse. Delays in treatment in such cases have a very detrimental effect - the functioning of the upper body is disrupted, and fainting occurs.
This type of manifestation is fraught with great danger. Before diagnosing this type of hypertension, specialists will try to collect additional information through fairly lengthy clinical studies. Otherwise, treatment may be ineffective or even erroneous. As a result, final confirmation of the diagnosis will be obtained only at the last, irreversible stage of the course of hypertension. Differential diagnosis must be timely.
Focal
Such manifestations are most often noticeable during a visual examination of the patient. In a hospital setting, during daily rounds, the attending physician constantly assesses the patient’s condition. Damage in this case should be minimal, this will indicate the absence of other violations.
Most often, focal manifestations are expressed by the appearance of tumors. As a result, a person begins to experience constant headaches, he is tormented by endless tachycardia and high blood pressure. In such cases, delay in treatment becomes critical.
How does a doctor identify symptomatic arterial hypertension? Differential diagnosis helps with this. Modern medicine has a variety of techniques that allow you to quickly clarify a person’s condition. However, proven methods that provide accurate data also continue to be used. These include:
- Aortography.
- Auscultation of the heart.
- Radioisotope renography.
- Electrocardiogram.
Blood and urine tests also remain necessary. They have to be given to patients quite often. Doctors try to prescribe unnecessary tests in order to gradually identify all existing disorders. In the absence of such action, effective treatment remains unavailable.
88. Differential diagnosis of arterial hypertension. Treatment. Prevention
The main objectives of clinical and paraclinical examination of a patient with arterial hypertension are: 1) identification of secondary (symptomatic) arterial hypertension, which is potentially treatable;
2) clarification of the nature and severity of individual manifestations and complications of the disease that are important when prescribing treatment; 3) identification of risk factors for diseases associated with atherosclerosis. Complaints. Most patients do not complain and an increase in blood pressure is detected only when it is measured. Complaints may be associated with: a) increased blood pressure; b) vascular damage due to arterial hypertension; c) the underlying disease in cases of symptomatic arterial hypertension.
Symptoms of increased blood pressure are nonspecific. The most common complaint of headache occurs only with a sharp increase in blood pressure in cases of hypertensive encephalopathy and malignant arterial hypertension. An increase in blood pressure may be accompanied by dizziness, nosebleeds and weakness. However, these complaints are quite common even with normal blood pressure levels.
Symptoms of vascular damage caused by arterial hypertension include blurred vision, periodic weakness, dizziness due to transient ischemia of the central nervous system, hematuria
inicturia. Angina pectoris may occur due to the accelerated development of atherosclerosis, sharp chest pain during aortic dissection, shortness of breath and other signs of acute and chronic heart failure. Myocardial infarction and stroke are also possible.
Complaints associated with the underlying disease in cases of symptomatic arterial hypertension include severe muscle weakness, polydipsia and polyuria in primary hyperaldosteronism, arthralgia, weight loss and fever in periarteritis nodosa. Distinctive features of the anamnesis and examination data for arterial hypertension of various origins are given in Table. 51.
Features of the course of arterial hypertension. In favor of essential arterial hypertension
a family history and onset of the disease at the age of 35-45 years are typical, while symptomatic arterial hypertension is more characterized by an increase in blood pressure at the age of 30 and older 55
years.
In such cases, it is imperative to search for a possible cause of arterial hypertension! In women, an increase in blood pressure detected for the first time during pregnancy, even with subsequent normalization for a more or less long time, allows us to suspect the renal genesis of arterial hypertension.
Essential arterial hypertension is characterized by a gradual increase in blood pressure, while with symptomatic arterial hypertension, blood pressure increases in a relatively short time and is immediately established at more or less high numbers.
Hypertensive crises are characteristic of essential arterial hypertension, pheochromocytoma, borderline arterial hypertension and menopause, diencephalic syndrome.
In pheochromocytoma, unlike other diseases, crises are often associated with physical activity, straining, and heavy food, while in patients with essential arterial hypertension they are provoked by psycho-emotional stress, meteorological factors, and salt abuse.
When pheochromocytomecrisis lasts no more than 1 hour, usually 10-15 minutes, and AJ
often spontaneously normalizes. In contrast, with essential arterial hypertension, they continue for hours and do not stop on their own. During the intercrisis period, blood pressure is always within the normal range for diencephalic syndrome and can be normal in case of pheochromocytoma, whereas in patients with essential arterial hypertension it is often elevated. Hypertensive crises can be observed with some brain tumors and carcinoids. Other types of symptomatic arterial hypertension are characterized by a stable increase in blood pressure and the absence of crises.
Urinary system. The presence of urolithiasis, prostate adenoma and a history of repeated urinary tract infections, periodic dysuric phenomena and chills allows one to suspect chronic pyelonephritis, which, however, may also have
asymptomatic. Possible renal genesis of arterial hypertension is indicated by facial edema, gross hematuria and changes in urine tests that preceded an increase in blood pressure. Polyuria, nocturia and polydipsia are characteristic of both kidney disease and endocrine pathology. Suffered abdominal trauma in the flank area, back injury may be accompanied by damage to the kidney.
General complaints. Muscle weakness may indicate hyperaldosteronism, thyrotoxicosis, and less commonly, Itsenko-Cushing syndrome (disease).
The latter is characterized by an increase in body weight, while with pheochromocytoma, thyrotoxicosis, systemic vasculitis and diffuse connective tissue diseases, weight loss is noted.
Loss of body weight may be accompanied by an increase in body temperature.
Long-term use of medications, in particular glucocorticosteroids, oral estrogen-containing contraceptives, sympathomimetic drugs in the form of inhalations or drops, can cause iatrogenic arterial hypertension.
To assess the presence of vascular complications in arterial hypertension and concomitant atherosclerosis, the severity of angina pectoris, cerebral and peripheral vascular insufficiency, as well as chronic heart failure are clarified. The presence and severity of risk factors for diseases associated with atherosclerosis (smoking, diabetes mellitus, etc.) is also important for treatment and secondary prevention.
An objective examination begins with an assessment of the patient’s appearance. Cushing's disease (syndrome) is characterized by a moon-shaped face and body obesity, signs of acromegaly. Disproportionate development of the muscles of the shoulder girdle compared to the pelvic girdle allows one to suspect coarctation of the aorta.
When examining the skin, pay attention to the presence of striaae rubrae, acne, hypertrichosis, characteristic of hypercortisolism. With the development of heart failure, acrocyanosis appears, and in advanced cases, edema of the lower extremities.
Puffiness of the face and swelling of the eyelids are characteristic of renal
edema, and an enlarged thyroid gland and eye symptoms - thyrotoxicosis.
An important part of the clinical examination is the determination of pulsation of the arteries of the upper and lower extremities. When palpating the radial arteries, pulsus differens, characteristic of atherosclerosis and Takayasu's disease, can be detected.
The weakening or disappearance of pulsation of both femoral arteries is an important diagnostic sign of coarctation of the aorta, and one or both posterior tibial or dorsal arteries of the foot is a sign of their atherosclerotic lesion. Visible pulsation of the carotid arteries (carotid dancing) is characteristic of aortic valve insufficiency and patent ductus arteriosus.
In patients with essential arterial hypertension in the absence of heart failure, there is a tendency to bradycardia, while in patients with pheochromocytoma and thyrotoxicosis, persistent tachycardia occurs.
Blood pressure measurements are carried out on both upper extremities, three times on one side, and in all cases of arterial hypertension development at a young age (up to 30 years) - also on the lower extremities with a cuff placed on the lower third of the thigh.
It is important to carefully observe the correct technique for measuring blood pressure! Normally, systolic blood pressure in the lower extremities is approximately 10 mm Hg. Art. is higher than in the upper ones, and significantly reduced with coarctation of the aorta.
Asymmetry of blood pressure in the upper extremities is characteristic of atherosclerosis and Takayasui disease and, in the presence of other signs, may indicate a possible vasorenal genesis of arterial hypertension.
Comparison of the results of measuring blood pressure in the supine and standing positions has an important differential diagnostic value.
Essential arterial hypertension is more characterized by an increase in diastolic blood pressure during the transition to a vertical position, while symptomatic arterial hypertension (especially with pheochromocytoma), in the absence of antihypertensive therapy, is characterized by its decrease (so-called orthostatic arterial hypotension). An isolated increase in systolic blood pressure indicates possible atherosclerotic hypertension.
residential, thyrotoxicosis, aortic valve insufficiency. It is also observed with patent ductus arteriosus and complete atrioventricular block. A predominant increase in diastolic blood pressure with little change in systolic blood pressure requires, first of all, the exclusion of renal arterial hypertension.
The detection of vascular noise over the arteries during houseculturation indicates their significant narrowing, the cause of which in most cases is atherosclerosis and, rarely, aortoarteritis.
These murmurs are characterized by a diastolic component, which, however, cannot always be heard.
In the peri-umbilical region, such a murmur is heard in 50% of patients with renovascular arterial hypertension, which greatly facilitates its diagnosis.
In a clinical examination of the heart, attention is paid to the presence of murmur-aortic insufficiency, patent ductus arteriosus and coarctation of the aorta, IV and III sounds, dilatation of the cavities. Palpation of the abdomen makes it possible to detect enlarged kidneys due to polycysts, as well as an aneurysm of the abdominal aorta.
As a result of the examination, the presence and severity of congestive heart failure and retinopathy are assessed.
Additional examination. The diagnosis of essential arterial hypertension is preliminary upon the initial detection of elevated blood pressure in patients aged 35-45 years, especially in women with a family history. In 9 out of 10 cases this assumption turns out to be correct.
However, although the likelihood of symptomatic arterial hypertension is quite small, its recognition can save the patient from lifelong use of antihypertensive drugs. The exclusion of secondary arterial hypertension is mandatory when identifying elevated blood pressure in younger or, conversely, older people.
For these purposes, as well as to assess the degree of target organ damage, all patients with resistant arterial hypertension undergo a basic examination according to the following minimum program:
blood - general analysis, determination of glucose (fasting), creatinine, urea, uric acid, electrolytes (potassium, sodium), lipids (total cholesterol, triglycerides) on an empty stomach;
urine - general analysis (repeatedly), according to Nechiporenko, culture (if bacteria are detected in the general analysis);
ECG—chest radiography, echocardiography.
A complete blood test can reveal anemia characteristic of renoparenchymal diseases, polycythemia and signs of inflammation. Diabetes mellitus accelerates the development of arteriosclerosis and may be complicated by diabetic nephropathy. Hyperglycemia is also characteristic of Itsenko-Cushing disease (syndrome) and pheochromocytoma.
The level of creatinine and, to a lesser extent, urea allows you to assess the state of nitrogen excretion function of the kidneys. An increase in uric acid levels, in addition to gout and gouty nephropathy with symptomatic arterial hypertension, is often found in other types of renal hypertension.
The initial level of uric acid, like blood glucose, can also serve as a reference point for monitoring possible side effects of saluretics. Hypokalemia occurs with increased secretion of mineralocorticoids, but can also be a consequence of taking diuretics. Determination of sodium content in blood plasma can help distinguish primary from secondary hyperaldosteronism.
Elevated blood lipid levels are an important risk factor for atherosclerosis and may be exacerbated by treatment with certain antihypertensive drugs (particularly P-blockers).
The differential diagnostic significance of changes in urine tests characteristic of the most common causes of arterial hypertension is summarized in Table. 52.
The submitted ECG and EchoCG evaluate left ventricular hypertrophy. Left ventricular hypertrophy is a factor with an unfavorable prognostic value, regardless of the genesis of arterial hypertension. X-ray of the chest organs reveals changes in the aorta characteristic of atherosclerosis, as well as dilatation of the left ventricle, occasionally pathognomonic for coarctosis.
tiaorta rib patterns. Echocardiography is also important for assessing left ventricular function.
Special research methods are used to diagnose symptomatic arterial hypertension in cases where the results of clinical and basic laboratory and instrumental examinations give reason to suspect secondary arterial hypertension or when drug therapy is ineffective.
Indications for a special examination to clarify the cause of arterial hypertension are: 1) the presence of clinical signs of the disease that may serve
cause of arterial hypertension; 2) changes in the content of creatinine and potassium in the blood plasma; 3) changes in urine tests; 4) arterial hypertension in persons under 30 years of age; 5) malignant arterial hypertension; 6) arterial hypertension, refractory to drug therapy.
The nature of the additional examination is determined by the most likely cause of arterial hypertension. Specific diagnostic methods and confirmation of diagnosis for the most common types of symptomatic arterial hypertension are given in table. 53.
Determination of renin activity in blood plasma in all patients with arterial hypertension in order to assess the renin profile is currently not carried out. The accumulated clinical experience has not confirmed its any significant prognostic and therapeutic value, with the exception of cases of suspected renovascular arterial hypertension or hypersecretion of mineral corticoids.
Source: //studfile.net/preview/5165938/page:23/
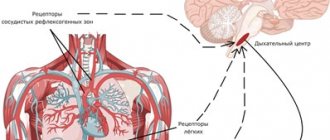
Radioisotope renography
A fairly complex technique used in some cases of differential diagnosis of arterial hypertension syndrome is radioisotope renography. It allows specialists to study the blood circulation process in detail in order to obtain the necessary information reflecting the lack of oxygen in some organs. The ideal option for obtaining such data is radioactive isotopes, which are subject to temporary introduction into the human body.
Radioisotope renography is the latest research. It is especially important for manifestations of arterial hypertension that affect the kidneys. Other methods do not provide accurate confirmation of the presence of functional disorders of this organ.
Differential diagnosis of arterial hypertension in children is mandatory.
Aortography
A modern X-ray examination is aortography. It is required for a detailed study of existing circulatory disorders. In the event that, simultaneously with the development of the disease, a violation of vascular capacity occurs, additional studies should be taken as seriously as possible.
Aortography provides the opportunity to obtain a detailed picture of the condition of the arteries. The results obtained using aortography make it possible to determine what additional drug therapy should be prescribed in order to restore normal blood circulation. It happens that the absence of such a study does not allow us to draw correct conclusions, but most often specialists use it to eliminate damage.
Electrocardiogram
It is important to conduct an electrocardiogram in the differential diagnosis of essential arterial hypertension. This type of research is basic. The patient should undergo it regularly. An electrocardiogram allows you to monitor changes in the patient’s condition, and this is especially important when being registered with a specialist such as a cardiologist. The data obtained from the electrocardiogram is ideal for being able to detect some very serious disorders.
The electrocardiogram quite clearly reflects the existing focal manifestations. Most often, this study is prescribed at the slightest suspicion. Therefore, you should listen to your doctor's recommendation and undergo this type of test as soon as possible. After all, the more complete the picture of the disease and the list of confirmed symptoms, the sooner it will be possible to receive qualified help, which involves effective drug therapy.
Differential diagnosis
EG must be differentiated from secondary (symptomatic) hypertension, which is understood as such forms of increased blood pressure that are causally caused by diseases of the organs and systems involved in the regulation of blood pressure. The main groups of secondary hypertension:
- Renal (nephrogenic) – 18% or 70-80% of symptomatic hypertension;
- Endocrine;
- Hemodynamic, caused by lesions of the heart, aorta, and its large branches;
- Centrogenic, caused by organic lesions of the central nervous system;
- Exogenous, due to medication (GCS, hormonal contraceptives), nutritional (tyramine).
A special form of hypertension is an increase in blood pressure caused by an increase in blood viscosity, for example, with polycythemia.
Classification according to Arabidze (1992)
- Renal arterial hypertension
Congenital anomalies of the kidneys and blood vessels (hypoplasia, dystopia, hydronephrosis, polycystic disease, horseshoe kidney, pathological mobility, atresia and hypoplasia of the renal artery, aneurysms.
- Acquired kidney diseases (diffuse glomerulonephritis, amyloidosis, Kimelstiel-Wilson syndrome, systemic vasculitis, tumors).
- Acquired lesions of the main renal artery (atherosclerosis, calcification, thrombosis, embolism, fibromuscular dysplasia, Takayasu's disease, aneurysm, endarteritis, hemangiomas, vascular compression, stenosis and thrombosis of the renal vein.
- Coarctation of the aorta
- Pheochromocytoma
- Encephalitis
- Damage to the kidneys and adrenal glands
In 13-30% of cases, symptomatic hypertension has a malignant course, whereas with EG such a course is observed only in 0.19%.
Renal (nephrogenic) hypertension
- Caused by diseases of the kidney parenchyma;
- Caused by impaired urine outflow;
- Vasorenal, caused by deterioration of renal circulation.
Chronic glomerulonephritis
The symptoms of hypertension are no different from those of other hypertension. Varies widely - from asymptomatic or low-symptomatic hypertension to malignant.
There is no strict parallelism between the nature of kidney damage (including morphological features) and the severity of hypertension, although the development of nephroangiosclerosis is often accompanied by an increase in hypertension.
Any kidney disease can be accompanied by hypertension of any severity.
In the characteristics of hypertension itself in kidney diseases, there are no signs that would allow us to associate it with a kidney disease or predict its further course, for example, the transition to a malignant form.
However, there are very relative and conditional distinctive features of hypertension in CGN and in kidney diseases in general:
- Young age of patients;
- Absence of “vegetative neurosis”;
- The course of the disease without crises;
- Dependence of exacerbations on sore throats and ARVI, and not on psycho-emotional factors;
- Patients with renal hypertension do not feel their high blood pressure, unlike patients with EG, in whom even a slight increase can be accompanied by an abundance of symptoms;
- Edema occurs in 1/3 of patients with CGN, but can also occur with EG, especially in the volume-sodium-dependent variant.
The diagnostic criteria for the hypertensive form of GN are:
- AG;
- Young age;
- Changes in urine (proteinuria, erythrocyturia, cylindruria);
- History of AGN;
Laboratory and instrumental research data are of decisive importance in diagnosis:
- Presence of urinary syndrome;
- During an exacerbation - acceleration of ESR, appearance of acute phase proteins, often anemia;
- In the presence of chronic renal failure - a decrease in glomerular filtration, an increase in residual nitrogen and urea, creatinine;
- In the fundus there is hypertensive retinopathy, usually more pronounced than in EG; transudates in the fundus can be observed even with moderate hypertension;
- Needle biopsy of the kidneys.
Source: https://studfile.net/preview/1469272/page:14/
Auscultation of the heart
This examination is initial. When you first visit a cardiologist, he always conducts a heart rhythm study. The data obtained allows the specialist to prescribe the necessary examinations and tests.
Rhythm disturbances and slight murmurs are very important symptoms to be taken into account by an experienced cardiologist. Taking them into account, it seems possible to draw initial conclusions. However, drug therapy is not prescribed at this stage until more detailed information is obtained.