Treatment of biliary hypertension
It is impossible to single out a single tactic for the treatment of biliary hypertension.
The principle of treatment will depend on the underlying cause of the syndrome. In some cases, conservative therapy is sufficient, and sometimes the disease requires surgical intervention. If the syndrome is the result of helminthiasis, the patient is prescribed antiparasitic drugs or surgery, during which the surgeon excises part of the affected organ. In other cases, treatment is carried out as follows:
- For gallstone disease, an operation is performed in which doctors simply remove the gallbladder. Shock wave lithotripsy is sometimes used (if there is only one stone).
- If polyps appear in the gallbladder, laparoscopic surgery or cholecystectomy is prescribed. If the polyp is small in size, the patient simply needs to undergo regular preventive examinations so that doctors can assess the dynamics of the disease.
- For malignant or benign neoplasms, surgery/chemotherapy/radiotherapy is indicated.
- If the cause is calculous cholecystitis, then surgical intervention is performed. Before surgical procedures, the patient is prescribed antibiotics, antispasmodics, and antiemetics.
- Obstructive jaundice is treated with medication. The patient is prescribed a diet, B vitamins, choleretic agents, intravenous glucose, antibiotics, and enterosorbents. If drug therapy is ineffective, surgery is performed.
In case of biliary hypertension, regardless of the etiology, the patient undergoes decompression of the biliary tract. It is also recommended to use droppers, which will help restore the water-salt balance.
Biliary hypertension is an extremely dangerous pathology. Against this background, very dangerous consequences can develop - ascites, liver necrosis. A fatal outcome is also possible. That is why the syndrome must be treated promptly and competently.
Causes and symptoms
Biliary hypertension is a pathology caused by problems with the gallbladder or pancreas. Sometimes it can also be caused by the liver. Most often, the prerequisites for this disease are a sedentary lifestyle, excess weight, and poor nutrition. An excess of fatty and fermented milk products in the diet, as well as fried foods, leads to serious disturbances in the functioning of the pancreas. Unfortunately, this can lead to partial or complete removal of the organ.
This symptom occurs against the background:
- tumors in the liver, gall bladder or pancreas;
- polyposis;
- formation of gallstones.
Neoplasms can be either benign or malignant. According to statistics, hypertension most often develops against the background of malignant tumors, which are growing rapidly. As the tumor grows, it puts pressure on the surrounding tissues, vessels, and organs, and prevents the normal outflow of bile. Most often, biliary hypertension is provoked by cancer of the head of the pancreas, but an ordinary cyst can also be the cause.
The cause may also be the presence of a gallstone, which simply clogs the bile duct. The same effect is also achieved by polyps growing into the lumen of the duct.
Symptoms may vary. It all depends on which organ was damaged. Most often, the disease has the following main manifestations:
- Weakness, general malaise.
- The appearance of a jaundiced color of the skin. This is especially noticeable on the face; the whites of the eyes turn yellow.
- Nausea, vomiting, belching. Such unpleasant symptoms most often occur immediately after eating.
- Pain in the abdominal area. The painful sensation can be of varying intensity and character. It is localized in the area of the affected organ, but can be felt in different parts of the abdominal cavity.
- Flatulence, bowel dysfunction (usually diarrhea, but constipation may also occur).
- Unpleasant sensations, pain, heaviness in the right hypochondrium.
Unfortunately, the main symptoms begin to appear already in the later stages of the primary disease. If biliary hypertension is provoked by a tumor, then at the initial stage the tumor will not make itself felt in any way. Symptoms appear already in the second and third stages of cancer.
As soon as such manifestations appear, you should immediately go to the hospital before the problem is too advanced.
Often people simply ignore the “first signs”, considering them unimportant. In fact, neglecting dyspeptic disorders (regular nausea, belching, flatulence), which occur in combination with general weakness and ailments, is extremely dangerous - in any case, it is necessary to consult a doctor as quickly as possible to identify the causes of the disease.
The most negative prognosis is if, in combination with all these manifestations, the patient also experiences sudden weight loss for no reason (he is not on a strict diet at this time). This is a clear sign of the presence of a malignant neoplasm. This is also indicated by a rise in temperature. Most often, the increase is not critical (up to 37.3-37.5 degrees), but is permanent (lasts more than a week without additional symptoms of a cold or other severe infection).
Signs
HD is distinguished by the degree of spread of hypertension, by the localization of liver blood flow disturbances, and by the stage of development of the disease. The basis of the circulatory system of the biliary apparatus is the portal vein of the liver, which receives venous blood from all organs of the gastrointestinal tract. Depending on the number of affected vessels of the portal system, pancreatic hypertension occurs:
- portal hypertension with damage to the portal vein;
- segmental – with damage to the splenic vein;
- total – when the entire vascular system is affected.
A large number of blood vessels exit into the portal vein. High blood pressure changes blood circulation, which causes dilation of the intrahepatic ducts and congestion at the junction of veins and arteries. Based on the location of the blockage of normal blood circulation, HD is divided into:
- prehepatic;
- intrahepatic;
- posthepatic;
- mixed.
HD occurs in stages. The initial stage lasts a long time without obvious signs. With later manifestations of the disease, HD can be diagnosed. The stages are distinguished by the severity of the dysfunction of the pancreas:
- initial – functional impairment;
- moderate – compensation for operational failures;
- severe – accumulation of bile in the abdominal cavity, swelling;
- complicated – stomach or intestinal bleeding, liver failure.
Diagnostics
When developing HD, the choice of diagnostic methods is quite important. In addition to standard urine and blood tests, instrumental studies will be required that are aimed at confirming the fact of biliary hypertension and establishing the cause of the development of the syndrome.
Ultrasound of the abdominal cavity and retroperitoneal space
Ultrasound diagnostics is one of the modern and quite informative research methods. With its help, you can examine and identify the structural features of the liver, spleen, gallbladder and its ducts. In the retroperitoneal space, the pancreas and its ducts, which are physiologically connected with the hepatobiliary system, are examined directly.
When performing an ultrasound, you can detect changes in the tissues of various organs, identify developmental abnormalities, determine the presence of stones in the ducts and other neoplasms that contribute to the course of the disease.
CT scan
Using this method, accurate images of all abdominal organs can be obtained. If there are volumetric formations, it is possible to study them in detail, determine their size and structure. Computed tomography also helps to identify tumor metastases and determine the extent of their invasion into other organs.
X-ray with contrast
Cholangiography is often used to detect biliary hypertension. This is a method of radiographic examination, which is carried out by introducing radiopaque substances into the body. Thanks to this, all bile ducts are clearly visible on photographs of the abdominal cavity, which makes it possible to determine the degree of their narrowing and patency.
Cholangiography
Biopsy
This is one of the invasive research methods, which is used in extremely severe cases. The need for such diagnostics most often arises when a malignant neoplasm is suspected.
The mini-surgery is performed under ultrasound guidance. Several cubes of tissue are collected from the pathological focus, which are subsequently sent for histological examination. Based on the results of the analyses, the nature of the emerging formation is determined.
Laparoscopy (laparotomy)
Also, in advanced cases, when standard diagnostic measures do not allow establishing the cause of biliary hypertension, surgery is required. With laparoscopy, it is possible not only to examine damaged organs, but also to perform surgical procedures aimed at improving the condition of the ducts.
Treatment
There are a number of therapeutic methods that can be used to relieve high pressure in the bile ducts. In some cases, biliary hypertension is provoked by gallstone disease. To relieve various diseases, conservative and surgical methods are used. Often, surgical intervention is used to get rid of unpleasant symptoms and eliminate relapses of pathology. A cholecystectomy is usually performed. The indication for surgery is worsening negative symptoms. During the operation, a complete resection of the gallbladder, including the formed stones, occurs. Both laparotomic and laparoscopic methods are used. The method of performing the operation is selected by the attending physician based on the characteristics of the patient’s body and the course of the underlying disease.
Biliary hypertension often develops in the presence of a growing tumor in the pancreas. In this case, surgery is also used, and the affected area is removed as quickly as possible. Before performing an operation, it is necessary to establish the features of the neoplasm, identify the exact parameters of the tumor, and determine the stage of the pathological process. If malignant neoplasms are detected in the pancreas area, not only surgery is used, but also chemotherapy and radiotherapy.
When bile duct polyps grow to gigantic sizes, surgical intervention is performed, but the operation is much simpler than in the cases listed above. Instrumental diagnostics are first used to identify the exact location of the polypous formation. Next, laparoscopic surgery is used. A complete resection of the polyp occurs, which is subsequently sent for laboratory testing. To diagnose the cause of the disease, it is necessary to determine the nature of the polyp.
Biliary hypertension is a dangerous pathology that indicates the development of other diseases. In most cases, surgical intervention is required to eliminate the causes of this disorder. Treatment tactics are being developed to restore the body’s condition during the postoperative period. To eliminate the disease and eliminate the likelihood of dangerous complications, it is necessary to seek medical help when the first symptoms of biliary hypertension are detected.
What is biliary hypertension
Biliary hypertension - what is it, causes of development
Liver cells produce bile, which contains bilirubin, cholesterol, some metabolic products and bile acids. Bile, which takes part in the digestive process, is excreted from the liver into the lumen of the duodenum through a system of hollow structures, which includes the intrahepatic ducts, gallbladder, cystic duct and common duct. These structures are called the hepatobiliary system.
An increase in bile pressure on the walls of the hollow structures of the hepatobiliary system is called “biliary hypertension.” In most cases, it develops as a result of outflow disturbances in various pathological processes. These include:
- Tumors (malignant or benign neoplasms) in one of the bile ducts that obstruct the outflow. Biliary hypertension can also be caused by compression of one of the ducts by a tumor developing in nearby organs (often caused by cancer of the head of the pancreas).
- Calculous cholecystitis and cholelithiasis are metabolic pathologies characterized by the formation of insoluble calculi (stones) with their localization in various parts of the hepatobiliary system and the development of obstructive jaundice (jaundiced discoloration of the skin due to an increase in the concentration of bilirubin in the blood).
- Parasitism of certain types of helminths (opisthorchids) in the ducts.
Also, this condition can develop as a result of congenital malformations of the biliary tract with a change in their shape and lumen diameter. Moreover, signs of this pathological process can appear already in childhood.
Doctors are shocked by the statement of the country's chief cardiac surgeon, Leo Bockeria.
Symptoms
Increased pressure in the hepatobiliary system is a syndrome, not an independent disease. This is due to the fact that this condition develops as a result of other pathological processes. There are several main clinical signs indicating the development of biliary hypertension:
- Unstable stool, which may have a light color or be colorless (due to insufficient flow of bile into the intestines).
Bloating and rumbling, which intensify after eating fatty foods (for the normal process of fat digestion, the presence of bile in the intestines is necessary). Jaundice staining of the sclera of the eyes and skin. Periodic severe itching of the skin caused by irritation of sensitive nerve endings with bile acids, which are absorbed from the hollow structures of the hepatobiliary system into the blood during biliary hypertension.
With a slight obstacle to the outflow of bile, increased pressure in the structures of the hepatobiliary system may not manifest itself in any way for a long time.
Diagnostics
The basis for diagnosing biliary hypertension is visualization of the liver and hollow structures of the hepatobiliary system using ultrasound (ultrasound). Usually this is determined by an increase in the size of the liver and gall bladder, and dilation of the ducts. Using this instrumental examination method, a mechanical obstruction is also identified. If necessary, additional radiography of the hollow structures of the hepatobiliary system is performed with the introduction of a contrast compound into them (the method allows you to visualize the shape of the ducts) and duodenal intubation (a functional method in which the intensity of the secretion of various portions of bile is determined, followed by their laboratory examination).
Treatment
In most cases, radical treatment of biliary hypertension is carried out, aimed at removing the obstruction to the outflow of bile. To do this, surgery is performed. Modern methods of surgical intervention involve the use of laparoscopy - a gentle, low-traumatic operation in which thin tubes with micromanipulators, a camera and lighting are inserted through small incisions. Under visual control on the monitor, the doctor removes the obstacle. Before surgical intervention, conservative therapy is required to improve the general condition of the body.
What is the mechanism of connection between the pancreas and blood pressure?
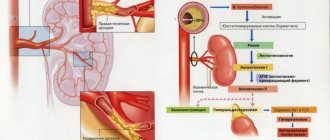
At first glance, it may seem that the pancreas and blood pressure cannot be connected in any way, since completely different body systems are responsible for them. But everything in the human body is interconnected, and diseases of the gastrointestinal tract, including the pancreas, are a common cause of hypertension.
There are several mechanisms by which high blood pressure relates to pancreatitis. Hypertension in acute inflammation of the gland is characteristic of the initial stage. Against the background of a severe pain attack, stress hormones are released and the autonomic nervous system is activated. As a consequence, vasospasm occurs and a violation of adequate blood circulation in all internal organs. It is even possible to develop a hypertensive crisis with all the ensuing complications. In the acute stage, the increase in pressure is not long-term and is replaced by persistent hypotension.
In the chronic course of pancreatitis, the pressure has an abrupt character, but more often patients suffer from hypertension. Since the affected pancreas cannot fully cope with its functions, nutritional deficiency occurs; micro- and macroelements necessary to strengthen the walls of blood vessels, the heart, and nourish the nervous system are not absorbed. With periodic exacerbations, intoxication of the body with decay products increases.
In addition, the inflamed gland swells, squeezing nearby lymph nodes, blood vessels, nerve endings and plexuses. Autonomic innervation is activated and blood pressure increases.
Also in the pancreas are cells that produce insulin, a hormone responsible for the utilization of glucose. If an organ suffers from chronic inflammation, pancreatogenic diabetes mellitus may begin to develop over time. In this disease, insulin production is affected, leading to persistent hyperglycemia (high blood sugar). Due to the pathology, kidney function is impaired (diabetic nephropathy), sodium is not excreted from the body and retains water, which leads to an increase in the volume of circulating blood and an increase in blood pressure.
Treatment
The described disease is treated in two ways, the choice of which depends on what stage of development the disease is at and what type it is (that is, where it is localized). So, treatment can be:
Conservative
It is prescribed if the patient’s condition is not critical and the cause of the disease is not a tumor. Conservative treatment can also be carried out to prepare the patient for surgery.
Treatment is medication. Experts prescribe the following groups of drugs:
- beta-blockers (Atenolol);
- nitrates (Nitroglycerin, Nitrosorbide);
- ACE inhibitors (Monopril);
- Glycoaminoglycans (Sulodexide).
Surgical
There are several indications for this surgical treatment:
- ascites;
- bleeding in the stomach, spleen and intestines;
- Hypersomnic syndrome.
The operation is needed to remove the cause of the disease (tumor or stone), as well as to perform bypass surgery.
If the blockage of the ducts is due to gallstones, surgery will remove the entire gallbladder and the stones. If a malignant tumor is discovered that obstructs the flow of bile, surgery and chemotherapy are performed. In this case, chemotherapy is needed to reduce the size of the tumor and prevent the spread of metastases.
If the cause of the pathology is a benign tumor, then after surgery parts of the tumor are studied histologically to identify the possibility of a secondary appearance of the tumor. For congenital pathology, treatment involves prosthetics. A special material is injected into the narrowed canal, which widens the canal, thereby normalizing the outflow of bile.
Symptoms of the disease
Biliary hypertension is caused by characteristic clinical manifestations and symptoms in the form of:
- Jaundice;
- General weakness and malaise;
- Pain in the abdominal area of various etiologies and duration;
- Dyspepsia, manifested by nausea, vomiting, belching and other symptoms;
- Unsteady stool, development of flatulence;
- Conditions of pain in the right hypochondrium.
Important! Biliary hypertension most often develops in the later stages of pathology. . According to the above, the main cause of this syndrome is malignant neoplasms of the described system
Due to the fact that the growth of such tumors is asymptomatic, the mechanism of development of biliary hypertension already indicates the neglect of this process.
According to the above, the main cause of this syndrome is malignant neoplasms of the described system. Due to the fact that the growth of such tumors is asymptomatic, the mechanism of development of biliary hypertension already indicates the neglect of this process.
Therefore, it is necessary to pay due attention to possible signs of diseases of the liver, biliary tract and pancreas. Since the nonspecific symptoms described above may indicate a disease such as biliary hypertension
The causes and symptoms of the described disease, of course, will help to adjust the correct treatment, but without instrumental research methods they will not be enough.
An obvious clinical sign of pathology can be considered an increase in the size of the spleen. When this condition is neglected, along with high blood pressure, the patient develops the so-called hypersplenism syndrome. In this case, the general symptoms are supplemented by changes in the composition of the blood - leukopenia, thrombocytopenia and anemia develop.
Without untimely therapy, the patient develops obstructive jaundice, which is not amenable to drug treatment. In this condition, mandatory surgical intervention is required.
Also, with increased pressure and insufficient outflow of bile, fluid begins to accumulate in the patient’s abdominal cavity, which requires immediate treatment by eliminating the root cause of the development of the pathological condition.
An external examination of a patient with hypertension may reveal not only an enlarged spleen and liver, but also swelling of the legs. Such progression of the described disease becomes obvious even without examination.
The main reasons for the development of pathology
Biliary hypertension can be an unexpected diagnosis for anyone at any age. However, it is women who are most often prone to difficult bile secretion in the described disease and to biliary hypertension of the biliary system.
Pathologies of the hepatobiliary system can be caused by psycho-emotional stress, hereditary predisposition and many other reasons:
- Tumor neoplasms of various origins. The tumor, regardless of the nature of its occurrence, blocks the path to the natural outflow of bile from the liver and gallbladder and causes signs of biliary hypertension. Moreover, the emerging neoplasm can take hold both in the duct itself and in nearby organs, which as a result can lead to compression of the bile ducts from their side;
- Helminths and other parasites settled in the bile ducts, blocking the path to the normal outflow of digestive secretions from the body. This condition is similar to the symptoms of cholecystitis, which can mislead the patient who actually has biliary hypertension;
- Systemic diseases of an organ such as the liver, bile ducts, leading to the formation of stones of various compositions, and obstructive jaundice along with hypertension;
- Obstruction of the outflow of bile at all levels of the described system due to congenital anomalies of the liver. The ducts may be narrowed or marked by absolute obstruction, which requires therapy with surgical intervention methods.
By identifying the cause of the disease based on the patient’s symptomatic condition and conducting certain clinical studies, it is possible not only to eliminate biliary hypertension, but also the main focus of the pathology.
Treatment
Factors influencing the appearance of HD, the root causes that caused it, the degree of development, forms and types of the disease determine the tactics of the prescribed treatment. GD is treated conservatively, in the early stages, or surgically. Surgical intervention is mandatory for deep damage to internal organs
It is important not to self-medicate and consult a doctor in time.
Conservative treatment
Early diagnosis of HD allows you to avoid surgical intervention. Conservative treatment must be carried out under the supervision of a physician. It is important to accurately select the drug and its dosage. Adrenergic blockers are prescribed, for example, Anaprilin or Atenolol; nitrates – Nitrosorbide, Nitroglycerin; glycosaminoglycans – Sulodexide; ACE inhibitors – Monopril or Ednit.
The basis of conservative treatment is vasodilating drugs, such as Atenolol, prescribed orally. The drug lowers arterial and venous pressure, reduces circulatory pressure, without affecting the lipid composition of the blood, and helps strengthen the walls of blood vessels. Advantages of the drug: speed of action, does not bind to plasma proteins; low solubility in fats. Contraindications: hypersensitivity to components, low blood pressure, hyperacidity, asthma, diabetes.
Nitroglycerin is rarely prescribed in its pure form. The drug has a vasodilating effect and relieves attacks of angina pectoris - sharp pain in the hypochondrium and abdominal cavity, therefore it is prescribed in emergency cases. Treatment with Nitroglycerin requires constant monitoring; exceeding the dose contributes to a sharp decrease in blood pressure. Long-term use of the drug causes a decrease in the body's sensitivity.
Monopril is prescribed for all types of hypertension and heart failure. Its advantage in HD is that it does not disrupt blood flow inside the liver and kidneys and does not change the body’s metabolism. Disadvantages: has a number of side effects on the gastrointestinal tract and respiratory system, contraindicated for children, pregnant women, and lactation. The dosage is selected individually.
Surgery
HD requires surgical treatment. Deep damage to internal organs, tumors, purulent formations, etc. must be removed to prevent complications. The method of surgical intervention depends on the root cause of the disease:
| Root cause of HD | Recommendations for operations |
| Cholelithiasis | Crushing and removal of gallstones. Removal of the bladder along with stones. |
| Tumors of internal organs | Removal of tumor, chemotherapy, radiotherapy. |
| Parasitic formations, polyps | Laparoscopy. Polyp removal. |
| Congenital pathology | Prosthetics is the introduction of expanding material into abnormal canals. |
Pathogenesis of the disease
Increased pressure in the liver ducts occurs with malignant damage to both the detoxifying organ and the gallbladder. This condition is complicated by obstructive jaundice in most cases. Most often, the location of a pancreatic tumor is at its head, which mediates signs of increased pressure due to compression of the ducts. Additional pressure is created by obstructive objects - stones and polyps. In response to this, the biliary ducts strive to expand for their full functioning. All this causes the development of hypertension, to which additional pressure is imparted by vascular resistance.
High pressure can form in certain parts of the bile excretory system, which divides biliary hypertension into several types.
The pathology is difficult to diagnose and can be detected already at advanced stages of its development.
Its hidden and imperceptible symptoms until a certain moment allow the disease to develop and form complications, which are the ones that are most often paid attention to first.
Patients weaken and cannot perform their usual work, they are tormented by dyspeptic disorders and unbearable abdominal pain.
Such a complex of clinical manifestations should be an immediate reason to consult a doctor, since only timely diagnosis determines a favorable outcome in eliminating the pathological focus.
Emergency surgical treatment creates additional complications that lead to a decrease in quality of life and, sometimes, death.
Diagnostic measures
The primary diagnosis of the described disease begins with a visit to a therapist who conducts a general examination. Based on complaints, the patient is referred to a gastroenterologist.
To diagnose biliary hypertension, it is necessary to measure the pressure in the ducts that remove bile. It is impossible to do this directly, so the patient is prescribed the following procedures - ultrasound, CT or MRI with contrast, x-rays. The scanning method is selected individually depending on the patient’s complaints and general health.
When scanning, doctors pay special attention to the study:
- ducts (how dilated they are);
- liver (is the organ enlarged);
- spleen and gallbladder (state of the organs’ vessels, and whether they are enlarged or not).
As part of the diagnosis, blood is also taken from a patient's vein for biochemical analysis to determine the response to tumor markers.
In 90% of cases, the listed diagnostic measures are sufficient to detect biliary hypertension. In rare cases, when there is doubt about the diagnosis, laparoscopy is additionally prescribed.
Symptoms
Biliary hypertension causes a variety of symptoms. If we are talking about jaundice, then one of the visible symptoms is the yellow color of the patient’s face and eye sclera.
At the initial stage of the disease, you may not pay attention to the symptoms that appear, because they are mild. However, sometimes in the first stages of the disease the following signs of the disease may occur:
- Bloating.
- Vomiting and nausea.
- General weakness.
- Regular belching.
- Decreased appetite or reluctance to eat.
- Unpleasant taste in the mouth, possible perversion of taste (bitterness in the mouth).
- Pain in the epigastric region and the area of the right hypochondrium.
- Flatulence (increased gas formation).
In severe or complicated forms of biliary hypertension, the following are added to the above symptoms:
- Modification of bowel movements. Feces become suspiciously light or transparent due to a lack of bile.
- Urine becomes darker.
- Flatulence occurs due to abnormal digestion of food associated with a lack of bile.
- The anterior abdominal veins become dilated.
To prescribe emergency therapy, a thorough diagnosis will be required, during which specialists can detect fluid in the abdominal cavity, an enlarged spleen and other factors confirming the presence of the disease. Otherwise, human organs may fail to function.
If biliary hypertension is detected at an advanced stage (with complications), in addition to the symptoms described above, bleeding may appear due to damage to the veins of the digestive system and rectum, and severe kidney failure. Very often, these deviations are accompanied by leukopenia, thrombocytopenia and a critical lack of iron in the body. This problem occurs due to the destruction of blood cells, particles of which settle in the spleen.
If the patient refuses treatment or does not want to visit the clinic, he may put himself in even greater danger. With cholangitis, a purulent inflammatory process of the biliary tract, microbes that cause infection are detected.
Also, due to impaired outflow of bile, liver cells gradually die, and in their place fibrous tissue appears, causing biliary cirrhosis. A liver abscess may also occur, in which a cavity filled with pus forms inside the liver.
If a person seeks help from a doctor in time, he can avoid the problems described above and incur lower treatment costs. It is recommended that the whole family undergo an examination of the body annually to prevent severe forms of many diseases, including biliary hypertension.
What is the prognosis of a patient with hypertension due to pancreatitis?
The prognosis of a patient with a combination of pancreatitis and hypertension is unfavorable. In severe acute cases of the disease, death is possible in the first days due to the development of shock.
Chronic inflammation of the pancreas with periodic exacerbations leads to exhaustion of the body, deviations in water-salt and electrolyte balance. Anemia, hypoproteinemia, disturbances in the ratio of protein fractions, and accelerated ESR are possible. These factors negatively affect the functioning of the cardiovascular system and, against the background of hypertension, can cause a lot of complications, including strokes and heart attacks. The appearance of pancreatogenic diabetes further aggravates the course of the disease and worsens the further prognosis.
Prevention of complications of pancreatic hypertension are:
- following a diet (excluding fatty, fried, spicy foods, eating plant foods);
- cessation of drinking alcohol and smoking;
- normalization of body weight;
- performing moderate physical activity;
- avoidance of stressful situations;
- compliance with doctor's recommendations.