Blood transfusion is a transfusion of donor (sometimes own, previously prepared) blood. Most often, it is not whole blood that is used, but its components (erythrocytes, platelets, plasma). The procedure has strict indications - severe blood loss with anemia, shock, sepsis. Causes a reaction because foreign proteins are introduced into the body.
With repeated or massive transfusion, or insufficient consideration of compatibility with the donor’s blood, life-threatening complications arise. Find out more about them and the rules of blood transfusion in this article.
What types of blood transfusions are there?
There are five main types of blood transfusion, depending on the method of transfusion.
Direct transfusion
Blood is taken from a previously screened donor using a syringe and injected directly into the patient. To prevent the liquid from coagulating during the procedure, substances that prevent this process can be used.
Shown if:
- Indirect infusion did not show effectiveness, and the patient’s condition is critical (shock, 30-50% of blood lost),
- A patient with hemophilia has extensive hemorrhage,
- Disturbances in hemostatic mechanisms were detected.
Blood transfusion procedure
Exchange transfusion
During this procedure, blood is removed from the patient and donor blood is injected at the same time. This method makes it possible to quickly remove toxic substances from the bloodstream and restore the lack of blood elements. In some cases, using this method, a complete blood transfusion is performed.
Carried out when:
- Hemolytic jaundice in newborns,
- A state of shock that developed after a failed blood transfusion,
- Acute renal failure,
- Poisoning with toxic substances.
Transfusion of a patient's own blood (autohemotransfusion).
Before surgery, a certain amount of blood is withdrawn from the patient, which is then returned to him if bleeding occurs. This method, associated with the introduction of one’s own blood, has an advantage over others due to the absence of negative effects that arise when introducing donor material.
Indications for transfusion:
- Problems in selecting a suitable donor,
- Increased risks when transfusing donor material,
- Individual characteristics (rare group, Bombay phenomenon).
Blood compatibility
Autohemotransfusion has found application in sports and is called blood doping: the athlete is injected with his previously withdrawn material 4-7 days before the competition. It has a number of adverse effects and is prohibited for use.
Contraindications:
- Low protein concentration,
- Heart failure grade 2 or higher,
- Severe weight deficiency
- Systolic pressure below 100 mm,
- Mental illnesses that are accompanied by disturbances of consciousness,
- Disruptions in cerebral blood supply processes,
- Oncological diseases in the terminal stage,
- Problems with the liver or kidneys,
- Inflammatory reactions.
Indirect transfusion
The most common method of blood transfusion. The material is prepared in advance using special substances that extend its shelf life. When the need arises, blood of suitable characteristics is transfused to the patient.
Reinfusion
This technique is considered part of autohemotransfusion, since the patient is injected with his own blood. If bleeding occurs during surgery and fluid enters one of the body cavities, it is collected and reinjected. This technique is also used for traumatic injuries of internal organs and blood vessels.
Reinfusion blood transfusion is not practiced if:
- There was blood in the abdominal cavity for more than a day,
- The patient has cancer,
- The damage affected the hollow organs of the thoracic and abdominal areas (intestines, stomach, bladder, bronchi, esophagus, gall bladder).
Before administration, the collected blood is filtered through eight layers of gauze. Other cleansing methods may be used.
Blood transfusion is also divided according to the method of administration:
Intravenous. This is done either with a syringe (venipuncture) or with a catheter (venesection). The catheter is connected to the subclavian vein, and donor material is supplied through it. Can be installed for a long time.
The subclavian vein is well suited for catheterization, as it is conveniently located, easy to find under any circumstances, and the speed of blood flow in it is high.
Intra-arterial. It is carried out in the following cases: when the heartbeat and breathing stop, which were caused by extensive blood loss, with low effectiveness of classical infusions into a vein, with an acute state of shock, during which a pronounced decrease in blood pressure is observed.
The blood transfusion process uses arteries in the thigh and shoulder. In some cases, administration is carried out intra-aortically - the blood is directed into the aorta, the largest artery of the body.
Transfusion is indicated for clinical death, which occurs due to volumetric blood loss during surgical interventions in the chest, and to save life in other critical situations, when the likelihood of death due to severe bleeding is very high.
Intracardiac. This procedure is done in extremely rare cases when there are no alternative options. Donor material is infused into the left ventricle of the heart.
Intraosseous. It is used only in cases where other methods of blood transfusion are not available: when treating burns that cover a large part of the body. Bones that contain trabecular substance are suitable for introducing the material. The following areas are most convenient for this purpose: chest, calcaneus, femur, iliac crest.
Intraosseous infusion occurs slowly due to the structure, and to speed up the process, increased pressure is created in the blood container.
In what cases is blood transfusion necessary?
Due to the risks of blood transfusion, which are associated with varying degrees of sensitivity of the body to components of foreign material, a strict list of absolute and relative indications and contraindications for the procedure has been defined.
The list of absolute indications includes situations where blood transfusion is necessary, otherwise the probability of death is close to 100%.
Absolute readings
Severe blood loss (over 15% of the total blood). With significant blood loss, consciousness is impaired, a compensatory increase in heart rate is observed, and there is a risk of developing soporous states and coma.
Donor material restores lost blood volume and speeds up recovery.
Severe shock caused by excessive blood loss or other factors that can be eliminated by blood transfusion.
Any shock requires urgent treatment, otherwise there is a high probability of death.
When relieving the vast majority of shock conditions, the use of donor material is often necessary (this is not always whole blood).
If cardiogenic shock is detected, transfusion is carried out with caution.
Anemia, in which the hemoglobin concentration is below 70 g/l. Severe types of anemia rarely develop against the background of malnutrition; usually their development is due to the presence of serious diseases in the body, including malignant neoplasms, tuberculosis, stomach ulcers, and diseases that are associated with impaired coagulation processes.
Also, severe anemia of the posthemorrhagic type develops against the background of severe blood loss. Blood transfusion, done on time, allows you to restore the lost volume of hemoglobin and valuable elements.
Traumatic injuries and complex surgical operations that resulted in massive hemorrhage. Any surgical intervention requires the availability of pre-prepared supplies of donor blood, which will be transfused if the integrity of the walls of large vessels is compromised during the operation. This is especially true for complex interventions, which include those performed in areas where large vessels are located.
The list of relative indications includes situations in which blood transfusion is an additional measure along with other therapeutic procedures.
Relative readings
Anemia. Blood transfusions are used to treat anemia of varying severity.
This procedure is performed if there are special indications, including:
- Disturbances in the mechanisms of oxygen transport into venous blood,
- Heart defects
- Intense hemorrhages,
- Heart failure,
- Atherosclerotic changes in cerebral vessels,
- Problems with lung function.
If one indication (or more than one) is present, transfusion is recommended.
Hemorrhages that are caused by disruptions in homeostasis mechanisms. Homeostasis is a system that maintains blood in a liquid form, controls coagulation processes and removes remnants of clotted blood.
Severe intoxication. In these situations, exchange blood transfusion is used, which is indicated for the rapid removal of poisons from the body. It is effective in removing toxic substances that remain in the blood for a long time (akrikhin, carbon tetrachloride), and in restoring substances that lead to the breakdown of red blood cells (lead, nitrophenol, aniline, nitrobenzene, sodium nitrite) after entering the body.
Low immune status. If there is a shortage of leukocytes, the body is vulnerable to infections, and in some cases they can be replenished with the help of donor material.
Kidney disorders. One of the symptoms of severe kidney failure is anemia. Its treatment is not started in all cases and is indicated if a low hemoglobin concentration can lead to the development of heart failure.
Blood transfusion for this pathology provides short-term benefit, and the procedure must be repeated periodically. Red blood cell transfusions are common.
Liver failure. Transfusion of blood and its elements is indicated to correct disturbances in the mechanisms of homeostasis. Carried out when indicated.
Oncological diseases , which are accompanied by internal bleeding, homeostasis disorders, and anemia. Transfusion reduces the risk of complications, alleviates the patient’s condition, and helps to recover from radiation therapy and chemotherapy. But whole blood is not transfused, as this accelerates the spread of metastases.
Septic lesion. In case of sepsis, blood transfusion enhances immune defense, reduces the severity of intoxication and is used at all stages of treatment. This procedure is not performed if there are serious disturbances in the functioning of the heart, liver, spleen, kidneys and other organs, as this will lead to a worsening of the condition.
Hemolytic disease in newborns. Blood transfusion is a key method of treating this pathology both before and after the birth of a child.
Treatment with blood transfusions is also carried out for severe toxicosis and purulent-septic diseases.
41% of cancer patients report wanting relief from severe fatigue due to anemia, which is treated with blood transfusions.
Indications for blood transfusion
Due to the high risk of destruction of red blood cells (hemolysis), infectious complications, allergic reactions, whole blood is transfused in case of acute blood loss, if it is impossible to eliminate the deficiency of red blood cells and plasma in other ways. There are many more indications for the administration of blood components:
- blood loss of more than 15% of the total volume of the bloodstream;
- hemorrhagic, traumatic shock (due to bleeding);
- extensive operations with massive tissue damage;
- severe anemia;
- infectious, septic processes with severe intoxication;
- blood clotting disorder;
- continued bleeding after surgery or injury;
- burn disease;
- disruption of the formation of blood cells in the bone marrow;
- long-term inflammatory reaction with decreased immunity;
- poisoning with poisons that destroy red blood cells.
Hemotransfusion and transfusion of blood components are carried out for replacement and hemostatic purposes; such therapy also has a stimulating and detoxifying (cleansing) effect.
We recommend reading the article on blood rheology. From it you will learn about disorders of blood rheology, measurement methods and evaluation of indicators. And here is more information about the hematocrit analysis.
When is transfusion contraindicated?
The presence of contraindications to blood transfusion is due to:
- Increased risk of a rejection reaction,
- Increased stress on the heart and blood vessels due to increased blood volume after transfusion,
- Exacerbation of inflammatory and malignant processes due to accelerated metabolism,
- An increase in the amount of protein breakdown products, which increases the load on organs whose functions include removing toxic and waste substances from the body.
Absolute contraindications include:
- Infectious endocarditis in acute or subacute form,
- Pulmonary edema,
- Severe disturbances in the mechanisms of cerebral blood supply,
- Thrombosis,
- Myocardiosclerosis,
- Sclerotic changes in the kidneys (nephrosclerosis),
- Myocarditis of various etiologies,
- The third and fourth stage of hypertension,
- Severe heart defects,
- Retinal hemorrhage,
- Severe atherosclerotic changes in the vascular structures of the brain,
- Sokolsky-Buyo disease,
- Liver failure,
- Kidney failure.
Hemolysis of foreign red blood cells
When transfusing blood components, many absolute contraindications become relative. Also, most absolute contraindications are neglected if the risk of death if blood transfusion is refused is high.
Relative contraindications:
- Amyloid dystrophy,
- High sensitivity to protein, allergies,
- Disseminated pulmonary tuberculosis.
Representatives of some religions (for example, Jehovah's Witnesses) may refuse transfusions for religious reasons: their teaching defines this procedure as unacceptable.
The attending physician weighs the pros and cons associated with the indications and contraindications, and makes a decision regarding the advisability of the procedure.
Contraindications for direct transfusion
Direct blood transfusion is unacceptable in the following cases:
- Lack of proper medical equipment and specialists capable of performing the procedure.
- Medical tests for donor diseases.
- The presence of acute viral or infectious diseases of both participants in the procedure (donor and recipient). This does not apply to children with purulent-septic diseases, when the material is supplied in small doses of 50 ml via a syringe.
The entire procedure takes place in specialized medical centers, where medical examinations of both the donor and recipient are carried out.
What tests are done before a blood transfusion?
Before giving a blood transfusion, the doctor needs to do the following:
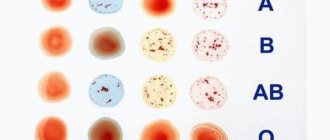
- An analysis that allows you to determine which group the recipient’s blood belongs to and what its Rh factor is. This procedure is always performed, even if the patient claims to know exactly the characteristics of his own blood.
- A test to determine whether the donor material is suitable for a particular recipient: a biological test during transfusion. When a needle is inserted into a vein, 10-25 ml of donor material (blood, plasma or other components) is injected. After this, the blood supply stops or slows down, and then, after 3 minutes, another 10-25 ml is injected. If after three injections of blood the patient’s well-being has not changed, the material is suitable.
- Baxter test : 30-45 ml of donor material is infused into the patient, and after 5-10 minutes blood is taken from a vein. It is placed in a centrifuge, and then its color is assessed. If the color has not changed, the blood is compatible; if the liquid has become paler, the donor material is not suitable.
Also, in some cases, other compatibility tests are carried out:
- Test using gelatin,
- Coombs test,
- Test on a plane
- Two-step test using antiglobulin,
- Test with polyglucin.
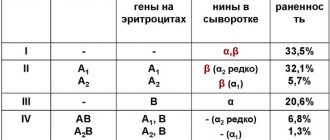
Blood group I: compatibility scheme
During transfusion, group I with a negative Rh value (0(I)Rh-) can be a donor for all blood groups with positive and negative Rh factor in case of emergency transfusion and, if a large volume is needed, act as a donor for group I with an identical Rh value.
For a recipient with the first blood group and a positive Rh factor, the donor blood can be the first positive or negative group 0(I)Rh-/+. In case of the first blood group with a negative Rh index, transfusion is performed only with an identical group 0(I)Rh-.
Which doctor performs blood transfusion?
A hematologist is a doctor who specializes in pathologies of the blood and hematopoietic system.
The main functions of a hematologist:
- Treatment and prevention of diseases of the circulatory system and hematopoietic organs (including anemia, leukemia, pathologies of hemostasis),
- Participation in bone marrow and blood tests,
- Identification of blood characteristics in complex cases,
- Carrying out highly specialized tests,
- Control of blood transfusion processes.
There is also a separate direction in medicine, which is directly related to the processes of blood transfusion - transfusiology. Transfusiologists check donors, monitor transfusion treatment, and collect blood.
How is the donor prepared?
A donor can be a person 18-45 years old who has no contraindications for donating blood and has the results of a preliminary examination and tests confirming the absence of AIDS, hepatitis B and syphilis. Typically, in specialized departments, a donor is selected from a special personnel reserve, based on his willingness to provide assistance to the patient and his blood type.
On the day of direct blood transfusion, the donor is provided with tea with sugar and white bread. After completing the procedure, he is given a hearty lunch and a certificate of release from work is issued for rest after blood sampling.
What are the rules for blood transfusion?
The general rules for the procedure include the following:
- The blood transfusion process must be done in complete disinfection,
- Preparation for transfusion should include all necessary tests and tests,
- The use of donated blood that has not been tested for infections is unacceptable,
- The volume of blood taken during one procedure should not exceed 500 ml. This material is stored for no more than 21 days from the date of removal under special temperature conditions,
- When carrying out blood transfusion in a newborn, a strict dosage should be observed, determined individually.
Failure to comply with these rules is dangerous, as it leads to the development of severe complications in the patient.
Blood transfusion algorithm
Information on how to correctly perform a blood transfusion in order to prevent complications has long been known to doctors: there is a special algorithm according to which the procedure is carried out:
- It is determined whether there are contraindications and indications for transfusion. The patient is also interviewed to find out whether he has had a blood transfusion before, and if he has had such an experience, whether complications have arisen. If the patient is female, during the interview it is important to find out whether there has been any experience of pathological pregnancies.
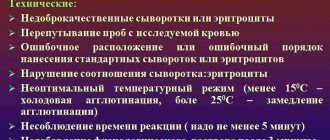
- Studies are carried out to determine the characteristics of the patient’s blood.
- A donor material suitable for its characteristics is selected. A macroscopic evaluation is then carried out to determine its suitability. If there are signs of infection in the vial (presence of clots, flakes, cloudiness and other changes in the plasma), this material should not be used.
- Analysis of donor material according to the blood group system.
- Carrying out tests that allow you to find out whether the donor material is suitable for the recipient.
- The transfusion is carried out by drip, and before the procedure, the donor material is either heated to 37 degrees or left at room temperature for 40-45 minutes. You need to drip at a speed of 40-60 drops per minute.
- During blood transfusion, the patient is under continuous monitoring. When the procedure is completed, a small amount of donor material is stored so that it can be examined if the recipient has any problems.
- The doctor fills out a medical history, which includes the following information: blood characteristics (type, Rh), information about the donor material, date of the procedure, results of compatibility tests. If complications arise after a blood transfusion, this information is recorded.
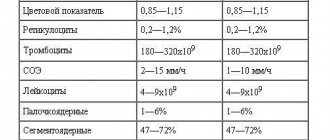
- After the blood transfusion, the recipient is monitored for 24 hours; urine tests are also carried out, blood pressure, temperature, and pulse are measured. The next day, the recipient donates blood and urine.
Why can't you transfuse a different blood type?
If a person is given blood that is not suitable for him, a rejection reaction will begin due to the reaction of the immune system, which perceives this blood as foreign. If a large amount of inappropriate donor material is transfused, it will lead to the death of the patient. But errors of this kind are extremely rare in medical practice.
Antibodies affecting blood compatibility
How long does a blood transfusion take?
The rate of infusion and the total duration of the procedure depends on various factors:
- The chosen method of administration,
- The amount of blood that needs to be transfused
- Features and severity of the disease.
On average, a blood transfusion lasts from two to four hours.
How is blood transfusion given to newborns?
The dosage of blood for a newborn is determined individually.
Most often, blood transfusion is performed to treat hemolytic disease and has the following features:
- The method of exchange blood transfusion is used,
- The material is transfused either from the first group or from the one identified in the child,
- Red blood cells are used for transfusion,
- Plasma and solutions that replace it are also dripped,
- Before and after the procedure, albumin is administered in an individual dosage.
If a child has been transfused with blood type I, his blood temporarily acquires this group.
Where is blood taken?
The main sources of material include:
- Donation. Central source of blood. If the diagnosis has confirmed that the person who wants to donate blood is healthy, he can be a donor.
- Waste blood. It is removed from the placenta, preserved and used for the manufacture of drugs, including fibrinogen and thrombin. About 200 ml of material is obtained from one placenta.
- Corpse material. It is seized from dead people who did not have serious illnesses. Seizure is carried out in the first six hours after death. From one body you can get about 4-5 liters of material, which is carefully checked for compliance with standards.
- Autoblood. The patient donates his own blood before a complex surgical procedure, and it is used if bleeding occurs. Material that has been shed into body cavities is also used.
What types of blood transfusion media are there?
Transfusion media include all components and drugs that have been created on a blood basis and are introduced into the blood vessels.
- Canned blood. To preserve blood, preservative, stabilizing substances and antibiotics are added to it. The duration of storage is related to the type of preservative. The maximum period is 36 days.
- Heparinized. Contains heparin, sodium chloride and glucose, which stabilize it. Used in the first 24 hours, used in devices that provide blood circulation.
- Fresh citrate. Only a stabilizing substance is added to the material, which prevents clotting - sodium citrate. This blood is used in the first 5-7 hours.
Whole blood is used much less frequently than components and drugs based on it, and this is associated with a large number of risks, side effects and contraindications. Transfusion of blood components and drugs is more effective, since it is possible to have a targeted effect.
- Erythrocyte suspension. Consists of red blood cells and a preservative.
- Frozen red blood cells. Plasma and blood cells, except red blood cells, are removed from the blood using a centrifuge and solutions.
- Erythrocyte mass. Using a centrifuge, the blood is separated into layers, and then 65% of the plasma is removed.
- Platelet mass. Obtained using a centrifuge.
- Leukocyte mass. The use of leukocyte mass is indicated for septic lesions that cannot be cured by other methods, with a low concentration of leukocytes and to reduce leukopoiesis after chemotherapy treatment.
- Liquid plasma. Used in the first 2-3 hours. Contains beneficial elements and protein.
- Dry plasma. It is produced using a vacuum from pre-frozen food.
- Protein. Used in sports, a source of amino acids.
- Albumen. Used for ascites, severe burns and for recovery from shock states.
Red blood cells and hemoglobin
Transfusion material is stored in special containers.
What are the risks of blood transfusion?
Disorders and illnesses after blood transfusion are usually associated with medical errors at any stage of preparation for the procedure.
The main reasons for the development of complications:
- Mismatch between the blood characteristics of the recipient and the donor. Blood transfusion shock develops.
- Hypersensitivity to antibodies. Allergic reactions occur, including anaphylactic shock.
- Poor quality material. Potassium poisoning, febrile reactions, infectious-toxic shock.
- Mistakes during blood transfusions. Blocking the lumen in a vessel with a thrombus or air bubble.
- Massive blood volume transfusion. Sodium citrate poisoning, massive transfusion syndrome, cor pulmonale.
- Infected blood. If the donation material has not been properly tested, it may contain pathogenic microorganisms. Dangerous diseases, including HIV, hepatitis, and syphilis, are transmitted through transfusion.
Second group compatibility
The second negative group A(II)Rh- can become a donor for the second and fourth with any Rh index. The second positive group A(II)Rh+ is used as a donor only for the second and fourth AB(IV)Rh+ with a positive Rh factor.
A recipient with the second positive group A(II)Rh+ can accept donor blood of the first 0(I)Rh-/+ and the second group A(II)Rh -/+ with any Rh index. If the recipient's blood is indicated by a negative Rh value A(II)Rh, the transfusion is performed with the same groups as for the second positive, only with an exclusively negative Rh factor value.
What are the benefits of blood transfusion?
To understand why blood is transfused, it is worth considering the positive effects of the procedure.
Donor material introduced into the circulatory system performs the following functions:
- Substitute. Blood volume is restored, which has a positive effect on heart function. Gas transport systems are restored, and fresh blood cells perform the functions of lost ones.
- Hemodynamic. The functioning of the body improves. Blood flow increases, the heart works more actively, blood circulation in small vessels is restored.
- Hemostatic. Homeostasis improves, blood clotting ability increases.
- Detoxification. Transfused blood accelerates the body's cleansing of toxic substances and increases resistance.
- Stimulating. Transfusion causes the production of corticosteroids, which has a positive effect on both the immune system and the general condition of the patient.
In most cases, the positive effects of the procedure outweigh the negative ones, especially when it comes to saving lives and recovering from serious illnesses. Before discharge after a blood transfusion, the attending physician will give recommendations regarding nutrition, physical activity and prescribe medications.