What is a biological sample and its features
Blood transfusion or blood transfusion is a treatment that has saved millions of lives. But the result of transfusion can be not only positive, but also negative.
It is impossible to give a 100% guarantee that patients who have received donor blood transfusions will not experience negative reactions and complications. To prevent this from happening, samples are taken from the donor and recipient for individual blood compatibility.
A biological test for blood transfusion is performed at the beginning of the transfusion procedure. It protects the patient from complications caused by secondary red blood cell group systems. They are represented by a large number of antigens.
Tests for individual compatibility
Tests for individual compatibility are carried out according to two systems: according to the AB0 system, as well as according to the Rh factor of the donor and recipient.
According to the AB0 system
Centrifuge used to determine blood groups
When conducting an AB0 individual compatibility test (also known as a cold test):
- Take 3-5 ml of fresh blood from the recipient and centrifuge it
- take a drop of the resulting serum.
- The drop is then placed on a white plate next to a small drop of the donor's blood and the drops are mixed
- After 5-10 seconds it is assessed whether the solution has changed or not.
- If “clumping” of red blood cells has not occurred, then you can proceed to a test to determine individual compatibility according to the Rh factor.
By Rh factor
There are two generally accepted ways to determine Rh compatibility.
The first involves the use of a centrifuge. To do this, place 2 drops of the patient’s serum, 1 drop of blood from the vial, 1 drop of 33% dextran into a centrifugation tube and centrifuge for 5 minutes. After this, 3-4 ml of saline solution is added to the mixture and the results are assessed. If there is no agglutination, you can proceed to the biological compatibility test.
The second method (the so-called thermal test) is as follows. The flask contains 1 drop of donor blood, 2 drops of warm 10% gelatin solution and a couple of drops of recipient serum. The mixture is incubated for 10 minutes in a water bath, where the temperature is maintained at +46-+48 degrees, and then 5 ml of physiological isotonic solution is also added. The results are assessed in the same way as a centrifuge test.
Types of group affiliation that are checked during testing
Upon admission of a patient who needs a biofluid transfusion, an initial study is carried out on the R-factor and blood type. The procedure is carried out in clinics and diagnostic laboratories.
Blood components used for transfusion:
- red blood cells;
- platelets;
- leukocyte mass;
- plasma.
All components must correspond to the ABO system group and the Rh factor that the recipient has.
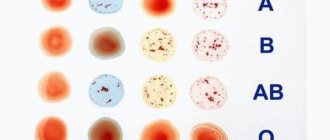
According to the AB0 system
Blood group ABO is the main blood classification system used throughout the world. This is the basis for comparing blood between donors and patients. A person's blood group ABO status is determined through genetic inheritance. Some people inherit genes known as A genes. These code for antigens that cause blood cells to be rejected.
These people have type A blood. Others inherit B genes, which code for the B antigen and have blood type B. It is also possible to inherit one copy of each antigen from their parents, resulting in AB blood. Some people inherit neither A nor B genes. They have type 0 blood in their bodies.
Test technique using the AB0 system:
- a plate is taken, on one side of which the patient’s data is entered, and on the other side 2 drops of his blood serum are applied;
- a drop of donor blood is added to it (ratio 10:1);
- the blood is mixed by periodically shaking the plate, the reaction is observed by a laboratory assistant;
- if there is no adhesion of the donor’s red blood cells, the laboratory assistant concludes that the blood is compatible for groups ABO;
- if sticking (agglutination) appears, this indicates their incompatibility.
By Rh factor
The blood grouping system is complicated by the presence or absence of the Rh factor, another important component in the blood. The presence or absence of the R factor indicates that someone has "negative" or "positive" blood. Instead of dividing people by blood type into A, B, AB or 0, doctors determine whether they are A-, A+, B-, B+, AB-, AB+, 0- or 0+.
The specificity of any organism is determined by the set of proteins or antigens that are part of any tissue. In the blood, red blood cells are surface antigen complexes.
One of them is the Rh factor or Rh antigen. Depending on this, all people are divided into carriers of the R+ antigen and the R- antigen. With regard to donor compatibility, we are talking only about red blood cells and washed red blood cells.
In the classic version, only blood with the same R-factor and group is considered fully compatible. But this rule does not always work in practice. In some situations, when an urgent transfusion is needed, there is no time to determine compatibility. The only salvation remains a transfusion of whole blood or red blood cells in accordance with the principle of hypothetical compatibility.
Its options are shown in the table:
| donor patient | I group, 0(I) | Group II, A (II) | Group III, B (III) | IV group, AB (IV) |
| I group 0 (I) | compatible | incompatible | incompatible | incompatible |
| II group A (II) | compatible | compatible | incompatible | incompatible |
| III group B (III) | compatible | incompatible | compatible | incompatible |
| IV group AB (IV) | compatible | compatible | compatible | compatible |
From the table we can draw conclusions:
- People with the first blood group are universal donors, but they can only be recipients of blood of the first group.
- People with blood type IV are universal recipients, although they can only donate to people with type IV.
RH factor compatibility in the blood is determined by only two options, regardless of group membership: people with RH-negative blood can only receive RH-negative blood transfusions. People with RH-positive blood can become recipients of either RH-positive or RH-negative blood donors.
Compatibility test for blood groups of the ABO system (on a plane)
Procedure for conducting the study:
The sample is performed on a plate with a wetted surface.
1. The tablet is marked, for which the full name is indicated. and recipient's blood group, full name. and the donor’s blood type and blood container number.
2. Carefully pipet the serum from the test tube with the recipient’s blood and apply 1 large drop (100 µl) to the plate.
3. From a segment of the tube of a plastic bag with a transfusion medium, which is prepared for transfusion specifically for this patient, take a small drop (10 μl) of donor red blood cells and apply next to the recipient's serum (serum to red blood cells ratio 10: 1).
4. The drops are mixed with a glass rod.
Assessing the suitability of blood for transfusion
Before the start of the transfusion, donor blood is checked by the same doctor who will carry out the transfusion procedure and trial actions.
He must inspect the product, noting:
- blood expiration date;
- availability and correctness of certification of the introduced product.
- appearance and condition of biological fluid.
Visually, the blood intended for infusion is divided into 3 layers:
- the top layer is transparent yellow plasma;
- middle layer - a strip of leukocytes and platelets of a grayish color;
- lower – red erythrocytes.
Three layers are characteristic of whole blood intended for transfusion and are clearly visible in glass vials.
If erythrocyte blood components are intended for transfusion, they can be in the form of a suspension, cryopreserved. Another commonly used component is plasma. It is available in liquid and dry, lyophilized form.
Indications and contraindications for transfusion
There are many reasons why a blood transfusion may be needed.
Here are just a few of them:
- Complex surgery or injury that resulted in significant blood loss.
- Bleeding in the gastrointestinal tract due to an ulcer or other disease.
- For leukemia or kidney disease that has caused anemia (a lack of healthy red blood cells).
- After radiation or chemotherapy.
- Blood disease or serious liver problems.
Indications for red blood cell transfusion:
- Acute sickle cell crisis (for stroke prevention).
- Major blood loss >30% of blood volume.
- Hemoglobin <7 g/dl.
- Symptomatic anemia.
Indications for transfusion of plasma products:
- Prevention of active bleeding in a patient on anticoagulant therapy before the procedure.
- Active bleeding.
- Intracranial hemorrhage
- Acute disseminated intravascular coagulopathy.
- Microvascular bleeding during massive infusion.
Platelet transfusions may be indicated to prevent hemorrhage in patients with thrombocytopenia.
An absolute contraindication to blood transfusion is acute heart failure, which is accompanied by pulmonary edema and myocardial infarction. If a person has suffered a traumatic shock and lost a large amount of blood, then in this case blood must be transfused urgently, despite the symptoms of the disease.
Relative contraindications include:
- functional disorders of the liver, kidneys;
- consequences of damage to the walls of blood vessels during thrombolism and thrombosis;
- stage III hypertension;
- complex cerebrovascular disorders;
- cross allergy;
- bronchial asthma;
- heart defect, myocarditis, septic endocarditis;
- miliary, acute tuberculosis;
- hemorrhagic vasculitis.
Blood compatibility between donor and recipient
During a transfusion, the blood must be accurately matched. If a person with blood type A is given blood from a blood type B donor, anti-B antibodies will stick to the B antigens on the donor red blood cells that enter their body. This causes a reaction that can be fatal. Therefore, an exact match is critical.
Cross-matching is a procedure performed before a blood transfusion to determine whether the donor blood is compatible or incompatible with the recipient's blood.
Compatibility is determined by comparing different blood group systems, the most important of which are the ABO and Rh systems, or by direct testing for the presence of antibodies on donated tissue or blood samples. Cross-matching reveals incompatibilities between donor and recipient that would not be visible during blood typing.
Basic cross-matching involves testing the patient's serum with donor cells to determine whether the patient has an antibody that may cause a hemolytic transfusion reaction or decreased donor cell survival.
Biological sample and transfusion procedure
A biological test for blood transfusion is carried out at the beginning of the blood transfusion. Despite checking the AB0 and R-factor groups, doctors cannot always be sure of the complete compatibility of the blood of the donor and the patient. To exclude complications, another test is performed at the beginning of the transfusion - biological.
What a doctor should do before taking a sample
Before blood transfusion, the doctor performs the following actions:
- Indicates the presence of indications for transfusion of one of the blood components in the patient's chart.
- Obtains the voluntary consent of the recipient or his representative to carry out a therapeutic procedure.
- Checks all the data on the label of the container with donor blood, which is inserted into the medical record after the procedure is completed.
- Records the results of testing the patient's blood according to the AB0 system and Rh factor.
- Checks red blood cells or full blood in the container according to the R-factor and AB0 system, and records the test results in the medical record.
- Records both positive and negative results of a biological test performed three times during a blood transfusion.
Where and how is the sample taken?
Blood transfusions, as well as immunohematological tests, are carried out in hospitals, specialized clinics or outpatient clinics. To do this, you need an equipped room with natural light, a temperature of at least 16–25°C, as well as devices, tools, and consumables for testing and therapeutic operations.
A biological test during blood transfusion during blood transfusion is carried out in a hospital setting by the attending or duty doctor. In clinics it is carried out on an inpatient or outpatient basis as prescribed by a surgeon, therapist or hematologist.
Transfusion algorithm
The container with the biological mass is kept in the refrigerator before the procedure begins. Before use, remove it and keep at room temperature for 30–35 minutes. By the time of transfusion it should reach +37°C.
Before starting a transfusion, a biological test must be done, and the doctor carries out a certain sequence of actions:
- 10 ml of blood transfusion fluid is injected dropwise. The rate of administration is from 40 to 60 drops per minute.
- Closes the clamp on the intravenous infusion system.
- Within 3 min. monitors the patient's condition.
During observation the following is checked:
- pulse;
- HELL;
- breath;
- Body temperature;
- change in skin color, if any;
- general state.
The entire sequence of actions is carried out 2 more times. No blood is administered between biological samples.
After the administration of biological test blood, some patients experience alarming signals: chills, nausea, vomiting, feeling hot, chest tightness. If at least one sign is detected, immediate termination of the entire transfusion procedure is required.
After stopping the therapeutic operation, blood is drawn from the patient and sent to the laboratory, where an individual selection of red blood cell mass is performed.
A biological test during blood transfusion is carried out regardless of the amount of blood administered or the speed of its administration. The procedure is also performed in case of emergency transfusion. If several units of blood are administered to a patient, a biological test should be performed before each new dose.
A blood transfusion is a common medical procedure in which donated blood is given through a narrow tube placed in a vein in the arm. People receive blood transfusions for many reasons—surgery, injury, illness, and bleeding disorders.
Blood has several components, including:
- Red cells carry oxygen and help remove waste.
- White cells help the body fight infections.
- Plasma is the liquid part of blood.
- Platelets help blood clot form and stop bleeding.
Transfusion provides the portion of blood that is needed, and red blood cells are most often transfused. Whole blood containing all parts is often given, but whole blood transfusions are not common.
Other routes are used to administer red blood cells in medical practice: intra-aortic, intraosseous, intra-arterial. The donor container with a small remainder of biological fluid should be stored for 48 hours after the procedure.
Transfusion rules
The next step is to take a general blood test and then divide it into two studies, the first of which will be carried out in the laboratory, and the second in special donor departments to determine the group, Rh factor, hemoglobin level and the presence of infections. The results obtained are necessarily compared with each other and if the similarity is confirmed without the presence of infectious diseases, the patient is invited to the office to take a sample. After all the tests, the donor’s blood is collected in a special container and undergoes a degree of purification in a centrifuge, where the plasma is separated from the red blood cells. Next, it is placed in a plasma extractor, which separates the plasma from the cells. All these cleaning measures are mandatory, since whole blood for transfusion, not purified of its contents, has not been used in medical practice for a long time in order to avoid the transmission of infectious diseases.
About 300-400 ml is taken to take.
Detailed video about transfusion
What can and cannot be done after a transfusion?
A patient who has received a dose of blood in a hospital setting must remain in bed for 2 hours. The attending physician is monitoring him at this time. The recipient's blood pressure and body temperature are measured hourly.
The presence of urine is monitored in the form of hourly volume and changes in its color are recorded. A reddish color with transparency indicates the destruction of red blood cells and the development of hemolysis. The next day, the patient undergoes a general urine and blood test.
In the case of blood transfusion in a clinic, the patient after the procedure must be under medical supervision for at least 3 hours. If there is stable blood pressure and pulse, normal urinary function, and the absence of adverse reactions, the patient is released from the clinic.
After a blood transfusion, most people feel fine and experience mild side effects. In rare cases, patients react poorly to blood transfused during the procedure. In such cases, the process is interrupted and the person is given medical assistance. A thorough examination before transfusion is the best way to avoid a bad reaction.
Patient's condition after transfusion
In the vast majority of cases, people can resume normal activities after a blood transfusion, including eating, drinking normally, and taking all existing medications.
Most people can go home soon after a transfusion, unless an underlying medical condition requires a hospital stay. Patients should be aware of the signs of an adverse reaction and seek immediate medical attention if necessary.
It is important that the healthcare professional performing the transfusion screen before the procedure and closely monitor the patient during the process. Reactions are more likely early in the transfusion, although they can sometimes occur later. Acute reactions can be life-threatening if not treated immediately.
Acute hemolytic reactions occur when incompatible red blood cells are given to a patient. This is more often due to errors in obtaining or labeling panel samples and antibody samples or failure to perform necessary bedside checks prior to blood administration.
Signs and symptoms of red blood cell incompatibility:
- Pain at the cannulation site.
- Pain in the chest, back or stomach.
- Hypotension/hypertension.
- Tachycardia.
- Feverish condition.
- Bleeding
- Collapse.
- Hemoglobinuria.
Platelet infusions may cause complications if a contaminated substance is introduced.
Common signs include:
- feverish condition;
- tachycardia;
- collapse;
- acute lung injury caused by transfusion.
Complications from transfusion of plasma containing white cell antibodies occur within 6 hours of transfusion and include:
- nonproductive cough;
- hypotension;
- acute shortness of breath;
- hypoxia.
Allergic reactions usually occur at the beginning of a transfusion, and symptoms include:
- hypotension;
- bronchospasm;
- pain in the chest, stomach;
- shortness of breath;
- nausea, vomiting;
- hives;
- skin redness;
- conjunctivitis.
Serious allergic reactions may occur, anaphylactic shock, in which the patient cannot breathe normally, and heart problems may begin. The post-transfusion reaction is the immune system's response to donated blood. It may occur immediately or much later, and may be mild or severe. The delayed reaction after the procedure may last for 3-10 days.
You should seek medical help if the following signs appear:
- double vision, headache;
- dizziness, feeling of impending fainting;
- nausea, diarrhea, or abdominal cramps;
- purple spots on the body in the form of dots;
- dizziness and weakness approximately 7 days after the procedure;
- sweaty and cool skin;
- blue lips;
- yellowing of the skin and whites of the eyes.
Medicines will help improve the condition:
- Antihistamines will reduce itching and swelling in mild allergic reactions.
- Steroids can be taken to prevent inflammation.
- Medicines to reduce fever will help improve the condition.
- Diuretics will help get rid of excess fluid.
The medications taken should be agreed in advance with the doctor who performed the blood transfusion procedure.
Blood transfusion helps restore blood volume, activate prothrombin, increase blood flow, help the body resist anoxemia, and improve protective functions and resistance to disease. To ensure that the blood transfusion procedure takes place without complications and does not cause further reactions, doctors carry out a serious check in the form of tests for the Rh factor, AB0 and biological samples.
Biological compatibility test
Before the blood transfusion procedure, it is necessary to conduct a biological test
A test for biological compatibility, in fact, is the first stage of blood transfusion itself and is carried out exclusively by a doctor. The doctor conducting the test performs the following actions:
- connects the drip system and injects the first 15-20 ml of donor blood in a stream;
- stops the transfusion;
- waits 3-5 minutes, observing the patient. The appearance of tachycardia, difficulty breathing, lower back pain, chills or fever should alert you.
- if everything goes well, the sample is considered positive and further transfusion is performed
Thus, if all compatibility tests have passed successfully, a blood transfusion can be performed. The correct transfusion rate is 50-70 drops per minute.
Of course, there are not only groups described in the ABO and Rh factor systems, since a total of 250 blood groups have been described to date. However, the compatibility tests described above make it possible to identify incompatibility for most other agglutinins and agglutinogens, which ultimately makes blood transfusions a relatively safe procedure with proper preparation.