In medical terminology, the concept of “blood group conflict” is widely used. This expression denotes the immunological incompatibility that occurs between the blood of a woman and a baby by group.
This effect can occur if blood was transferred from a man, which, in turn, does not coincide with the woman’s and is in conflict with her. This can be observed when the mother has the first group, and the child the second or third, but other variations also occur.
If the situation develops in this way, the danger to health is not as great as with undesirable combinations of Rh factors, but sometimes harm to health is still caused.
Usually, children's and women's blood cannot be mixed during pregnancy, but some of it passes to the mother. The mother's body detects a foreign blood type and detects foreign protein. The body begins to defend itself by producing antibodies.
They attack, sometimes causing pregnancy loss. It happens that this process leads to damage to the fetus: the child is born with acquired hemolytic disease of the newborn.
A blood conflict during the first pregnancy is less dangerous than a conflict due to the Rh factor. With subsequent births from this man, the level of danger will increase, because the mother’s body adapts to foreign blood and becomes sensitized.
What it is?
Since ancient times, women with negative Rh factor blood immediately lost their babies or were born too weak and sickly. Today, the conflict between the blood groups of mother and father can be prevented, since specialized drugs have been created for this. This may be immunoglobulin, which is created from human blood. This injection must be given to a pregnant woman at 28 weeks of pregnancy and must be repeated three days after birth if the baby’s Rh factor is positive.
There is an opinion among doctors that it is advisable for a woman with a negative Rh factor not to have an abortion at all, since this can significantly affect her condition and subsequent ability to bear and give birth to a child. In a situation where an abortion is not planned and childbirth will have to occur, it is necessary to take into account the fact that such women need to give birth at least once.
Then there is a high probability that the child will be healthy, and the mother’s health will not be in any danger either. Her blood composition during the first pregnancy will produce antibodies to the child’s Rhesus, but the second time it will not allow its intervention.
What causes blood type conflict between mother and child?
In medical terminology, the concept of “blood group conflict” is widely used. This expression denotes the immunological incompatibility that occurs between the blood of a woman and a baby by group.
This effect can occur if blood was transferred from a man, which, in turn, does not coincide with the woman’s and is in conflict with her. This can be observed when the mother has the first group, and the child the second or third, but other variations also occur.
If the situation develops in this way, the danger to health is not as great as with undesirable combinations of Rh factors, but sometimes harm to health is still caused.
Usually, children's and women's blood cannot be mixed during pregnancy, but some of it passes to the mother. The mother's body detects a foreign blood type and detects foreign protein. The body begins to defend itself by producing antibodies.
They attack, sometimes causing pregnancy loss. It happens that this process leads to damage to the fetus: the child is born with acquired hemolytic disease of the newborn.
A blood conflict during the first pregnancy is less dangerous than a conflict due to the Rh factor. With subsequent births from this man, the level of danger will increase, because the mother’s body adapts to foreign blood and becomes sensitized.
Mechanism of action
A stable placenta protects against the development of blood group conflict. Its special device prevents the blood of the mother and fetus from mixing, mainly through the placental barrier. However, this can still happen due to the destruction of the blood vessels of the placenta, its detachment and other defects, or, more often, during delivery.
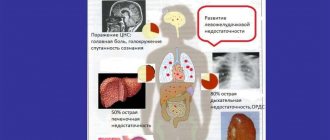
When incompatible, fetal cells that have entered the maternal blood provoke the production of antibodies that can penetrate the fetal body and attack its blood cells, resulting in hemolytic disease. The toxic element - bilirubin, which is formed during such an interaction in significant quantities, can cause damage to the child’s body, mainly to the brain and excretory system. This can be fraught with significant disruptions in the functioning of the body.
In case of compatibility, there is nothing to worry about, but if incompatibility between the blood groups of mother and child is revealed, then the expectant mother will need to be constantly monitored by a specialist in order to prevent negative consequences for the child.
What causes conflict?
A blood conflict during pregnancy occurs if, during the development of pregnancy, incompatible antibodies O± and OI, as well as antigens A and B, are detected.
- If the pregnancy proceeds normally, then mixing does not take place: the placental barrier fully fulfills its role.
- The barrier separates the layers of the placenta belonging to the mother and the pregnant child. During normal gestation, it is a sufficient condition of safety, but sometimes pathological conditions arise: the placenta can exfoliate, which causes displacement.
- Antibodies produced by the mother's body have a destructive effect on the child's cells. Their breakdown leads to the release of toxins that have a destructive effect on the kidneys, liver, etc.
- With this course of events, a hemolytic disease is formed; children are born with jaundice, anemia and various diseases.
- Sometimes dropsy of the brain of the head occurs, caused by the fact that the destruction of cells contributes to the accumulation of excess fluid in the tissues.
The spleen and liver may be enlarged. However, such consequences are quite rare.
Incompatibility
It makes sense to study in detail what incompatibility of blood groups of mother and child is. People with blood type I do not have antibodies A and B, but have beta and alpha antibodies. Other blood groups have antibodies: second (A), third (B), fourth (AB).
As a result of this, the immunity of a woman with the first blood group begins to fight against elements of other blood groups that are foreign to the body. The protective mechanisms of the expectant mother decompose the child’s red blood cells, killing unnecessary antigens contained in the child’s blood. This is what is called incompatibility of the blood groups of mother and baby.
Treatment, possible consequences
Currently, medicine is unable to completely prevent the consequences caused by discrepancies in blood groups. However, it is possible to reduce the risk of unwanted consequences.
If antibodies are detected, you should immediately begin treatment: clean the blood, prescribe activated charcoal and Enterosgel.
At birth, the baby should be tested to detect antibodies. If they are detected, you need to perform phototherapy: use a special lamp to reduce bilirubin. This measure will help when the antibody titer is within the acceptable range; in the case when a rapid increase occurs, phototherapy is powerless. In this case, other methods are used: transfusions, plasmapheresis, hemosorption. They are aimed at improving the baby's health.
Sometimes breastfeeding is not recommended to avoid the penetration of maternal antibodies to the child. In severe situations, breastfeeding is canceled immediately, and special nutrition is prescribed that does not include components harmful to health.
When does it occur?
A conflict occurs when the mother’s blood is incompatible with the child’s blood type. A blood type conflict during pregnancy can contribute to hemolytic abnormalities in the baby.
Hemolytic disease of the newborn is fraught with the production of hemolysis of red blood cells. As a result, there is a great danger of the baby's death. One way or another, erythroblastosis disrupts the natural functioning of the child’s circulatory system. With this type of deviation, the unborn baby is not able to develop harmoniously.
Are there any symptoms?
A pregnant woman may not experience the symptoms associated with blood type conflict during pregnancy. Analysis can reveal its presence. Laboratory tests will determine the high level of antibodies in the blood of the expectant mother. This is the main diagnostic method. With the development of blood diseases in the fetus or infant, the following may occur:
- swelling;
- yellow tint of the skin;
- anemia;
- increased size of excretory organs.
Prevention of significant complications can be achieved by constant monitoring of the mother's blood and determination of certain elements in it - hemolysins. If they are present, the expectant mother is carefully observed by specialists.
If, in the course of further research, the number of antibodies continues to constantly increase, and the condition of the fetus gets worse and worse, then it may be necessary to organize a premature birth or a blood transfusion to the fetus. Some specialists regularly test pregnant women with the first blood group for group antibodies when there is a reason for it.
Assessment of the condition of the fetus and feto-placental complex
To assess the condition of the fetus and feto-placental complex, instrumental diagnostic methods such as cardiotocography (CTG) and ultrasound can be used. According to CTG data, in case of fetal suffering, there are clear signs of fetal heart rhythm disturbances, slowing of heartbeats, monotonous rhythm, etc. An ultrasound examination evaluates the size of the fetus, the condition of its internal organs, the structure and thickness of the placenta, and the volume of amniotic fluid. The functional activity of the fetus is also determined and the intensity of blood flow in the mother-placenta-fetus system is studied using Doppler sonography.
Ultrasound examination in women with expected hemolytic disease of the fetus should be performed at 20-22 weeks, 24-26 weeks, 30-32 weeks, 34-36 weeks. and shortly before delivery. Until 20 weeks of pregnancy, signs of hemolytic disease are not detected echographically. Repeated studies are necessary to exclude dynamic hemolytic disease of the fetus. For each pregnant woman, the timing of repeated scans is determined individually; if necessary, the interval between studies is reduced to 1-2 weeks.
Taking into account that with hemolytic disease of the fetus, swelling of the placenta occurs, its thickening by 0.5 cm or more may indicate a possible disease of the fetus. However, other complications should be excluded, in which thickening of the placenta can also occur (for example, intrauterine infection or diabetes mellitus).
For hemolytic disease of the fetus, along with thickening of the placenta, an increase in the size of its abdomen is possible in comparison with the chest and head of the fetus. This increase is due to the excessive size of the fetal liver, as well as excessive accumulation of fluid in its abdominal cavity (ascites). Swelling of the fetal tissues manifests itself in the form of a double contour of its head. With severe fetal hydrops, there is also an accumulation of fluid in other cavities (hydrothorax, hydropericardium), and signs of swelling of the intestinal walls.
Ultrasound scanning also evaluates the behavioral reactions of the fetus (motor activity, respiratory movements, fetal tone). If its condition is disturbed, corresponding pathological reactions from these indicators are noted. According to Doppler ultrasound, there is a decrease in the intensity of blood flow in the feto-placental complex.
Determination of the optical density of bilirubin, fetal blood type, and antibody titer in amniotic fluid is of great diagnostic importance. On the eve of delivery, it is advisable to examine amniotic fluid to assess the degree of maturity of the fetal lungs.
To study amniotic fluid, starting from 34-36 weeks of pregnancy, amniocentesis is performed, which is a puncture of the uterine cavity to take a sample of amniotic fluid. The procedure is carried out under ultrasound control with anesthesia and in compliance with all rules of asepsis and antisepsis.
Amniocentesis can be performed either through the anterior abdominal wall or through the cervical canal. The puncture site is chosen depending on the location of the placenta and the position of the fetus. Possible complications in this case may be: increased uterine tone, placental abruption, bleeding, rupture of amniotic fluid and the onset of labor, development of inflammation.
Based on the optical density of bilirubin in amniotic fluid, if it is more than 0.1, the possible severity of fetal hemolytic disease is assessed. If this indicator is more than 0.2, one can expect the birth of a child with a moderate to severe form of hemolytic disease.
Detection of the fetal blood type by amniotic fluid is one of the tests that determines the prognosis for the fetus. More often, one can expect the development of hemolytic disease due to incompatibility of the Rh factor, with the same blood group of the mother and fetus.
It is important to determine the blood group if the development of an AB0-conflict pregnancy is suspected. A significant diagnostic test is the determination of antibody titer in amniotic fluid.
To study fetal blood, puncture of the umbilical cord vessels (cordocentesis) under ultrasound guidance is used. A study of the fetal blood obtained in this way makes it possible to determine its blood type and Rh status, assess the level of hemoglobin, serum protein and a number of other indicators that reflect the presence and severity of the complication.
As part of pregnancy management, all patients and their husbands should have their Rhesus status and blood group determined at the first visit to the doctor, regardless of whether childbirth is imminent or termination of pregnancy is planned. In pregnant women with the first blood group, if their husbands have a different blood group, it is necessary to conduct a test to determine group antibodies. Pregnant women with Rh-negative blood must be examined for the presence of antibodies and their titer once a month until 20 weeks, and then once every 2 weeks. If a pregnant woman with Rh-positive blood has an indication of the birth of a child with a hemolytic disease, the blood should be examined for the presence of group immune antibodies, as well as for “anti-c” antibodies if the husband’s blood contains the “c” antigen. The presence of Rh sensitization in pregnant women is not an indication for termination of pregnancy.
Advertising
When to undergo treatment?
If parents find out in advance that their Rh factors are incompatible, then before conception it is best, and in some cases simply mandatory, to take a specialized course in order to prevent the woman’s body from rejecting the fetus.
If, nevertheless, spouses with different Rh factors are already expecting a replenishment, and no preventive steps were taken during pregnancy planning, then it is necessary to carefully monitor the condition of the fetus throughout pregnancy. Currently, if a Rh conflict is detected, it is possible to prevent unpleasant consequences by introducing antibodies - immunoglobulin - at 26-27 weeks.
Planning a pregnancy
Many people ask how to prevent blood type conflict during pregnancy. Most people have the first group, 50% of them. The second occurs in 40% of the population. The third - in 30% of the population. The fourth is the rarest, observed in 15% of residents.
When planning conception, many couples ask whether it is possible to prevent complications of conflict in pregnant women. Parents should be aware of the risk, and in such a situation, the father and mother should be registered in a consultation under the supervision of a specialist. Restoring the number of hormones in the woman’s bloodstream that affect the formation of the placenta - lactogen and gonadotropin - can help.
The placenta is a barrier that prevents the woman's blood from contacting the embryo's bloodstream. If the placenta does not develop properly, detachment or other diseases are observed, then the possibility of conflict increases, and this can cause negative consequences.
If doctors have diagnosed a conflict, then the following measures can be taken:
- Phototherapy is prescribed, which removes toxins from the embryo’s body, including bilirubin.
- Vitamins B, C, E, choleretic agents, and sorbents are prescribed to slow down the absorption of bilirubin by the digestive system.
- The mother is prescribed cleansing enemas and detoxification treatment.
- An intrauterine blood transfusion is given to the child; if the timing allows, a premature birth is performed.
AVO conflict
In most cases, the ABO conflict is expressed in hemolytic (or physiological) jaundice in the child. In addition, children become restless, often scream or, on the contrary, lose activity, become overwhelmed, and sleep longer than children of their age should. In advanced situations, a bilirubin attack affects the baby’s brain and other important organs. But in most cases, congenital jaundice disappears within a couple of weeks with the support and constant monitoring of doctors. The main treatment is to support the child's body.
As during the period of bearing a child, if a high degree of group antibodies is detected, the specialist may prescribe additional injection of glucose into the veins or adding it to the baby’s diet, taking vitamins designed to improve the process of blood purification by the excretory system. If a child has an increased amount of bilirubin, there is no need to resist the prescription of additional complementary foods or medical procedures. As a rule, this does not interfere with breastfeeding. This is a kind of “first aid” for the baby to improve his health. Such activities contribute to the harmonious growth and formation of the body.
Is jaundice possible?
If there is a conflict in the blood type of a newborn, the doctor may prescribe other medications, including during inpatient treatment. If jaundice begins to affect the baby's brain cells, therapy is carried out under close supervision by doctors. Nowadays they often talk about the benefits of late cutting of the umbilical cord after the birth of a child. The tying of the umbilical cord is delayed until its movement stops, which allows the child to receive useful substances after birth. This is exactly the procedure that is prohibited if the parents have different blood types.
Even if it is assumed that the baby received the mother's blood type and there is a high risk of developing a blood type conflict, the umbilical cord should be removed immediately after birth. This will protect the baby from possible problems. However, the main thing with neonatal jaundice is prevention. During the process of bearing a child, a woman does not feel the negative effects of incompatibility with the child. In this regard, if a blood type conflict may arise, it is necessary to be examined in a timely manner, plan the birth with an experienced specialist and remember the need for a correct lifestyle.
Prevention and treatment of hemolytic disease of the fetus
All pregnant women with Rh-negative blood, even in the absence of antibodies in their blood, as well as in the presence of AB0 sensitization, should undergo 3 courses of nonspecific desensitizing therapy on an outpatient basis lasting 10-12 days, at 10-22, 22-24, 32-34 weeks.
As part of nonspecific desensitizing therapy, the following is prescribed: intravenous administration of 20 ml of 40% glucose solution with 2 ml of 5% ascorbic acid solution, 100 mg of cocarboxylase; orally rutin 0.02 g 3 times a day, theonicol 0.15 g 3 times a day or methionine 0.25 g and calcium gluconate 0.5 - 3 times, iron supplements, vitamin E 1 capsule. Antihistamines are used at night: diphenhydramine 0.05 or suprastin 0.025.
In case of complicated pregnancy: threat of miscarriage, early toxicosis of pregnant women, gestosis, etc., patients should be hospitalized in the department of pathology of pregnant women, where, along with treatment of the underlying disease, a course of desensitizing therapy is carried out.
Pregnant women who have a high titer of Rh antibodies and a history of spontaneous miscarriages or delivery of a fetus with an edematous or severe form of hemolytic disease are recommended to use plasmapheresis. This procedure removes antibodies from the blood plasma. Plasmapheresis is carried out once a week under the control of antibody titer, starting from 23-24 weeks. pregnancy, before delivery.
To treat hemolytic disease of the fetus, hemosorption using activated carbon is also used to remove antibodies from the blood and reduce the degree of Rh sensitization. Hemosorption is used in pregnant women with an extremely complicated obstetric history (repeated miscarriages, stillbirth). Hemosorption begins at 20-24 weeks in the hospital, with an interval of 2 weeks.
Treatment of hemolytic disease of the fetus during pregnancy is also possible by transfusion of blood to the fetus under ultrasound guidance.
Pregnant women with Rh sensitization are hospitalized in the maternity hospital at 34-36 weeks. pregnancy. With AB0 - sensitization, hospitalization is carried out at 36-37 weeks. If there are appropriate indications indicating a pronounced nature of the complication, hospitalization is possible at an earlier date.
In the presence of hemolytic disease of the fetus, early delivery is advisable due to the fact that towards the end of pregnancy the flow of antibodies to the fetus increases. In case of severe hemolytic disease of the fetus, pregnancy is terminated at any time during pregnancy. However, in most cases, pregnancy can be prolonged until an acceptable delivery date. As a rule, delivery is carried out through the natural birth canal. Caesarean section is performed in the presence of additional obstetric complications.
During childbirth, careful monitoring of the condition of the fetus is carried out, and hypoxia is prevented. Immediately after birth, the baby is quickly separated from the mother. Blood is taken from the umbilical cord to determine the content of bilirubin, hemoglobin, the child’s blood type, and his Rh status. A special test is performed to identify the newborn's red blood cells associated with antibodies.
Advertising
Hormone levels
It will help to prevent the formation of a blood group conflict during pregnancy by identifying and regulating hormones in a woman’s body that affect the proper formation of the placenta. Since the placental embryonic organ turns out to be a reliable barrier to prevent contact of the mother’s blood with the blood of the fetus. This barrier is located between the maternal and fetal layers of the placenta.
Most often, pregnancy and childbirth proceed well, and advanced forms of hemolytic disease occur once in 200 pregnancies. In addition, it is necessary to register with the antenatal clinic in a timely manner, take all the required tests, and monitor whether the number of antibodies increases. The child’s father must also take a blood test to determine the group and Rh factor. After all, if he has blood of the first group, then there will be no blood group conflict. The effectiveness of controlling such a deviation during pregnancy will depend on how long it will be detected.
Why does immunological conflict occur?
There are four blood groups: first (0), second (A), third (B), fourth (AB). Blood also has a Rh factor: it can be positive or negative.
So, if a pregnant woman and her baby have different blood types or Rh factors, it turns out that the child’s blood contains an antigen that is not in the mother’s blood. This antigen could have been inherited by the baby from the father, whose blood type or Rh is different from the mother’s.
Thus, the mother’s body perceives the fetal blood cells as a foreign formation and begins to produce antibodies aimed at destroying “foreign” cells.
Normally, the placental barrier prevents the mixing of maternal blood with the baby’s blood, but in some pathological conditions (placental abruption, etc.), the functions of the barrier may be impaired.
When does Rh conflict appear?
The baby develops a Rh factor and a Rh blood group conflict during pregnancy, starting from the 7-8th week of fetal development. It is during this period that the child develops his own Rh factor. At the same time, antibodies tend to accumulate, and the situation can change rapidly.
Today you can read many sad stories of mothers who were faced with the result of blood group conflict. As the brain is damaged, they note delays in the baby’s development; at times, vision or hearing may be lost. Some mothers battle baby seizures or raise their children with severe stages of cerebral palsy. But it is no longer possible to restore complete health to such children.
When a woman is Rh negative, she is strongly recommended to take an antibody test during the 7th to 8th week of pregnancy. If there is a risk of developing abnormalities, a new analysis should be performed at 28-30 weeks. With increased values of the number of antibodies in the first trimester, fluctuations in the growth of blood enzymes are monitored more often - once every 14 days. In this case, much will depend on the position of the fetus.
If a blood transfusion cannot be given, then a decision must be made about premature birth. It is absolutely impossible to take risks with such a deviation. If the baby’s pulmonary system has already formed (28th week of pregnancy), then labor must be induced, otherwise the expectant mother may have a miscarriage.
Blood type (AB0)
Determines belonging to a certain blood group according to the ABO system.
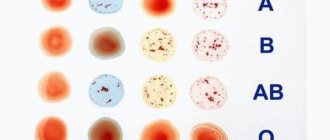
Functions. Blood groups are genetically inherited characteristics that do not change during life under natural conditions. A blood group is a specific combination of surface antigens of erythrocytes (agglutinogens) of the ABO system. Determination of group membership is widely used in clinical practice during transfusion of blood and its components, in gynecology and obstetrics when planning and managing pregnancy. The AB0 blood group system is the main system that determines the compatibility and incompatibility of transfused blood, because its constituent antigens are the most immunogenic. A feature of the AB0 system is that in the plasma of non-immune people there are natural antibodies to an antigen that is absent on red blood cells. The AB0 blood group system consists of two group erythrocyte agglutinogens (A and B) and two corresponding antibodies - plasma agglutinins alpha (anti-A) and beta (anti-B). Various combinations of antigens and antibodies form 4 blood groups:
- Group 0 (I) - there are no group agglutinogens on red blood cells, alpha and beta agglutinins are present in the plasma.
- Group A (II) - red blood cells contain only agglutinogen A, agglutinin beta is present in the plasma;
- Group B (III) - red blood cells contain only agglutinogen B, plasma contains agglutinin alpha;
- Group AB (IV) - antigens A and B are present on red blood cells, plasma does not contain agglutinins.
Determination of blood groups is carried out by identifying specific antigens and antibodies (double method, or cross reaction).
Blood incompatibility is observed if the red blood cells of one blood carry agglutinogens (A or B), and the plasma of another blood contains the corresponding agglutinins (alpha or beta), and an agglutination reaction occurs.
Transfusion of red blood cells, plasma and especially whole blood from a donor to a recipient must be strictly observed in group compatibility. To avoid incompatibility between the blood of the donor and the recipient, it is necessary to accurately determine their blood groups using laboratory methods. It is best to transfuse blood, red blood cells and plasma of the same group as determined for the recipient. In emergency cases, group 0 red blood cells (but not whole blood!) can be transfused into recipients with other blood groups; Group A red blood cells can be transfused into recipients with blood group A and AB, and red blood cells from a group B donor can be transfused into group B and AB recipients.
Blood group compatibility cards (agglutination is indicated by a + sign):
| Donor blood | Recipient's blood | |||
| 0 (I) | A (II) | B (III) | AB (IV) | |
| 0(I) | — | + | + | + |
| A(II) | + | — | + | + |
| B(III) | + | + | — | + |
| AB (IV) | + | + | + | — |
| Donor's red blood cells | Recipient's blood | |||
| 0 (I) | A (II) | B (III) | AB (IV) | |
| 0(I) | — | — | — | — |
| A(II) | + | — | + | — |
| B(III) | + | + | — | — |
| AB (IV) | + | + | + | — |
Group agglutinogens are found in the stroma and membrane of erythrocytes. Antigens of the ABO system are detected not only on red blood cells, but also on cells of other tissues or can even be dissolved in saliva and other body fluids. They develop in the early stages of intrauterine development, and are already present in significant quantities in the newborn. The blood of newborn children has age-related characteristics - characteristic group agglutinins may not yet be present in the plasma, which begin to be produced later (constantly detected after 10 months) and the determination of the blood group in newborns in this case is carried out only by the presence of antigens of the ABO system.
In addition to situations involving the need for blood transfusion, determination of blood type, Rh factor, and the presence of alloimmune anti-erythrocyte antibodies should be carried out during planning or during pregnancy to identify the likelihood of an immunological conflict between mother and child, which can lead to hemolytic disease of the newborn.
Hemolytic disease of the newborn
Hemolytic jaundice of newborns, caused by an immunological conflict between mother and fetus due to incompatibility of erythrocyte antigens. The disease is caused by incompatibility of the fetus and mother for D-Rhesus or ABO antigens, less often there is incompatibility for other Rhesus (C, E, c, d, e) or M-, M-, Kell-, Duffy-, Kidd- antigens. Any of these antigens (usually D-Rh antigen), penetrating into the blood of a Rh-negative mother, causes the formation of specific antibodies in her body. The latter enter the fetal blood through the placenta, where they destroy the corresponding antigen-containing red blood cells. Predispose to the development of hemolytic disease of the newborn by impaired placental permeability, repeated pregnancies and blood transfusions to a woman without taking into account the Rh factor, etc. With early manifestations of the disease, an immunological conflict can cause premature birth or miscarriages.
There are varieties (weak variants) of antigen A (to a greater extent) and less frequently of antigen B. As for antigen A, there are options: “strong” A1 (more than 80%), weak A2 (less than 20%), and even weaker ones (A3 , A4, Ah - rarely). This theoretical concept is important for blood transfusion and can cause accidents when assigning donor A2 (II) to group 0 (I) or donor A2B (IV) to group B (III), since the weak form of antigen A sometimes causes errors in the determination blood groups of the ABO system. Correct identification of weak A antigen variants may require repeated testing with specific reagents.
A decrease or complete absence of natural agglutinins alpha and beta is sometimes noted in immunodeficiency states:
- neoplasms and blood diseases - Hodgkin's disease, multiple myeloma, chronic lymphatic leukemia;
- congenital hypo- and agammaglobulinemia;
- in young children and the elderly;
- immunosuppressive therapy;
- severe infections.
Difficulties in determining the blood group due to suppression of the hemagglutination reaction also arise after the introduction of plasma substitutes, blood transfusion, transplantation, septicemia, etc.
Inheritance of blood groups
The laws of inheritance of blood groups are based on the following concepts. At the ABO gene locus, there are three possible variants (alleles) - 0, A and B, which are expressed in an autosomal codominant manner. This means that individuals who have inherited genes A and B express the products of both of these genes, resulting in the AB (IV) phenotype. Phenotype A (II) can be present in a person who has inherited from parents either two genes A, or genes A and 0. Accordingly, phenotype B (III) - when inheriting either two genes B, or B and 0. Phenotype 0 (I) appears when inheritance of two genes 0. Thus, if both parents have blood group II (genotypes AA or A0), one of their children may have the first group (genotype 00). If one of the parents has blood type A(II) with a possible genotype AA and A0, and the other has B(III) with a possible genotype BB or B0, children can have blood groups 0(I), A(II), B(III) ) or AB (!V).
Indications for the purpose of analysis:
- Determination of transfusion compatibility;
- Hemolytic disease of newborns (detection of incompatibility between the blood of mother and fetus according to the AB0 system);
- Preoperative preparation;
- Pregnancy (preparation and follow-up of pregnant women with negative Rh factor)
Preparation for the study: not required
Material for the study: whole blood (with EDTA)
Determination method: Filtration of blood samples through a gel impregnated with monoclonal reagents - agglutination + gel filtration (cards, crossover method).
If necessary (detection of the A2 subtype), additional testing is carried out using specific reagents.
Execution time: 1 day
Research result:
- 0 (I) - first group,
- A (II) - second group,
- B (III) - third group,
- AB (IV) - fourth blood group.
When subtypes (weak variants) of group antigens are identified, the result is given with an appropriate comment, for example, “a weakened variant A2 has been identified, individual selection of blood is required.”
Rh factor Rh
The main surface erythrocyte antigen of the Rh system, by which a person’s Rh status is assessed.
Functions. Rh antigen is one of the erythrocyte antigens of the Rh system, located on the surface of erythrocytes. There are 5 main antigens in the Rh system. The main (most immunogenic) antigen is Rh (D), which is usually referred to as the Rh factor. The red blood cells of approximately 85% of people carry this protein, so they are classified as Rh positive (positive). 15% of people do not have it and are Rh negative (Rh negative). The presence of the Rh factor does not depend on group membership according to the AB0 system, does not change throughout life, and does not depend on external reasons. It appears in the early stages of intrauterine development, and is already found in a significant amount in the newborn. Determination of Rh blood is used in general clinical practice during transfusion of blood and its components, as well as in gynecology and obstetrics when planning and managing pregnancy.
Incompatibility of blood according to the Rh factor (Rh conflict) during blood transfusion is observed if the donor's red blood cells carry Rh agglutinogen, and the recipient is Rh negative. In this case, the Rh-negative recipient begins to produce antibodies directed against the Rh antigen, leading to the destruction of red blood cells. Transfusions of red blood cells, plasma, and especially whole blood from a donor to a recipient must strictly observe compatibility not only by blood type, but also by Rh factor. The presence and titer of antibodies to the Rh factor and other alloimmune antibodies already present in the blood can be determined by specifying the “anti-Rh (titer)” test.
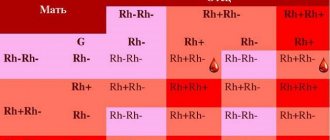
Determination of blood type, Rh factor, and the presence of alloimmune anti-erythrocyte antibodies should be carried out when planning or during pregnancy to identify the likelihood of an immunological conflict between mother and child, which can lead to hemolytic disease of the newborn. The occurrence of Rh conflict and the development of hemolytic disease of newborns is possible if the pregnant woman is Rh negative and the fetus is Rh positive. If the mother is Rh + and the fetus is Rh negative, there is no danger of hemolytic disease for the fetus.
Hemolytic disease of the fetus and newborns is hemolytic jaundice of newborns, caused by an immunological conflict between mother and fetus due to incompatibility of erythrocyte antigens. The disease can be caused by incompatibility of the fetus and mother for D-Rhesus or ABO antigens, less often there is incompatibility for other Rhesus (C, E, c, d, e) or M-, N-, Kell-, Duffy-, Kidd antigens (according to statistics, 98% of cases of hemolytic disease of newborns are associated with D - Rh antigen). Any of these antigens, penetrating the blood of a Rh-negative mother, causes the formation of specific antibodies in her body. The latter enter the fetal blood through the placenta, where they destroy the corresponding antigen-containing red blood cells. Predisposition to the development of hemolytic disease of newborns is impaired placental permeability, repeated pregnancies and blood transfusions to a woman without taking into account the Rh factor, etc. With early manifestations of the disease, an immunological conflict can cause premature birth or repeated miscarriages.
Currently, there is a possibility of medical prevention of the development of Rh conflict and hemolytic disease of newborns. All Rh-negative women during pregnancy should be under medical supervision. It is also necessary to monitor the level of Rh antibodies over time.
There is a small category of Rh-positive individuals who are able to form anti-Rh antibodies. These are individuals whose red blood cells are characterized by significantly reduced expression of the normal Rh antigen on the membrane (“weak” D, Dweak) or expression of an altered Rh antigen (partial D, Dpartial). In laboratory practice, these weak variants of the D antigen are combined into the Du group, the frequency of which is about 1%.
Recipients containing Du antigen should be classified as Rh-negative and should be transfused only with Rh-negative blood, since normal D antigen can cause an immune response in such individuals. Donors with the Du antigen qualify as Rh-positive donors, since transfusion of their blood can cause an immune response in Rh-negative recipients, and in the case of previous sensitization to the D antigen, severe transfusion reactions.
Inheritance of the Rh blood factor.
The laws of inheritance are based on the following concepts. The gene encoding the Rh factor D (Rh) is dominant, the allelic gene d is recessive (Rh-positive people can have the DD or Dd genotype, Rh-negative people can only have the dd genotype). A person receives 1 gene from each parent - D or d, and thus has 3 genotype options - DD, Dd or dd. In the first two cases (DD and Dd), a blood test for Rh factor will give a positive result. Only with the dd genotype will a person have Rh negative blood.
Let's consider some variants of the combination of genes that determine the presence of the Rh factor in parents and children
- 1) The father is Rh positive (homozygote, genotype DD), the mother is Rh negative (genotype dd). In this case, all children will be Rh positive (100% probability).
- 2) Father is Rh positive (heterozygote, genotype Dd), mother is Rh negative (genotype dd). In this case, the probability of having a child with negative or positive Rh is the same and equal to 50%.
- 3) The father and mother are heterozygotes for this gene (Dd), both are Rh positive. In this case, it is possible (with a probability of about 25%) to give birth to a child with negative Rh.
Indications for the purpose of analysis:
- Determination of transfusion compatibility;
- Hemolytic disease of newborns (detection of incompatibility between the blood of mother and fetus according to the Rh factor);
- Preoperative preparation;
- Pregnancy (prevention of Rh conflict).
Preparation for the study: not required. Material for research: whole blood (with EDTA)
Determination method: Filtration of blood samples through a gel impregnated with monoclonal reagents - agglutination + gel filtration (cards, crossover method).
Execution time: 1 day
Interpretation of results:
The result is given in the form: Rh + positive Rh - negative When weak subtypes of antigen D (Du) are detected, a comment is given: “a weak Rh antigen (Du) has been detected, it is recommended to transfuse Rh-negative blood if necessary.”
Anti-Rh (alloimmune antibodies to the Rh factor and other erythrocyte antigens)
Antibodies to the clinically most important erythrocyte antigens, primarily the Rh factor, indicating the body's sensitization to these antigens.
Functions. Rh antibodies belong to the so-called alloimmune antibodies. Alloimmune anti-erythrocyte antibodies (to the Rh factor or other erythrocyte antigens) appear in the blood under special conditions - after a transfusion of immunologically incompatible donor blood or during pregnancy, when fetal red blood cells carrying paternal antigens that are immunologically foreign to the mother penetrate through the placenta into the woman’s blood. Non-immune Rh-negative people do not have antibodies to the Rh factor. In the Rh system, there are 5 main antigens, the main (most immunogenic) is antigen D (Rh), which is usually referred to as the Rh factor. In addition to the Rh system antigens, there are a number of clinically important erythrocyte antigens to which sensitization can occur, causing complications during blood transfusion. The method of screening blood for the presence of alloimmune anti-erythrocyte antibodies, used in INVITRO, allows, in addition to antibodies to the Rh factor RH1(D), to detect alloimmune antibodies to other erythrocyte antigens in the test serum.
The gene encoding the Rh factor D (Rh) is dominant, the allelic gene d is recessive (Rh-positive people can have the DD or Dd genotype, Rh-negative people can only have the dd genotype). During pregnancy of a Rh-negative woman with a Rh-positive fetus, the development of an immunological conflict between mother and fetus due to the Rh factor is possible. Rh conflict can lead to miscarriage or the development of hemolytic disease of the fetus and newborns. Therefore, determination of blood type, Rh factor, as well as the presence of alloimmune anti-erythrocyte antibodies should be carried out when planning or during pregnancy to identify the likelihood of an immunological conflict between mother and child. The occurrence of Rh conflict and the development of hemolytic disease of newborns is possible if the pregnant woman is Rh negative and the fetus is Rh positive. If the mother has a positive Rh antigen and the fetus is negative, a conflict regarding the Rh factor does not develop. The incidence of Rh incompatibility is 1 case in 200-250 births.
Hemolytic disease of the fetus and newborns is hemolytic jaundice of newborns, caused by an immunological conflict between mother and fetus due to incompatibility of erythrocyte antigens. The disease is caused by incompatibility of the fetus and mother for D-Rhesus or ABO (group) antigens, less often there is incompatibility for other Rhesus (C, E, c, d, e) or M-, M-, Kell-, Duffy- , Kidd antigens. Any of these antigens (usually D-Rh antigen), penetrating into the blood of a Rh-negative mother, causes the formation of specific antibodies in her body. The penetration of antigens into the maternal bloodstream is facilitated by infectious factors that increase the permeability of the placenta, minor injuries, hemorrhages and other damage to the placenta. The latter enter the fetal blood through the placenta, where they destroy the corresponding antigen-containing red blood cells. Predisposition to the development of hemolytic disease of newborns is impaired placental permeability, repeated pregnancies and blood transfusions to a woman without taking into account the Rh factor, etc. With early manifestations of the disease, an immunological conflict can cause premature birth or miscarriages.
During the first pregnancy with an Rh-positive fetus, a pregnant woman with Rh “-” has a 10-15% risk of developing an Rh conflict. The first meeting of the mother's body with a foreign antigen occurs, the accumulation of antibodies occurs gradually, starting from approximately 7-8 weeks of pregnancy. The risk of incompatibility increases with each subsequent pregnancy with a Rh-positive fetus, regardless of how it ended (induced abortion, miscarriage or childbirth, surgery for an ectopic pregnancy), with bleeding during the first pregnancy, with manual separation of the placenta, and also if childbirth is carried out by caesarean section or accompanied by significant blood loss. with transfusions of Rh-positive blood (if they were carried out even in childhood). If a subsequent pregnancy develops with an Rh-negative fetus, incompatibility does not develop.
All pregnant women with Rh “-” are placed on special registration in the antenatal clinic and dynamic monitoring of the level of Rh antibodies is carried out. For the first time, an antibody test must be taken from the 8th to the 20th week of pregnancy, and then periodically check the antibody titer: once a month until the 30th week of pregnancy, twice a month until the 36th week and once a week until the 36th week. Termination of pregnancy at less than 6-7 weeks may not lead to the formation of Rh antibodies in the mother. In this case, during a subsequent pregnancy, if the fetus has a positive Rh factor, the probability of developing immunological incompatibility will again be 10-15%.
Testing for alloimmune anti-erythrocyte antibodies is also important in general preoperative preparation, especially for people who have previously received blood transfusions.
Indications for the purpose of analysis:
- Pregnancy (prevention of Rh conflict);
- Monitoring of pregnant women with negative Rh factor;
- Miscarriage;
- Hemolytic disease of newborns;
- Preparation for blood transfusion.
Preparation for the study: not required. Material for research: whole blood (with EDTA) Determination method: agglutination + gel filtration method (cards). Incubation of standard typed erythrocytes with the test serum and filtration by centrifugation of the mixture through a gel impregnated with a polyspecific antiglobilin reagent. Agglutinated red blood cells are detected on the surface of the gel or in its thickness.
The method uses suspensions of erythrocytes from group 0(1) donors, typed according to erythrocyte antigens RH1(D), RH2(C), RH8(Cw), RH3(E), RH4(c), RH5(e), KEL1( K), KEL2(k), FY1(Fy a) FY2(Fy b), JK (Jk a), JK2(Jk b), LU1 (Lu a), LU2 (LU b), LE1 (LE a), LE2 (LE b), MNS1(M), MNS2 (N), MNS3 (S), MNS4(s), P1 (P).
Execution time: 1 day
When alloimmune anti-erythrocyte antibodies are detected, their semi-quantitative determination is carried out. The result is given in titers (the maximum dilution of the serum at which a positive result is still detected).
Units of measurement and conversion factors: U/ml
Reference values: negative.
Positive result: Sensitization to Rh antigen or other erythrocyte antigens.
Prevention of antibodies
The most effective method of preventing the appearance of antibodies to the D protein is considered to be the administration of anti-Rh (D) immunoglobulin to the expectant mother. The drug allows you to block the antigenic areas of Rh-positive red blood cells, preventing the appearance of new ones. When passive antibodies are introduced, their excess appears, which leads to the suppression of their occurrence in the body.
Family planning is of primary importance in preventing incompatibility. A negative Rh factor does not pose any threat to conceiving a child. When planning maternity, you need to determine the indicators of the woman and her spouse. Before conception, it is necessary to carry out a study for the presence of Rh antibodies in the woman’s blood. When pregnancy occurs, you must register as early as possible and strictly follow all doctor’s instructions.
Healing procedures
Blood diseases in infants require comprehensive, thorough treatment to avoid unpleasant and untreatable complications. The more pronounced the signs, the more noticeable the conflict of blood groups, to establish which an analysis is carried out for an increased amount of bilirubin.
The essence of the treatment procedures is to eliminate antibodies, affected red blood cells and excess bilirubin in the child’s blood. For this purpose, phototherapy and other treatment methods are used that are aimed at eliminating symptoms. In situations where this does not bring results, or the amount of bilirubin in the blood increases too rapidly, a blood transfusion is performed.
Manifestations of group conflict, its treatment and prevention
While pregnant, there may be no signs of blood group conflict. The baby can be absolutely healthy until the moment of birth, when the placental barrier disappears and the mother’s blood enters the baby’s circulatory system.
A blood test is taken from the newborn to see if there is any group conflict. If it is present, the child will have severe anemia - a low level of hemoglobin in the blood.
The baby may also develop hemolytic jaundice. Unlike physiological jaundice, which appears a few days after birth, is safe and goes away on its own, hemolytic jaundice is a pathological condition. The baby may be born immediately with yellow skin, or may turn yellow a little later. Even the whites of a baby's eyes can turn yellow. This is caused by a huge excess of bilirubin in the blood, which puts a tremendous burden on the baby's liver.