Acute myeloid leukemia In everyday life, we often hear about cancer, in particular about blood cancer. One of these is acute myeloblastic leukemia (AML) or acute leukemia, which is commonly referred to as blood cancer or leukemia. The complexity of AML, firstly, is that in the initial stages there are no obvious signs of the disease. Secondly, the treatment process itself is very difficult, both from a medical point of view and emotionally for patients.
So, let's figure out what it is - acute myeloblastic leukemia, what is the cause, how is it treated, what are the prognosis for cure, can it be cured and what does it depend on.
What is chronic myeloid leukemia?
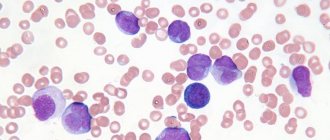
Blood smear of a patient with chronic myeloid leukemia
Chronic myeloid leukemia (CML) is a malignant neoplasm of hematopoietic tissue, accompanied by the progressive proliferation of immature granulocytes. The disease initially has a sluggish nature, gradually flowing into the stage of exacerbation with severe symptoms and the formation of systemic disorders. It is one of the most dangerous and disabling diseases.
CML is the first cancer in which a relationship between the development of carcinogenesis and a mutation in the gene has been identified. The characteristic anomaly is based on the translocation of chromosomes 9 and 22, that is, sections of these chromosomes change places, forming an aberrant chromosome. A mutated chromosome was identified by researchers from Philadelphia, so it was called the Philadelphia or Ph chromosome.
The study of the Ph chromosome and its influence made it possible to develop a new drug for suppressing oncological processes, thanks to which the life expectancy of patients has significantly increased. However, the disease still remains incurable. The number of primary CML is diagnosed in 1.5:100,000 of the population per year, the peak incidence occurs at the age of 30-50 years, 30% of CML is detected in people over 60 years of age, in children the disease is diagnosed in less than 5% of cases.
Reasons for development
Pesticides have a negative effect on hematopoiesis
The disease has been known to science since 1811, but until now the factors that provoke the mutation in the gene have not been determined. There are a number of reasons contributing to the development of pathology:
- radioactive exposure, including during radiation therapy;
- chemotherapy of other oncological diseases;
- a number of genetic diseases characterized by a chromosomal abnormality (for example, Down syndrome);
- interaction with chemical compounds (petroleum products, pesticides).
Pathogenesis of chronic myeloid leukemia
Pathogenesis of chronic myeloid leukemia
The BCR-ABL 1 hybrid gene, formed as a result of chromosome translocation, produces the synthesis of the BCR-ABL protein. This protein is a tyrosine kinase, which normally contributes to the transmission of signal impulses for cell growth. The tyrosine kinase created by mutation becomes an active factor in cell proliferation; they begin to divide and spread independently of growth factors. The process of creating clones of the mutated cell occurs.
Uncontrolled division is accompanied by a violation of apoptosis - programmed cell death. Also, the hybrid tyrosine kinase suppresses the natural repair functions in DNA molecules, creating the prerequisites for subsequent mutations, which aggravates the pathological process.
Proliferating cells are immature, blast precursors of full-fledged blood elements. Gradually, blast cells replace functional red blood cells, platelets and leukocytes. Abnormalities are added to other chromosomes, which triggers an accelerated process of destruction of the body as a whole.
Stages of chronic myeloid leukemia
Blast crisis is one of the stages of myeloid leukemia
- Chronic - <15% blast cells. Usually the stage lasts several years. Signs of the disease are often detected only in the results of a general blood test. CML is detected at this stage in more than 80% of patients. The mutated cell is still controlled by the BCR-ABL gene, the ability to differentiate is preserved, and healthy cells function naturally.
- Progressive (acceleration) - 15 - 29% of blast cells. The accelerated process of proliferation of immature cells reduces the median life expectancy to a year. Thrombocytopenia develops, the number of leukocytes increases, and signs of resistance to therapy appear. At this stage, pathology is detected in 10-12% of patients. Tumor cells begin to suppress healthy ones, lose contact with the microenvironment, and actively move from the bone marrow into the bloodstream. Subsequent mutations in chromosomes begin to occur.
- Blast crisis - > 30% blast cells. The stage is characterized by the aggressive nature of the mutated cells, the patient’s condition deteriorates sharply. Additional anomalies both in the BCR-ABL gene and in the genome as a whole provoke a chain of pathological reactions that are practically untreatable. At this stage, the tissues of internal organs, skin and mucous membranes may be affected, myeloid cells transform into sarcoma.
Chronic form of the disease
The manifestation of symptoms of a blood tumor process depends on the form of the disease. The most common form is chronic myeloid leukemia. This condition is malignant.
Chronic myeloid leukemia – what is it? This is a condition that occurs when an abnormal gene appears in the body that affects blood cells. The location of the gene is the bone marrow. With the blood flow, pathological cells spread throughout all organs.
The disease does not have an acute onset and a clear clinical picture. It is characterized by a slow flow. The danger is that this form of the disease can go into the acute phase at any time, which can be fatal for the patient.
Myeloid leukemia has several stages of development:
- chronic;
- acceleration stage;
- terminal stage.
Symptoms and signs
Hemorrhagic syndrome
Signs of CML become noticeable closer to the progressive stage.
- Symptoms of tumor intoxication: weight loss, fatigue, wave-like increase in temperature, skin itching, nausea, joint pain.
- Symptoms of tumor proliferation are enlarged spleen and liver, pain in the left hypochondrium, skin lesions.
- Anemic syndrome - dizziness, severe pallor, rapid heartbeat, feeling of lack of air.
- Hemorrhagic syndrome - a tendency to bleeding of the mucous membranes, a rash in the form of red dots, prolonged bleeding with minor cuts.
Primary symptoms of leukemia in children
In the vast majority of cases, the acute form of leukemia begins as a common childhood cold. The child may have a cough and runny nose, but more often it is simply weakness, drowsiness, decreased activity, refusal to eat and play, poor weight gain, and growth retardation.
The average daily temperature for leukemia in children, as a rule, rises to low-grade fever, which also gives parents reason to assume a banal acute respiratory infection, acute respiratory viral infection or acute intestinal infection. Such nonspecific symptoms of leukemia in children lead to adults self-medicating the child instead of carrying out a differentiated diagnosis as soon as possible and identifying a dangerous pathology.
For the sake of fairness, it is worth noting that even a timely visit to a pediatrician or family doctor does not guarantee that he will suspect the presence of blood cancer in his ward and refer him to a hematologist or oncologist for a detailed examination. Sometimes parents must be persistent and demand the right direction. Especially if, in addition to those described above, other signs of the disease are observed.
More clear symptoms of leukemia in children are the following:
- hemorrhagic syndrome, expressed in hemorrhages under the skin and mucous membranes;
- signs of intoxication of the body - nausea, vomiting, abnormally intense sweating, especially at night and immediately after waking up, dizziness and headaches, non-healing abrasions and minor wounds;
- change in color of the skin and mucous membranes from pink to white, yellowish or grayish;
- the appearance of diseases such as stomatitis, gingivitis, tonsillitis;
- painless enlargement of the lymph nodes, not accompanied by a change in the color of the skin over them;
- changes in the salivary glands;
- the appearance of blood in the urine, nasal and various internal bleeding, bleeding gums.
Symptoms of acute leukemia in children also include pain in the spine, bones, and joints. With enlargement of the liver and spleen, unpleasant sensations may appear in the area where these organs are located.
Diagnosis of the disease
One of the methods for diagnosing the disease is x-ray
Diagnosis of CML includes:
- Initial examination of the patient with the study of anamnesis, complaints, as well as examination by palpation of the size of the spleen and liver.
- A general blood test reveals the number and characteristics of blood cells.
- Biochemical analysis is carried out to determine the level of bilirubin, electrolytes, glucose, LDH, AST, ALT.
- Histological examination of the bone marrow reveals accumulations of blast cells.
- Cytogenetic analysis reveals chromosome translocation.
- At stage 3, immunophenotyping is performed to identify blast cells.
- The gene sequencing method is used to identify gene mutations.
- An ultrasound scan of internal organs is performed, primarily the spleen and liver.
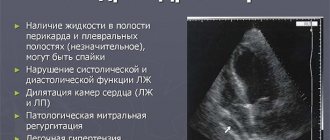
- Additionally, chest X-ray, ECG, echocardiography, ELISA for markers of various diseases, coagulogram and other studies are prescribed.
Symptoms in relation to prognosis
The pathology has many clinical manifestations. However, there are no specific symptoms as such. This aggravates the situation, since late diagnosis does not allow us to talk about recovery. Symptoms directly depend on the age and at what stage of the cancer process the pathology was detected.
In most cases, patients complain that they are bothered by an increase in temperature parameters and persistent pain impulses in the bones. In addition, there are:
- increasing weakness and increased fatigue;
- the skin becomes cyanotic;
- there is practically no appetite;
- severe shortness of breath develops;
- dyspeptic disorders - nausea, vomiting, alternation of constipation with diarrhea, increased flatulence;
- unpleasant discomfort, heaviness in the hypochondrium;
- increased parameters of the spleen and liver;
- pain impulses in all groups of joints.
All of the above undermines a person’s reserves of strength, he lacks the desire to fight the tumor, and survival times are reduced many times over. And since, against the background of damage to blood germs, the number of platelets also decreases sharply, cancer patients will have a tendency to prolonged bleeding, up to a diffuse variant, leading to death.
Such varied symptoms are due to the fact that all tissues and organs receive blood with mutated cells contained in it. They infiltrate into healthy tissues, followed by the formation of multiple tumor foci.
Modern diagnostic methods help put everything in its place and carry out adequate differential diagnosis, as well as decide whether myeloblastic leukemia can be cured.
Treatment
The mainstay of treatment is tyrosine kinase inhibitors
CML therapy is currently based on the use of tyrosine kinase inhibitors. The first generation drug imatinib blocks the activity of the hybrid tyrosine kinase, penetrating into the “pocket” of the BCR-ABL protein. The creation of imatinib made a breakthrough in the treatment of CML due to its effectiveness. However, patients often develop resistance to the drug, which led to the creation of second-generation inhibitors. Combination with other treatment methods allows achieving high levels of improvement in quality and life expectancy.
The choice of drug and dose are determined depending on the stage of CML and the risk of side effects. Typically, treatment begins with imatinib at a dosage of 400 mg/day in the initial stage, 600 mg/day in subsequent stages, and then the dose can be increased or decreased. Various aberrations in genes cause low sensitivity to drugs, so the patient can change one inhibitor to another.
Bone marrow transplantation
If therapy does not have an effect, allogeneic bone marrow transplantation is recommended. New stem cells can produce healthy elements of the circulatory system. But the operation is associated with a number of high risks.
Therapy with interferon drugs is usually prescribed in the 1st stage of CML, as it is not effective in subsequent stages.
To reduce the tumor mass and if treatment with inhibitors fails, chemotherapy is performed. In the blast crisis stage, polychemotherapy is used similar to the treatment of acute leukemia.
Radiation therapy may be prescribed in cases of severe splenomegaly. If there is a risk of splenic rupture, a splenectomy is performed.
Today, research continues to create an even more advanced drug. Russian scientists, with the help of the Skolkovo Foundation, are conducting clinical trials of a third-generation inhibitor, which should surpass the previous ones in its effectiveness.
What's the forecast?
Pathology can successfully disguise itself as many other diseases, which makes its timely detection very difficult. And this, of course, worsens the prognosis for the life of a cancer patient.
Acute myeloid leukemia and the prognosis of life with it are influenced by practically uncontrollable factors such as the age of the cancer patient and the stage at which the disease was detected.
This type of pathology never goes away on its own. But adequate treatment measures can significantly prolong a person’s life, as well as significantly improve the prognosis.
Additional prognostically unfavorable factors include the following:
- formed splenomegaly;
- failure in the activity of central nervous system structures;
- multiple lesions of lymph nodes;
- patient's age category is more than 65-75 years;
- significant depression of blood parameters;
- the person has other cancer pathologies;
- lack of a positive reaction to the ongoing treatment measures.
No oncologist can give an accurate prognosis of life expectancy with diagnosed myeloblastic leukemia. Malignant lesions of the hematopoietic system are quite unpredictable. They can recur even with established long-term remission.
Prevention and prognosis
The prognosis of the disease is determined by the doctor
The cause of the formation of CML has not been established, so prevention includes measures to avoid contact with carcinogenic substances and exposure to radioactive radiation.
The prognosis is determined by the stage and severity of the disease. One of the prognostic models (Kantarjian HM) includes factors:
- advanced age of the patient at diagnosis;
- concentration of blast cells in the blood ≥ 3%, in the bone marrow ≥ 5%;
- basophil concentration ≥ 7%;
- platelet concentration ≥ 700*10 9/l;
- severe splenomegaly.
This model is designed for the initial phase of CML, if ≥ 3 signs are present, the prognosis is unfavorable, subsequent phases are considered “always unfavorable”. However, each case of CML is individual; patients with a life expectancy of more than 30 years are known in the chronic stage. On average, with timely treatment with tyrosine kinase inhibitors, 70-80% of patients live more than 10 years. When the disease moves into a progressive phase, survival rate decreases by 3-4 times; with a blast crisis, it is still up to 6 months.