What it is
A defect of the mitral valve with reverse blood flow (regurgitation) from the left ventricle into the atrium as a result of incomplete closure of the valves is called mitral regurgitation. In its independent form, the acquired disease is rare and for a long time is benign in nature.
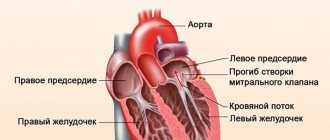
But as part of combined and concomitant defects, it is detected in half of all cases of cardiac defects and quickly leads to serious complications. Normally, the left ventricle ejects its contents into the aorta during systole, which branches, forming a systemic circulation. In this way, nutrients and oxygen are transferred to organs, including the myocardium. Under pressure, the butterfly valve closes and does not allow reverse movement. If there is a hole during contraction, regurgitation occurs, and some of the blood returns, stretching the left atrium. As the condition progresses, there is a steady increase in the volume of the heart cavities, increased pressure, and congestion in the blood vessels of the lungs.
The mechanism of defect formation can be seen in the figure:
Causes
In children, this pathology is common and is congenital and acquired. The main reasons affecting the intrauterine development of mitral type heart failure:
- Radiation exposure of the mother's body;
- Exposure of a woman’s body during pregnancy to increased doses of x-ray radiation;
- Presence of infectious diseases in a pregnant woman (sepsis, brucellosis, tonsillitis, syphilis);
- Hereditary factor;
- Genetic diseases accompanied by connective tissue abnormalities (Ehlers-Danlos, Marfan syndromes, etc.) and congenital pathologies.
Many genetically determined heart defects can either be inherited or occur spontaneously for unknown reasons.
Factors influencing the development of this disease in a child after birth:
- Consequences of surgery (heart surgery);
- Previous endocarditis of septic or rheumatoid etiology;
- Consequences of valvulitis (inflammatory process in one or more heart valves);
- Consequences of a heart injury with rupture (tear) of the valve leaflets.
Factors lead to organic damage (changes) to the mitral valve leaflets, which causes insufficiency of varying degrees. In addition, there are a number of reasons that lead to functional insufficiency of the valve, but do not cause damage to it. Such reasons include:
- Damage or death of areas of the heart muscles surrounding the valve and responsible for its movement;
- Ruptures of the connective tissues that attach the papillary muscles;
- Divergence of the valve leaflets as a result of expansion of the fibrous ring to which the walls are attached;
- Tumor.
The same reasons can cause defects of the aortic, tricuspid and pulmonary valves.
Causes
The formation of a defect can occur in the prenatal period, in which case it is considered congenital. The causes of this pathology may be:
- alcoholism, drug use and maternal smoking during pregnancy;
- ionizing radiation;
- poisoning and taking certain drugs (antibiotics, non-steroidal anti-inflammatory drugs);
- systemic and infectious diseases.
The etiological factors of acquired deviation are usually:
- streptococcal and staphylococcal infections with the development of septic endocarditis;
- autoimmune diseases (lupus, multiple sclerosis);
- myocardial damage as a result of a heart attack;
- mitral valve prolapse;
- Marfan syndrome;
- chest injuries with rupture of the valves or fibers that hold them.
Relative mitral valve insufficiency is observed with pronounced enlargement of the left ventricle. The cause of this condition may be dilated cardiomyopathy, aortic valve disease, myocarditis and hypertension.
Signs of mitral and aortic valve insufficiency
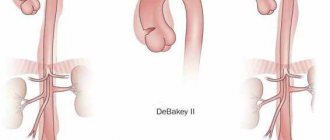
Acute aortic insufficiency is formed when a dissecting aneurysm occurs, and mitral insufficiency occurs when parts of the valve or the connective tissue cords that hold them are torn off. They are accompanied by a rapid increase in congestion and pulmonary edema, a drop in pressure with a fatal outcome.
Chronic valve failure occurs initially without symptoms. This condition can last up to several years. Signs of progression of mitral and aortic pathology:
- increased pulsation of the vessels of the neck and head,
- intense beats and tremors in the heart,
- tachycardia,
- headache,
- dizziness,
- decreased vision.
Then, as the degree of blood reflux increases, pain in the heart, rhythm disturbances, and difficulty breathing appear.
A sign of decompensation is the addition of right ventricular failure - edema, enlarged liver, swollen neck veins, episodes of cardiac asthma.
Watch the video about aortic valve insufficiency:
Symptoms
At the initial stage of the disease there are no clinical signs. The problem can only be identified during an instrumental examination of the heart. The prognosis depends on the size of the hole through which blood returns to the left atrium. In those who are unlucky, congestion occurs in the pulmonary vessels, and signs of ischemia of the myocardium and other organs appear. Such a patient usually presents the following complaints:
- lack of air during exercise, and then at rest;
- cardiac asthma;
- fatigue when performing normal activities;
- cough that gets worse when lying down;
- the appearance of sputum with blood;
- pastiness or swelling of the legs;
- pain on the left side of the chest;
- increased heart rate, atrial fibrillation;
- hoarseness (as a result of compression of the laryngeal nerve by the dilated pulmonary trunk or left atrium);
- heaviness in the right hypochondrium due to liver enlargement.
When examining such a patient, I try to note the presence of the following signs of mitral regurgitation:
- acrocyanosis (blue discoloration of the limbs and tip of the nose, ears) against a background of general pallor;
- bulging veins in the neck;
- trembling of the chest during palpation, determination of the cardiac impulse and pulsation in the epigastrium;
- upon percussion, an increase in the boundaries of cardiac dullness is noted;
- during auscultation – weakening of the first tone, intensification and splitting of the second tone, noise during systole.
Degrees of deficiency
Degrees of mitral insufficiency:
- First (I). The reverse blood flow does not exceed 25%, the person’s condition is characterized as satisfactory. Hypertrophy of the heart muscle (left sections) is observed, which helps to temporarily compensate for the deficiency. For some time, this mechanism allows you to restrain the increase in pressure in the small circle. There are no symptoms.
- Second (subcompensated, II). The reflux rate is 50%, and congestion develops in the lungs. The first signs of the disease appear.
- Third (decompensated, III). Blood return increases to 60–90% of the total volume. High load on the right ventricle leads to its dilatation. Acute grade 3 mitral valve insufficiency can cause pulmonary edema.
Symptoms
The most typical complaint is shortness of breath, which occurs with moderate and severe chronic mitral regurgitation and the clinic of acute left ventricular failure with acute mitral regurgitation. The presence of atrial fibrillation before surgery is an independent predictor of reduced long-term survival after mitral valve surgery for chronic mitral regurgitation.
Diagnostics
You can identify the problem using the following methods:
- ECG. It will show signs of hypertrophy of the left myocardium, and later of the right ventricle. Sometimes it is possible to detect tachycardia and rhythm disturbances.
- Plain radiography of the chest. On it you can see an increase in the left sections, displacement of the esophagus, and in later stages - hypertrophy of the right ventricle. Congestion in the lungs is manifested by dilation of blood vessels and blurred outlines.
- Phonocardiogram. A very informative examination, in which it is possible to determine all the noise produced by the heart muscle. A sign of the disease will be a decrease in the sound of ventricular contraction, systolic murmur, and a click of the valves closing.
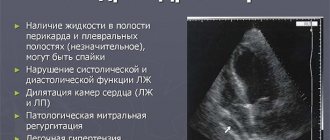
- The disorder is confirmed by echocardiography. The ultrasound method reveals enlargement of the heart chambers and incomplete closure of the mitral orifice.
Types, forms, stages
With NMC, the total stroke volume of the blood of the left ventricle is assessed . Depending on its quantity, the disease is divided into 4 degrees of severity (the percentage indicates the part of the blood that is redistributed incorrectly):
- I (the softest) - up to 20%.
- II (moderate) - 20-40%.
- III (medium form) - 40-60%.
- IV (the heaviest) - over 60%.
According to the forms of its course, the disease can be divided into acute and chronic:
When determining the characteristics of movement of the mitral leaflets, 3 types of pathology classification :
- 1 - standard level of mobility of the leaflets (in this case, painful manifestations consist of dilatation of the fibrous ring, perforation of the leaflets).
- 2 - destruction of the valves (the chords take the greatest damage, as they are stretched or ruptured, and a violation of the integrity of the papillary muscles also occurs.
- 3 - decreased mobility of the valves (forced connection of commissures, reduction in the length of the chords, as well as their fusion).
Treatment methods
Treatment of mitral valve insufficiency at the compensation stage consists of constant monitoring of the patient, reducing physical activity and using medications to prevent the progression of the disease. If complications arise and there is no way to solve the problem surgically, symptomatic therapy is used:
- cardiac glycosides;
- diuretics;
- beta blockers;
- calcium antagonists;
- ACE inhibitors;
- anticoagulants and antiplatelet agents.
No drugs can cure the disease. Conservative methods only help to temporarily delay deterioration and improve the quality of life. The only way to fix the problem is to perform an operation.
Surgical interventions: indications and techniques
The indication for surgical treatment is a gross violation of the structure of the valves, leading to a pronounced deviation of hemodynamics. Valve restoration or replacement is required in the following cases:
- history of endocarditis;
- first manifestations of heart failure (shortness of breath, swelling);
- rhythm disturbances;
- frequent severe pain in the chest, signs of congestion in the pulmonary system.
You cannot operate in the following cases:
- onset of an acute disease or exacerbation of a chronic one;
- stroke or heart attack;
- heat;
- extreme degree of heart failure.
The main types of interventions are complete replacement or valve repair. The second option is carried out in the following ways:
- annuloplasty using soft or hard rings;
- valve resection;
- replacement of chords with artificial materials;
- edge-to-edge technique.
Features of the course of mitral valve insufficiency of the 2nd degree
With mitral valve insufficiency of the 2nd degree, the formation of a passive form of venous pulmonary hypertension manifests itself. The following symptoms are characteristic of this stage:
- Tachycardia that occurs at rest and during physical activity;
- Dyspnea;
- Attacks of cardiac asthma and cough;
- Hemoptysis.
During studies, expansion of the borders of the heart to the right (usually no more than 0.5 cm), to the left (from 1 to 2 cm), and also upward is usually diagnosed. In addition, the ECG reveals changes in the atrial component, as well as the presence of systolic murmurs.
Types and features of mitral prostheses
Cardiac surgeons use three types of prostheses:
- Mechanical ones, which were initially made in the shape of a ball, and a little later - in the form of hinges. Blood clots often form on them, and installation may be complicated by embolism. The patient has to constantly take antiplatelet drugs. The most modern are products that are processed with a biologically intact titanium alloy.
- Biological. They are created from pericardium or other natural tissues. They do not have the ability to form blood clots.
- Allografts are taken from a corpse and cryopreserved before being implanted into a suitable donor.
Case study: advanced mitral regurgitation
I would like to give an example of a clinical case in which the lack of timely treatment led to such a diagnosis - mitral regurgitation of the 3rd degree. A patient was admitted to the hospital with complaints of severe shortness of breath at rest, worsening with physical activity, cough with sputum, which sometimes contains streaks of blood, weakness, and swelling.
He considers himself unhealthy for many years, often suffered from sore throats, and had joint problems. The deterioration occurred after suffering from acute respiratory viral infection. When listening to the lungs, fine bubbling rales are detected, a weakening of the apical impulse, a click of the opening of the mitral valve, and systolic murmur are observed. The liver is enlarged, the lower edge is determined 5 cm below the hypochondrium. EchoCG shows thickening of the valve leaflets, calcification, dilatation of the left atrium, grade III mitral valve regurgitation.
The patient is scheduled for prosthetic surgery, after which he can be saved. Get treatment on time!
How to live with mitral regurgitation
At the initial stage, when there are no circulatory problems, the patient can simply lead a normal healthy lifestyle. Strong psycho-emotional shocks and heavy physical labor in unfavorable conditions are contraindicated for him. When the first signs of abnormality develop, we recommend:
- transition to easier work;
- for young people – learning a new profession;
- mental activity is not limited;
- service in the army is determined by a commission; most often the conscript is sent to the communications and radio engineering departments.
In case of edema, enlarged liver, ascites, severe shortness of breath and arrhythmia, a person must undergo a commission where he may be assigned a disability with the possibility of partial work or complete exemption from it. In this case, the conscript is considered unfit for service.