Description of left ventricular failure
The ventricle, located in the left half of the pumping organ, has a thick muscular wall that allows it to supply blood to the entire body. During diastole, blood from the pulmonary artery enters the left atrium and then fills the left ventricle. Its task is to completely push the oxygen-enriched biological fluid into the aorta (the largest artery) at the moment of systole.
If the myocardium of the left ventricle for any reason loses its contractility, venous blood stagnates in the pulmonary circulatory system (pulmonary circulation), resulting in pulmonary edema. Ineffective blood pumping instantly causes oxygen deficiency in all tissues of the body.
Left ventricular failure has been reported in 0.4-2.0 percent of European residents, and there are 40 million patients with this diagnosis in the world. The pathology is included in the international directory of diseases, its ICD-10 code is I50.1. With age, the likelihood of developing LN increases: it is diagnosed in almost 20% of all hospitalized patients over 65 years of age. Mortality, taking into account etiology, varies between 50-80%. In the rapid course of heart failure, the first and main sign of the disease, as well as a threatening factor, is pulmonary edema.
Forms of left ventricular failure
According to the classification accepted in medicine, acute or chronic forms of pathology are distinguished. Despite the common basis, they differ significantly from each other - etiology, causes, symptoms.
Acute form (ALF)
Its peculiarity is a sharp deterioration in the patient’s condition due to a delay in the movement of blood through the lungs under the influence of any factors. Stagnant blood penetrates the thin walls of the capillaries, seeps through the connective tissue and finally ends up in the alveoli of the lungs. Normally, these are bubbles containing air, but when a liquid substance gets into them, a complete breakdown of gas exchange processes occurs. The patient cannot breathe, suffocation occurs, indicating pulmonary edema.
Pulmonary edema due to cardiac dysfunction
Chronic form (CLN)
If acute left ventricular failure is characterized by a rapid course, then the chronic disease develops sequentially, going through several stages, sometimes over many years. Symptoms of a chronic condition are expressed in attacks of cardiac asthma, which then lead to pulmonary edema. In any case, the heart wears out, and without adequate treatment it can give out at any time.
Signs of the occurrence of LVN
Symptoms of left ventricular failure are determined by the reasons for its development.
Acute left ventricular failure is characterized by the following symptoms:
- sudden shortness of breath;
- increased blood pressure (during hypertensive crises);
- increased heart rate (at the initial stage of the disease);
- cough;
- expansion of the heart size to the left side;
- the appearance of a horizontal position on the electrocardiogram;
- symptoms of cardiac asthma;
- respiratory failure;
- swelling of the lower extremities.
The manifestation of the chronic form of LVN begins gradually, with the appearance of fatigue, fatigue, and loss of appetite. Patients are characterized by swelling of the lower extremities and shortness of breath during physical exertion. If timely treatment is not undertaken, the symptoms of the disease intensify and the patient’s condition worsens.
Causes
The development of an acute form of LI can potentially begin in any person, regardless of gender and age, provided that he or she has cardiovascular disorders. Although, according to statistics, men of pre-retirement age with coronary heart disease are a particular risk group.
The causes of ALVN are divided into 2 types:
- Cardiac diseases associated with pathological changes in the heart muscle:
- myocarditis – acute inflammatory processes in the myocardium;
- death of myocardial muscle fibers, often observed in the post-infarction period (the degree of necrosis depends on the timeliness of medical care);
- anatomical changes in the heart caused by congenital defects in a child;
- unstable heartbeat (atrial fibrillation, ventricular tachysystoles);
- hypertensive crisis.
- Extracardiac diseases that occur in various organs and indirectly affect the activity of the heart:
- pneumonia;
- severe poisoning;
- thromboembolic pulmonary artery syndrome;
- electrical injuries;
- asphyxia;
- severe anemia;
- terminal forms of liver and kidney diseases.
The reasons described above can also lead to the appearance of a chronic form of the disease.
Important: A sudden attack of left ventricular failure can be provoked by excessive physical activity, overheating of the body in a sauna, psycho-emotional stress, or a large dose of alcohol.
Risk factors
Risk factors for right heart failure may include:
- Age: Men between 50 and 70 years of age often experience right-sided heart failure, especially if they have previously had a heart attack.
- Chronic diseases: Lung pathologies such as COPD or pulmonary fibrosis, diabetes, HIV, hyperthyroidism, hypothyroidism or iron/protein accumulation can lead to right-sided heart failure.
- Irregular heartbeats (arrhythmias): Abnormal heart rhythms, especially if they are very fast and fast, can weaken the heart muscle.
- Lung conditions: Blood clots or high blood pressure in the lungs may increase the risk of right-sided heart failure.
- Inflammation of the pericardium: the disease provokes a decrease in the size of the pericardial sac, which compresses and tightens the heart muscle.
- Racial Predisposition: African-American men are at higher risk than others for developing right-sided heart failure.
- Certain chemotherapy and diabetes drugs: Certain medications have been found to increase the risk of PHF.
- Valvular heart disease: Damage or defect in one of the four heart valves may prevent effective hemodynamics.
- Viral infection: Some viral diseases can damage the heart muscle, including the right ventricle.
How does an acute condition develop?
The process of pulmonary edema occurs quickly, but it has a certain algorithm. With a sharp decrease in blood output from the heart muscle, acute left ventricular failure develops in this order.
- Hydrostatic blood pressure increases in the veins and capillaries of the pulmonary circulatory network.
- Blood leaks from the capillaries into the connective tissue of the lungs, they lose their elasticity, and interstitial edema begins in them (cardiac asthma). It manifests itself in the form of shortness of breath, cough, rapid pulse, and increased diastolic pressure. Sometimes cold sweat is added to the syndrome, and the veins in the neck swell.
- Having accumulated in the tissues, edematous fluid displaces air from the alveoli and causes alveolar edema. The swelling rises higher, causing an increase in vascular pulmonary and bronchial resistance.
- There is a sharp disturbance in gas exchange. As fluid accumulates in the bronchioles, the airways narrow - this is evidenced by loud wheezing, bronchospasms, and increased suffocation.
- Stagnant blood from the alveoli enters the left atrium, where it mixes with oxygenated blood. The partial pressure of oxygen in the arteries begins to fall, and as this process deepens, hypoxemia develops.
In the first phase of ALVN, oxygen starvation is caused only by a weak release of blood. At the stage of alveolar edema, hypoxia increases due to the fact that the gaps in the alveoli and tracheobronchial tree are filled with foamy sputum, which then protrudes from the mouth. The person loses the ability to breathe. Cardiogenic shock occurs: blood pressure decreases, consciousness is impaired or lost, the pulse accelerates, and the extremities become cold.
Causes of pathology
There are many factors that can cause the development of left ventricular failure:
- myocardial infarction is the most common cause;
- high blood pressure, which is constant;
- arrhythmia, which causes a significant decrease in the heart’s ability to pump blood;
- inflammation in cardiac tissues;
- expansions of the cavities of the heart of a pathological nature can have a different nature, but have a common complication - left ventricular failure;
- congenital or acquired valve lesions;
- ischemia;
- head injuries;
- complex operations;
- pulmonary artery damage;
- coronary syndrome that has developed into an acute form;
- nephritis;
- many lung pathologies;
- diseases that cause fluid accumulation in the body;
- exposure to toxins or heavy metals on the heart.
Symptoms and stages of the chronic form of the disease
A distinctive feature of the pathology is a systematic violation of the blood ejection regime of the left ventricle. Chronic left ventricular failure leads to constant interruptions in the blood supply to the entire body, congestion in the pulmonary circulation and lower respiratory tract. The patient's condition worsens gradually, each phase of the disease is characterized by its own clinical manifestations.
Stage 1. Shortness of breath and increased heart rate are noticeable during intense physical movements. This sign will be noticed only by trained people who previously reacted calmly to increased loads. For an ordinary person, such a reaction is normal.
Stage 2a. When climbing stairs above the 4th floor, walking for half an hour, or short jogging, a person cannot catch his breath, and a strong heartbeat begins. A dry cough is a constant concern (in the absence of respiratory tract disease caused by infection). Blueness appears on the lips, called cyanosis.
Cyanosis of lips
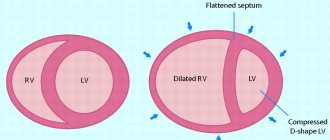
Stage 2b. In addition to the left ventricular failure, right ventricular failure develops, due to which stagnation of venous blood is already observed in the systemic circulation. Shortness of breath and an accelerated pulse are observed with minor exertion (moving around the house, light housework), and then at rest. Impaired blood flow leads to liver enlargement (pain in the right hypochondrium), cough, cyanosis, and attacks of cardiac asthma. In addition to swelling of the extremities, swelling of the abdominal cavity (ascites) is added. Since the blood supply to the brain suffers, it often hurts and feels dizzy.
Stage 3. All of the above symptoms are most pronounced. The transformations that have occurred in the lungs, heart, and liver become irreversible. It is no longer possible to recover at stage 3.
Characteristics and symptoms of the disease
Left ventricular failure can manifest itself in several forms, the symptoms for each of them are different. It is not surprising that we decided to combine the symptoms and classification of the disease into one section. But first, let's talk a little about the symptoms. According to the nature of the manifestation, the pathology is divided into several stages:
- at the initial stage, clinical manifestations are insignificant, and they appear exclusively under high loads;
- the moderate form is characterized by the presence of symptoms regardless of the state of rest or performing heavy physical work;
- terminal is the most dangerous form of pathology, in which irreversible changes occur in the internal organs.
Left ventricular failure is the cause of death
Impaired contractility of the left ventricular myocardium is one of the most negative factors depressing the activity of the heart. The pump ceases to cope with the supply of biological fluid to the body systems. Blood stagnates in the large and small circles of the bloodstream. This leads to hypoxia of all organs, metabolic processes are disrupted, and the rate of synthesis of molecules decreases. Oxygen starvation is especially dangerous for brain cells.
Stagnation of blood in the lungs prevents them from carrying out full gas exchange, so in case of left ventricular failure, suffocation becomes the main cause of death. Fulminant pulmonary edema is fatal within a few minutes. Acute edema is characterized by a rapid course for about 4 hours, and even with immediate resuscitation it is not always possible to avoid the death of the patient.
Against the background of hypoxia, heart rate and the overall load on the heart increase; malfunctions in the aortic and mitral valves are very likely. Due to insufficient tissue nutrition, complications such as myocardial infarction, kidney failure, and scarring of liver cells are possible.
Causes
There are two broad groups of factors contributing to the development of right ventricular heart failure.
- Primary right ventricular failure in the absence of pulmonary hypertension. Myocardial infarction
- Pulmonary embolism
More recently, a high mortality rate has been identified among patients with isolated RV myocardial infarction, which has forced a reassessment of the risk of the disease.
Various congenital heart defects are often associated with RV failure, usually due to increased workload, volume overload, or both. Septal defects are commonly associated with PVC; usually because blood is shunted from the left side of the heart to the right. Tetralogy of Fallot is another birth defect in which RV hypertrophy and eventual RV failure occurs due to obstruction of the pulmonary artery that receives blood from the RV. In an adult with repaired tetralogy of Fallot, RV failure may still occur due to pulmonary regurgitation, especially when the tricuspid valve has been used to repair the structure of the affected vessel.
Diagnostics
First, the doctor conducts a visual examination, identifying external symptoms of the pathology: cyanosis of the lips and nails, anxiety, dry cough, shortness of breath. Using a tonometer, blood pressure and heart rate are measured (as a rule, they are higher than normal). During auscultation, box sounds are detected - with percussion of the lungs, isolated dry wheezing - with bronchospasms. Heart sounds are almost inaudible due to noisy, hoarse breathing. Indirect signs of the disease are an enlarged liver and swollen lower limbs.
Hardware and laboratory research methods will help to establish an accurate diagnosis.
The main directions of hardware diagnostics are as follows.
- X-ray. It helps to identify pulmonary edema by changes in their pattern, especially in the hilar areas. The roots change their structure, their contours become unclear. The transparency of the pulmonary lobes decreases.
- Pulse oximetry. The study shows low blood oxygen levels (less than 90%).
- Measurement of venous pressure in large vessels. For this purpose, a Waldmann phlebotonometer is connected to the subclavian vein. Pulmonary edema is indicated by an increase in venous pressure to 12 mm Hg. Art.
- ECG. It is used to determine cardiac pathologies that cause pulmonary edema. The electrocardiogram shows signs of arrhythmia, thickening of the walls of the heart chambers, hypertrophy of its left parts, ischemia, and myocardial infarction.
- Transthoracic echocardiography. It serves to check the functioning of the myocardium and the condition of the valves if the causes of pulmonary edema are not established during examination and x-rays. Echocardiography is the most important criterion for determining the need for surgical intervention.
Ultrasound of the heart - Pulmonary artery catheterization. A catheter is used to measure vessel wedge pressure to determine the cause of pulmonary edema, and to monitor cardiac output and vascular resistance during treatment.
Laboratory diagnostics includes several mandatory points that make it possible to establish the nature of LN and determine treatment tactics.
- Blood chemistry. It shows what caused pulmonary edema: myocardial infarction, decreased protein levels in the blood (hypoproteinemia) or renal pathology.
- Measuring the concentration of carbon dioxide and oxygen in the blood. In acute LN syndrome, the partial pressure of the first is 35 mm Hg, the second is 60 mm Hg.
- Coagulogram. It records changes in blood clotting if pulmonary edema appears due to pulmonary embolism - in this case fibrinogen increases to 4 g/l, and prothrombin - to 140%.
- Determination of BNP (brain natriuretic peptide) concentration. Modern techniques serve to clarify the diagnosis of LN.
Stages of emergency care
If a heart attack occurs with symptoms of left ventricular failure, its acute form, immediately call an ambulance. Only a qualified specialist can save a patient’s life, draw correct conclusions about his condition and prescribe adequate treatment. Until doctors arrive, pre-medical measures should be carried out according to a certain algorithm, the purpose of which is to mitigate the acute manifestations of the disease.
- To facilitate breathing, the patient should be placed in a semi-sitting position (if blood pressure is high, sit down), unbutton the collar of the clothes, open the window.
- To stop an attack, a Nitroglycerin tablet is placed under the tongue.
- To relieve the load on the heart muscle, the thighs are bandaged with tourniquets. This should be done no earlier than 10 minutes after the patient sits down, so that the blood has time to redistribute.
- When foam appears, it is removed using suction with a catheter or a laryngoscope. If the patient is conscious, he is recommended to cough more often to clear the upper respiratory tract naturally.
- For unbearable pain in the sternum, use Morphine or Fentanyl.
- Swelling is removed using Furosemide or Uregita tablets.
Important: If breathing is uneven, the airways are filled with mucus, the person loses consciousness, it is prohibited to use Morphine.
The arriving ambulance doctor examines the patient, urgently diagnoses acute left ventricular failure and continues to provide emergency care.
- A forced supply of oxygen is provided through the mask. To neutralize foam coming out through the mouth or sinuses, oxygen is passed through ethyl alcohol.
- Drugs are administered to normalize cardiac activity, “Novocainamide”.
- To reduce blood pressure, the patient is given Enap.
- Droperidol is administered intra-arterially to reduce shortness of breath.
After stopping the acute phase, the patient is urgently hospitalized.
Please note: When transporting to a medical facility, the patient is placed on a stretcher so that the head remains elevated.
Stages of pathology
There are three main stages:
Initial. Symptoms of left ventricular failure are mild. A person notices the appearance of shortness of breath and increased heart rate during physical activity. At rest, the disease does not manifest itself in any way. If the symptoms appear quite clearly, this indicates that the disease is progressing. Therefore, it is important to start therapy as soon as possible to prevent the disease from progressing to a late stage.
Average. Swelling begins to appear, the patient’s complaints of severe shortness of breath and breathing problems will be typical.
Terminal. Processes occur in the body that lead to irreversible changes. After the onset of end-stage left ventricular heart failure, treatment becomes ineffective. There is a high probability of death.
Treatment
The hospitalized patient is placed in an intensive care unit and measures are taken to activate cardiac output and improve oxygen supply to the organs. In the absence of positive dynamics, surgery is recommended.
Therapeutic treatment
Tactics for combating acute and chronic forms of the disease are somewhat different from each other. If a patient is admitted after an acute attack, an ECG must be recorded in a hospital setting and, according to the recommendations of cardiologists, the following measures must be immediately taken:
- To inhibit metabolic processes and adapt cells to temporary oxygen deficiency, a Morphine solution is used. It is diluted with an isotonic solution and slowly injected into a vein; if necessary, repeat the procedure after 15-20 minutes. The drug depresses respiration and lowers blood pressure by dilating peripheral blood vessels.
- At the next stage, strong vasodilators (for example, sodium nitroprusside) are administered to reduce venous return. They increase the lumen of the coronary arteries and help relieve swelling. A universal remedy for eliminating edema is Furosemide. 20–200 mg of the drug is administered intravenously to dilate the venous vessels, activate urine flow and reduce the load on the myocardium.
- If signs of left ventricular failure are provoked by myocardial infarction or hypertensive crisis, but blood flow in the brain is not impaired, solutions of “Isosorbide dinitrate” or “Nitroglycerin” are administered intravenously. They are used for high or normal blood pressure.
- For pulmonary edema, the condition is alleviated by bloodletting up to 400-500 ml.
- Cardiogenic shock (if the heart rate is below 40 beats/min) is stopped with an Atropine solution, and then plasma-substituting solutions are administered.
If the attack of ALV is relieved, long-term treatment begins. First of all, for this purpose, etiotropic therapy is used, directed against the main provoking disease. The doctor usually prescribes the following groups of drugs:
- thrombolytics - to prevent blockages of blood vessels;
- nitrate-containing drugs;
- analgesics with a narcotic effect - to relieve acute pain and prevent painful shock;
- antihypertensive drugs to lower blood pressure;
- antiarrhythmic drugs;
- corticosteroids - they eliminate inflammatory processes in the myocardium.
Corticosteroid hormone Dexamethasone
As additional measures, diuretics are used to reduce the volume of fluid in the internal organs. This helps to normalize blood flow in the pulmonary circulation.
Various classes of medications are also used to treat chronic LI:
- diuretics - to drain excess fluid and improve kidney function;
- beta-blockers - to relieve the myocardium by reducing heart rate;
- ACE inhibitors - to stabilize blood pressure;
- nitrates - to increase the lumen of arteries and prevent acute attacks of pulmonary fibrosis;
- cardiac glycosides - to improve blood ejection into the aorta.
Surgical methods
Surgical intervention in this case is life-threatening and requires long-term rehabilitation. Various techniques involve implanting valves or stimulators, restoring the configuration of the heart muscle (cardiomyoplasty), or heart transplantation. The method is selected depending on the root cause of the pathology and the condition of the heart.
Here are the main types of operations for LVSD:
- coronary angiography – expansion of the lumen in the coronary vessels to improve blood flow;
Carrying out coronary angiography - stenting – mini-springs push the walls of the arteries apart, improving blood circulation;
- replacing worn valves;
- bypass surgery - sewing in sections of arteries or veins taken from different parts of the body to create a bypass route for blood to bypass narrowed coronary arteries;
- operations to reconstruct the shape of the heart - by passing electrical signals through it, dynamic cardiomyoplasty, Dor or Acorn procedures, laser exposure, radiofrequency ablation;
- heart transplant from a deceased donor.
Symptoms
Manifestations largely depend on the form of the pathological process. Two classifications are generally accepted.
The first concerns the staging of the disorder. There are 4 stages of violation (in some variations of the specified typing method - 3 with a more fractional division of points).
According to the second classification, acute and chronic failure are distinguished.
- Acute right ventricular failure develops rapidly, the symptoms are identical to chronic but more pronounced, the probability of death is about 80%.
An attack requires a trigger factor or provocateur; it does not appear out of the blue.
- A chronic or latent, sluggish pathological process is accompanied by a gradual increase in manifestations. Progression corresponds to the described stage scheme.
Stage 1
Initial manifestations. Pathological changes in the heart and blood vessels are already present.
However, they are nonspecific and negligible in intensity. In addition, the patient does not pay enough attention. This makes early diagnosis a difficult issue.
An approximate list of symptoms at the first stage:
- Dyspnea. Lightweight, almost imperceptible. It develops against the background of extremely intense physical activity.
A person has little chance of meeting this level of activity; as it progresses, the bar decreases.
The approximate time frame for aggravation of the pathological process is several years. Rarely faster.
There are cases where right ventricular failure at the first stage lasted 10-15 years or more.
- Weakness, drowsiness. Unexplained fatigue. It is called “asthenia”. It appears suddenly, accompanies the patient constantly and does not go away. Efficiency, productivity of thinking and activity decreases.
- Cough. Dry, regular. Lasts from a few minutes to a couple of hours. Accompanied by a feeling of lack of air. Typically, patients attribute the symptom to a cold, smoking and other common causes.
- Acceleration of cardiac activity. Sinus tachycardia. An increase in the number of heart contractions to 110-115 beats per minute is not even a background of rest. During physical activity, the indicators increase slightly.
A patient in the initial stage of heart failure encounters this clinical picture. Sometimes there are fewer symptoms, rarely there are more. The best time for therapy.
Stage 2
Moderate violations. This is no longer the beginning of the disorder, but it is not yet the terminal phase.
Attention:
Recovery is still possible, so you can’t give up, you need to urgently contact a cardiologist.
Symptoms of right ventricular failure at stage 2 are pronounced, cardiac and pulmonary, neurogenic and mental.
Among them:
- Dyspnea. It occurs during physical activity, but the required intensity to provoke the symptom is much less than at the initial stage. For example, going up to the 4th-5th floor. Accompanied by increased cardiac activity.
- Fatigue, lethargy, drowsiness. More pronounced, it is impossible to perform work duties normally. After rest, the condition is partially corrected, but after a couple of hours everything returns to normal and the person is broken again.
- Insomnia. Characterized by frequent awakenings at night. Every 10-30 minutes. The symptom provokes a worsening of the previous symptom.
- Emotional lability, irritability. Mental disorder. The affect is heightened, a person can explode for an unimportant reason, a minute later fall into euphoria, and after another two into dysthymia, a depressive state. This is the result of a hormonal imbalance in the system with insufficient nutrition of the brain.
- Tachycardia. Increased heart rate to levels above 100 beats per minute. Accompanied by shortness of breath and sweating. At rest it weakens, but does not go away completely. It occurs in fits and starts. Each lasts from 10 to 120-180 minutes.
- Chest pain. Pressing, burning, bursting. Which directly indicates the cardiac, ischemic nature of the discomfort. There are no shooting or tingling sensations.
Attention:
Localization is not always obvious. In some cases, the patient is sure that his stomach hurts.
- Headache. The result of insufficient blood circulation in cerebral structures. Pressing, shooting in character. Localized in different parts, can be diffuse (spread), without a clear location.
- Nausea. Vomit. Both symptoms are relatively rare and are reflexive in nature. Therefore, relief does not occur after the act of emptying the stomach.
- Dizziness. Vertigo. Inability to navigate in space. At the time of an acute attack, a person is forced to take a lying position and move less, so as not to provoke an increase in the symptom. There is a disorder of the vestibular apparatus, extrapyramidal system, and also muscle weakness.
- Sweating. Hyperhidrosis.
- Cyanosis of the nasolabial triangle. Blue discoloration of the area around the mouth. It looks like a ring.
- Paleness of the skin. Also nail plates, mucous membranes. The symptom is always identified.
- Cough. Dry, unproductive reflex. Accompanies the patient at all times. The intensity is low, there are no “clogging” attacks, but it is impossible not to notice the violation.
Stage 3
Severe right ventricular failure produces disabling symptoms that put an end to professional activity and normal life.
A complete cure is impossible, but there are chances to partially correct the condition.
The symptoms are identical, but their intensity is much higher. There are other aspects that have not been discovered before.
- Shortness of breath occurs with minimal physical activity and even at rest. The patient cannot move normally, walking becomes unbearably difficult, as does performing household duties.
- Tachycardia. Constant. But, after a few days or weeks, the person gets used to the condition and ceases to feel the acceleration of cardiac activity.
- Fall in blood pressure. Objective sign. Indicates insufficient contractility of the myocardium, ineffectiveness of the heart. It is not yet at critical levels, there is no collapse, but the possibility of an emergency condition is present.
- Hemoptysis. Cough with the release of liquid tissue drop by drop. Differential diagnosis with the tuberculosis process is required.
- Edema. They are caused by impaired renal function and a reduced rate of fluid excretion. Filtration weakens, because the quality of the heart and pumping function drop to minimum levels. Recovery requires stimulation of cardiac activity.
Stage 4
Considered terminal. Cure is impossible, as is correction of the condition. This is the finale of the pathological process, which ends in death in all cases.
Palliative care is aimed at alleviating the condition and possibly maintaining well-being at an acceptable level.
The symptoms are critical. A person cannot breathe normally, even in a state of complete rest.
Bradycardia is detected with a decrease in heart rate to 40-60 beats per minute. Other arrhythmias occur, such as extrasystole.
Signs of right ventricular failure - cardiac, pulmonary, neurogenic, mental - pose a great danger to the patient’s life and his capabilities.
Prevention
Left ventricular failure (if it is not associated with congenital structural pathologies) can be prevented if you adhere to the following rules:
- control body weight, preventing obesity;
- do not include too fatty foods in the diet, do not add too much salt to food, and do not allow constant intake of large volumes of liquid;
- follow a daily routine, dose physical activity, avoid stress;
- give up alcohol and smoking;
- systematically monitor blood pressure.
Forecast
Left ventricular failure allows for a favorable prognosis only at the onset of the disease and with timely treatment. Only in this case can the development of irreversible disorders in the heart be prevented. The acute form of the disease significantly worsens the prognosis, since it contributes to the destruction of not only the heart muscle, but also other internal organs.
Surgical operations help to significantly increase a patient’s life expectancy, but they require a long rehabilitation period to restore body functions.
Did you like the article? Save it!
Still have questions? Ask them in the comments! Cardiologist Mariam Harutyunyan will answer them.
Ivan Grekhov
Graduated from the Ural State Medical University with a degree in General Medicine. General practitioner
Description
Until recently, right ventricular function has been overshadowed by large-scale studies of left ventricular function. However, recently the importance of the right ventricle has become apparent. Initially, researchers tried to extrapolate data obtained from the left ventricle to the right ventricle, but from the very beginning it became clear that the left and right ventricles differ significantly in many ways. Historically, understanding of right ventricular function has been limited by the perception of contractile right ventricular function as hemodynamically insignificant. Nowadays, right ventricular failure is widely discussed among professional communities, however, numerous questions regarding this topic have not been fully explored. This is largely due to differences in approaches to assessing and analyzing right ventricular function, the lack of standards and basic knowledge. This review is an attempt to systematize the available data, identify the most important aspects of right ventricular failure, and identify further directions for research.