Few people know that the heart also needs proper rest for its productive work. If proper relaxation of the heart chambers, for example, the left ventricle, does not occur, diastolic dysfunction of the left ventricle develops, and this can lead to more serious disturbances in its functioning. But when does the heart rest, because its work occurs non-stop? What kind of pathology is left ventricular diastolic dysfunction, what are its symptoms? What is the danger? Can this heart disorder be treated? The answers to these questions will be presented in our article.
Causes and mechanism of disease development
Left ventricular diastolic dysfunction is a process where the heart muscles are unable to relax completely, causing the organ to receive insufficient amounts of the blood it needs. During normal heart function, there are the following stages:
- relaxation of the heart muscle;
- movement of blood along a specific route;
- saturation of all necessary components of the heart with blood.
With diastolic function of the left ventricle, the process of filling with blood at the moment of its relaxation is disrupted. The body wants to correct this situation and in order to fill the blood deficit, the left atrium works to the maximum to fill the gap in the current situation.
As a result of such hard work, it increases in size, and this situation leads to its overload. Persistent high blood pressure and myocardial ischemia are the most common causes of this disease.
Type 1 left ventricular diastolic dysfunction is observed to a greater extent in older people, particularly women. The main causes of left ventricular diastolic dysfunction are:
- Myocardial ischemia.
- Arterial hypertension.
- Advanced age.
- Overweight.
- Aortic stenosis.
Insufficient elasticity of the muscle tissue of the heart, which leads to impaired ability to contract and relax, is a major factor in the disease. Left ventricular diastolic dysfunction can occur in both adults and newborns.
Special treatment is not needed here, this condition does not pose a great danger, the exception is the prematurity of the baby or in the case when the child has suffered oxygen starvation.
A clear distinction must be made between diastolic dysfunction and diastolic heart failure. If the second term includes the first, then diastolic dysfunction does not always indicate heart failure.
Characteristics of the disease
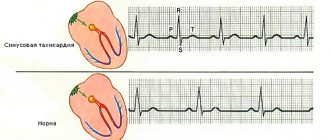
The cardiac cycle is divided into two phases - systole and diastole. During the first, the ventricles (the main chambers of the heart) contract, pushing blood out of the heart into the arteries, and then relax. When they relax, they refill with blood to prepare for the next contraction. This relaxation phase is called diastole.
The cardiac cycle consists of systole (contraction of the heart) and diastole (relaxation of the myocardium), during which the heart fills with blood
However, sometimes due to various diseases the ventricles become relatively “hard”. In this case, they cannot relax completely during diastole. As a result, the ventricles are not completely filled with blood, and it stagnates in other parts of the body (in the lungs).
Pathological hardening of the walls of the ventricles and the resulting insufficient filling of them with blood during diastole is called diastolic dysfunction. When diastolic dysfunction is so severe that it causes congestion in the lungs (that is, accumulation of blood in them), it is considered to be diastolic heart failure.
Signs of heart failure - video
Probable causes
The most common cause of diastolic dysfunction is the natural effect of aging on the heart. With increasing age, the heart muscle becomes stiffer, impairing the filling of the left ventricle with blood. In addition, there are many diseases that can lead to this pathology.
Diseases that provoke diastolic dysfunction - table
| Disease | What is this? | How does it cause diastolic dysfunction? |
| Cardiac ischemia | A disease caused by blockage of the coronary arteries that supply blood to the heart. | Poor blood supply to the heart (ischemia) can prevent it from relaxing and filling with blood. |
| Arterial hypertension | High blood pressure. | To overcome the increased pressure, the heart muscle and the wall of the left ventricle thicken. This limits their ability to relax and fill with blood. |
| Aortic stenosis | Narrowing of the aortic valve opening. | The walls of the left ventricle thicken, which impairs its ability to fill with blood. |
| Hypertrophic cardiomyopathy | Hereditary pathology of the myocardium, leading to significant thickening of the walls of the heart. | Thickened heart muscle interferes with the filling of the left ventricle with blood. |
| Pericardial diseases | Pathology of the membrane that surrounds the heart (pericardium). | Fluid in the pericardial cavity (cardiac tamponade) or thickening of the pericardium (constrictive pericarditis) can limit the left ventricle's ability to fill with blood. |
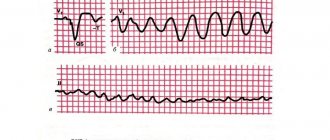
| Tachyarrhythmias | Heart rhythm disturbances with a very high frequency of contractions. | Diastole time is reduced, which negatively affects the degree of filling of the left ventricle with blood. |
Why can type 1 left ventricular diastolic dysfunction develop? The reasons for this phenomenon lie in the following:
- hypertensive pathologies;
- hypertrophic cardiomyopathy;
- infiltrative (periodic) heart lesions (that is, heart attacks, ischemic heart disease, chronic hypertension (arterial), as well as hypertrophy of individual cardiac segments that are outside the zone of dilatation and thinning).
Symptoms
Signs of left ventricular diastolic dysfunction make themselves felt when serious changes have already begun in the body. List of characteristic symptoms:
- Heartbeats become rapid both in an active state and in a calm state.
- The person cannot take a deep breath, as if the chest is being compressed.
- Attacks of dry cough indicate the appearance of congestion in the lungs.
- Any slight effort is difficult.
- Shortness of breath occurs both during movement and at rest.
- Increased frequency of sleep apnea attacks is also an indicator of problems in the left ventricle.
- Another sign is swelling of the legs.
Distinctive features of the violation
Symptomatic manifestations of the abnormal condition are presented:
- a constantly present cough - in some cases, attacks are noted;
- paroxysmal type of dyspnea - short-term cessation of breathing during sleep;
- periodic shortness of breath.
Additional signs of the disease are:
- painful sensations in the retrosternal space - attacks resemble ischemic damage to the heart muscle;
- severe swelling of the tissues of the lower extremities;
- sharp spasms;
- feeling of insufficient oxygen supply.
Types of pathology
Hypertrophic origin - refers to the primary stage of the lesion, often recorded in patients with early stages of arterial hypertension. Patients experience a superficial change in muscle relaxation of the left ventricle.
Pseudonormal - recorded in patients with serious deviations in the performance of the heart muscle. Against the background of the anomaly, there is a decrease in the level of muscle relaxation and an increase in pressure in the left atrium. The filling of the ventricle of the same name occurs due to the difference in pressure marks.
Restrictive - the terminal stage of dysfunction is among the most dangerous. The filling of the ventricle is minimal - against the background of a decrease in the level of elasticity of its walls and an increase in their rigidity.
Diagnosis of diastolic heart failure
Diagnosing the disease at an early stage will help avoid irreversible changes.
To establish a diagnosis, three conditions are usually necessary:
- manifestation of symptoms and signs of heart failure;
- PV systolic function is normal or slightly decreased;
- instrumental diagnostic methods reveal disturbances in the functioning of the LV and an increase in its stiffness.
Early diagnosis helps prevent irreversible changes in heart function
The main instrumental diagnostic methods include:
- two-dimensional echocardiography with Doppler ultrasound is one of the most effective methods for determining the diagnosis;
- radionuclide ventriculography will determine the failure of myocardial contractility;
- EchoCG reveals signs of myocardial ischemia;
- A chest x-ray will help determine pulmonary hypertension.
Early diagnosis helps prevent irreversible changes. In order to identify the development of pathology, the following diagnostic methods are used:
- two-dimensional echocardiography with Dopplerography is one of the accessible and informative methods of diagnosis verification;
- radionuclide ventriculography is a highly informative method for diagnosing disorders of myocardial contractility, indicated in case of unsatisfactory results of echocardiography;
- electrocardiography is an auxiliary diagnostic method that allows you to identify signs of myocardial ischemia and the presence of hypertrophied myocardium;
- Chest x-ray – used to look for signs of pulmonary hypertension.
Causes and mechanism of disease development
Impaired functionality in the diastole phase in the left ventricle refers to age-related abnormal processes, the majority of patients are female. The disease provokes disturbances in circulatory processes and atrophic lesions of the structural elements of the myocardium.
The process of filling the heart chamber with blood includes several steps:
- complete relaxation of the muscle tissue of the organ;
- passive passage of blood into the ventricle - under the influence of differences in pressure;
- Contraction of the atria provokes the release of the remaining blood into the ventricle.
If pathological changes occur in one of the above stages, then cardiac output does not fully occur. The anomaly provokes the formation of insufficient functionality of the left-sided ventricle.
Symptoms and types of disease
The symptoms that bother people with diastolic dysfunction are the same as those experienced in patients with any form of heart failure.
With diastolic heart failure, signs of pulmonary congestion come to the fore:
- dyspnea;
- cough;
- rapid breathing.
Patients with this diagnosis often suffer from these symptoms in the form of sudden attacks that appear without any warning. This distinguishes diastolic heart failure from other forms of heart failure, in which shortness of breath usually develops gradually over several hours or days.
The sudden and severe difficulty breathing that often occurs in diastolic heart failure is called a “pulmonary edema flare” episode.
Although the hallmark of diastolic HF is bursts of pulmonary edema, patients with this disease may also experience less severe episodes of difficulty breathing that develop more gradually.
Main symptoms of the disease
Diastolic myocardial dysfunction is not considered an independent disease. As a rule, this in itself is a sign of an already developing disease. This pathology leads to heart failure and is manifested by the following symptoms:
- swelling of the legs;
- high fatigue;
- the appearance of shortness of breath even with little physical activity. If it manifests itself at rest, then the disease has already become serious;
- increased heart rate;
- the skin turns pale, especially in areas of the body distant from the heart.
Cough can also be considered one of the symptoms of heart failure. Most often it appears at night, indicating congestion in the lungs.
Diagnosis of dysfunction
The presence of diastolic dysfunction can be detected using cardiac ultrasound - echocardiography. This examination method allows you to evaluate the characteristics of myocardial relaxation during diastole and the degree of stiffness of the walls of the left ventricle.
Echocardiography can also sometimes help detect the cause of diastolic dysfunction. For example, with its help you can identify: .
- thickening of the walls of the left ventricle in hypertension and hypertrophic cardiomyopathy;
- aortic stenosis;
- some types of restrictive cardiomyopathies.
However, many patients with evidence of diastolic dysfunction on echocardiography do not have other pathologies that could explain its presence. In such people it is impossible to determine the specific cause of the disease.
It should be noted that for each degree of diastolic dysfunction there are specific criteria for echocardiography, so they can only be determined using this study.
When seeking professional help, the patient undergoes a number of laboratory and instrumental examinations:
- clinical and biochemical blood tests;
- ECG;
- Holter monitoring;
- Ultrasound using Doppler technique;
- echocardiography.
Additional diagnostic measures are:
- determination of hormonal levels;
- X-ray images;
- coronary angiography, etc.
Diastolic dysfunction: new diagnosis or difficult to diagnose disease
Recently, cardiologists and therapists are increasingly giving their patients a “new” diagnosis - diastolic dysfunction. In severe cases, diastolic heart failure (HF) may occur.
Nowadays, diastolic dysfunction is found quite often, especially in older women, most of whom are surprised to learn that they have heart problems.
Often, patients diagnosed with diastolic dysfunction may develop diastolic heart failure.
Neither diastolic dysfunction nor diastolic heart failure are actually “new” diseases—they have always affected the human cardiovascular system. But only in recent decades have these two diseases become frequently identified. This is due to the widespread use of ultrasound methods (echocardiography) in diagnosing cardiac problems.
It is believed that nearly half of patients presenting to emergency departments with acute heart failure actually have diastolic HF. But making the correct diagnosis can be difficult because once the patient's condition has been stabilized, the heart may appear completely normal on echocardiography unless the specialist specifically looks for signs of diastolic dysfunction. Therefore, inattentive and unwary doctors often miss this disease.
Treatment
To ensure the presence of these diseases, you need to take the following tests and examinations:
- Blood and urine tests (general, hormone levels).
- ECG.
- Electrocardiography.
- Chest X-ray.
- MRI.
- Coronary angiography.
Treatment of dysfunction is carried out with medications and is aimed, among other things, at reducing complications. If the disease is asymptomatic, treatment at an early stage consists of taking ACE inhibitors. These are drugs that protect other organs from the effects of high blood pressure and have a beneficial effect on the myocardium, preventing its modification. Among them:
- Enalapril.
- Lisinopril.
- Quadripril.
- Perindopril.
If the symptoms are pronounced, the following are prescribed:
- diuretics (prevent stagnation in organs): Veroshpiron, Diuver, Lasix, Furosemide;
- calcium channel blockers and beta blockers (relax blood vessels, make the heart beat less often, which reduces the load on the organ);
- glycosides (improves the strength of heart contractions);
- statins (normalize cholesterol levels, which is important for atherosclerosis);
- blood thinner Aspirin.
In case of left ventricular dysfunction, a diet is prescribed that consists of limiting salt intake to 1 g per day and fluid intake to 1.5 liters. It is necessary to limit the consumption of fried, spicy, salty foods and increase the amount of fruits, vegetables and dairy products in the menu.
If these requirements are met and therapy is prescribed in a timely manner, the prognosis of the disease can be favorable.
The best treatment strategy for diastolic dysfunction and diastolic HF is to attempt to identify and treat the cause. Thus, the following problems need to be overcome:
- Arterial hypertension. People with diastolic dysfunction often have elevated blood pressure that is difficult to detect. Moreover, very often such hypertension is treated inadequately. However, it is very important for patients with diastolic dysfunction to control their blood pressure within normal limits.
- Cardiac ischemia. People with diastolic dysfunction should be evaluated for coronary artery disease. This disease is a common cause of diastolic dysfunction.
- Atrial fibrillation. The rapid heartbeat caused by this rhythm disorder can cause significant deterioration in heart function in people with diastolic dysfunction. Therefore, rhythm control is a very important aspect in the treatment of a patient with atrial fibrillation and diastolic dysfunction.
- Diabetes mellitus and overweight. Weight loss and glucose control help stop the worsening of diastolic dysfunction.
- Passive lifestyle. Many people with diastolic dysfunction lead a predominantly sedentary lifestyle. An aerobic exercise program can improve diastolic heart function.
In addition to measures aimed at identifying and treating the causes of diastolic dysfunction, the doctor may prescribe medications that affect its symptoms. For this purpose, diuretics (Furosemide) are most often used, which remove excess water and sodium from the body, reducing the severity of symptoms of pulmonary congestion.
Therapy depends on the stage and severity of the disease; it is strictly contraindicated to prescribe this or that drug to yourself, because the heart is a vital organ, so it is better not to harm your health by improper actions.
If there are no symptoms of deficiency, your doctor may recommend taking angiotensin-converting enzyme (ACE) inhibitors. It regulates blood pressure and protects target organs in this disease.
Target organs are those that suffer primarily from dysfunction of the cardiovascular system, that is, they are the first “targets” along the path of blood failure. These include the kidneys, brain and spinal cord, heart, blood vessels and retina.
By taking ACE inhibitors daily at a dose prescribed by your doctor, you can reduce the risk of complications in target organs and prevent the development of chronic heart failure. Such drugs include Enalapril, Quadropril, Lisinopril.
It is difficult to say which is better; everything is discussed at an appointment with a therapist or cardiologist and prescribed based on symptoms and past experience with medication.
If you are intolerant to ACE inhibitors or for some objective reason the doctor has decided that they will not help you, ARA II (angiotensin receptor antagonists) are prescribed. They have exactly the same properties. These include Losartan, Valsartan and others.
If signs of the disease are pronounced, even more drugs are prescribed to relieve symptoms:
- diuretics (diuretics) – reduce the volume of circulating blood by removing excess fluid;
- beta blockers - make the heart rate slower, reducing the load on the organ;
- cardiac glycosides - increase the force of heart contractions;
- Aspirin - prescribed to reduce the risk of blood clots and, therefore, ischemia;
- statins – carry out lipid control in the blood by normalizing cholesterol fractions that are harmful to blood vessels.
Currently, there is no single treatment regimen that would be recognized by most specialists. This is partly due to the fact that this disease is rather difficult to diagnose. As mentioned above, such a deviation occurs asymptomatically for a very long time, as a result of which the patient seeks medical help too late.
So what should you do if you have type 1 left ventricular diastolic dysfunction? Treatment of such a disease comes down to eliminating the causes that provoke negative tendencies. Thus, patients need:
- cure existing ischemia;
- normalize heart rate;
- lower blood pressure.
Among other things, if such a pathological condition is detected, the patient is prescribed drugs from the ACE blocker group. Most often, the choice of specialists falls on Lizonopril. It is prescribed in the form of tablets of 20-40 milligrams per day (in two doses).
Good results in the treatment of this deviation can be achieved by using calcium blockers. Thus, both drug groups lower blood pressure, significantly reduce the oxygen demand of cardiac tissues, and also stop and reduce left ventricular hypertrophy.
By the way, as a result of taking these drugs, the work of heart diastole improves, which subsequently leads to normalization of hemodynamics.
The best results in the treatment of this disease were observed when potassium-sparing diuretics were combined with cardiac drugs. If urgently needed, other antihypertensive medications can be used.
What examination is needed?
If a patient experiences symptoms similar to signs of dysfunction of the ventricular myocardium, he should consult a cardiologist or therapist. The doctor will conduct an examination and prescribe any of the additional examination methods:
- Routine methods - blood and urine tests, biochemical blood tests to assess hemoglobin levels, indicators of the functioning of internal organs (liver, kidneys),
- Determination of potassium, sodium, sodium uretic peptide in the blood,
- Blood test for hormone content (determining the level of thyroid hormones, adrenal glands) if there is a suspicion of an excess of hormones in the body that have a toxic effect on the heart,
- An ECG is a mandatory research method to determine whether there is myocardial hypertrophy, signs of arterial hypertension and myocardial ischemia,
- Modifications of the ECG - treadmill test, bicycle ergometry - this is the recording of an ECG after physical activity, which allows you to assess changes in the blood supply to the myocardium due to exercise, as well as assess tolerance to exercise in the event of shortness of breath with CHF,
- Echocardiography is the second mandatory instrumental study, the “gold standard” in the diagnosis of ventricular dysfunction of the heart, it allows you to assess the ejection fraction (normally more than 50%), assess the size of the ventricles, visualize heart defects, hypertrophic or dilated cardiomyopathy. To diagnose dysfunction of the right ventricle, its end-diastolic volume is measured (normally 15 - 20 mm, with dysfunction of the right ventricle it increases significantly),
- X-ray of the chest cavity is an auxiliary method for myocardial hypertrophy, allowing to determine the degree of expansion of the heart in diameter, if hypertrophy is present, to see the depletion (with systolic dysfunction) or strengthening (with diastolic dysfunction) of the pulmonary pattern due to its vascular component,
- Coronary angiography is the introduction of a radiopaque substance into the coronary arteries to assess their patency, the violation of which accompanies coronary heart disease and myocardial infarction,
- Cardiac MRI is not a routine examination method, but due to its greater information content than cardiac ultrasound, it is sometimes prescribed in diagnostically controversial cases.
Forecast
In patients with diastolic dysfunction, the prognosis for recovery is favorable, but only if the patient unquestioningly follows all the specialist’s recommendations.
With diastolic HF, the chance of recovery is greater than with systolic HF, but less than in people with diastolic dysfunction without heart failure. Timely diagnosis and competent therapy can improve the prognosis of the disease.
Diastolic dysfunction is much more common than previously thought. This disease occurs in 15% of patients under the age of 50 years, and in 50% of people over 70 years of age. Therefore, we can say with confidence that the role of this disease in the development of heart failure is clearly underestimated.
Complete cure of diastolic dysfunction of the left ventricle cannot be achieved. To prolong the patient’s life, cardiologists recommend:
- seek professional help in a timely manner;
- do not interrupt the prescribed drug therapy (prescribed to correct problems of the circulatory system);
- undergo full treatment of the underlying pathological process;
- switch to the recommended diet;
- comply with work and rest requirements.
If the above conditions are met, the prognosis becomes favorable - patients return to their usual way of life for many years.
What lifestyle should a patient with ventricular dysfunction follow?
First of all, you need to follow a diet. You should limit the intake of table salt from food (no more than 1 gram per day) and control the amount of liquid you drink (no more than 1.5 liters per day) to reduce the load on the circulatory system. Nutrition should be rational, according to the eating regimen with a frequency of 4 - 6 times a day. Fatty, fried, spicy and salty foods are excluded. It is necessary to expand the consumption of vegetables, fruits, fermented milk, cereals and grain products.
The second point of non-drug treatment is lifestyle correction. It is necessary to give up all bad habits, observe a work-rest schedule and devote sufficient time to sleep at night.
The third point is sufficient physical activity. Physical activity must correspond to the general capabilities of the body. It is quite enough to take walks in the evening or sometimes go out to pick mushrooms or go fishing. In addition to positive emotions, this type of rest contributes to the good functioning of neurohumoral structures that regulate the activity of the heart. Of course, during the period of decompensation, or worsening of the disease, all stress should be excluded for a period determined by the doctor.