Content
Definition and general information [edit]
Sinus tachycardia is understood as an increase in heart rate above the age norm from 10 to 60%. An increase in heart rate from 10 to 20% above the age norm can be considered as moderate (grade I), from 20 to 40% as moderate (grade II) and from 40 to 60% as severe (grade III) sinus tachycardia. If the heart rate exceeds 210-220 per minute in young children and 150-160 per minute in school-age children, then in such cases it is necessary to differentiate sinus tachycardia from ectopic tachycardia. In this case, the nomotopic rhythm should be proven by the presence and polarity of the P wave in the corresponding leads, its constant amplitude and fixed PQ interval.
Sinus tachycardia can be physiological and pathological, and pathological - functional and organic.
Etiology and pathogenesis[edit]
Physiological tachycardia occurs during physical and psycho-emotional stress, transition to orthostasis, when the ambient temperature rises, after a large intake of food and liquid, in a stuffy room and during high-altitude hypoxia. It is characterized by a rapid (within 3-5 minutes) restoration of rhythm after the end of the load or exposure to environmental factors. Functional sinus tachycardia occurs with increased body temperature, hypoxemia associated with anemia or lung damage, with pheochromocytoma and thyrotoxicosis, and infectious toxicosis. Functional tachycardia is sometimes associated with VSD syndrome of the sympathotonic type. It can be characterized by a moderate increase in heart rate at rest and its inadequate increase in response to normal physical and psycho-emotional stress, and an extended time of restitution. Such functional sinus tachycardias occur more often in girls in the prepubertal period and are associated with the formation of hormonal balance, as well as with hypercatecholaminemia and hypersympathicotonia. Organic sinus tachycardia is caused by organic damage to the heart of an inflammatory, ischemic-necrotic, degenerative or dystrophic-fibrotic nature. Sinus tachycardia occurs with increased sensitivity to certain drugs (aminophylline, atropine, etc.).
Clinical manifestations[edit]
Sinus tachycardia is most often accompanied by an increase in IOC and coronary blood flow. However, with prolonged tachycardia and shortened diastole, a discrepancy between the coronary blood flow and the increased work of the heart is noted, resulting in the development of myocardial dystrophy.
Children tolerate moderate sinus tachycardia satisfactorily. But with severe tachycardia, complaints of palpitations, discomfort, and sometimes cardialgia appear. Physically, with functional tachycardia (hyperthermia, thyrotoxicosis, etc.), the first heart sound is increased, but with organic damage to the heart, sinus tachycardia is usually accompanied by a weakening of the first sound at the apex, an accentuation of the second sound over the pulmonary artery and other signs of heart failure.
Tachycardia, unspecified: Diagnosis[edit]
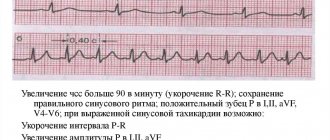
• Marked shortening or absence of the TR interval.
• The P wave is sinus, pointed, increased in amplitude and decreased in duration.
• Shortening of PR and QT intervals.
• Possible displacement below the ST segment isoline.
• Decrease in the amplitude of the T wave and increase in the amplitude of the U wave
Differential diagnosis[edit]
Severe sinus tachycardia should be differentiated from paroxysmal and, especially, non-paroxysmal tachycardia.
Tachycardia, unspecified: Treatment[edit]
Treatment consists of identifying and eliminating the cause. In most cases, β-blockers are used. Diltiazem and verapamil may be useful for thyrotoxicosis if β-blockers are contraindicated.
Treatment of inappropriate sinus tachycardia is symptomatic. Although there are no randomized, double-blind, placebo-controlled studies, β-blockers are considered the treatment of choice (Class I, Level of Evidence C).
Prevention[edit]
Other [edit]
Inappropriate sinus tachycardia
remains at rest regardless of or inconsistent with the level of physical, emotional, pathological or pharmacological stress. There are two main mechanisms for its occurrence: increased automatism of the sinus node and disruption of its regulation by the autonomic nervous system with a predominance of sympathetic tone.
Diagnostic criteria for inappropriate sinus tachycardia:
• persistent sinus tachycardia (heart rate >100 per minute) throughout the day with a pronounced increase in heart rate during activity and normalization of heart rate at night (according to 24-hour ECG monitoring);
• non-paroxysmal nature of tachycardia (and symptoms);
• morphology of P waves characteristic of sinus rhythm;
• absence of secondary causes of tachycardia (hyperthyroidism, pheochromocytoma, detraining, etc.).
Sinus tachycardia code according to ICD 10 in adults
An increase in heart rate can be either a physiological reaction of the body or a sign of serious pathology.
Sinus tachycardia (heart rate more than 100 per minute) is one of the most common forms of paroxysmal tachycardia, sinus tachycardia code according to ICD 10 I47.1. Cardiologists and general practitioners use the code of this disease according to the International Classification of Diseases, Tenth Revision, to record morbidity and correctly complete medical documentation.
Causes
The occurrence of tachycardia should not always be regarded as a manifestation of the disease. An increase in heart rate is a normal reaction to strong emotions (both positive and negative), physical activity, and lack of oxygen. Sinus tachycardia is also a consequence of the following pathological processes:
- external or internal bleeding;
- anemia of any etiology;
- hypotension;
- high fever;
- hyperfunction of the thyroid gland;
- dysfunction of the left ventricle of the heart;
- cardiopsychoneurosis.
An increase in heart rate in the presence of the above diseases occurs at rest and is often accompanied by other unpleasant symptoms.
Sometimes an increase in heart rate can be accompanied by arrhythmia (disturbance in the correct rhythm of heart contractions).
An increase in heart rate can occur with atrial and ventricular blockade, Wolff-Parkinson-White syndrome.
Diagnosis and treatment
Paroxysmal tachycardia in ICD 10 has code I47 and belongs to the section of heart diseases. If there is an increase in heart rate at rest, you should consult a physician or cardiologist.
A mandatory instrumental research method for patients with an increase in heart rate or rhythm disturbances is an ECG; echocardiography and a number of other studies are also additionally performed to determine the cause of the disease.
Tachycardia and bradycardia (heart rate less than 60 per minute) are serious symptoms, so you should consult a doctor promptly.
Treatment depends on the cause that caused the increase in heart rate, the presence of rhythm disturbances, and concomitant diseases. You also need to limit the consumption of caffeine, alcoholic beverages, and stop smoking. Lifestyle modification gives good results for all patients, regardless of the stage and severity of the underlying disease.
Save the link, or share useful information on social media. networks
Excluded:
- complicating: abortion, ectopic or molar pregnancy (O00-O07, O08.8)
- obstetric surgical interventions and procedures (O75.4)
- NOS (R00.0)
ICD-10 alphabetical indexes
External Causes of Injury - The terms in this section are not medical diagnoses, but rather a description of the circumstances under which the event occurred (Class XX. External Causes of Morbidity and Mortality. Heading Codes V01-Y98).
Medicines and chemicals - table of medicines and chemicals that have caused poisoning or other adverse reactions.
In Russia, the International Classification of Diseases, 10th revision (ICD-10) has been adopted as a single normative document for recording morbidity, reasons for the population's visits to medical institutions of all departments, and causes of death.
ICD-10 was introduced into healthcare practice throughout the Russian Federation in 1999 by order of the Russian Ministry of Health dated May 27, 1997 No. 170
The release of the new revision (ICD-11) is planned by WHO in 2022.
Abbreviations and symbols in the International Classification of Diseases, 10th Revision
NOS - no other indications.
NEC - not classified elsewhere.
†—code of the underlying disease. The main code in the dual coding system contains information about the underlying generalized disease.
* is an optional code. An additional code in the double coding system contains information about the manifestation of the main generalized disease in a separate organ or area of the body.
Sinus tachycardia - what does this diagnosis mean?
Have you been struggling with HYPERTENSION for many years without success?
Head of the Institute: “You will be amazed at how easy it is to cure hypertension by taking it every day.
The correct heart rhythm depends on the uniform occurrence of impulses in the sinus node and their conduction through the conduction system of fibers. The sinus node is a collection of nerve cells located in the atrium. It receives “commands” via a special nerve from the brain.
Next, the “instructions” are distributed along the nerve bundles. Thanks to the precise work, the contractions of the atria and ventricles, the filling (diastole) and contraction (systole) phases are coordinated. The endocrine system is involved in rhythm regulation through the hormone adrenaline and its derivatives.
Our readers successfully use ReCardio to treat hypertension. Seeing how popular this product is, we decided to bring it to your attention. Read more here...
The norm for sinus rhythm is the number of contractions ranging from 60 to 90 beats per minute. Sinus tachycardia is an increase in frequency over 90.
Sinus tachycardia is also called “normotopic” because it always depends on the main sinus, in contrast to “heterotopic”, which occurs due to increased activity of other nodes. This is how paroxysmal tachycardia is formed.
In this case, the heart rate (HR) will also be above 90, but the heart rhythm goes the wrong way, the work of different departments becomes uncoordinated and incomplete. This form is dangerous for the development of complications.
The terms “sinus tachycardia” and “sinusoidal”, used by inexperienced patients, are incorrect from a medical point of view.
Types of sinus tachycardia
The causes of sinus tachycardia have been studied quite well. They are not always associated with cardiac pathology. Moderate sinus tachycardia serves as a normal physiological mechanism for overcoming physical exertion and emotional stress. Depending on the predominance of causes, several varieties are distinguished.
Constitutional
It is relatively rare. Associated with a congenital disorder of excitation formation in the sinus node. A person suffers from tachycardia throughout his life. Heart rate in children is 120 per minute, in adolescents and adults it is 100 and higher.
Endocrine
Increased thyroid function during thyrotoxicosis leads to the production of excess thyroxine hormone. It speeds up the basal metabolism, heart rate and blood circulation speed.
Toxic
Sinus tachycardia is caused by substances such as atropine, adrenaline, caffeine, nicotine, alcohol, and digitalis.
This type of arrhythmia is characteristic of infectious diseases. Here, in addition to the toxic effect on the node, the following play a role:
- temperature increase;
- drop in blood pressure;
- anemia (decreased hemoglobin level).
It is believed that an increase in temperature by one degree causes an increase in heart rate by 8–10 beats per minute. Hypertension is accompanied by a decrease in heart rate; with low blood pressure, tachycardia is observed. Sinus tachycardia is especially pronounced in severe infections and septic conditions, in which all types of effects are combined.
Cardiogenic
This type of tachycardia is characteristic of the initial symptoms of heart failure. It occurs as a result of a compensatory mechanism that improves the supply of oxygen to tissues. Observed when
- myocardial infarction,
- heart aneurysm,
- endocarditis,
- heart defects,
- hypertensive crises,
- atherosclerosis of the coronary arteries.
Orthostatic
When moving from a lying position to an upright position, the heart rate increases. In people with a certain type of nervous system, this acceleration is very strong. Such manifestations are especially often observed during the period of recovery from various diseases, if a person has been forced to remain in bed for a long time.
Diagnostics
According to ICD-10 (International Classification of Diseases, Tenth Revision), sinus tachycardia is classified as class I 47.1, “supraventricular tachycardia.” The terminology adopted in Russia in this case does not contradict the ICD, but clarifies it.
Clinical manifestations of tachycardia from the sinus node in the form of palpitations, pulsating tinnitus, dizziness, shortness of breath are often symptoms of other diseases and are associated with neuroses.
The diagnosis can be made by a doctor after an electrocardiographic examination (ECG). Regular listening to the heart and counting the pulse can indicate an increase in heart rate, but does not say anything about the correct rhythm.
So the symptoms of sinus tachycardia can only be seen with a special study. The ECG is taken in the supine position. The pulses are recorded by electrodes and converted into a graphic image.
By the nature of the teeth, the length and position of the intervals, a doctor in a functional diagnostics office can judge many diseases, including the correctness of the rhythm.
Holter observation is carried out during the day in a cardiology hospital. This is important for diagnosis if no acceleration of the rhythm is recorded on the ECG.
Sometimes, to resolve the issue of a person’s suitability for work in difficult conditions (service in the army, in units of the Ministry of Internal Affairs, admission to a military school, contact with occupational hazards), a medical commission prescribes stress tests.
The most popular is to take an ECG before the test, then the patient is asked to do 20 squats at a moderate pace and an ECG is taken after the exercise. The increase in heart rate is used to judge the adaptive capabilities of the cardiovascular system.
A more thorough examination is carried out on specially equipped simulators. At the same time, not only the rhythm is monitored, but also other indicators of the functioning of different parts of the heart.
To eliminate sinus arrhythmia, it is often sufficient to carry out good treatment of the diseases that caused it (thyrotoxicosis, infectious diseases, hypertension, heart disease). When prescribing therapy, the doctor always takes into account the heart rate. Usually they warn about the need to control the pulse when treating with certain medications.
General procedures that strengthen the nervous system (massage, baths, showers), physiotherapeutic treatment simultaneously calm the patient and normalize arrhythmia. In complex neurogenic cases, consultations with a psychologist, treatment with hypnosis, and auto-training are recommended.
If palpitations occur, there is a well-known method of self-help: try to breathe deeply, after several breathing movements, hold your breath at the height of inspiration, tighten your abdominal muscles. This simple method helps to cope with tachycardia.
People's recommendations
- lemon balm herb,
- hawthorn flowers and fruits,
- viburnum berries,
- valerian root.
You can prepare them without a steam bath, pour a tablespoon of crushed raw materials into a half-liter thermos and pour boiling water. Leave it overnight or for 5 – 6 hours.
After straining, drink before meals throughout the day, combine with honey. Hawthorn can be purchased at the pharmacy in the form of an alcohol tincture. It can be added to tea 10 - 15 drops.
We should not forget that prolonged tachycardia is dangerous due to its consequences. Incomplete and incorrect contraction of the heart muscle causes it to overstrain, requires more oxygen, and disrupts the delivery of blood to the brain. An examination by a specialist doctor should be carried out as early as possible. Timely initiation of treatment will prevent the development of serious diseases.
Drugs for the treatment of sinus tachycardia
Normal heart rate in children and adults
- Treatment of joints
- Weight loss
- Varicose veins
- Nail fungus
- Fighting wrinkles
- High blood pressure (hypertension)
Source: https://serdce-moe.ru/zabolevaniya/tahikardiya/sinusovaya-tahikardiya-kod-po-mkb-10-u-vzroslyh
What you need to know about sinus tachycardia? Cardiologists' opinion
Sinus tachycardia consists of rapid contractions of the heart.
This condition can be either situational (paroximal) or long-term (non-paroxymal or chronic). Most often, the disease occurs as a reaction to extracardiac stimuli. An early correct diagnosis based on the symptoms below and timely treatment will avoid the development of complications. In the article we will consider this deviation of the heart rhythm: what does it mean and how to detect it in time in children and adults (men and women) of different ages?
What it is?
Sinus (sinusoidal or sinusoidal) tachycardia is diagnosed regardless of the age and gender of the patient. Often it can be accompanied by hyperthyroidism , that is, an increase in the amount of hormones in the thyroid gland, and anemia - a decrease in hemoglobin levels.
In most cases, the disease does not have pronounced clinical manifestations. The patient has:
- dizziness;
- increased heart rate;
- pain in the sternum;
- low performance;
- general weakness;
- dyspnea.
An electrocardiogram is used for diagnosis. On the ECG interpretation, the rhythm change in question is characterized by the following signs:
- increase in heart rate - more than 100 beats per minute;
- indicators of sinus rhythm (sinus rhythm) are normal;
- positive P wave in leads I, II, aVF, V4-V6.
Symptoms
Paroxysms during supraventricular tachycardia can last from several seconds to several days; the duration of the attack is directly influenced by the cause of the pathology.
The clinical picture of the disease is as follows:
- a sharp increase in the frequency of rhythmic contractions of the heart;
- darkening of the eyes, dizziness, lightheadedness or fainting;
- trembling of the upper extremities;
- speech disorders;
- temporary unilateral muscle paralysis;
- increased work of the sebaceous glands;
- active contraction of blood vessels, which can be seen with the naked eye;
- rapid fatigue and deterioration in performance;
- frequent urination;
- shallow breathing.
It must be said that supraventricular tachycardia is not accompanied by severe symptoms in all cases, and even the presence of symptoms may vary from person to person. In old age, patients very rarely notice any signs of the disease, and the pathology is most often diagnosed accidentally, during a routine ECG.
During pregnancy , supraventricular tachycardia is observed quite often, this is explained by hormonal imbalances and changes.
Reasons for development
The disease occurs in different age groups. Most often, sinus tachycardia is observed in patients with cardiac abnormalities . This is facilitated by cardiac and extracardiac etiological factors.
In patients with heart and vascular diseases, sinus tachycardia may indicate early heart failure or the development of left ventricular dysfunction.
Intracardiac causes of the disease:
- heart attack;
- severe angina;
- heart disease;
- rheumatic myocarditis;
- bacterial endocarditis;
- congestive heart failure.
The development of the deviation is facilitated by severe emotional stress, the presence of congenital defects and heavy physical exertion.
Other causes of the disease include:
- anemia;
- endocrine disorders;
- acute episodes of pain;
- vascular insufficiency in acute form;
- hypoxemia.
Fever and infectious-inflammatory diseases contribute to the formation of a pathological condition.
The toxic and drug-induced form of sinus tachycardia occurs when taking:
- vagolytics;
- corticosteroids;
- sympathomimetics;
- diuretics;
- caffeine;
- nicotine;
- antihypertensive drugs;
- poison;
- alcohol.
According to the type of severity of symptoms, the considered cardiac arrhythmia (HRA) can be:
- moderate – most often occurs in children under 6 years of age or in adolescents, during the period of active hormonal changes. The moderate form has rather mild manifestations, so it should not cause discomfort or cause concern.
- pronounced - can be diagnosed in both children and older people. It occurs against the background of a malfunction of the cardiovascular system. If pronounced tachycardia is combined with bradycardia, this may indicate neurosis. In this case, the doctor prescribes appropriate drug treatment.
Diagnostic methods
The main method for diagnosing tachycardia is electrocardiography (ECG). Sensors are placed on the patient's chest and arms that send electrical signals through the heart. On the monitor screen you can see the averaging of all vectors of action potentials, which appears during the work of the heart muscle.
Using an ECG, a specialist can easily determine the type of arrhythmia and draw a conclusion about the influence of associated factors on the functioning of the heart. The results of the study may indicate problems such as hypertrophy of the right or left ventricle, myocardial infarction, chronic myocardial ischemia.
Other informative diagnostic methods include:
- Daily Holter ECG monitoring allows you to track changes in heart activity in a person’s everyday life. It is used at home and allows you to record the slightest changes in the load of the heart muscle. Recording is carried out through a special portable device, consisting of a recorder worn on the shoulder or belt. Contact with the body is carried out through adhesive electrodes. Daily ECG monitoring allows you to identify episodes of painful or silent myocardial ischemia, analyze the cause-and-effect relationships of fainting states, etc.
- Echocardiography is performed in real time. Allows you to identify intracardiac pathology, assess the condition of soft tissues and valve apparatus, and also measure the thickness of the walls of the heart and its volume. Thanks to the use of echocardiography, it is possible to monitor the characteristics of the movement and speed of blood in the atria and ventricles.
- An electrophysiological study of the heart allows us to understand how an electrical impulse penetrates the heart muscle, at what speed and what features this process is characterized by. Thanks to this type of study, cardiac conduction disturbances become visible and the mechanisms of tachycardia are revealed. The effectiveness of non-pharmacological and drug therapy is also successfully monitored.
Reference Information! Additional diagnostic methods are EEG of the brain, complete blood count, blood test for thyroid hormone levels and other tests that the doctor prescribes to the patient based on the results of basic studies.
What are the dangerous consequences?
The danger of the disease depends on its form. For example, a mild physiological form should not cause any particular concern. Pathological sinus tachycardia indicates the development of a number of serious diseases:
The paroxysmal form of the disease is also dangerous for the patient. It leads to disruptions in the functioning of the atrioventricular node mechanism. An irregular heart rhythm in both adults and children causes the development of arrhythmia.
Treatment
In most cases, treatment specifically for sinus tachycardia is not required. Therapy is aimed at eliminating the cause of the arrhythmia. Typically this means quitting smoking, alcohol or coffee.
Drug treatment is carried out in cases where the syndrome causes angina attacks, which in turn provokes insufficient blood circulation.
For highly symptomatic disease or resistance to drug therapy, radiofrequency catheter ablation of the sinus node is performed, and a permanent electrical stimulator is installed.
Drugs
The choice of drugs for drug therapy depends on the causes of the pathology. Therapy should be aimed at eliminating the primary disease. The doctor selects the type of medication, dosage and duration of the therapeutic course individually for the patient.
For treatment, the following groups of drugs are prescribed:
- beta blockers;
- non-dihydropyridine calcium antagonists;
- auxiliary medications depending on the underlying disease.
The action of beta blockers is aimed at reducing the levels of adrenaline and norepinephrine. These hormones cause stress, which has a negative effect on the heart muscle.
The most commonly prescribed drug is Bisoprolol. Most patients respond normally to it, but sometimes severe side effects may occur.
The group of non-dihydropyridine calcium antagonists is represented by the drugs Verapamil and Diltiazem.
The tablets can reduce atrial conductivity, reduce heart rate, and also reduce the contractile activity of the heart muscle. Auxiliary drugs are prescribed depending on the primary disease:
- neurosis, depression - sedatives;
- hyperthyroidism – medications that suppress the production of thyroid hormones;
- sore throat - an antibiotic with a wide spectrum of action;
- anemia - products that contain iron.
Surgical methods
Sinus tachycardia can acquire a malignant course that cannot be corrected with drug therapy. In order to prevent disruption of the heart due to coronary insufficiency, surgical intervention is performed. To do this, one of the following procedures is carried out:
- cardiac intervention – full-fledged cardiac surgery involves stenting, bypass surgery and angioplasty of narrow arteries. As a result, normal blood flow through the vessels of the heart is restored.
- Radiofrequency ablation is a modern and effective method of surgical intervention. It involves cauterizing pathological lesions in the heart.
- implantation of a pacemaker allows you to avoid a number of serious deviations that can threaten the patient’s life. The procedure is carried out quite quickly. If it is not carried out, sinus tachycardia will progress, thereby provoking the development of other diseases.
Traditional methods
For sinus tachycardia, treatment with folk remedies is often used. The most commonly used herbal mixture is motherwort and valerian, as well as lemon balm tincture.
To prepare the herbal mixture you will need dried valerian root, dried motherwort herb, yarrow herb and anise fruits. All components are crushed and mixed. To use this medicine, you need to pour it into 1 tbsp. collecting 300 ml of boiling water. The product should be infused in a thermos for an hour. It must be taken in equal portions throughout the day.
Melissa tincture has a calming effect. For 100 g of dry base, take 200 ml of alcohol. The medicine must be infused for 10 days. It must be strained before use. The tincture is taken 4 times a day: 1 tsp. The product is diluted in 50 ml of water.
For sinus tachycardia, doctors recommend drinking herbal teas. Oregano, rose hips, mint and valerian can be used to prepare them.
First degree atrioventricular block
Upon diagnosis
Level of consciousness, respiratory rate and efficiency, heart rate, pulse, blood pressure, ECG, medical history if possible
Additional (according to indications)
Laboratory tests: hemoglobin, blood gases, CBS indicators,
electrolytes (K, Na, Mg, Ca, Cl), blood glucose, leukocytes, blood count, CPK enzymes, ALT, AST
R-graphy of the chest organs
During treatment
Monitoring in accordance with clause 1.5. Repeatedly according to indications - ECG, laboratory parameters, depending on the clinical situation
Discontinuation of drugs that prolong the PQ interval on the ECG. Ensuring adequate ventilation, oxygen inhalation, intravenous access
Atropine 0.5-1 mg IV, up to a total dose of 0.04 mg/kg
Percutaneous external pacing, if not possible or as a temporary alternative until transvenous pacing is provided - dopamine 5-20 mcg/kg/min. adrenaline 2-10 mcg/min. as a continuous dosed infusion
Correction of water and electrolyte balance
Extracardial pathological sinus tachycardia occurs with increased body temperature, acidosis, hypoglycemia, hypoxemia associated with anemia or lung damage, with pheochromocytoma and thyrotoxicosis, infectious toxicosis (neurotoxicosis when taking or overdose of drugs: adrenaline, isadrine, aminophylline, atropine, inhalation of large doses 2-adrenergic receptor agonists (terbutaline, salbutamol, etc.).
Lymphostasis, chronic fatigue syndrome. Osteopathy helps at any age. Treatment by an osteopath will be useful even for infants - two or three treatment sessions can help restore normal sleep and relieve causeless whims and anxiety. A course of pediatric osteopathy helps improve the child’s appetite, helps normalize reflexes and muscle tone.
Types, causes, symptoms and treatment of arrhythmia
Have you been struggling with HYPERTENSION for many years without success?
Head of the Institute: “You will be amazed at how easy it is to cure hypertension by taking it every day.
Arrhythmia is a condition in which the frequency, strength and sequence of heart contractions change. In the International Classification of Diseases, 10th revision (ICD-10), arrhythmia is assigned class 149 - Other cardiac arrhythmias. According to ICD-10, we can distinguish:
- Ventricular fibrillation and flutter - 149.0 (ICD-10 code).
- Premature atrial depolarization - 149.1.
- Premature depolarization emanating from the atrioventricular junction - 149.2.
- Premature ventricular depolarization - 149.3.
- Other and unspecified premature depolarization - 149.4.
- Sick sinus syndrome (bradycardia, tachycardia) - 149.5.
- Other specified cardiac arrhythmias (ectopic, nodular, coronary sinus) - 149.8.
- Unspecified rhythm disturbance - 149.9.
This ICD-10 class excludes unspecified bradycardia (code R00.1), arrhythmia in newborns (P29.1), as well as arrhythmia complicating pregnancy, abortion (O00-O07) and obstetric operations (O75.4).
In most cases, arrhythmia involves an abnormal heart rhythm even when the heart rate is normal. Bradyarrhythmia is an abnormal rhythm accompanied by a slow heart rate not exceeding 60 beats per minute. If the contraction frequency exceeds 100 beats per minute, then we are talking about tachyarrhythmia.
Types of arrhythmia and reasons for their development
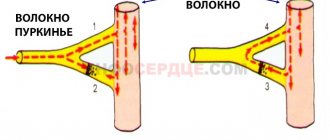
To find out the causes of rhythm disturbances, it is necessary to understand the nature of the normal rhythm of the heart. The latter is provided by a conducting system consisting of a system of successive nodes formed from highly functional cells. These cells provide the ability to create electrical impulses passing along each fiber and bundle of the heart muscle. Such impulses ensure its reduction. The sinus node, located in the upper part of the right atrium, is responsible for the generation of impulses to a greater extent. Heart contraction occurs in several stages:
- Impulses from the sinus node spread to the atria and the atrioventricular node.
- At the atrioventricular node, the impulse slows down, allowing the atria to contract and pump blood into the ventricles.
- Next, the impulse passes through the branches of the His bundle: the right one conducts impulses passing through the Purkinje fibers to the right ventricle, the left one to the left ventricle. As a result, the mechanism of excitation and contraction of the ventricles is triggered.
If all structures of the heart function smoothly, the rhythm will be normal. Rhythm disturbances occur due to pathology of one of the components of the conduction system or due to problems with the conduction of impulses along the muscle fibers of the heart.
There are the following types of arrhythmia:
- Extrasystoles are premature contractions of the heart, the impulse in which does not come from the sinus node.
- Atrial fibrillation, or atrial fibrillation, is a heart rhythm disturbance caused by disordered excitation and contraction of atrial fibers.
- Sinus arrhythmia is caused by an abnormal sinus rhythm, accompanied by alternating deceleration and acceleration.
- Atrial flutter is an increase in the frequency of atrial contractions up to 400 beats per minute, combined with their regular rhythm.
- Supraventricular tachycardia forms within a small area of atrium tissue. Atrial conduction disturbance is observed.
- Ventricular tachycardia is an acceleration of the heart rate coming from the ventricles, due to which they do not have time to fill with blood normally.
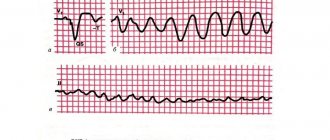
- Ventricular fibrillation is a chaotic fluttering of the ventricles, provoked by a flow of impulses from them. This condition makes it impossible for the ventricles to contract and, accordingly, further pumping blood. This is the most dangerous type of rhythm disturbance, as a person falls into a state of clinical death within a few minutes.
- Sinus node dysfunction syndrome is a violation of the formation of an impulse in the sinus node and its transition to the atria. This type of arrhythmia can provoke cardiac arrest.
- The blockade occurs against the background of a slowdown in the conduction of the impulse or its cessation. They can manifest themselves in both the ventricles and atria.
Paroxysmal supraventricular tachycardia – Tachycardia supraventricularis paroxismalis
(NB! Cardiograms were taken at a speed of 25 mm/s, so all sizes are halved.
) Criteria: The rhythm is correct with a frequency of 120-250 per minute, the RR interval is constant, the QRS complexes are narrow (QRS less than 0.12 s).
Depending on the frequency of tachycardia and its location, P waves may precede, overlap or follow the QRS complex. In this example, the P waves are practically invisible.
Paroxysmal supraventricular tachycardias are paroxysmal disturbances of the heart rhythm, characterized by a high heart rate (150-250 per minute) and, in most cases, a regular rhythm.
According to pathogenesis, they distinguish: re-entry
or circular movement of the impulse, trigger, pathological automatism and additional pathways. The EMS does not differentiate supraventricular tachycardia into atrial and atrioventricular.
For practical reasons, supraventricular tachycardia with QRS complexes
and tachycardia with
wide QRS.
The importance of this difference is due to the fact that with wide QRS
There may be additional conduction pathways (WPW syndrome), in which the administration of drugs that slow down AV conduction (verapamil, digoxin) is contraindicated due to the risk of developing ventricular fibrillation.
Treatment
Non-drug therapy
Against the background of stable hemodynamics and clear consciousness of the patient, relief of paroxysm begins with techniques aimed at irritating the vagus nerve and slowing down conduction through the atrioventricular node. Vagal tests are contraindicated in the presence of acute coronary syndrome, suspected pulmonary embolism, or in pregnant women.
Vagal tests
■ Holding your breath. ■ Forced cough. ■ Sharp straining after a deep breath (Valsalva maneuver). ■ Stimulation of vomiting by pressing on the root of the tongue. ■ Swallowing a crust of bread.
■ Immersion of the face in ice water (“diving dog reflex”); ■ The Aschoff test (pressure on the eyeballs) is not recommended due to the risk of retinal damage; ■ Massage of the carotid sinus is permissible only if you are sure that there is no insufficiency of blood supply to the brain (usually in young patients).
These techniques are not always effective for supraventricular tachycardia. With atrial fibrillation and flutter, they cause a transient decrease in heart rate, and with ventricular tachycardia they are generally ineffective.
The heart rate response to vagal tests serves as one of the differential diagnostic criteria to distinguish ventricular tachycardia from supraventricular tachycardia with widened QRS complexes.
With supraventricular tachycardia, the heart rate decreases, while with the ventricular rhythm remains the same.
Drug therapy
Relief of supraventricular tachycardia can be started with one of three drugs: adenosine, verapamil (only with narrow QRS complexes),
procainamide If other therapy is impossible, WPW syndrome, against the background of coronary or heart failure, the use of amiodarone (delayed onset of effect) is permissible.
■ Adenosine
a dose of 6 mg is administered intravenously as a bolus over 1-3 s, then sodium chloride solution 0.9% - 20 ml and the limb is raised. As a rule, it is possible to stop paroxysmal supraventricular tachycardia within 20-40 s after administration.
If there is no effect, 12 mg (3 ml) of adenosine is reintroduced after 2 minutes and, if after 2 minutes the rhythm has not been restored, 12 mg (3 ml) of adenosine is reintroduced. The drug is low-toxic, the most common side effects (usually with slow administration): hyperemia, dyspnea, chest pain, bronchospasm.
In approximately 50% of cases, a 3-15 second asystole occurs, and in 0.2-3% of cases, the asystole can last more than 15 seconds, which may require a precordial beat and even chest compressions (usually only a few are required). massage movements).
The risk of developing such complications is the reason why the use of adenosine in the EMS is permissible only with control of rhythm, blood pressure, heart rate and ECG monitoring. The effectiveness of adenosine in supraventricular tachycardia reaches 90%.
Administration of adenosine intravenously also makes it possible to differentiate atrial flutter with 1:1 conduction from supraventricular tachycardia; inhibition of AV conduction makes it possible to identify characteristic flutter waves (“saw”), but the rhythm is not restored.
■ Verapamil
(only for narrow
QRS complexes)
is administered intravenously as a bolus at a dose of 2.5-5 mg over 2-4 minutes (to avoid the development of collapse or severe bradycardia) with possible repeated administration of 5-10 mg after 15-30 minutes if tachycardia persists and the absence of hypotension. It is necessary to monitor heart rate, blood pressure, and ECG.
Side effects of verapamil include: arterial hypotension (up to collapse with rapid intravenous administration due to peripheral vasodilation and negative inotropic effect); bradycardia (up to asystole with rapid intravenous administration due to suppression of the automatism of the sinus node); AV block (up to complete transverse with rapid intravenous administration); transient ventricular extrasystole (self-limited); increase or appearance of signs of heart failure (due to negative inotropic effects), pulmonary edema. Before using verapamil, you should clarify the anamnestic indications for WPW syndrome and/or evaluate previous ECGs with sinus rhythm ( PQ
less than 0.12 s, the
QRS
is widened, a delta wave is detected). Contraindications to the use of verapamil are: WPW syndrome, arterial hypotension (SBP less than 90 mm Hg), cardiogenic shock, chronic and acute heart failure, as well as in patients taking β-blockers due to the high risk of developing complete AV- blockade or asystole.
■ Procainamide
(novocainamide*) 10% - 10 ml (1000 mg) diluted with 0.9% sodium chloride solution to 20 ml (concentration 50 mg/ml) and administered IV slowly at a rate of 50 mg/min for 20 minutes at constant monitoring of rhythm, heart rate, blood pressure and ECG. When sinus rhythm is restored, drug administration is stopped.
To prevent a decrease in blood pressure, administration is carried out in a horizontal position of the patient. Side effects more often occur with rapid intravenous administration: collapse, disturbance of atrial or intraventricular conduction, ventricular arrhythmias, dizziness, weakness.
The use of procainamide is contraindicated in cases of arterial hypotension, cardiogenic shock, severe heart failure, and prolongation of the QT interval.
In Russia, when administering procainamide to correct hypotension, it is practiced to use phenylephrine (for example, mezaton* 1% - 0.1-0.3 ml).
The action begins immediately after intravenous administration and continues for 5-20 minutes. However, it should be remembered that the drug can cause ventricular fibrillation, angina, and dyspnea.
Phenylephrine is contraindicated in children under 15 years of age, pregnant women, ventricular fibrillation, acute myocardial infarction, hypovolemia; Use with caution for fibrillation, angle-closure glaucoma, tachyarrhythmia; occlusive vascular diseases (including a history), atherosclerosis, thyrotoxicosis, in the elderly.
Indications for hospitalization
■ The appearance of complications that required electrical pulse therapy.
■ Newly registered rhythm disturbances.
■ Lack of effect from drug therapy (only one arrhythmic drug is used at the prehospital stage).
■ Frequently recurrent rhythm disturbances.
Recommendations for sick people left at home
■ Limit the consumption of coffee, strong tea, and eliminate alcohol and smoking.
■ Contact your local physician to decide on further tactics and the need for examination, correction of treatment and consultation with specialists (cardiologist).
Common errors
■ Refusal to carry out electrical pulse therapy in case of unstable hemodynamics.
■ Use of unsafe vagal tests: pressure on the eyeballs, massage of the carotid sinus, pressure on the solar plexus area.
■ Impaired rate of administration of antiarrhythmics. In particular, intravenous administration of adenosine is too slow - more than 3 seconds, at the same time - too fast
intravenous administration of verapamil, procainamide (procainamide).
■ Use of verapamil, digoxin for WPW syndrome (wide QRS complexes).
■ Simultaneous combination of several drugs that slow down AV conduction. In particular, if verapamil is ineffective, procainamide (procainamide*) can be prescribed, only not earlier than 15 minutes after its administration, provided that stable hemodynamics are maintained.
■ Prescribing verapamil to patients taking β-blockers.
■ Prophylactic use of phenylephrine (mesatone) with initially normal blood pressure, as well as insufficient knowledge of contraindications to this drug.
Clinical examples
Man, 41 years old. Complains of palpitations, weakness, dizziness.
This state lasts for half an hour. Suffers from a congenital heart defect – patent foramen ovale. Rarely there are attacks of palpitations. Takes verapamil. Objectively: The condition is severe, consciousness is clear. The skin is pale, of normal moisture. Blood pressure = 80/60 mm. Heart rate 210 per minute. Vesicular breathing. The abdomen is soft and painless. The ECG shows supraventricular tachycardia. D.S.
Supraventricular paroxysmal tachycardia. (I47.1) 200 ml of saline solution and 0.2 ml of 1% mesatone solution were injected intravenously through the catheter. At the stage of mesatone administration, the rhythm was restored on its own. A repeat ECG shows sinus rhythm, heart rate 65 per minute. Blood pressure – 130/80 mm Hg. The patient was left at home.
~~~
Woman 62 years old. Complaints of palpitations, general weakness. This morning, about an hour ago, palpitations and dizziness appeared in an upright position. Periodically, there are attacks of palpitations, which are relieved by intravenous administration of verapamil. He suffers from coronary artery disease. Doesn't take medications regularly. Availability of other records.
Denies diseases and drug allergies. Habitual blood pressure is 130/80 mm. Objectively. Consciousness is clear. The skin and mucous membranes are pale, of normal moisture. Vesicular breathing. Heart rate is 180 per minute, the rhythm is correct. Blood pressure 100/80 mm Hg. The abdomen is soft and painless. The ECG shows supraventricular tachycardia.
Ds.
Supraventricular paroxysmal tachycardia
The intravenous administration of 4 ml of 0.25% verapamil solution without dilution was started slowly (within 1-2 minutes). After administering 3 ml, the rhythm was restored. She noted an improvement in her health. Blood pressure 120/70 mm, heart rate 85 per minute.
Left at home.
“,”author”:””,”date_published”:”2020-03-17T18:32:00.000Z”,”lead_image_url”:”//4.bp.blogspot.com/-fiX8Uw-48eE/Th9Kz8yj9eI/AAAAAAAAABbc/ iVvL_mfl5XY/w1200-h630-pk-no-nu/%25D0%25BD%25D0%25B0%25D0%25B4%25D0%25B6%25D0%25B5%25D0%25BB%2B%25D1%2582%25D0%25B0%25D1%2585show .php.jpeg”,”dek”:NULL,”next_page_url”:NULL,”url”:”//ambulance-russia.blogspot.com/2011/10/blog-post_4415.html”,”domain”:”ambulance -russia.blogspot.com”,”excerpt”:”бДог Ñ Ñ‚Ð°Ð½Ð´Ð°Ñ€Ñ‚Ð°Ñ… Ñ ÐºÐ¾Ñ€Ð¾Ð¹ медициР½Ñ кой п¾Ð¼Ð¾Ñ‰Ð¸, Ñ Ñ‚Ð°Ð½Ð´Ð°Ñ€Ñ‚Ñ‹ Ñ ÐºÐ¾Ñ€Ð¾Ð¹ п¾Ð¼Ð¾Ñ‰Ð¸,”,”word_count”:1274,” direction”:”ltr”,” total_pages”:1,”rendered_pages”:1}
Source: //ambulance-russia.blogspot.com/2011/10/blog-post_4415.html