Causes of arrhythmia
Heart rhythm disturbances (causes, symptoms and treatment are described later in the article) are often diagnosed in completely healthy people.
Predisposing factors that provoke arrhythmia can be divided into 2 categories:
- primary pathologies;
- disorders of the cardiac conduction system.
Primary diseases that can provoke arrhythmia include the following pathologies:
- heart defects (including congenital);
- heart failure;
- atherosclerosis.
Causes of heart rhythm disturbances
People who systematically abuse alcohol, drugs and tobacco products are at risk. Heart rhythm is often disturbed due to senseless and uncontrolled use of medications (during self-diagnosis and self-medication).
If the functioning of the cardiac conduction system is disrupted, blood circulation is disrupted. It is formed by several nodes, each of which is a cluster of cells that create and conduct electrical impulses to the fibers. In the upper part of the right atrium is the sinus node (Kis Flak node).
It controls heart contractions. Sinus rhythm is considered normal if a person’s pulse does not exceed 80-85 beats per minute. Any deviations (to a lesser or greater direction) are called arrhythmia.
Slow heart rate
Heart rhythm disturbances (the symptoms, causes and treatment presented below cannot be considered a call for self-diagnosis) can be caused by psycho-emotional disorders. There are physiological and pathological causes of slow heart rate.
Category 1 includes:
- playing sports;
- state of sleep or rest;
- lack of vitamins, macro- and microelements in the body.
Pathological causes include the following diseases:
- malignant tumors in the heart area;
- surgical interventions;
- heart disease;
- cardiosclerosis;
- myocarditis;
- myocardial dystrophy;
- neurocirculatory dystonia.
People at risk are those suffering from:
- endocrine system disorders;
- ulcerative lesions of the duodenum and stomach;
- intracranial hypertension.
A slowing of the pulse is observed with the development of intoxication caused by taking medications or poisoning with chemicals.
Heart rate acceleration
Heart palpitations occur for a number of reasons.
Predisposing factors include:
- natural;
- cardiological;
- extracardiac.
Natural reasons:
- Stress. In a stressful situation, corticosteroids and catecholamines are released into the blood. Under the influence of hormones synthesized by the pituitary gland and the adrenal cortex, blood vessels constrict and blood pressure increases. This leads to increased heart rate.
- Fright. In this case, adrenaline, cortisol and norepinephrine are released into the blood. Their concentration increases in a few seconds, which provokes an immediate increase in heart rate. The condition is temporary, it goes away in 3-5 minutes. on one's own.
- Physical activity. An increase in heart rate is observed during training. In this state, 110-120 beats per minute is considered normal.
- Abuse of caffeinated drinks. They contain substances that can speed up the pulse. To normalize your heart rate, you need to avoid drinking coffee and energy drinks.
- Pregnancy. During pregnancy, the heart rate increases. Without a cardiac examination, it is difficult to determine the cause of the disorder. Each case is individual.
Cardiac factors:
- Stenosis of the artery and aorta. Blood flow is impaired due to blockage of blood vessels by fatty plaques. The heart rate increases in direct proportion to the increase in blood pressure.
- Mitral valve stenosis. Narrowing of the lumen of the mitral valve leads to an increase in pulse.
- Heart failure (chronic or acute). In this case, the organ is not able to saturate the body with blood. To maintain activity, the heart is forced to speed up its contraction rate.
Extracardiac factors:
- Cachexia. Increased heart rate is observed in people who abuse diets. In the absence of appetite and weight loss, the body destroys lipid deposits.
- Neurological conditions. Rapid heartbeat is observed due to poor circulation in the brain or the growth of tumors in it.
Vertebrobasilar insufficiency develops against the background of osteochondrosis. In addition to increased heart rate, patients complain of vertigo, nausea and headache.
Irregular contractions
An uneven heart rate can be caused by the following factors:
- potassium deficiency in the body;
- psychoemotional disorders;
- abuse of caffeinated drinks;
- low blood glucose levels.
An uneven pulse is diagnosed with pathological changes in the functioning of the cardiovascular system.
These include:
- cardiomyopathy;
- heart disease;
- coronary heart disease.
To stabilize the patient’s well-being, medication is prescribed. In severe cases, surgical intervention is prescribed.
Atrial flutter
With this diagnosis, the heart rate increases to 200-400 contractions, for example, against the background of the correct atrial rhythm.
The reasons here, as a rule, are organic heart disease, heart surgery (especially the first week after the intervention). Often, hypertension and myocardial dystrophy can provoke atrial flutter.
Risk groups include men over 60 years of age, smokers, people with a lack of potassium or excessive production of thyroid hormones. An attack of such arrhythmia can be caused by extreme heat, physical strain, stress, or the use of alcohol or drugs.
Symptoms are a strong increase in heart rate, weakness, a sharp decrease in pressure with the development of a semi-fainting state, dizziness. Along with this, pulsation of the veins in the neck is often observed.
How to determine on an ECG. On the ECG, flutter is indicated by F-waves appearing instead of the P wave. Heart rate is 240-350 beats per minute. There is also atypical flutter, in which the same waves occur at a heart rate of 340-430 beats.
Classification of heart rhythm disorders
Heart rhythm disturbances (symptoms, causes and treatment - individual factors) are classified according to characteristic features.
Main types:
- sinus tachycardia;
- bradycardia;
- ventricular and atrial fibrillation;
- extrasystole;
- AV block;
- paroxysmal tachycardia.
Arrhythmia often occurs against the background of neurological disorders. Most often, this type of pathology is diagnosed in women.
Diagnosis of arrhythmia
Some types of arrhythmia are absolutely not noticeable by humans, so they can be identified using such types of diagnostics as:
— electrocardiography (ECG); - echocardiography; — daily or multi-day ECG monitoring; - Ultrasound.
Read also Brucellosis - first signs, symptoms, causes, treatment and prevention of brucellosis
The most important method for diagnosing arrhythmia is, of course, an ECG. But it cannot always show arrhythmia, since it shows the heart rate only for the period of time in which it is written, and attacks of arrhythmia can occur suddenly and be short-lived.
Signs of pathologies
Heart rhythm disturbances (the symptoms, causes and treatment described in this article cannot be considered a guide to self-diagnosis) are accompanied by characteristic signs. They may vary depending on the type of pathology. The patient may experience dizziness during the attack.
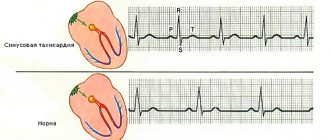
Manifestations of sinus tachycardia
Sinus tachycardia is accompanied by increased heart rate (over 90 beats per minute). This disorder is diagnosed less frequently in children than in adults.
The severity of characteristic symptoms directly depends on the following aspects:
- duration of the attack;
- severity of the course;
- the presence of predisposing factors.
If sinus tachycardia occurs in a mild form, then the symptom complex is almost completely absent.
Moderate pathology is also often asymptomatic, but sometimes the following signs may indicate the development of the disease:
- mood swings;
- fatigue, fatigue;
- sleep disturbance;
- dyspnea;
- feeling of stiffness or discomfort in the sternum;
- pounding in the ears.
Sinus tachycardia, which occurs in severe form, is accompanied by the following symptoms:
- disturbance of the outflow of urine (including a decrease in its volume);
- numbness of the limbs;
- decreased blood pressure;
- fainting;
- loss of appetite;
- aversion to food;
- prolonged insomnia;
- shortness of breath that occurs at rest;
- attacks of suffocation;
- pain in the left hypochondrium;
- dizziness.
If a person suddenly loses consciousness, then first of all their pulse is felt. Provided that the heart rate is increased, it is necessary to call an ambulance as soon as possible.
Symptoms of bradycardia (decreased heart rate)
With bradycardia, a decrease in heart rate is observed (less than 60 times per minute).
Characteristic symptoms of the pathology include:
- black spots before the eyes;
- increased sweating;
- dizziness;
- noise in ears;
- confusion;
- inability to concentrate attention on a specific subject;
- partial amnesia;
- pain in the chest area;
- blood pressure surges;
- drowsiness, fatigue.
If the patient's pulse has dropped to 35-40 beats per minute, then the risk of developing Adams-Stokes syndrome is quite high.
Characteristic signs of pathology include:
- dilated pupils;
- blue discoloration of the nasolabial triangle;
- panic attacks, overexcitement.
When the heart rate decreases to 30-35 beats per minute. the person loses consciousness, convulsions appear, and blood circulation in the brain is disrupted. The condition is life-threatening.
Atrial or ventricular fibrillation
Against the background of ventricular fibrillation, the pulse increases to 450-480 beats per minute. The reduction is unproductive, chaotic and irregular. The condition is life-threatening; a person’s heart may stop if help is not provided.
Symptoms of fibrillation include:
- weakness and dizziness appearing after 5-7 seconds. after the onset of the attack;
- loss of consciousness after 17-20 seconds;
- occurrence of tonic convulsions after 40 seconds;
- relaxation of the sphincters, dilation of the pupils after 50-70 seconds.
After 1.5 min. after the onset of the attack, the patient is diagnosed with clinical death. Resuscitation actions must be carried out within 1.5-2 minutes to restore brain function.
With the development of ventricular fibrillation, the patient begins to breathe noisily. In clinical death, the pulse in the carotid arteries is practically not palpable. The pupils are dilated, the skin becomes pale gray.
Extrasystole
The symptom complex of extrasystole can vary depending on the patient’s well-being, his age and the causes of the development of disorders. Isolated attacks that occur due to stress or abuse of caffeine-containing drinks may be asymptomatic. Occasionally a person feels sharp shocks of the myocardium, often painful.
Clinical picture for extrasystoles that developed against the background of pathologies of the cardiovascular system:
- weak thready pulse;
- pain in the chest and left hypochondrium;
- increased sweating;
- restlessness, anxiety, panic attacks.
- painful myocardial shocks;
- attacks of suffocation.
Against the background of group extrasystoles, accompanied by frequent heart rhythm disturbances, there is a high risk of developing cerebral hypoxia.
Signs of AV block
Symptoms of artrioventricular block may vary depending on the severity of the disease. Atrioventricular block is often accompanied by bradycardia or is asymptomatic.
It is impossible to independently identify signs of the development of pathology; electrocardiography is used for diagnosis. Signs of 1st degree AV block are expressed during physical activity by shortness of breath, weakness, dizziness or confusion.
Signs of 2nd degree AV block:
- fast fatiguability;
- weakness;
- chest pain.
With the development of 3rd degree atrioventricular block, symptoms of Adams-Stokes syndrome appear:
- convulsions;
- numbness of the face;
- decrease in heart rate to 35-40 beats per minute;
- fainting;
- chest pain;
- dizziness;
- darkening of the eyes.
If 3rd degree AV block is detected, the patient is given a pacemaker.
Paroxysmal tachycardia
With paroxysmal tachycardia, an increase in heart rate is observed (up to 180-300 beats per minute). The distribution of impulses is frequent and regular.
Associated symptoms of the pathology include:
- fatigue;
- general weakness;
- anxiety;
- anxiety;
- irritability;
- increased sweating;
- flushes of heat to the face;
- pain in the chest area (on the left side).
The onset of an attack is indicated by rapid breathing and pale skin. The pulse becomes painful.
Cardiac arrhythmias
Cardiac arrhythmias
(Greek: arrhythmia, absence of rhythm, irregularity)
various disorders of the functions of automaticity, excitability and conductivity of the myocardium, often leading to disruption of the normal sequence or frequency of heart contractions.
Changes in the actual rhythm and rate of heart contractions can be felt by the patient himself and are easily recognized by auscultation of the heart. At the same time, many A. s. are detected only by recording an ECG, and some can only be detected by recording intracardiac electrograms.
The most common forms of A. s. include atrial fibrillation, paroxysmal tachycardia, extrasystole, arrhythmias due to conduction disorders (see Heart block, Premature excitation syndrome of the ventricles of the heart).
Cardiac arrhythmias have multiple etiologies. Their origin may be due to dysregulation of cardiac activity, pathology of the myocardium and conduction system of the heart (Heart), as well as a combination of these. A. s. due to impaired regulation of the heart, are possible with psycho-emotional stress, may have a neuro-reflex nature in diseases of other organs (cholecystitis, diaphragmatic hernia, etc.), often occur with organic damage to the central and autonomic nervous system (for example, with cranial trauma, brain tumors, cerebrovascular accidents, after vagotomy), as well as in disorders of the endocrine regulation of autonomic functions (for example, during menopause). Pathological changes in the myocardium are the cause of A. s. for myocardial ischemia and infarction, myocarditis, cardiomyopathies, cor pulmonale, cardiosclerosis, various forms of myocardial dystrophy, incl. for endocrinopathies (hypothyroidism, thyrotoxicosis, etc.) and intoxications, when they can be reversible. A number of drugs (drugs of the digitalis group, quinine, stimulants and blockers of β-adrenergic receptors, agents used for local anesthesia, etc.), as well as poisons (bacterial toxins, carbon monoxide, organophosphorus compounds, etc.) can cause A. pp., stopping after eliminating the influence of the toxic factor. In elderly and senile people A. s. usually occur against the background of cardiosclerosis, but their origin often involves ischemic myocardial dystrophy, and sometimes also disturbances in electrolyte metabolism due to age-related changes in renal function. Organic changes in the myocardium most contribute to the occurrence of A. when they are localized in the region of the sinus node and in the conduction system. Cardiac arrhythmias can also be caused by congenital anomalies of these formations.
In the pathogenesis of A. s. a major role belongs to shifts in the ratio of the content of potassium, sodium, calcium and magnesium ions inside myocardial cells and in the extracellular environment. These shifts lead to changes in the excitability, refractoriness and conductivity of the sinus node, conduction system and contractile myocardium. A. s. develop with the following violations of the listed functions: strengthening, inhibition or complete suppression of the activity of the sinus node; increased activity of lower-order automatism foci; shortening and lengthening of the refractory period; reduction or complete cessation of conduction through the conduction system or contractile myocardium; pathological conduction of an impulse in the direction opposite to normal (retrograde conduction), or along pathways that do not function under normal conditions. Most of A. s. is caused by the occurrence of pathological circulation of an excitation wave in the heart.
The basis for the classification of A. s. the pathophysiological mechanisms of their occurrence are laid down. Among the latter, there are disturbances in the formation of impulses in the sinus node, passive and active heterotropic automatism, conduction disturbances, as well as combined disorders.
Impaired impulse formation in the sinus node and passive heterotropic automatism. Sinus arrhythmia is an irregular heart rate associated with fluctuations in the activity of the sinus node. Under physiological conditions, it is observed mainly in young people and is associated with the act of breathing (respiratory arrhythmia); with increased intrathoracic pressure, i.e. at the beginning of exhalation or as a result of straining, the tone of the vagus nerve increases, which leads to a temporary slowdown in the rate of heart contractions. Occasionally, sinus arrhythmia occurs, not associated with the respiratory phases, caused by various pathological processes in the myocardium (infarction, myocarditis, heart defects) and neuroregulatory disorders. Patients do not feel sinus arrhythmia. Respiratory arrhythmia is easy to recognize clinically by the relationship between pulse rate and respiratory phases; For accurate diagnosis of sinus arrhythmia of other origin, an electrocardiographic study is necessary. There is unevenness of the intervals between the ventricular complexes with a normal configuration of the P wave and a constant, within the normal range of the duration of the PQ (R) interval. Treatment for pathological forms of sinus arrhythmia is aimed at the underlying disease.
Sinus bradycardia - see Bradycardia.
Sinus paroxysmal tachycardia - see Paroxysmal tachycardia.
Sinus tachycardia - see Tachycardia.
Sinus extrasystole - see Extrasystole
Atrial asystole (atrial arrest) is associated with complete suppression of sinus node activity or with sinoauricular block, the absence of heterotopic foci of excitation in the atrial myocardium and the absence of retrograde conduction from the ventricles to the atria. The role of pacemaker is assumed by lower-order centers of automaticity. A so-called nodal (atrioventricular) or ventricular (idioventricular) rhythm occurs (see below). Accurate recognition is difficult: the ECG does not show P waves, flutter waves or atrial fibrillation. In doubtful cases, they resort to recording an intraatrial electrogram.
Vagal pacemaker in the sinus node. The etiology and pathogenesis are unknown. The probable cause is fluctuations in the tone of the parasympathetic nervous system, which leads to a changing order of propagation of excitation in the area of the sinus node. Electrocardiographically, it is manifested by the shape of the P wave (or P loop of the vectorcardiogram) changing in different cycles with a normal PQ (R) interval that is the same in all cycles.
Migration of the pacemaker in the atria. The presumptive cause is fluctuations in the tone of the vagus nerve. Electrocardiographically, it is manifested by a changing shape of the P wave and P loop of the vectorcardiogram and changes in the PQ (R) interval in different cardiac cycles.
Jumping atrioventricular (nodal) impulses. If the activity of the sinus node is completely suppressed, as well as with a complete interruption of conduction at one level or another, the role of pacemaker is assumed by one of the centers of lower-order automatism. With inconsistent suppression of the automatism of the sinus node (for example, with sinus arrhythmia, sinoauricular block, short-term irritation of the vagus nerve), during periods of lengthening of the pause between its impulses, the automatism of the atrioventricular connection may appear (normally suppressed, like the automatism of the ventricles, by more frequent impulses from the sinus node) . A single nodal impulse occurs, differing from a nodal extrasystole only in that it is preceded on the ECG by an extended diastolic pause rather than a shortened one. Accurate diagnosis is only possible using ECG data ( Fig. 2 ).
Atrioventricular (nodal) rhythm appears with a sharp increase in the tone of the vagus nerve or depression of the sinus node caused by other reasons. The atrioventricular node does not have automaticity and, in fact, the so-called nodal rhythms arise either at the border between the atrial myocardium and the atrioventricular node, or at different levels of the His bundle - from its beginning to its branching. Nevertheless, the rhythms arising in this area are called nodal. Clinically manifested by bradycardia; sometimes pulsation of the jugular veins appears, which is associated with simultaneous or almost simultaneous contraction of the atria and ventricles. An accurate diagnosis is possible only on the basis of an analysis of ECG changes: a negative P wave and a shortened PQ interval (the source of the rhythm is at the border of the atria and the upper part of the node); absence of the P wave, which superimposes on the QRS complex and somewhat deforms it (midnodal rhythm); a negative P wave follows the QES complex (the rhythm comes from the underlying sections of the His bundle before its bifurcation, but according to tradition it is usually called inferior nodal. These criteria are not recognized by all researchers. There is an opinion that changes in the shape of the P wave are associated with disturbances of intraatrial conduction, almost always detected during atrioventricular tachycardia, or with the presence of abnormal additional pathways in the atrioventricular node itself. A variant of the nodal rhythm is considered to be the coronary sinus rhythm, reminiscent of the supernodal rhythm in ECG changes (Fig . 3 ); diagnostic signs are considered to be a negative P wave in leads II, Ill aVF, positive the P wave in lead aVL and very rarely a negative P wave in leads V4 - V6. The atropine test helps to distinguish between functional and organic junctional rhythm: after the subcutaneous injection of 1 ml of 0.1% atropine sulfate solution, the functional junctional rhythm is replaced by sinus.
Idioventricular (ventricular) rhythm occurs when the activity of the foci of automatism of the first and second orders is suppressed and with complete transverse heart block. If the suppression of the activity of first- or second-order foci is short-lived, jump-out ventricular contractions may occur. On the ECG, against the background of sinus or atrioventricular rhythm, a deformed QRS complex appears after an extended diastolic pause. The ventricular rhythm itself is always associated with severe organic lesions of the heart. The heart rate can be sufficient to maintain the vital functions of the body only if the source of impulse in the ventricles is located high enough. Slow idioventricular rhythm occurs in terminal conditions. The diagnosis is based on ECG analysis.
Treatment for A. s., caused by a violation of the formation of an impulse in the sinus node, is aimed at the underlying disease, and if A. s. lead to disturbances in intracardiac and general hemodynamics, symptomatic (antirhythmic) therapy is carried out. Medications for bradycardia may include atropine, β-adrenergic stimulants (isadrin, etc.), and for tachycardia - β-blockers (anaprilin, etc.). In cases of organic damage to the sinus node with atrial asystole or pronounced bradycardia or alternating brady- and tachyarrhythmias (sick sinus syndrome), especially in the presence of syncope (see Morgagni-Stokes syndrome (Morgagni-Adams-Stokes syndrome)) or heart failure implantation of an artificial pacemaker is indicated.
Active heterotropic automatism. The identification of this group of arrhythmias, including atrial, nodal and ventricular arrhythmias, is most conditional, because in most cases, they are apparently caused not only by the appearance in the myocardium of a focus with a pathological impulse frequency, but also by the presence of conduction disturbances, as well as refractoriness, which leads to the occurrence of circulation of an excitation wave (see Atrial fibrillation, Paroxysmal tachycardia, Extrasystole).
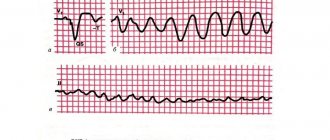
Fluttering (tachysystole) and fibrillation (fibrillation) of the ventricles. Terminal forms of A. s., expressed in a sharp disturbance (with flutter) or a complete disorder of coordination of the activity of the entire myocardium, usually occur with severe and extensive damage to the myocardium (for example, with a heart attack, severe myocarditis, cardiomyopathies, heart defects), as well as with damage electric shock. The mechanism of development of ventricular flutter and fibrillation is similar to the pathogenesis of atrial flutter and atrial fibrillation, but uncoordinated activity is inherent in the entire myocardium in general, and not just in the atrial myocardium. Due to the fact that the propulsive activity of the heart during these A.s. is absent, they manifest themselves as clinical death. Distinguish fibrillation and flutter of the ventricles from other forms of terminal A. s. only possible electrocardiographically. Ventricular flutter is characterized by the presence on the ECG of frequent (200 per minute or more) high regular waves ( Fig. 4 ), ventricular fibrillation is characterized by even more frequent waves of various sizes and shapes, following one after another without any order ( Fig. 5 ). If resuscitation measures are not taken, the average amplitude of the flicker waves gradually decreases and after some time asystole occurs. Treatment is urgent electrical cardiac defibrillation.
Arrhythmias of mixed origin. Atrioventricular dissociation is the complete or partial independence of the contractile activity of the ventricles from the contractions of the atria. Complete atrioventricular dissociation occurs with third degree atrioventricular block. Incomplete atrioventricular dissociation is associated with a decrease in the activity of the sinus node and an increase in the activity of lower-order impulse foci, when the impulse frequency in the two sources of automaticity becomes almost the same (isorhythmic dissociation, Fig. 6 ). It also occurs if the rhythm of the heterotropic focus of automatism is more frequent than the rhythm of the sinus node, and there is no retrograde conduction from the ventricles to the atria ( Fig. 7 ). The latter form is called interfering dissociation. Various forms of atrioventricular dissociation can occur both in practically healthy people (for example, jumping out nodal contractions), and as a result of medicinal effects (digitalis, antiarrhythmic drugs) and many diseases (myocardial infarction, myocarditis of various etiologies). Subjectively, they usually do not manifest themselves in anything; occasionally patients complain of a feeling of interruptions. The diagnosis is made using electrocardiography. Treatment is aimed at combating the condition (disease, intoxication) that caused the arrhythmia.
Reciprocal rhythms (echorythms, reciprocal, reciprocal rhythms). The essence of these arrhythmias is that the same impulse, as a result of the presence of pathological retrograde conduction in the atrioventricular node, returns to the part of the heart in which it originated and causes its re-excitation. The source of reciprocal rhythms can be various parts of the heart: the atria, the atrioventricular node and the ventricles. The diagnosis is made based on ECG analysis. Atrial forms are characterized by the presence of a positive P wave, a normal duration of the PQ interval, a regular shape of the ventricular complex and a negative second P wave following it with a shortened interval ( Fig. 8 ). The most common atrioventricular form ( Fig. 9 ) is characterized by the presence on the ECG of paired ventricular complexes, between which there is a deformed negative P wave (the so-called sandwiches), and the distance between the paired ventricular complexes does not exceed 0.5 s. Ventricular forms also have the appearance of paired ventricular complexes, but the first of them is deformed like a ventricular extrasystole, and the second has a normal shape; between them there is a negative P wave. Treatment is ineffective. With atrioventricular forms, atropinization helps.
Parasystoles are caused by the simultaneous existence in the myocardium of two foci of impulses, one of which generates impulses with a lower frequency, but being protected from the action of impulses of the other (the so-called inspiratory block), causes periodic contraction of the entire heart or its parts. They occur (rarely) in practically healthy people; they are more often observed in various myocardial diseases. Subjectively they can be perceived as interruptions. When analyzing the ECG, against the background of the main rhythm, deformed P waves (atrial extrasystole), nodal or ventricular complexes are visible, which are repeated at equal intervals or multiple intervals thereof. The second pathognomonic sign of parasystole is the absence of a clear constant temporal connection (“coupling interval”) between the R wave of the main rhythm and the R wave of the parasystole. With extrasystole, such a connection can always be traced ( Fig. 10 ). Treatment - see Extrasystole.
Intraatrial and interatrial dissociation. A rare form of A. s., consisting in independent activity of the right and left atria or in different types of rhythm in different parts of the same atrium. It is observed, in particular, after a heart transplant, when the remaining part of the recipient’s heart works in a different rhythm than the donor’s heart. It is very rare to make a diagnosis based on conventional ECG data (various forms of supraventricular arrhythmias in different leads). No treatment has been developed.
Electrical alternans of the heart - uneven height of the QRS complexes on the ECG. Occurs in myocardial diseases, digitalis intoxication. Most often on the ECG it is displayed by a decrease in the QRS amplitude in each even complex; in this case, the distance between the ventricular complexes is the same and each of them is preceded by a normal P wave.
Treatment for resistant A. s. mixed genesis is developed with the participation of a cardiologist, whose consultation or observation is subject to all patients with resistant A. s. Often it is determined only after a special diagnostic examination of the patient in a hospital. In all cases, the underlying disease is treated. Because with many A. s. Antiarrhythmic drugs of mixed origin are not very effective, treatment can be limited to the effect only on the circulatory regulation apparatus - exercise therapy, an individual regimen of exercise and rest, and sometimes sedatives are prescribed.
Features of cardiac arrhythmia in children . A. s. in children they can be congenital (with malformations of the conduction system of the heart, immaturity of autonomic regulation) and associated with diseases that affect the heart or the apparatus for regulating its activity; Psychovegetative deviations are of great importance.
Frequency A. s. in children, according to various authors, is 0.6-8%, and in the general structure, extrasystole makes up 40-45%, paroxysmal tachycardia - 10%, non-paroxysmal tachycardia - 10-14%, atrial flutter and fibrillation - up to 6%.
Sinus arrhythmia, associated with uneven generation of impulses in the sinus node against the background of excessive vagal influences, is typical for children over 5 years of age. Most often it is observed in the form of respiratory arrhythmia. At the height of inhalation, the heart rate increases, and at exhalation it decreases. Sinus A. s. differentiate with extrasystole, sinoauricular block. Sinus bradycardia (decrease in heart contractions to 100 or less per minute in children of the first 2 years of life and up to 80-60 per minute in older children) may be a manifestation of vagal hyperactivity, sometimes genetically determined, but more often observed in children with signs of an athlete's heart , with hypothyroidism, traumatic brain injury. With sudden and persistent bradycardia, patients may complain of dizziness, weakness, and fatigue; Possible syncope. In these cases, it is necessary to exclude the connection of bradycardia with junctional rhythm, atrioventricular or sinoauricular heart block. The functional and organic nature of persistent sinus bradycardia is distinguished using tests with physical activity and a 0.1% atropine solution, which is administered intravenously at a dose of 0.02-0.025 mg/kg in 4 ml of isotonic sodium chloride solution. An increase in heart rate during testing by less than 30% of the initial value indicates organic damage to the sinus node. Sinus tachycardia (beat frequency above 140-200 per 1 min in young children and above 100-110 per 1 min in older children) can also be functional, caused by autonomic dysregulation, and organic. Its functional genesis is confirmed by a positive test with obzidan (0.5-1 mg/kg): contractions decrease by at least 10-12 per minute.
Pacemaker migration in children is detected by ECG in the same way as in adults. Its connection with vagotonia is assumed if it disappears in an upright position, during physical activity or a test with atropine; persistence of disturbances is characteristic of weakness of the sinus node.
Extrasystoles in children are detected more often than other A. with., and supraventricular extrasystoles predominate. Diagnosis and treatment are based on the same principles as in adults (see Extrasystole).
Paroxysmal tachycardia in children is also more often supraventricular and in most cases is not associated with acquired organic heart disease; Often its occurrence is based on autonomic dysfunction against the background of congenital features of the conduction system of the heart. Ventricular paroxysmal tachycardia is very rare in children. Diagnosis and treatment are the same as for adults. Sometimes children experience non-paroxysmal chronic heterotropic tachycardia, which can exist from several weeks to several years. It can be suspected by auscultation of the heart by a frequent, rigid heart rate (130-180 per minute), which may alternate with several heartbeats of normal frequency. Its origin is associated with delayed maturation of the central nervous system and imperfect regulation of heart rhythm. Children with chronic heterotropic tachycardia must be examined in a hospital.
Recognition and treatment of atrial and ventricular fibrillation, atrioventricular block and other disorders of the automaticity and conductivity of the heart in children are basically the same as in adults - see Heart block, Atrial fibrillation, Pre-excitation syndrome of the ventricles of the heart.
Bibliography: Belokon N.A. and Kuberger M.B. Diseases of the heart and blood vessels in children, vol. 1-2, M., 1987; Children's diseases, ed. P.N. Gudzenko, s. 502, Kyiv, 1984; Children's diseases, ed. A.F. Tura et al., p. 385, 388, M., 1985; Mazur N.A. Paroxysmal tachycardias, M., 1984; Mazurin A.V. and Vorontsov I.M. Propaedeutics of childhood diseases, p. 143, M., 1985; Sumarokov A.V. and Mikhailov A.A. Arrhythmias of the heart, M., 1976; Tomov L. and Tomov Il. Heart rhythm disturbances, trans. from Bulgarian, Sofia, 1976; Chazov E.I. and Bogolyubov V.M. Heart rhythm disturbances, M., 1972; Yanushkevicius Z.I. and others. Disturbances of rhythm and conduction of the heart, M., 1984.
Rice. 3. ECG with coronary sinus rhythm. The P wave in leads II, III and aVF is negative, in leads I and V6 it is smoothed, and in lead aVL the P wave is positive. At the bottom is a time marker (0.05 s). The heart rate is 48 per minute.
Rice. 1a). Electrocardiogram of a healthy person. Schematic representation of an electrocardiogram (ECG). P is a wave reflecting the progress of excitation propagation through the atrium, the P-Q interval is the time of passage of excitation through the atrioventricular connection. QRST is the ventricular complex of the electrocardiogram, reflecting the spread of excitation through the ventricles of the heart (ORS complex is the phase of ventricular depolarization, ST segment is the state of complete depolarization, T wave is the phase of late rapid depolarization). The U wave, the origin of which has not been precisely established, is not always observed normally. The horizontal side length of a small cell corresponds to 0.04 s, and the vertical length corresponds to 0.1 mV.
Rice. 2. Jumping nodal contraction (indicated by a cross) against the background of sinoauricular block. R1R2R4 - normal sinus contractions, they are preceded by atrial waves P1, P2, P4. SAB (sinoauricular block) is the area where regular normal P waves should be located, which are absent due to blockade between the sinus node and the atrial myocardium. Due to the long pause, the automatism of the atrioventricular connection is manifested (waves R3 and R5, which are not preceded by the atrial P wave; however, due to the absence of retrograde conduction in the atrioventricular connection, the normal next P wave is recorded after the jumping nodal contraction - P3 and P5). The numbers indicate the intervals between R waves in seconds.
Rice. 9. Inferior nodal rhythm (upper ECG), which turned into a reciprocal atrioventricular rhythm (lower ECG) (according to L.I. Fogelson). ECGs were recorded in lead II. The upper curve shows the correct inferior nodal rhythm (each ventricular complex is followed by a negative P wave; pulse frequency 32 per minute). Curve - paired ventricular complexes (so-called sandwiches).
Rice. 8. ECG for the atrial form of reciprocal rhythm. P - normal atrial wave. In the third complex, the P wave is clearly visible (negative, following the unchanged ventricular complex), which reflects the return of the excitation wave to the atrium from the area of the atrioventricular junction (see diagram in Fig. 8, C). Vertical lines indicate the atrial waves P and P'.
Rice. 7. ECG (in lead II) with incomplete atrioventricular dissociation, such as interference with dissociation. The frequency of impulses from the heterotropic focus of automatism is higher than the frequency of impulses of the sinus node (atrial P waves are indicated by arrows). There is no retrograde conduction from the ventricles to the atria, so most ventricular complexes are not associated with atrial P waves. However, if the excitation impulse accidentally reaches the ventricles after the end of their refractory period, during the excitability phase, a sinus “captured” contraction (SC) occurs. At the bottom is a time counter (0.1 s).
Rice. 5. ECG for ventricular fibrillation.
Rice. 10. Ventricular parasystole (ECG in lead II). Against the background of sinus rhythm, deformed ventricular complexes appearing at almost equal intervals of time, the distance between which corresponds to 302-324 s. The impulse frequency in the sinus node is 78 per 1 min, in the focus of heterotropic automatism - 19 per 1 min. The numbers in the figure are time intervals in hundredths of a second.
Rice. 1b). Electrocardiogram of a healthy person in 12 generally accepted leads: standard (I, II, III), unipolar from the limbs (aVR, aVL, aVF) and thoracic (V1-V6).
Rice. 4. ECG for ventricular flutter: below - timer (0.1 s).
Source: Medical Encyclopedia on Gufo.me
Meanings in other dictionaries
- cardiac arrhythmias - Cardiac arrhythmias - a group of disorders of the formation and conduction of an excitation impulse in the heart muscle; any deviation from normal sinus rhythm. Medical dictionary
- HEART ARRHYTHMIAS - honey. Cardiac arrhythmias are a group of disorders in the formation and conduction of excitation impulses in the heart muscle; any deviation from normal sinus rhythm. Directory of diseases
- cardiac arrhythmias - HEART ARRHYTHMIAS, cardiac arrhythmias; are observed in animals more often with myocardial diseases involving patol. process of the cardiac conduction system. Many of A. s. can only be detected by electrocardiography. A. Veterinary encyclopedic dictionary
- Blog
- Jerzy Lec
- Contacts
- Terms of use
© 2005—2020 Gufo.me
Diagnosis of pathologies
When visiting a medical facility, the doctor must carefully examine the patient and interview him. After collecting the medical history, the patient is sent for an electrocardiogram. The diagnostic method will help confirm arrhythmia if the pathology is stable or permanent. If tachycardia is suspected, the electrocardiogram should be recorded around the clock.
Holter monitoring is not always able to detect the disease. Additionally, transesophageal cardiac stimulation is performed. This is a deeper method that allows you to confirm or refute sick sinus syndrome. To detect arrhythmia, a title test is used.
The technique is able to determine the root cause of the development of pathology. The most informative study is considered to be invasive (intracardiac) electrophysiological diagnostics.
Rare variants of arrhythmia on ECG
When conducting electrocardiography, doctors are able to identify any type of cardiac arrhythmia. Some disorders are more common, others less common. Most rarely, doctors encounter such a manifestation on the electrocardiogram as sinus node dysfunction syndrome.
This disease is characterized by a disruption of the heart rhythm resulting from a deterioration in automaticity or a sudden cessation of the functioning of the atrial node. The following factors can provoke the development of the disease:
- Violation of impulse formation.
- Slow heart rate.
- Ectopic pathologies.
This syndrome poses a danger to human life, as it can cause sudden cardiac arrest. It can also be combined with diseases such as pulmonary edema, coronary insufficiency, and heart attack.
Thus, there are several classifications of arrhythmia, which differ from each other by different criteria. It is impossible to determine the type of pathology by symptoms alone; this requires a heart examination. This is important, since further treatment tactics depend on the type of disorder.
Emergency care for extrasystole
To stop an attack of extrasystole, the patient is prescribed drug therapy.
It includes:
- Preparations with chitin-like action. During an attack, Novocainamide is administered intramuscularly or intravenously (5 ml of 10% solution) up to 2 times a day.
- Antiarrhythmic medication. Quinidine falls into this category. The drug is able to weaken the excitability of the myocardium and reduce its activity. For extrasystole, the medicine can be taken up to 4 times a day (10 mg once).
- Potassium-containing drugs. During an attack of extrasystole, take potassium salts, Tromcardin or Panangin, 1-2 tablets once 3-4 times a day.
- Sedative medications. In emergency cases, Seduxen (10 mg IV) is administered parenterally or the patient is given Corvalol, Valocordin (35-45 drops once).
To stabilize the condition, during the rehabilitation period the patient is prescribed fish oil and vitamin and mineral complexes.
How to act in case of arrhythmias
During an attack of arrhythmia, the patient must be laid horizontally and the basic principles of breathing exercises explained to him. The patient should take a deep breath, hold it, and exhale slowly. To stabilize the heart rate, lightly massage the carotid artery at the site of pulsation. The patient should close his eyes and press his fingers on the eyeballs.
If the arrhythmia is manifested by a decrease in heart rate, then the patient is placed on his back, raising his legs above his head. For pain in the heart area, the patient is given nitroglycerin. Until the ambulance arrives, the patient is kept at rest. It is recommended to ventilate the room.
Diagnostics
Diagnosis of arrhythmia includes a comprehensive examination of the patient.
One of the simplest and most reliable diagnostic methods is electrocardiographic examination. Since arrhythmias can be transient, and during the day they can appear and disappear several times, then for the most accurate determination of arrhythmias it is necessary to carry out Holter monitoring. This is the same electrocardiographic study, only registration occurs within 24 hours. In this case, the patient must mark his actions in a special notebook by the hour (climbed the stairs, had a fight with a friend, etc.). Holter monitoring is the most accurate type of research.
When interpreting an electrocardiogram, doctors can evaluate the heart rhythm (sinus, atrial, atrioventricular, ventricular), its regularity or irregularity. Then the conductivity is assessed. To do this, the duration of the teeth and intervals is measured; as they expand, slow conduction is noted. Next, the electrical axis of the heart is determined and the heart rate is calculated. After this, they move on to evaluating each tooth and interval separately.
For diagnosis, an echocardiographic study is also performed to identify structural changes in the heart. If the cause of the arrhythmia is unknown, then a comprehensive examination of all organs and systems is carried out, based on complaints and anamnesis to exclude concomitant diseases.
Blockades and sinus node arrest
If characteristic signs of AV block appear, you must immediately call an ambulance. Patients with conduction disorders of the cardiac system are subject to mandatory hospitalization. In a hospital setting, they are provided with ECG monitoring and strict bed rest. Drug therapy is prescribed individually, depending on the severity of the symptom complex.
Before transportation to the hospital, a patient with complete AV block is administered Atropine (1 ml 0.1% solution). If conduction disturbances are accompanied by an Adams-Stokes attack, then upon arrival of the ambulance the patient is given an indirect cardiac massage and Novodrin is administered intravenously (0.05% solution, 2 ml).
Differences between the concepts of pulse rate and rhythm.
The concepts of heart rate and human pulse rhythm should not be confused. What's the difference? The easiest way to explain this difference is with a simple example. It is known that pulse rate is the number of pulse oscillations per minute. So, suppose we counted 60 pulse beats per minute. In this case we can say that the heart rate is 60 per minute. Now let's try to evaluate the rhythm. After all, all 60 beats can be evenly distributed during this minute, in which case we characterize the pulse as rhythmic. But if we see that the pulse either accelerates or slows down, that extraordinary contractions of the heart appear, or that it seems to “fall out,” then we will characterize such a pulse as irregular. Unlike the pulse rate, which normally differs depending on age: in children - more often, in adults - less often, the correct pulse rhythm in children implies the same as in adults: orderly contractions of the heart.
Actions for sinus node weakness
Vagal methods (pressure on the eyeballs and deep breathing) will help restore the pulse in sick sinus syndrome. First of all, you need to call an ambulance, especially if the attack is acute. The patient's blood pressure and heart rate are measured.
If both indicators deviate from the norm in the direction of increase, then the patient is laid horizontally in a well-ventilated room and a cold compress is applied to the forehead. The patient must be provided with complete rest. For people who are fainting, cotton wool soaked in ammonia is brought to their nose.
Classification
There are several main classifications of arrhythmias. According to the speed of impulse formation, arrhythmias can be divided into tachyarrhythmias (increased heart rate) and bradyarrhythmias (decreased heart rate).
According to the place of formation, the following types of arrhythmia are distinguished: supraventricular (atrial), ventricular and atrioventricular.
In accordance with the type of disorder, the classification of arrhythmias involves division into three main groups:
I. Rhythm disturbance.
- Violation of the automaticity of the pacemaker (sinus node):
- tachyarrhythmia;
- bradyarrhythmia;
- simple sinus arrhythmia;
- sick sinoatrial node syndrome.
- Arrhythmias caused by the occurrence of ectopic pacemakers (not sinus node):
- slow atrial, ventricular or atrioventricular escape rhythms or complexes;
- accelerated atrial, ventricular or atrioventricular escape rhythms or complexes.
- Arrhythmias arising due to a recurrent excitation wave in the conduction pathways:
- extrasystoles (atrial, ventricular, atrioventricular);
- paroxysms of tachycardia (can occur in the atria, ventricles, and atrioventricular node);
- ventricular/atrial flutter;
- ventricular/atrial fibrillation.
II. Impaired impulse conduction.
- blockade of the sinoatrial node;
- blockade of the atrioventricular connection (three degrees);
- intraventricular blockade of the His bundle and its branches;
- ventricular asystole;
- premature ventricular contraction syndrome.
III. Mixed disorders.
Help with the development of bradycardia
During an attack of bradycardia, the patient should be asked to take a warm bath. Water treatments will help increase your heart rate. In case of a sudden attack of bradycardia, a person can drink coffee or strong tea. These drinks contain caffeine, which can restore heart rate.
If your heart rate is 50-55 beats per minute, then physical exercise (jogging, brisk walking, climbing stairs) will help stabilize your heart rate. When the heart rate drops to 30-40 beats per minute. high risk of loss of consciousness. In this case, you must call an ambulance.
AV block
AV block occurs when the heart partially or completely stops conducting impulses from the atria to the ventricles. Because of this, the heart rate is disrupted, and organs and tissues do not receive enough blood and oxygen.
Symptoms . When the disease develops:
- weakness, shortness of breath;
- angina pectoris – pain in the sternum;
- dizziness, darkening of the eyes;
- bradycardia - a decrease in heart rate to 30-50 beats per minute.
Diagnosis and treatment . AV block is diagnosed by ECG and echocardiography. If the problem appears due to taking certain medications (for example, papaverine or drotaverine), to eliminate it, it is enough to stop taking the medications. If there are concomitant heart diseases, beta-agonists are prescribed; in severe cases, a pacemaker is implanted.
Drugs for the treatment of arrhythmias
Heart rhythm disturbance is a serious pathology that requires timely treatment. The severity of symptoms directly depends on the causes of the disease.
Drug therapy includes the following drugs:
- Quinidine. Belongs to the group of membrane-stabilizing drugs. It goes on sale in tablet form. The principle of operation is based on the ability to increase the speed of passage of electrical impulses to the fibers. The drug normalizes blood pressure. Dosage regimen: no more than 400 mg per day (100 mg once). The tablets are taken before or after meals. Contraindications include impaired ventricular conduction and hypersensitivity to the active ingredients.
- Digoxin. Cardiac glycoside helps improve the functioning of the muscular organ and increase the stages of myocardial relaxation. It goes on sale in tablet form. Dosage regimen: 1-2 tablets per day, depending on the clinical picture. Contraindications: myocardial infarction (acute), hypersensitivity to the main components, glycoside poisoning.
- Warfarin. Inhibits the synthesis of substances involved in the blood clotting process. Release form: tablets. The daily dose is no more than 5 mg. With the permission of the doctor, the therapeutic norm is increased to 10 g. The drug is taken at the same time every day, for 10-20 days. Contraindications: pregnancy, poor blood clotting, liver and kidney disease (including failure).
- Bisoprolol. Beta-blocker, acting selectively. Effective for arrhythmia. Available in tablet form. The daily norm is no more than 10 mg. Contraindications: childhood, acute heart failure.
The above medications must be taken with the permission of a doctor. Independent selection of drug therapy is strictly prohibited.
Peculiarities
Signs of the disease can be very frightening for the patient, even if this particular type of pathology is not dangerous. It often seems to a person that the rhythm of his heart is seriously disturbed or that the organ has completely stopped. This condition occurs especially often during extrasystole. It should be borne in mind that even harmless types of arrhythmia must be treated so that the patient feels normal and the manifestations of the disease do not interfere with his life.
With such a disease, the heart rhythm can not only be erratic, but also become more frequent or less frequent than normal, which is why the disease is classified by doctors.
Kinds:
- The sinus type of arrhythmia is associated with the respiratory process; the rate of contraction of the organ increases with inhalation and decreases with exhalation. Sometimes this form of the disease appears regardless of breathing, but indicates damage to the cardiovascular system. Adolescence, in which arrhythmia often occurs, is distinguished by the fact that autonomic disorders provoke the disease. This type of disease is not dangerous and does not require therapy.
- The sinus type of tachycardia is caused by an increase in heart rate of more than 90 beats per minute. Of course, the physiological factors contributing to such an increase in the activity of the organ are not taken into account. With such a deviation, the heart rate (heart rate) increases, but not more than 160 beats per minute, if the person does not experience anxiety or other similar phenomena.
- The sinus type of bradycardia is the correct pace of the organ, but slow, below 60 beats per 1 minute. This disorder is associated with a decrease in the automatic function of the sinus node, which appears against the background of physical activity in people who are professionally involved in sports. Pathological factors also cause the development of this form of arrhythmia. There are medications that can slow down the heart rate.
- Extrasystole is a condition of an organ in which excitation occurs prematurely, and one of the parts of the heart contracts or all at once. This form of the disease is divided into several varieties, depending on the location of the disorder in which the impulse is formed, leading to deviation. There are ventricular, atrial, and atrioventricular types.
- The paroxysmal type of tachycardia is similar to extrasystole, which begins to appear suddenly and also stops abruptly. Heart rate in such a state can be above 240 beats per 1 minute.
- Impaired conduction or blockade is a deviation that is well detected by the electrocardiogram. This form of the disease can occur for many reasons, and it can only be eliminated after treating the underlying disease. Blockades are an emergency that requires immediate medical attention. Some types of such disorders cannot be removed with medication. Only after installing a pacemaker does the heart function stabilize.
- Atrial fibrillation or ventricular fibrillation are the most severe types of the disease. Excitation and contraction of the organ is formed only in individual fibers of the atrium. This erratic excitation does not allow electrical impulses to pass normally into the area of the atrioventricular node and the ventricles.
Rhythm disturbances on the ECG look different, but we can definitely say that arrhythmia is detected immediately by this diagnostic method. If the case concerns a child, then this method of examination is also used. Timely examination of heart function allows immediate treatment to be prescribed. In the event of a sudden attack of this disease, you need to go to an ambulance; a paramedic will do an ECG diagnosis even at home, which will allow you to identify the paroxysm in time and stop it.
Traditional methods of treating arrhythmia
For arrhythmia, remedies based on hawthorn are effective. Plant extracts normalize blood pressure and stabilize pulse.
Infusions:
- From berries. 100 g of dry fruits are poured with boiling water (1 l). The thermos is hermetically sealed and the product is infused for 30 minutes. After the allotted time has passed, add 3 tbsp to the infusion. l. any flower honey. Take 100 ml of the product per day.
- From leaves. 1 tbsp. l. dry hawthorn leaves are poured with boiling water (300 ml). The container with the infusion is hermetically sealed and infused for 5 hours. The cooled drink is taken 100 ml 2 times a day for 30 minutes. before dinner and breakfast.
Treatment with folk remedies is quite long. It is recommended to take infusions, decoctions and teas regularly for 25-30 days.
Complications
In the absence of proper treatment, the risk of complications is quite high.
These include:
| Pathology | Symptoms | Treatment |
| Vegetovascular dystonia | Headache, temperature fluctuations, tinnitus, fainting, dizziness, drowsiness, hypochondria. | Manual and drug therapy, giving up bad habits, lifestyle correction. |
| Hypertension | Dizziness, weakness, headache, tinnitus, mild nausea. | Drug treatment, proper nutrition, losing excess weight (for obesity). |
| Thromboembolism | Severe pain in the peritoneum, increased gas formation, collapse, dizziness, asthenia, drowsiness. | If drug therapy (at an early stage) does not bring the expected result, surgical intervention is required. |
| Vagotonia | Shortness of breath, attacks of suffocation, painful dry appetite, nausea, heartburn, headache, heartburn. | Drug therapy in combination with traditional medicine. |
Ventricular fibrillation can lead to death. People suffering from arrhythmia need to undergo regular cardiac examinations and take medications prescribed by their doctor.
Heart rhythm disturbances lead to disorders of the vascular system, the symptoms of which do not always appear. The causes of the development of pathologies are determined in the laboratory, treatment is prescribed only after an accurate diagnosis has been made.
Types of arrhythmia according to electrophysiological criteria
This classification of cardiac arrhythmia takes into account the type of disorder that occurs during the pathology. It looks like this:
- Impulse creation failed.
- Violation of signal conduction.
- A combination of these pathological changes.
The first type refers to tachycardia, bradycardia, the second – to heart block, the third combines both options.
Types of arrhythmia according to Lown
Lown classification involves dividing pathology into classes as the disease progresses. The higher the class, the more dangerous the disease and the higher the risk of developing serious complications.
Progressive disease has a higher Lown class
The following classes are distinguished:
- 0 – no arrhythmia.
- 1 – assigned when there are less than 30 extrasystoles per hour, and there is only one source.
- 2 – extrasystoles increase by more than 30 per hour, the source remains the same.
- 3 – several foci of pathological impulses are already observed.
- 4a – paired extrasystoles arise from one source.
- 4b – polymorphic extrasystoles appear, which are combined with other arrhythmias.
- 5 – extrasystoles “type R to T”.
This classification was created many years ago, but is still used in medical practice.