Regurgitation - this term is often found in the professional life of doctors of various specialties, for example, therapists, cardiologists, functional diagnosticians. And many patients have encountered it, but have no idea what it is about. It’s time to understand this issue so that when the doctor says that there is “pulmonary valve regurgitation,” you clearly know what it is and what dangers it is associated with.
Zmist:
- Causes
- Symptoms
- Diagnostics
- Treatment
Regurgitation refers to the reverse flow of blood from one chamber of the heart to another. This means that when the heart muscle contracts, some blood volume for some reason returns to the heart cavity from which it moved. It cannot be said that regurgitation is an independent disease, therefore this term cannot be used as a diagnosis. However, it characterizes other pathological changes and conditions, an example is heart disease.
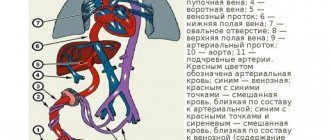
It is important to understand that blood moves continuously from one part of the heart to another. It comes from the pulmonary vessels and goes into the main circulation of the blood. But the term "regurgitation" applies to all four valves where backflow can occur. A different blood flow returns back, which makes it possible to distinguish the degrees of regurgitation. Such degrees include identifying the clinical signs of the condition. To better understand pulmonary regurgitation, it is necessary to understand the anatomy.
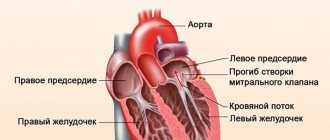
As you know, the heart is a hollow muscular organ that has 4 chambers, namely: a pair of ventricles and atria. Between the heart chambers and the vascular bed there are valves that act as gates. They allow blood to flow in only one direction. Thanks to this system, normal blood flow from one circle to another is ensured, since the heart muscle contracts rhythmically. It pushes blood into the blood vessels and inside the heart.
When the valve apparatus and myocardium work normally during the period of contraction of any cavity, the valve leaflets close tightly. With various cardiac lesions, the mechanism can be disrupted. The following valves are available:
- mitral;
- tricuspid;
- pulmonary and aortic valves.
Depending on the problem area, an exact definition of the condition is given: mitral, tricuspid or aortic regurgitation. This means that if the mechanism associated with the pulmonary valve is disrupted, then pulmonary regurgitation of a certain degree has occurred. Insufficiency of this valve causes blood to flow from the pulmonary artery into the RV during diastole.
to the point ↑
Classification (forms, types, degrees)
The course of the disease can be acute or chronic; by etiology - ischemic and non-ischemic.
The main factors in the occurrence of the acute form of the disease are:
- rupture of the chordae tendineus or papillary muscle;
- rupture of the mitral valve leaflet;
- acute form of infective endocarditis;
- myocardial infarction;
- blunt heart injuries.
Various causes of the chronic form of the disease include:
- inflammation;
- degenerative processes;
- infection;
- structural processes;
- genetic abnormalities.
There is a distinction between organic and functional mitral insufficiency. The first can develop in the process of structural changes in the valve itself or the tendon threads that hold it. The second is considered the result of an enlarged cavity of the left ventricle during a period of hemodynamic overload, which is caused by diseases of the heart muscle.
Considering the severity, 4 degrees of the disease are distinguished: with minor mitral regurgitation, moderate, severe and severe.
The clinical course is divided into 3 degrees:
- 1 (compensated) – insignificant minor mitral regurgitation; it reaches 20-25% of the systolic blood volume. Failure can be compensated by hyperfunction of the left parts of the heart. The blood flow is small (approximately 25%) and can only be observed at the valve. The patient's condition is normal , symptoms and complaints may be absent. An electrocardiogram will not show any changes; during the diagnostic process, murmurs during systole and the limits of the heart are slightly expanded to the left side.
- 2 (subcompensated) – regurgitation reaches 25-50% of the systolic blood volume. Blood may stagnate in the lungs and biventricular overload may slowly increase. During stage 2, reverse blood flow can reach the middle of the atrium, blood flow exceeds 25 - 50%. The atrium is unable to pump out blood without increasing blood pressure. Pulmonary hypertension may develop. , tachycardia during exercise and at rest, and cough may appear The electrocardiogram shows no changes in the atrium; at the time of diagnosis, systolic murmurs and an increase in the limits of the heart are detected.
- 3 (decompensated) – severe deficiency. Blood returns to the left atrium in systole and reaches 50-90% of the total volume. Total heart failure may develop. During stage 3, blood can reach the posterior wall of the atrium and reaches up to 90% of the volume. There may be an enlargement of the left atrium , which is not able to push out the entire volume of blood. Swelling occurs, the size of the liver increases, and the pressure in the veins increases. An electrocardiogram indicates the presence of changes in the left ventricle and mitral wave.
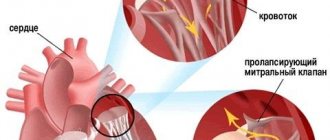
Mitral valve prolapse - what is it?
The mitral (bicuspid) valve separates the chambers of the left side of the heart: the atrium and the ventricle. Mitral valve prolapse is the bowing of the valve leaflets during contraction (systole) of the left ventricle.
The pathology is caused by a violation of the structure of the valve (its fibrous layer, less often the chordae tendineae) due to connective tissue dysplasia. In this case, the valve flaps not only bend, but may also not close tightly.
When the left ventricle contracts, blood rushes back into the atrium through the remaining lumen of the valve. This process is called regurgitation.
MVP is most often diagnosed in young people 20-35 years old. It is extremely rare that deviations in the structure and function of the mitral valve are found in young children. Among adults, the frequency of pathology ranges from 10-25%, and in the elderly - 50%.
The main reasons for the formation of a valve defect:
- Hereditary connective tissue dysplasia (Marfan and Ehlers-Danlos syndromes) - primary valve prolapse develops;
- Incorrect osteogenesis, leading to deformation of the chest;
- Rheumatic damage to the heart, inflammatory processes in its membranes, heart attack, chronic cardiac ischemia, atherosclerosis/calcification of the valve ring - secondary prolapse is formed.
According to the severity of the deflection, mitral prolapse is distinguished:
- 1st degree - the height of the dome-shaped deflection of the valves does not exceed 0.6 cm (the norm is 1-2 mm);
- 2 degrees - bulging up to 0.9 cm;
- 3 degrees - the dome of the valve is more than 0.9 cm high.
Symptoms of prolapse by degree of regurgitation
The classification of MVP according to the severity of deflection of the valve leaflets is quite arbitrary. The most important factor influencing the general condition of a person and treatment tactics is the degree of regurgitation (grade 1 - 3), which determines the symptomatic picture of mitral regurgitation.
Features 1st degree
- Regurgitation in the mitral valve leaflets can be observed due to the fact that they do not completely close at the moment of systole and a regurgitant wave appears from the left ventricle to the left atrium.
- When reverse blood flow is not significant , mitral regurgitation can be compensated by an increase in cardiac work with the appearance of adaptive dilatation and increased function of the left ventricle and left atrium of the isotonic type. Such a mechanism is capable of maintaining an increase in pressure in the pulmonary circulation for a long time.
- This degree of illness is considered normal . It occurs in both young and old people.
- It is not possible to make a diagnosis using noise measurement on an ECG, therefore for diagnostic purposes, mitral valve prophylaxis is used, determined by listening to heart murmurs, so doctors try to determine systolic clicks.
- The most popular way to identify this stage is an ECG study, as it reveals the level of resulting regurgitation and probing of the leaflets.
- When all the necessary studies have been completed and the diagnosis has been correctly made, the patient should undergo an examination by a specialist in order to completely eliminate the likelihood of the disease and adverse consequences, then the mitral valve. Once the diagnosis is established, the patient should be examined 3-5 times a year.
Symptoms
Mitral regurgitation can be pronounced at the time of valve insufficiency or when mitral valve prolapse is detected. During contraction of the left ventricular muscle, some blood may return to the left atrium through an incompletely closed mitral valve. At the same time, the left atrium fills with blood that flows from the lungs.
Excess blood during the contraction of the atria enters the left ventricle, which is forced with redoubled force to pump a larger volume of blood into the aorta, which can cause it to become thicker and then expand.
For a certain period of time, mitral valve dysfunction may remain unnoticed by the patient, since the heart, to the extent possible, compensates for blood flow by expanding and changing its own cavities.
At this stage of the disease, laboratory symptoms may be absent for years, and during a significant volume of blood returning to the atrium, it may become wider, the veins of the lungs may fill with excess blood, and symptoms of pulmonary hypertension will appear.
The causes of this disease, which is the second most common acquired heart defect after changes in the aortic valve, include:
- Rheumatism;
- Prolapse;
- Atherosclerosis, deposition of calcium salts;
- Certain connective tissue diseases, autoimmune processes, metabolic disorders;
- Ischemia.
During this disease, the only sign is often a murmur near the heart, which is detected by auscultation; the patient does not complain, and no signs of circulatory failure are observed. An ECG makes it possible to detect minor divergence of the leaflets with the least disruption in blood flow.
Possible complications
The likely consequences are:
- Heart failure. Considered the leader in frequency. The cause of death in patients with mitral regurgitation in 80% of cases is acute suspension of the muscular organ.
- Myocardial infarction. As a result of malnutrition of cardiac structures. If the process continues for a long time, but does not reach a critical mass, insufficiency and dysfunctional disorder are likely.
- Coronary heart disease (CHD).
- Stroke. Acute deviation of blood supply to brain structures.
- Arrhythmias of various kinds. Fibrillation, paired or group extrasystoles.
Diagnostics
- Examination and conversation with the patient make it possible to determine symptoms and identify pathology. It is necessary to find out about a person’s previous illnesses and his predisposition. Analyzes help detect inflammation, cholesterol, sugar, protein in the blood and other characteristics. When antibodies are detected, it is possible to see inflammation or infection in the myocardium.
- The initial diagnosis can be made in a clinical setting and confirmed by ECG. Doppler ECG is used to detect the flow of regurgitation and to assess its severity. A 2-dimensional ECG is used to identify the causes of this disease and detect pulmonary arterial hypertension.
- If endocarditis or valve thrombi are suspected, transesophageal echocardiography can be used to visualize the mitral valve and left atrium in much more detail. It is prescribed in situations where valve plastic surgery is needed, rather than replacement, since diagnosis makes it possible to confirm the absence of severe fibrosis and calcification.
- First, an electrocardiogram and chest x-ray are done. Thanks to the ECG, hypertrophy of the left atrium and dilatation of the left ventricle with coronary heart disease or its absence are revealed.
- A chest x-ray demonstrates potential swelling in the lungs. Changes in the shadow of the heart are not detected when there are no chronic pathological processes. Chest X-ray in chronic forms shows hypertrophy of the left atrium and left ventricle. Possible congestion of blood vessels and swelling of the lungs.
- Before surgery, cardiac catheterization is performed to detect coronary heart disease. A pronounced atrial systolic wave is detected in the process of detecting the pressure of pulmonary artery occlusion during ventricular systole. Cardiac systole - what is it?
- Sometimes other methods are used to make a diagnosis, but the data are considered the main ones, and often they are quite enough.
How does pulmonary regurgitation occur?
When the myocardium and the entire valve apparatus are functioning normally, during contraction of the heart chamber the valve leaflets close tightly. Due to various diseases of the heart valves, these functions may be impaired.
The appearance of pulmonary regurgitation is usually associated with impaired functioning of the pulmonary valve. In this case, during the relaxation of the heart, blood is sent back to the ventricle from the pulmonary artery.
Causes
This disease is a consequence of damage to the valve itself or the structures of the heart. It can be acute or chronic and is provoked by various difficulties and ailments.
Due to damage to various cardiac structures, the valve performs its function weaker. Both the valves and the muscles that ensure their operation, or the tendons that control the valves of the mitral valve, suffer.
Mitral regurgitation is promoted by the following processes:
- dysfunction or damage to the papillary muscles;
- endocarditis;
- MK lesions;
- sudden left ventricular hypertrophy;
- ischemia;
- inflammatory processes of a rheumatic nature.
It must be said that grade 1 mitral regurgitation is quite difficult to diagnose. When the disease occurs in an acute form, it is accompanied by swelling in the lungs and ventricular failure. The patient feels a lack of oxygen. But often the above manifestations will be felt in moderate to severe cases of the disease.
Reasons for development
During regurgitation of the pulmonary valve of the pulmonary artery, blood flows back from the artery into the ventricle and atrium of the right heart in diastole. This deviation can develop for various reasons:
- Primary and secondary pulmonary hypertension,
- Chronic and acute diseases of the pulmonary and bronchial system, including emphysema, obstructive diseases of the respiratory system,
- Pathological changes in the structure of the heart as a result of ischemia, congenital and acquired defects, cardiomyopathy,
- Formation of blood clots in the pulmonary artery,
- Pickwick's syndrome, characterized by respiratory failure,
- Mitral stenosis,
- Damage to the valve leaflets by syphilis,
- Endocarditis of infectious origin,
- Rheumatic chronic heart disease,
- carcinoid syndrome,
- Drug use by injection.
Treatment
When there is an acute form of the disease, the administration of diuretics and vasodilators is required. No special therapy is needed for mild forms and initial stages of the disease.
In the subcompensated stage the following is prescribed:
- angiotensin-converting enzyme inhibitors,
- beta blockers,
- vasodilators,
- cardiac glycosides,
- diuretics.
When atrial fibrillation is developed, indirect anticoagulants are used.
The treatment method for regurgitation is selected based on the cause that caused it, its severity, the presence of heart failure and accompanying pathological processes.
Probably surgical correction of malfunctions in the structure of the valves, medicinal conservative treatment, which is aimed at normalizing blood flow in the organs, counteracting arrhythmia and circulatory failure.
Degrees of the disease
There are 4 degrees of this disease, which are characterized by the length of the return flow of blood into the cavity of the right atrium.
Tricuspid regurgitation 1st degree - what is it? In this case, the backflow of blood is insignificant and barely detectable. In this case, the patient does not complain about anything. There is no clinical picture.
With a diagnosis of “tricuspid regurgitation of the 2nd degree,” the reverse flow of blood is carried out within 2 cm of the valve walls. The clinical picture at this stage of the disease is almost absent; pulsation of the jugular veins may be weakly expressed.
Grade 3 tricuspid valve regurgitation is defined by backflow of blood more than 2 cm from the tricuspid valve. In addition to pulsation of the neck veins, patients may experience palpitations, weakness and fatigue; even with little physical exertion, slight shortness of breath may be observed.
Stage 4 disease is characterized by a pronounced backflow of blood over a long distance from the valve into the cavity of the right atrium. In severe cases, the patient may experience symptoms of severe heart failure and pulmonary hypertension (pulmonary and tricuspid regurgitation). In this case, the symptoms listed above are joined by others. Namely: swelling of the lower extremities, a feeling of pulsation on the left in the sternum, which intensifies with inspiration, disturbance of heart sounds, cold extremities, an increase in the size of the liver, ascites (accumulation of fluid in the abdominal cavity), abdominal pain, and with the rheumatic nature of this disease, it can be observed aortic or mitral valve disease.
Possible complications, consequences, what are the dangers?
Adverse consequences of the disease:
- arrhythmia - appears due to disruptions in normal movement
the presence of electrical impulses in the heart; - atrioventricular block - the progression of the electrical impulse from the atria to the ventricles worsens;
- secondary infective endocarditis;
- heart failure (decreased heart rate with inadequate blood supply);
- pulmonary hypertension (pressure in the vessels of the lungs increases due to stagnation of blood).
Patients who have undergone surgery are at risk of experiencing the following consequences:
- thromboembolism of the arteries of internal organs . A blood clot appears at the surgical site. The most unsafe are ischemic stroke (part of the brain dies due to the cessation of its blood supply) and mesenteric thrombosis (part of the intestine dies due to the cessation of its blood supply);
- infective endocarditis (inflammation of the inner lining of the heart);
- atrioventricular block (the propagation of the electrical impulse from the atria to the ventricles slows down and completely stops);
- paravalvular fistulas (sections of the sutures that hold the artificial heart valve are cut through when blood flow occurs behind it);
- prosthetic thrombosis (blood clots form near the prosthetic valve, which interfere with proper blood flow);
- destruction of a biological prosthesis with a similar surgical intervention;
- calcification of a biological prosthesis (calcium salts are deposited in an artificial heart valve, which is created from animal tissue).
Prognosis for such a disease varies from the degree and form of the main disease that formed such a heart defect, from the expression of the defect in the valve and from the general condition of the myocardium.
When a moderate stage of the disease is observed, the person’s normal condition and performance will remain for several years.
A severe form of the disease, a decrease in myocardial strength, quickly leads to the appearance of heart failure (blood stagnation develops as a result of a decrease in cardiac output). 9 out of 10 people live more than 5 years, 4 out of 5 patients live more than 10 years.
Recommendations for illness, what not to do?
- Initial preventive measures during the 1st degree of illness.
- Prevention of diseases that are accompanied by damage to the valve apparatus, that is, rheumatism (a systemic inflammatory disease with cardiac damage), infective endocarditis (a disease of the inner lining of the heart), etc.
When there is a disease that is accompanied by damage to the valvular apparatus of the heart, the occurrence of heart disease can be prevented by early effective therapy:
- Hardening the body.
- Treatment of foci of persistent infection:
- during chronic tonsillitis - surgery to remove tonsils;
- during the period of caries (formed under the influence of microparticles that destroy teeth) – voids are filled, etc.
- Secondary preventive measures are aimed at preventing the development of damage to the valve apparatus and heart failure.
- Conservative therapy for patients with this disease. They use medications: drugs with a diuretic function - help remove excess fluid;
- inhibitors - used to prevent deficiency;
- nitrates – promote vasodilation, improve blood flow, lower pressure in the pulmonary vascular system;
- potassium supplements – increase myocardial tone;
- glycosides (help increase heart rate, slow it down, are used during atrial fibrillation and heart failure).
- antibiotic treatment;
Treatment methods
Treatment of grade 1 mitral valve prolapse is not required in some cases. This applies to identifying such changes during ultrasound in a child who does not experience any symptoms of the disease. At the same time, children have no restrictions for physical education, but it is not advisable to engage in professional sports.
If there are symptoms of the disease, then it is necessary to select therapy to reduce or eliminate them. In each case, the doctor prescribes therapy, taking into account individual characteristics. The main groups of drugs used in the treatment of MVP include:
- sedatives (calming), which are used when disorders of the autonomic nervous system occur;
- beta blockers are indicated for tachycardia and extrasystole;
- products that improve myocardial nutrition (panangin, magnerot, riboxin) contain electrolytes necessary for the functioning of the heart;
- Anticoagulants are prescribed quite rarely, only for concomitant thrombosis.
It is very important to optimize your lifestyle, because the symptoms are often aggravated by chronic fatigue and nervous tension. Necessary:
- observe the rest and work regime;
- maintain motor activity at an acceptable level (as far as general condition allows);
- periodically go to specialized sanatoriums, where they conduct restorative courses of massage, acupuncture, mud therapy, etc.
In some cases, herbal medicine is recommended, which includes the use of infusions from various mixtures containing motherwort, hawthorn, sage, and St. John's wort.
Mitral regurgitation in a child
- Mitral valve prolapse may be different depending on the degree of deflection
leaflets and the degree of reverse blood flow through the valve (regurgitation). - Regurgitation itself during pregnancy is not considered a prohibition for pregnancy or childbirth, but only when the valve performs its main function - ensuring one-way blood flow.
- For children, proper diet and the functioning of the heart and circulatory system play an important role, but failures are quite common. Most often, valve defects with insufficiency and return of blood in childhood are predetermined by genetic developmental abnormalities.
- Severe regurgitation , if there is an abnormal cardiac structure, appears almost immediately after birth with symptoms of respiratory failure, blueness of the skin, and insufficiency in the right ventricle.
- Often, significant failures can lead to death, so every mother should take care of herself before pregnancy and be promptly observed by an ultrasound specialist while carrying a child.
Manifestation of pulmonary valve dysfunction
Stage 1 pulmonary valve regurgitation often occurs without any special symptoms. In some cases, symptoms of functional heart failure associated with impaired functioning of the right ventricle are noted. The first stage of tricuspid regurgitation does not cause significant changes in the human vascular system. The entry of significant volumes of blood into the ventricle can lead to an increase in the thickness of its walls, and subsequently dilatation. These changes provoke the appearance of signs of acute insufficiency of the pulmonary artery and heart valves, congestion in the venous system.
The main signs of pulmonary artery regurgitation are:
- Blue skin
- Frequent shortness of breath,
- Swelling,
- Rapid pulse.
Against the background of congenital heart pathologies, signs of the disease can be detected during the first months after the birth of the child. In most cases, they manifest themselves in severe form and cannot be compensated. The disease is accompanied by cyanosis of the skin, insufficiency of respiratory function, and symptoms of dysfunction of the right ventricle. In its most severe manifestations, this pathology leads to cardiac arrest. For this reason, pregnant women are prescribed ultrasound diagnostics, which can detect defects and pathological development of the fetus.
Attention: physiological pulmonary regurgitation (outside of pathologies) occurs without obvious clinical signs and is not dangerous to health.
Such phenomena also occur on other heart valves. Symptoms of tricuspid regurgitation and valve insufficiency can only manifest themselves when a large volume of blood is refluxed into the right atrium, which causes dilatation and hypertrophy of the right ventricle with further hemodynamic disturbances.
Mitral valve insufficiency leads to overload of the left atrium first, and then the ventricle.
Attention! With regurgitation of the 1st degree, the return of blood into the blood is characterized by an insignificant volume, and in itself cannot overload the ventricle. Therefore, during this process, the size of the cavities and the thickness of the myocardium are not disturbed, and there are no negative hemodynamic changes.