Is it possible to play sports with prolapse?
In order to determine the degree of risk for an athlete due to valve prolapse, the following indicators are taken into account:
- complaints of fatigue and shortness of breath;
- arrhythmia and early repolarization on the ECG; when they are combined, an additional transesophageal study is performed;
- the degree of sagging of the valves and their length;
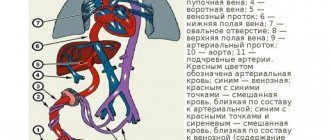
- the presence of reverse blood flow into the left atrium;
- myxomatous changes in the leaflets (increase in thickness above 5 mm) of the valve apparatus.
If the examination reveals the opposite direction of blood flow during the period of ventricular contraction, then you need to stop exercising for a while and undergo treatment. Based on the results of the therapy, a conclusion will be made about the possibility of further sports activities.
Sports doctors are especially wary if MVP is detected in children or adolescents. At the same time, they have a typical asthenic physique, characteristic of genetic pathology - tall stature, deformed or flattened chest.
Individuals may be allowed to engage in non-severe sports if there are no complaints, grade 1 valve prolapse, mild regurgitation, no signs of MVP, extrasystoles and ischemia on the ECG, and good exercise tolerance.
We recommend reading about mitral valve prolapse. You will learn about the reasons for the formation of MV prolapse, types of MVP, symptoms and diagnosis, treatment of MVP. And here is more information about mitral heart disease.
During pregnancy
If a diagnosis of grade 1 mitral valve prolapse is made, pregnancy, as a rule, proceeds favorably and without symptoms.
This is the most common heart pathology, occurring in 17% of young women. The state of health and general well-being for 9 months largely depends on the form, degree and nature of the pathology.
In general, there are no special contraindications for women in labor with MVP, since minor deformation does not affect the state of health. But if the disease is accompanied by weakened heart activity, it is likely that a cesarean section will be used. In addition, changes in heart rhythm sometimes occur.
General recommendations for managing pregnancy with grade 1 mitral valve prolapse syndrome:
- do not overcool or overheat;
- you cannot sit for a long time;
- exclude prolonged stay in baths and saunas;
- get more rest;
- eat foods high in potassium and magnesium;
- take vitamin and mineral complexes;
- walks in the open air.
There is a possibility that pregnancy will be accompanied by gestosis, which is characterized by the following symptoms:
- swelling;
- increased blood pressure;
- convulsions;
- decrease in protein content in the body.
Such complications can lead to insufficient oxygen supply to the fetus. In medical practice, the possible occurrence of premature birth is noted. Treatment of MVP with medications is used only in special episodes caused by severe prolapse.
In most cases, MVP is transmitted to the child, so it is very important to manage the pregnancy under the supervision of a cardiologist.
Half of the female population has a pathology, but not everyone is aware of it. When undergoing a mandatory medical examination, mitral valve prolapse is most often discovered in pregnant women. Many women immediately wonder about the compatibility of the disease and future motherhood.
The occurrence of valve deflection is associated with increased load on the heart and increased blood ejection into the aorta. Fetal hypoxia and growth retardation are a consequence of hypoxia caused by pathology.
If there was no regurgitation in the first months of pregnancy, despite the diagnosed prolapse, then the risk of developing pathology is almost zero.
Most often, the consequence of the disease in pregnant women is premature birth or weakened labor. In this case, a caesarean section becomes necessary. If arrhythmia may occur, drug treatment is also required.
Moderate or severe course of the disease is determined by the following symptoms:
- Autonomic-vascular dysfunction, expressed by heart pain, lack of air, cardiac arrhythmia, chills;
- Vascular disorders, including frequent headaches, swelling;
- Hemorrhagic, which occurs in the form of bruises with the slightest pressure and bleeding from the nose;
- Psychopathological: sudden feeling of anxiety and fear, mood swings.
Recommendations for pregnant women with stage 1 mitral valve prolapse:
- Avoid sudden changes in temperature, heat and cold;
- Do not sit for a long time;
- Rest in a reclining position.
- Planning pregnancy is a necessary measure to reduce the risk of pathology in a woman.
Mitral valve prolapse and contraindications to sports
With mitral valve prolapse, professional sports are contraindicated; patients with the following conditions are not allowed to compete:
- at least one loss of consciousness (it can be provoked by disturbances in the rhythm of heart contractions);
- sudden increase in heart rate, ECG detection of periods of paroxysmal tachycardia with a rhythm source in the atria, ventricles, fibrillation, flutter, Wolf-Parkinson-White syndrome, frequent or group extrasystoles;
- reverse movement of blood through the valve according to ultrasound of the heart;
- decreased strength of left ventricular contractions, leading to low ejection fraction (less than half normal);
- previous vascular thrombosis;
- with a hereditary predisposition to prolapse and cases of sudden cardiac arrest in blood relatives with a similar diagnosis.
What sports are acceptable for grade 1-3 mitral valve prolapse?
Although there are no clear criteria by which it is possible to determine an acceptable sport for each patient with MVP, there is a division into dangerous and relatively non-traumatic for the heart. At the same time, the general approach to the selection of athletes is that grade 3 prolapse is a categorical contraindication, and for grades 1 and 2 load restrictions are introduced.
Is it possible to go jogging? For grade 1 prolapse, running is permitted, and for grade 2 prolapse, permission can be issued with circulatory compensation confirmed by a diagnostic study.
Is swimming allowed? Synchronized swimming is not indicated for grade 2 MVP, since due to prolonged exposure to water there is a risk of loss of consciousness. For regular swimming, the restrictions are the same as for other non-strength sports.
What kind of loads are possible in the gym? Patients with MVP should not lift weights; their own body weight is recommended as a burden; jumping should be avoided. When training, you should prefer cardio.
Is dance training acceptable? Since the load when dancing is the fast rhythm of movements, with 1st degree of prolapse such hobbies are not excluded. You just need to choose types that exclude the support of partners, as this can lead to sudden disruption of cardiac and cerebral circulation.
Is it possible to choose boxing if you have valve prolapse? This sport is associated with the risk of sudden impacts to the chest, which can cause the valve to rupture under intense impact, therefore boxing is prohibited for all athletes diagnosed with mitral valve prolapse, even with 1 degree of prolapse.
Diagnostics
If typical signs of mitral valve prolapse are noted, your emergency doctor will ask questions about your symptoms, general health, lifestyle, and medications.
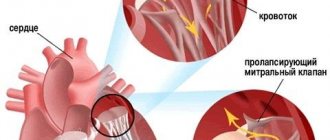
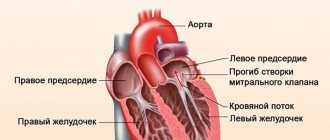
Physical examination is not always helpful in identifying signs that indicate mitral valve prolapse. In particular, during auscultation there may be a “click” with each opening of the valve or a heart murmur similar to a “cat purring”.
Diagnostic tests help rule out serious heart disease and also help assess the contractile function of the heart and the performance of the valves. These tests are non-invasive, painless and quick to perform. The most common diagnostic methods are:
- Electrocardiogram (ECG) : records the rhythm and electrical activity of the heart from different leads. This information is very useful for diagnosing various heart problems such as cardiac arrhythmias, myocardial infarction or hypertrophy of the heart muscle.
- Echocardiogram (echocardiogram): relies on the analysis of sound waves (ultrasound) that are displayed as a moving image of the heart on a video screen. This test can evaluate the function of all heart valves, as well as determine the degree to which the mitral valve bends backward when it closes. Usually echocardiography is sufficient to establish the diagnosis of mitral valve prolapse, but in some cases the method cannot determine the anomaly.
- Holter monitoring: A small device records the heart rhythms and electrical activity of the heart over an extended period, usually 24 hours. During this time, the device is constantly with the patient, usually near the chest. A person's heart activity continues throughout the recording period, so any abnormalities seen on an ECG may be related to what the person was doing and feeling at the time. This test may be recommended if a person experiences dizziness, fainting, or palpitations.
- Stress tests: Similar to a regular ECG, except that they show the heart's response to stress, usually in the form of physical activity. When ECG electrodes are connected, the person walks on a treadmill or rides a bicycle. Most people with symptoms, especially chest pain or signs of arrhythmias, should have a stress test because in such cases there is often underlying heart disease.
PMC degrees and physical activity
With grade 3 regurgitation (reflux of blood into the atrium), physical activity in sports is not indicated. Physical therapy is permitted after the examination. In the initial (first) degree there are no restrictions, but the patient is not allowed to participate in sports competitions in almost all forms. Exceptions may be badminton, shooting, cricket.
If the second degree is detected, then the following are allowed:
- table tennis,
- figure skating,
- sprint,
- swimming,
- gymnastics,
- judo.
Before starting equestrian and motorcycle sports, car racing, diving, and synchronized swimming, a comprehensive examination and an individual opinion from a cardiologist are required.
What are the dangers of excessive physical activity during MVP?
The asymptomatic course of MVP usually does not cause problems for athletes. With significant changes in the configuration of the valve apparatus, the following complications arise:
- Mitral valve insufficiency
Mitral valve insufficiency; - acute or chronic hemodynamic disturbance;
- infective endocarditis;
- vascular thromboembolism;
- arrhythmia;
- sudden cardiac arrest.
The reasons for the reverse flow of blood during MVP are excess tissue (thickening of the valves), widening of the hole to which they are attached, lengthening of the tendon threads (chords). Leaf rupture often occurs after chest trauma. Blockage of cerebral vessels develops quite rarely in the form of ischemic stroke or intermittent disturbances of cerebral blood flow.
Sudden death with MVP occurs, as a rule, among family cases of pathology, its main cause is an attack of ventricular fibrillation. Predisposing risk factors for this complication include complex arrhythmias, a long QT interval, and signs of myocardial ischemia on the ECG.
These changes may not be detected during a routine ECG study. Therefore, if complaints include short-term loss of consciousness, patients should undergo ECG monitoring or functional stress tests.
If at least one risk factor has been identified, then sports, and especially participation in competitions, should be stopped. At the same time, ordinary physical activity is not limited. Athletes with MVP, even with good load tolerance, achieve lower results than healthy individuals.
Watch this video about playing sports for heart disease:
Possible causes of the disease
Modern researchers name a large number of causes of MV prolapse, so they can be systematized as follows.
Valvular diseases
- Increased number of leaflets in the heart valve,
- Elongated filaments of the chord and their abnormal attachment,
- Changed structure of papillary muscles.
Changes in the structure of the mitral valve
- Increase in the size of the fibrous ring,
- Valves expansion,
- Extended LV chord.
Other pathologies
- Preliminary relaxation of the valve leaflet,
- Myocarditis,
- SVC syndrome.
Pathologies of the innervation of the valve apparatus
- Neuroses and hysterical states,
- Dystonia,
- Anorexic exhaustion.
Doctors consider mitral valve prolapse as a polyetiological disease, so it is difficult to name the exact cause of the pathology.
If a person has first-degree MV prolapse, this indicates that the mitral valve is not able to maintain the required pressure. The valves bend under the blood flow. There are first, second and third degrees of prolapse. The development of pathology depends on the hereditary factor and individual characteristics of the body.
The best exercise for mitral valve prolapse
The basis of the health system for patients with MVP is cyclic exercises to increase endurance and aerobic reserves of the body. The most useful of them are walking and slow running. You need to start training with the very minimum load, which gradually increases. Features of exercises for mitral valve prolapse:
- The pace of movements should be slow.
- During static loads, there is no need to hold or deepen your breathing.
- You need to run only on soft soil, for at least 3 months running alternates with walking, the step length is minimal.
- The most optimal time for running or brisk walking is 30 minutes, which can be divided into three 10-minute cycles. There must be at least 4 classes per week.
The indicator of effectiveness is heart rate. It is calculated using the formula: 220 minus age, the favorable interval is in the range of 50 - 75 percent of the result obtained. Less load will not bring any benefit, and more is dangerous to health.
With regular exercise, the heart works in a more economical mode, the content of atherogenic lipids and the effect of stress hormones on the myocardium are reduced, the formation of blood clots is inhibited, and the rhythm and strength of contractions are normalized.
Running for mitral valve prolapse
Exercise therapy for mitral valve prolapse
General rules for conducting physical therapy classes for mitral valve prolapse:
- activity should be moderate, overexertion is not allowed;
- breathing must be smooth, it cannot be held at the height of the load;
- it is necessary to control the pulse rate; it is not allowed to increase above the limit values (the favorable interval is 50 to 75% of 220 minus age);
- Strength exercises and heavy lifting are not recommended;
- when compiling a complex, it includes movements involving large muscle groups;
- It is mandatory to warm up before training, and relaxation at the end;
- the duration should not exceed 30 minutes, especially in the first days; in just a week you need to train at least 150 minutes;
- on days free from physical therapy, dosed walking is indicated.
Exercise therapy for prolapse
Main preventive measures
The heart muscle, like the entire vascular system, can be strengthened - this will help reduce the degree of valve regurgitation, weaken the effect of prolapse on the heart, and allow you to engage in professional sports.
What preventive exercises will help restore normal heart function? The benefits will come from measured workouts that strengthen the entire cardiovascular system and muscle groups. These include:
- moderate jogging;
- bicycle rides;
- sets of gymnastic exercises.
The peculiarity of such training is its universal nature - joints, blood vessels, muscles of different areas of the body work.
Restoration of the cardiovascular system will be better with frequent consultations with the attending physician, who monitors changes in the functioning of the body. Prevention of mitral valve prolapse requires careful planning of activities and limiting the load on the heart (otherwise the disease will only worsen).
Exercises for prolapse
An approximate set of exercises for prolapse:
- walking in place with acceleration and deceleration (1 minute);
- high bent leg raises (30 seconds);
- walking on toes and heels (30 seconds each);
- circular movements of the arms forward and backward (10 times);
- body turns (hands on the belt, 8 hands in each direction);
- circular movements of the hips (10 circles);
- slow run 2 minutes;
- raise your arms up through your sides and sharply lower them down, tilting your torso (repeat 5 times).
Lying on your back:
- raise bent legs at the knees (inhale), lower them with exhalation (8-15 repetitions depending on how you feel);
- imitation of cycling (1 minute, then relax for 30 seconds);
- raise your legs at a right angle and, without changing position, lower them to the right and left of the body (10 repetitions);
- rest for 1 minute.
We recommend reading about physical activity for arrhythmia. From the article you will learn about permissible loads for arrhythmia, options for physical exercise for sinus and atrial fibrillation. And here is more information about useful exercises for arrhythmia.
In childhood and adolescence, dosed physical activity stimulates the development and growth of the body and activates metabolic processes. This helps the child adapt to stress and reduces the risk of complications that may arise with MVP. Therefore, excessive restrictions in physical development worsen the course of this pathology.
Mitral valve prolapse with an asymptomatic course and the absence of reverse blood flow during contraction of the left ventricle is not a contraindication to sports. To determine the correct level of physical activity, an ECG with functional tests is indicated.
Strength and traumatic sports are not recommended for patients with MVP; grade 3 prolapse implies a complete refusal of sports exercises, and for grades 1 and 2, the type of exercise depends on hemodynamic parameters. Therapeutic exercises are recommended for all patients; the indicator of its effectiveness is the pulse rate.