Changes in the heart and blood vessels
Fetal circulation
During pregnancy, another blood circulation circle is formed in a woman’s body - the placental one. The placenta is an organ that has a close relationship between the vessels of the uterus and the fetus.
It is through the vessels of the placenta that the unborn baby receives oxygen and nutrients necessary for its growth and development. Due to the formation of the so-called third circle of blood circulation, the volume of circulating blood in a woman’s body increases by 40-50%, the heart experiences a greater load, pumping an increased volume of blood, therefore cardiac output also increases, overflow of the heart chambers and their slight expansion may occur, and also an increase in the mass of cardiac muscle tissue.
The increased level of hormones in the body of a pregnant woman helps to reduce the tone of peripheral vessels, which causes a slight decrease in blood pressure in the early stages. Reduced vascular tone and increased blood volume cause the heart to contract with greater intensity, which results in an increase in contraction frequency; a heart rate of 100 beats per minute in pregnant women is not a pathology, but rather an adaptive reaction of the body.
During pregnancy, the body of a healthy woman copes with the stress of the cardiovascular system, and after childbirth, all indicators of the heart and blood vessels return to normal. But in women with cardiac pathology, pregnancy can worsen the course of existing heart disease or provoke the emergence of new ones. How does pregnancy proceed in women with prolapse? Can prolapse occur during pregnancy or childbirth? Let's try to find out.
Course of pregnancy
MVP is not a contraindication for pregnancy. For most women, pregnancy proceeds without complications and ends with physiological labor on time.
In some situations, maternal complications arise, the most significant of which is hemodynamically significant mitral regurgitation. This term means the following: the backflow of blood from the LV cavity into the left atrium is so significant that it causes a general disturbance of blood circulation in the heart and large vessels. This complication is caused by the restructuring of the tissues of the valve leaflets with the loss of their normal properties - progressive myxomatous degeneration.
Initially severe MVP with significant mitral regurgitation predisposes to such a development of events, even if before pregnancy the heart coped with this load and the woman felt well.
Symptoms of significant mitral regurgitation are associated with stagnation of blood in the pulmonary circulation. This increases the pressure in the vessels of the lungs, and then in the pulmonary trunk. Pulmonary hypertension occurs. Clinically, it is manifested by shortness of breath with minimal physical exertion and in the supine position, cough mixed with pinkish sputum, fainting, and severe weakness.
Subsequently, the increased pressure spreads to the right side of the heart. Their wall is thinner than the left chambers, and they quickly cease to cope with their function. Right ventricular heart failure develops. It is manifested by liver enlargement, edema, ascites and other signs of fluid retention in the body.
LA stretching caused by the reflux of blood from the LV causes atrial rhythm disturbances: extrasystole, paroxysmal tachycardia, or even atrial fibrillation. These arrhythmias contribute to the formation of blood clots and thrombi in the left ear. Under unfavorable conditions, such blood clots “fly out” from the atrium into the LV, and from there into the systemic circulation, becoming the cause of strokes and heart attacks of various organs.
Significant mitral regurgitation can cause sudden death. In addition, it increases the risk of infection settling on the valve with the development of endocarditis.
What is mitral valve prolapse?
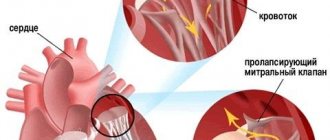
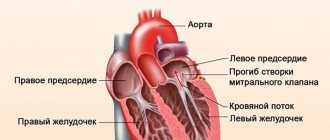
MK prolapse
The heart consists of right and left sections, between the left sections there is a bicuspid or mitral valve. It is responsible for the flow of blood from the atrium into the ventricle, as well as for preventing the reverse flow of blood from the ventricle during contraction of the latter. The bicuspid valve is a safety device that regulates the reverse flow of blood.
It consists of two doors adjacent to each other in such a way that there is not the slightest gap between them. It is this tight fit at the moment of slamming of the valves during contraction of the ventricle that ensures the impossibility of backflow of blood or regurgitation. The valve leaflets are dense, elastic, retaining their shape under blood pressure.
But situations arise when one or two valve leaflets begin to sag, prolapse towards the left atrium under blood pressure during ventricular contractions. This condition is mitral valve prolapse. If the mitral valves not only sag, but also do not close, forming a hole, blood from the ventricle flows back into the atrium, regurgitation is formed - reverse effusion.
Which women require special attention?
Pregnant women should be under special supervision when:
- expression of prolapse of the mitral valve leaflets;
- acute violation of the closing function of the valves;
- severe regurgitation of blood from the left ventricle into the left atrium;
- combined mitral valve defects with other cardiac pathologies.
Pregnancy and mitral valve prolapse, as a rule, proceed harmoniously, the defect does not cause any special complications during natural childbirth. Delivery can be carried out on time; in case of complications, surgery is required.
Before or during?
Prolapse in a pregnant woman
It is very important to know when prolapse occurs in a pregnant woman: before or during pregnancy. If a woman did not have any heart problems before pregnancy, the condition of the valves was fine, and during pregnancy a slight deflection of the valve without reverse blood flow occurred, and the woman’s condition is good, then there is no need to worry.
This condition indicates an increased load on the chambers of the heart and most likely, after childbirth, the valve apparatus will be restored. It’s another matter if a woman had prolapse before the interesting situation, with hemodynamically significant regurgitation, this condition is quite serious, and the management and course of pregnancy is determined by a gynecologist together with a cardiologist.
Why does prolapse occur?
Cardiomyopathy
There are two forms of prolapse - congenital and acquired. The acquired form is caused by various diseases of the woman: ischemia, systemic diseases, trauma, cardiomyopathies. The congenital form implies valve defects from birth and has a hereditary predisposition to connective tissue weakness.
It is noteworthy that before pregnancy this form may not manifest itself in any way, but with an increase in the load on the heart and blood vessels, it can make itself felt by the development of regurgitation and mitral insufficiency. The causes of congenital bicuspid prolapse can be the inferiority of the connective tissue of the valves, elongation of the chords, and other minor anomalies. Women with prolapse are most often thin, asthenically built, tall, with low muscle mass development.
Pathogenesis of disease development during pregnancy
During pregnancy, the volume of circulating blood in a woman’s body is replenished by 40%, as a result of which the volume of the heart also increases.
As pregnancy progresses, moderate tachycardia develops, which ensures normal blood circulation for the fetus.
With the enlargement of the heart cavities, in some women, compensatory mechanisms do not form, the valve leaflets cannot withstand the load, and do not close fully during systole.
Mitral valve prolapse and pregnancy are a very common combination, so all pregnant women should undergo mandatory consultation with a cardiologist.
Mitral valve prolapse of the 1st degree may not manifest itself symptomatically, and the acquired defect is determined during routine echocardiography. With a normal pregnancy in the third period, a woman can give birth on her own.
If the disease progresses after childbirth, the following symptomatic signs appear:
- disruption of the cardiac conduction system;
- shortness of breath and a sharp change in the frequency of respiratory movements;
- swelling of the soft tissues of the extremities.
In order to get rid of the risk of complications during childbirth and the postpartum period, pregnant women need to maintain strict bed rest, reduce the amount of physical activity and normalize sleep. It is also recommended to reduce the amount of table salt consumed throughout the day, this will reduce the risk of developing eclampsia during childbirth.
Classification and degrees of prolapse
Degrees of blood reversal
There are several classifications: according to the degree of sagging of the valves, as well as the degree of backflow of blood or regurgitation. Among cardiologists, the second one turns out to be more informative. According to the degree of prolapse:
- 1st degree - the valves bulge into the atrium by 0.2-0.6 cm,
- 2nd degree - by 0.6-0.9 cm,
- Grade 3 - more than 0.9 cm.
If a non-pregnant woman has been diagnosed with 1st degree of sagging, then during pregnancy there is a very high probability that the sagging will progress to the second or third degree. At the same time, the degree of sagging is not always proportional to the severity of the condition. For example, the third degree without regurgitation has a more favorable prognosis than the second with regurgitation. According to the degree of blood reversal:
- Regurgitation 1st degree - reverse blood flow to 25% of the entire depth of the left atrium,
- 2nd degree - up to 50%,
- 3rd degree - up to 75%,
- 4th degree - retrograde blood flow reaches the opposite edge of the atrium.
Grade 3-4 regurgitation may be a contraindication for pregnancy.
How does a pregnant woman with prolapse feel?
Shortness of breath during pregnancy
Pregnant women with prolapse without regurgitation or with its minimal degree may have no complaints. Their health does not suffer and pregnancy can proceed as in women without prolapse. Nonspecific complaints occur periodically in the form of general weakness, increased fatigue, headaches, stabbing pain in the chest. If mitral regurgitation develops during prolapse, the complaints progress: shortness of breath may occur, even at rest, dry cough with hemoptysis, swelling, pain in the right hypochondrium, acrocyanosis or facies mitralis may occur.
What is the danger of bicuspid valve prolapse during pregnancy?
If a pregnant woman is diagnosed with prolapse without regurgitation or with minimal significance, there is no danger to the health of the woman and the baby. Pregnancy is indicated, the woman is monitored by an obstetrician-gynecologist and a cardiologist; usually such a pregnancy does not entail any complications.
But if regurgitation is higher than grade 2, mitral insufficiency develops, which can lead to circulatory disorders, hemodynamic disorder, and stagnation in both the small and large circles. This can lead to the development of arrhythmias, thromboembolism, pulmonary edema, and death. If the woman’s condition is serious and circulatory failure has developed, then the pregnancy can be terminated for health reasons.
Diagnostic methods
Echocardiographic examination of the heart
Mitral sagging is diagnosed using the following methods:
- when listening to heart sounds with a stethoscope, a systolic murmur can be heard at the apex,
- Echocardiography,
- EchoCG with Doppler,
- ECG,
- Holter ECG.
Diagnostics
When making a diagnosis based on the patient's medical history, it is necessary to differentiate primary mitral valve prolapse from secondary one.
The auscultatory picture is characterized by clicks and systolic murmur, which is most pronounced with little physical activity.
| ECG | Allows you to determine myocardial hypertrophy of the left atrium and heart rhythm disturbances. |
| Echocardiography | Confirms the sagging of the valve leaflets into the cavity of the left atrium during ventricular contraction. |
| X-ray | With its help, an enlargement of the left cavities of the heart is visible. |
| Doppler echocardiography | Helps to examine the direction of blood flow with severe mitral regurgitation. |
| Screening | Genetic testing. |
If a heart defect is suspected, a pregnant woman from the antenatal clinic department is referred for examination to a therapist and cardiologist
murmur at the apex, accent of the second tone, change in the position of the heart. Therefore, it is necessary to use ECG, phonocardiography, ultrasound, spirometry, and determination of central venous pressure. Timely diagnosis of cardiac dysfunction in pregnant women is extremely important, since atrial tachycardia leads to the rapid development of heart failure.
One of the diagnostic methods is ECG
Management of pregnancy depending on the severity of prolapse
If a woman during pregnancy, after all the necessary examination methods and consultation with a cardiologist, is diagnosed with 1st degree prolapse with minor regurgitation, then the patient does not need specialized treatment or observation. The birth is planned to take place through the natural birth canal. If the degree of prolapse is 2 or higher, accompanied by regurgitation or deviations in the well-being of the expectant mother, then the patient is hospitalized in a specialized cardiology department for up to 12 weeks.
If the pregnancy is maintained, then the woman is subsequently hospitalized as planned at the time of maximum hemodynamic changes: 18-20 weeks, 28-32 weeks. 2-3 weeks before birth, planned prenatal hospitalization is carried out. For regurgitation of grade 2 or higher, delivery by cesarean section is usually recommended.
Treatment
Therapeutic measures also require the joint attention of cardiologists and obstetricians. Patients should visit the hospital 3 times: 8-12 weeks, 28-32 weeks, and 3 weeks before the planned birth. Medical care in such cases comes down to the correct regimen, diet, psychoprophylactic preparation for childbirth, oxygen therapy, and drug treatment. The diet should be easily digestible and fortified. Oxygen saturation should be carried out using oxygen cocktails or oxygen barotherapy.
Drug treatment is aimed at treating and preventing the underlying disease, preventing cardiac complications, and treating circulatory failure. To prevent exacerbation of rheumatism, bicillin-1 or -5 is used together with acetylsalicylic acid up to 14 weeks, from 20 to 32 weeks of pregnancy. For compensated heart failure, it is recommended to use adonis infusion, vitamins B and C. The main medications are diuretics and cardiac glycosides.
Pregnant women with MVP complicated by pulmonary edema need emergency treatment. In this case, treatment is carried out with pipolfen, seduxen, promedol, strophanthin. Emergency assistance is provided for rhythm disturbances. Verapamil is used to suppress paroxysms.
Features of treatment for pregnant women
Cardiac glycosides
Hemodynamically insignificant grade 1 prolapse does not require treatment. All patients, without exception, are recommended to have a work-rest regime, prevention of placental insufficiency, a rational balanced diet, be sure to avoid smoking and drinking alcohol, and not to consume salt and plenty of fluids.
According to indications, a cardiologist can prescribe magnesium supplements, sedatives, selective b-blockers, calcium antagonists, and vasodilators to a woman. For severe mitral regurgitation, diuretics and cardiac glycosides are indicated. Prophylaxis of thromboembolism with indirect anticoagulants is mandatory. Treatment is prescribed by an experienced cardiologist; self-medication is not allowed.