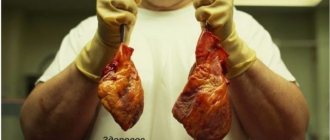
An acute condition of coronary heart disease, accompanied by necrosis of one or more sections of the heart muscle caused by an acute violation of the coronary blood supply, is diagnosed as myocardial infarction.
The disease affects men more often than women and older people. However, in the modern world, myocardial infarction is increasingly observed in young able-bodied people and middle-aged people.
Considering that pathological changes in the heart muscle lead to death in about a third of patients, it is necessary for every person to know the symptoms and stages of myocardial infarction.
Disease classification parameters
So, depending on the depth of necrotic damage, the disease can be:
- subendocardial, in which necrotic changes affect areas near the inner wall of the heart (endocardium);
- subepicardial with tissue necrosis in the area of the outer layer of the heart muscle (epicardium);
- intramural, the localization of which is observed directly in the heart muscle, affecting most of its thickness;
- transmural with changes throughout the thickness of the heart wall.
The size of the lesions allows the disease to be classified into large-focal and small-focal forms. The latter proceeds more mildly and, with timely treatment, does not lead to negative consequences.
It is worth noting that only 20% of patients are affected by the small-focal type of the disease, but it is possible that it will develop into a large-focal form.
When a heart attack is diagnosed for the first time in a patient’s life, it is characterized as primary. If the disease is detected a second time within two months after the first appearance, it is recurrent. The occurrence of pathological changes two months after the initial one is classified as repeated.
It is necessary to distinguish myocardial infarction from other infarction conditions (urate and lacunar infarction).
Regardless of the classification, the disease goes through certain stages with their inherent symptoms and changes in the cardiogram.
Regime and inpatient stage of rehabilitation of patients with myocardial infarction
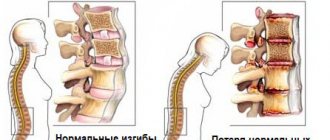
Previously, complete immobilization was recommended for 3 weeks, followed by less strict bed rest, and then gradual, careful activation for 6-8 weeks. However, it has been shown that prolonged bed rest leads to a decrease in the efficiency of the cardiovascular system, muscle weakness, osteoporosis, intestinal paresis, constipation, hypostatic pneumonia, and thromboembolic complications.
Currently, the duration of inpatient treatment for uncomplicated myocardial infarction is on average about 3 weeks, for large-focal myocardial infarction, including transmural, without significant complications - on average 4-5 weeks; in complicated forms of myocardial infarction - more than 4-5 weeks, depending on the condition of the patients.
Pre-infarction state
The pre-infarction state (prodromal period) is characterized by cessation of nutrition to the myocardium. Occurs as a result of hypertensive crises, constant nervous fatigue, stressful situations, overdose of alcoholic beverages, hypothermia, heat stroke, smoking, constant overeating, etc.
The duration of the pre-infarction state can vary from several days to a month
Experts attribute this stage to unstable angina, characterized by the appearance of attacks or their intensification during physical exertion, increased emotional arousal, after eating or being in the cold.
The duration of painful attacks can reach 20 minutes. and as the disease develops, it becomes more frequent and more severe. Eliminated with nitroglycerin or go away on their own.
The atypical course of the pre-infarction state is characterized by the absence of pain. In this case, the patient is exposed to irritability, sleep disturbances, a feeling of weakness, dizziness, shortness of breath, and cyanosis. Diagnosis of this condition is only possible using an ECG.
It is possible that abdominal syndrome may occur with pain localized in the left side of the sternum or upper abdomen.
The occurrence of any of the above symptoms necessitates urgent consultation with a doctor, especially if a person has previously been diagnosed with coronary artery disease.
This stage is not yet a direct heart attack and, with timely treatment, may not progress to it.
Expert advice
When the first signs of a heart attack appear, measures should be taken immediately. I advise you to immediately call an ambulance, and while the doctor is on the way, provide the patient with complete rest, sit him down or put him in a position that will alleviate the condition as much as possible. Give Corvalol, Nitroglycerin, Aspirin, ventilate the room.
The most dangerous period is the most acute period, which is usually manifested by very severe pain, shortness of breath, and rhythm disturbances. The patient’s life depends on the speed and correctness of the actions of the person nearby. When calling a doctor, it is best to describe the symptoms so that a specialized team can arrive to take an ECG, give oxygen, and administer medications to limit the area of necrosis.
The following sources of information were used to prepare the material.
The most acute period
The acute (ischemic) phase is the period from the onset of ischemia to the first symptoms of necrotic lesion. Its duration varies from 30 minutes. up to 2 hours.
The most acute period requires urgent placement of the patient in the intensive care unit
In 92% of cases, clinical manifestations develop as a pain or angina type. The patient is subjected to intense burning retrosternal pain for half an hour, radiating to the arm, neck, and lower jaw. Combat syndrome is accompanied by excitement, fear of death, the appearance of cold and sticky sweat, and pale skin. Nitroglycerin does not help in this case.
A large area of pathological changes is characterized by signs of cardiogenic shock:
- marbled skin color;
- blue lips and limbs;
- difficulties in determining blood pressure and pulse.
In other cases, symptoms depend on the type of myocardial infarction:
We recommend reading: Laboratory diagnosis of myocardial infarction
- In the asthmatic form of the pathology, there is no pain in the chest. The patient is exposed to causeless shortness of breath, suffocation accompanied by wheezing, audible from a distance. When pulmonary edema occurs, foamy fluid is released from the mouth and nose.
- The abdominal type of the disease leads to vomiting, nausea, intestinal upset, bloating, increased blood pressure, and tachycardia. Symptoms are similar to other gastrointestinal diseases (pancreatitis, cholecystitis, perforated ulcer, appendicitis, intestinal obstruction) and require differential diagnosis.
- The arrhythmic form of the pathology is accompanied by disturbances in heart rhythm (arrhythmia), disturbances in human consciousness and frequent fainting.
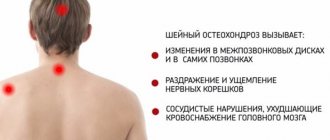
- The cerebral type of the disease resembles a stroke in its clinical manifestations. In this case, neurological symptoms dominate over the typical signs of heart attacks. Initially, the pathology provokes sharp headaches and a feeling of heaviness in the eyes. As necrotic changes develop, the patient becomes difficult to speak, has an unsteady gait and fainting states, and has impaired reflexes.
Very rarely, mainly in diabetics, there are no symptoms of myocardial infarction and its detection is possible only with the help of an ECG.
First aid
When the first symptoms of myocardial infarction occur, immediately calling an ambulance is mandatory, preferably a cardiology or resuscitation team. Attempts to independently eliminate the manifestations of the disease can cost the patient his life.
Before the arrival of specialists, it is necessary to provide the person with access to oxygen (open the windows), unbutton the collar of the shirt, remove the tie and other objects that have a compressive effect.
Place the patient on the bed, give a Nitroglycerin tablet, Aspirin (325 mg). For attacks of fear, sedatives will help, and for pain, painkillers (Analgin, non-steroidal anti-inflammatory drugs).
If vomiting occurs, the person's head should be turned to the side to prevent aspiration.
In case of cardiac arrest (lack of consciousness, breathing, pulse, blood pressure), resuscitation measures should be carried out immediately. A precordial blow has a good effect - a short strong blow to the sternum, which should be performed by a specialist.
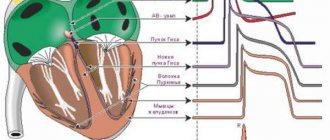
All stages of myocardial infarction can be seen on a cardiogram.
In extreme cases, they resort to indirect massage and artificial ventilation of the lungs, which must be carried out before the arrival of specialists
The patient is subject to urgent hospitalization, with placement in the intensive care unit.
The diagnosis is made on the basis of the clinical picture and electrocardiography data. It is also advisable to prescribe MRI, echocardiography, scintigraphy, coronary angiography, and analyzes of myocardial infarction markers.
The danger of myocardial infarction is the risk of death within 1 year after the disease (30%). Also, within 6 years after recovery, angina pectoris (25%), heart failure (20%), stroke (5%), and recurrent heart attack (20%) may occur.
To avoid myocardial infarction, it is important not only to lead a healthy lifestyle, but also to undergo electrocardiography annually, especially for persons predisposed to this pathology.
There is a simple test that even for people without medical education helps to quickly identify acute cerebrovascular accident in another person. It is called "FAST" or "Hand-Face-Speech".
Its essence:
- Ask the person who is in a strange state to smile. If he has a stroke, then one side of his face will noticeably “hang” relative to the other and asymmetry will appear.
- Ask him to raise both arms perpendicular to his body and hold them for 5 seconds. If the person is lying down, ask them to hold their arms at an angle of 45° C. If cerebral circulation is impaired, one arm falls.
- Ask them to say a simple phrase. If a stroke occurs, speech will be slurred, unintelligible, and unclear.
Acute period (necrotic stage)
Anginal pain disappears at the necrotic stage, which is its characteristic feature. However, pain persists with recurrent infarction and epistenocadial pericarditis.
The acute period of myocardial infarction (AMI) lasts about two days until the necrotic focus is completely demarcated. In case of a recurrent disease, this period can increase to 10 days or more.
In the patient:
- body temperature increases to 39ºС, which is accompanied by a feverish state;
- the conductivity and rhythm of the heart muscle is disrupted;
- blood pressure decreases.
The acute stage is considered the most dangerous, because contributes to severe disturbances of blood circulation in the vessels of the brain, arrhythmias, heart ruptures and thromboembolism.
Subacute stage
In the subacute period, deeply damaged muscle fibers move into the zone of necrosis. In this case, the rest of the damaged muscle fibers are restored with their transition to the ischemic zone, which leads to the expansion of the latter and the surrounding of tissues that have undergone acute necrosis.
Subsequently, the muscle fibers located in the area of ischemia are restored, and therefore it becomes smaller.
The subacute stage of myocardial infarction lasts 1–3 months with gradual stabilization of the patient’s condition. Happens:
- cessation of pain in the chest;
- reducing the frequency and severity of cardiac arrhythmias;
- restoration of cardiac conductivity;
- complete disappearance or reduction of shortness of breath, signs of blood stagnation in the lungs in the absence of a cardiac aneurysm;
- increased sonority of heart sounds without their complete restoration;
- gradual increase in blood pressure in most cases;
- disappearance of signs of resorption-necrotic syndrome (fever, leukocytosis).
The persistence of elevated temperature and leukocytosis indicates a recurrent infarction or complications (post-infarction syndrome, thromboendocarditis).
Angina attacks at this stage occur as a result of an incomplete heart attack or multivascular lesions and increase the risk of repeated and recurrent heart attacks.
At this stage, the development of complications cannot be ruled out: pneumonia, pericarditis, pleurisy, pain in the joints, skin rashes (such as urticaria).
Clinical picture of repeated
1) high frequency among men;
2) the beginning of the acute period with collapse and dynamic cerebrovascular accident;
3) frequent development of thromboembolic complications and hypostatic pneumonia;
4) the predominance of heart failure, cardiogenic shock, and cardiac arrhythmias in the clinical picture;
5) protracted or recurrent course, long-term persistence of increased rates of resorption-necrotic syndrome.
ECG symptoms of repeated MI can be clear and characteristic, while signs of previous scar changes in the myocardium remain, but sometimes ECG signs of repeated infarction are unconvincing; in this case, a special role in diagnosis belongs to dynamic analysis of the ECG, echocardiography, and determination of biomarkers of necrosis in the blood myocardium.
Post-infarction period (scarring stage)
The scarring stage is the final stage of myocardial infarction. The end of the disease is characterized by the formation of a scar in the area of necrosis, which is clearly visible on the ECG, with the development of compensatory hypertrophy in unaffected areas.
Extensive affected areas make full compensation impossible, which leads to the persistence of symptoms of heart failure, and in some cases to its increase. The development of recurrent myocardial infarction cannot be ruled out.
In the absence of complications, the patient's condition returns to normal. His motor capabilities increase, his heart rhythm improves, and no abnormalities are detected in laboratory tests.
The post-infarction state lasts approximately six months and may be accompanied by:
- low-grade fever;
- mild but prolonged heart pain lasting about 30 minutes;
- feeling of general weakness;
- shortness of breath;
- pain in the joints or chest area.
Despite the fact that during this period the treatment takes place at home, the patient must follow all the doctor’s recommendations, give up bad habits, and limit physical activity.
Of particular importance is a balanced diet of fresh, chopped food, which helps strengthen the body and reduce stress on the heart. Experts recommend following diet No. 10 throughout the course of treatment.
Secondary prevention after myocardial infarction
Secondary prevention after myocardial infarction is aimed at preventing death, the development of recurrent myocardial infarction and chronic heart failure.
- indirect anticoagulants (warfarin, syncumar, etc.);
- aspirin;
- β-blockers;
- calcium antagonists (verapamil, diltiazem);
- ACE inhibitors (in patients with symptoms of heart failure in the acute period of MI);
- amiodarone (cordarone) (in patients with dangerous ventricular arrhythmias);
- hypocholesterolemic drugs from the Vastatin group
The use of indirect anticoagulants for secondary prevention after myocardial infarction
Indirect anticoagulants are very effective for secondary prevention after MI. However, due to the great danger of hemorrhages, these drugs in patients who have had an MI are prescribed only if there is a high risk of developing systemic thromboembolism (atrial fibrillation, congestive heart failure, parietal thrombosis of the left ventricle). When the risk of developing systemic thromboembolism is reduced, indirect anticoagulants are discontinued and aspirin is prescribed
Use of aspirin for secondary prevention after myocardial infarction
Aspirin for secondary prevention after MI is less effective than indirect anticoagulants (reduces mortality by 15%, the rate of recurrent MI by 31%), but it causes side effects much less often. Aspirin is prescribed at a dose of 160-325 mg/day, but the preventive effect is achieved when using a dose of 75-150 mg/day.
The use of β-blockers for secondary prevention after myocardial infarction
It is advisable to prescribe β-blockers to all patients who have had an MI, in the absence of contraindications. They should be combined with cholesterol-lowering drugs from the Vastatin group (simvastatin, pravastatin, lovastatin, fluvastatin, etc.). These drugs neutralize the negative effect of β-blockers on lipid metabolism and, in addition, significantly reduce mortality and the incidence of recurrent myocardial infarction.
In the presence of life-threatening ventricular arrhythmias refractory to treatment with β-blockers, amiodarone (cordarone) is used.
Use of sulodexide for secondary prevention after myocardial infarction
D.M. Aronov et al. (1995) suggest using the low molecular weight heparin drug sulodexide (Wessel) for secondary prevention after myocardial infarction, as well as for unstable angina.
Sulodexide is not inferior in antithrombotic effect to heparin, but in comparison with it it very rarely causes hemorrhagic complications and thrombocytopenia. The drug is initially prescribed at 600 units intramuscularly 2 times a day for 15 days; then 500 units orally (in capsules) 2 times a day for three months or more.
The use of ACE inhibitors for secondary prevention after myocardial infarction
1) in patients with signs of left ventricular dysfunction (symptoms of heart failure or decreased ejection fraction on echocardiographic examination) that appear at any time after the development of acute myocardial infarction, it is necessary to immediately begin long-term therapy with ACE inhibitors in the absence of contraindications;
2) treatment with ACE inhibitors can be started on the first day of acute myocardial infarction after assessing the clinical condition and hemodynamic parameters (a decrease in diastolic blood pressure below 100 mm Hg is a contraindication) and prescribing other conventional drugs (thrombolytics, aspirin, β-blockers);
3) treatment with ACE inhibitors should not be delayed, given the high mortality rate in the acute phase of MI;
4) ACE inhibitors prescribed in the acute period of MI can be discontinued after 4-6 weeks in the absence of left ventricular dysfunction;
5) the dose of the ACE inhibitor should be selected individually.
ACE inhibitors reduce the incidence of recurrent myocardial infarction, mortality from myocardial infarction and prevent the development or reduce the severity of circulatory failure. The positive effect of ACE inhibitors is explained by the prevention of progressive dilatation of the left ventricle and a decrease in the activity of the renin-angiotensin system.
The use of cholesterol-lowering drugs for secondary prevention after myocardial infarction
1) statins are effective means of secondary prevention in patients with clinical manifestations of coronary artery disease;
2) long-term statin therapy increases survival not only of patients with angina or previous MI, but also of patients with hypercholesterolemia without clinical manifestations of coronary artery disease.