Biochemical blood test for calcium is a clinical test that determines the concentration of total calcium in the blood serum.
The concept of total calcium includes:
- Ionized calcium makes up 50% of all calcium in the blood.
- Calcium bound to proteins (mainly albumin) – 40%.
- Calcium, which is part of anionic complexes (associated with lactate, citrate, bicarbonate, phosphates) – 10%.
For the normal functioning of the body, it is necessary that the calcium level be within the reference values, since it takes part in many vital processes:
- Muscle contraction.
- The work of the endocrine glands.
- Blood coagulation, cell membrane permeability.
- Construction of the skeletal system and teeth.
- Transmission of nerve impulses, work of the nervous system.
- Enzyme activity, iron metabolism in the body.
- Normal heart rhythm, functioning of the cardiovascular system.
Blood test for ionized calcium
Ionized calcium is calcium that is not bound to any substances and circulates freely in the blood. It is the active form of calcium that is involved in all physiological processes. A blood test for ionized calcium will assess calcium metabolism in the body. This test must be given to patients in the following cases:
- Treatment after resuscitation, surgery, major trauma, burns.
- Diagnosis of cancer, hyperfunction of the parathyroid gland.
- Carrying out a hemodialysis procedure.
- Taking the following medications: bicarbonates, heparin, magnesium, calcium supplements.
A blood test for ionized calcium is carried out in conjunction with determining the level of total calcium and blood pH. The value of ionized calcium is inversely related to blood pH: the level of ionized calcium increases by 1.5 - 2.5% for each decrease in pH by 0.1 unit.
Place of calcium in the human body
In the human body, calcium is the main component of bone tissue, as well as the most important biogenic element that performs structural, metabolic and regulatory functions.
For reference. Calcium is the most abundant inorganic element in the human body. The body of an adult man contains, on average, about 1.5 kilograms of Ca, a woman - about 1 kilogram.
However, of this total amount, only 1% of Ca is found in the blood; the remaining 99% is found in bone tissue in the form of poorly soluble hydroxyapatite crystals. The crystals also contain phosphorus oxide. Normally, the body of an adult contains about 600 grams of this microelement, with 85% of phosphorus contained in the bones, along with calcium.
Hydroxyapatite crystals and collagen serve as the main structural components of bone tissue. Ca and P make up about 65% of the total bone mass. Therefore, it is impossible to overestimate the role of these microelements in the body.
Calcium in the blood
The calcium content in bones and blood may change. Normally, a small percentage of bone calcium is able to exchange with blood calcium. Thanks to this process, excess trace elements can be removed from the blood, or, conversely, the process of reverse transport of Ca from the bones into the blood is ensured (in cases where its content in the serum is reduced).
All calcium in the blood can be divided into three types:
- ionized Ca;
- calcium, in albumin-bound form;
- located in the composition of anionic complexes (bicarbonates, phosphates).
Normally, an adult has approximately 350 milligrams of calcium circulating in the blood, which is 8.7 mmol. The microelement concentration in mmol/l is 2.5.
About 45% of this amount is associated with albumin, up to five percent is included in anionic complexes. The rest is ionized, that is, free (Ca2+).
Important. It is ionized calcium that is physiologically active.
It is a vital part of the total amount of a microelement in the body, contained in all cells (nmol/L is used to measure the concentration in cells). It is important to remember that the calcium concentration in cells directly depends on the calcium concentration in the extracellular fluid.
Attention. It must be taken into account that the amount of ionized Ca does not depend on the level of albumin, therefore, for patients with low protein in the blood, the level of ionized calcium in the diagnosis of primary hyperparathyroidism is more reliable.
Functions of Ca in the body
Ionized calcium in the blood acts as a cofactor necessary for the full functioning of enzymes involved in maintaining the hemostasis system (that is, calcium participates in the process of blood coagulation, facilitating the transition of prothrombin to thrombin). In addition, ionized Ca serves as the main source of calcium, necessary for normal contractions of skeletal muscles and myocardium, conduction of nerve impulses, etc.
Calcium in the blood is involved in the regulation of the nervous system, inhibits the release of histamine, and normalizes sleep (calcium deficiency often leads to insomnia).
A normal level of calcium in the blood ensures the full functioning of many hormones.
Also, calcium, phosphorus and collagen are the main structural components of bone tissue (bones and teeth). Ca is actively involved in the process of mineralization of teeth and bone formation.
Calcium is able to accumulate in places of tissue damage, reduce the permeability of cell membranes, regulate the functioning of the ion pump, maintain the acid-base balance of the blood, and participate in iron metabolism.
Indications for analysis
Indications for a biochemical blood test for calcium:
- Signs of hypercalcemia and hypocalcemia.
- Malignant neoplasms (breast cancer, lung cancer).
- Peptic ulcer of the stomach and duodenum.
- Decreased albumin concentration.
- Preparation for surgery.
- Muscle hypotension.
- Hyperthyroidism.
- Kidney diseases, urolithiasis.
- Bone pain.
- Cardiovascular pathology (impaired vascular tone, arrhythmia).
- Polyuria.
- Paresthesia.
- Convulsive syndrome.
- Diagnosis and screening of osteoporosis.
Symptoms of hypercalcemia: adynamia (immobility), asthenia, increased reflexes, impaired consciousness, disorientation, weakness, headache, vomiting, acute renal failure, heart failure, tachycardia, extrasystole, vascular calcification.
Symptoms of hypocalcemia: migraine-like headaches; dizziness, caries, osteoporosis, nail destruction, hair loss, dry skin, increased reflexes leading to tetanic convulsions, weakness, blood clotting disorders (extended clotting time), angina pectoris, tachycardia (increased heart rate - pulse).
Hypercalcemia is a pathological condition that occurs when the body becomes ill. Physiological hypercalcemia occurs - after eating and in newborns after the fourth day of life. Hypocalcemia is diagnosed much more often than excess calcium in the body.
Calcium level in blood
The rules for preparing for analysis are general. Blood is drawn on an empty stomach (fasting for at least 14 hours). Smoking and drinking alcohol are excluded (at least 24 hours). Also, it is necessary to avoid physical and mental stress.
Consumption of milk, coffee, nuts, etc. may lead to inflated results.
Venous blood is used for diagnosis. The units of measurement are mol/l.
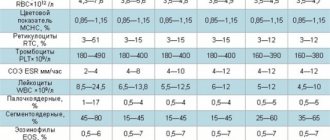
In children under ten days of life, the normal level of calcium in the blood ranges from 1.9 to 2.6.
From ten days to two years the norm is from 2.25 to 2.75.
From two to 12 years – from 2.2 to 2.7.
From twelve to sixty years of age, the normal level of calcium in the blood ranges from 2.1 to 2.55.
From 60 to 90 years old – from 2.2 to 2.55.
In patients over 90 years old – from 2.05 to 2.4.
Causes of high calcium
Ca may increase with:
- primary hyperparathyroidism (hyperplasia, carcinoma or other lesions of the parathyroid glands);
- oncological neoplasms (primary bone damage, spread of metastases, carcinoma affecting the kidneys, ovaries, uterus, thyroid gland);
- immobilization hypercalcemia (immobilization of a limb after injury, etc.);
- thyrotoxicosis;
- vitamin D hypervitaminosis;
- excessive intake of calcium supplements;
- acute renal failure and long-term kidney diseases;
- hereditary hypocalciuric hypercalcemia;
- blood diseases (myeloma, leukemia, etc.);
- adrenal insufficiency;
- Williams syndrome;
- severe overdose of diuretics (thiazide).
When the level is low
Such changes in the analysis may be due to:
- primary (hereditary) and secondary (after surgery, autoimmune damage to the glands) hypoparathyroidism,
- hypoparathyroidism in newborns (associated with maternal hypoparathyroidism), hypomagnesemia (magnesium deficiency),
- deficiency of tissue receptors for parathyroid hormone (hereditary disease),
- chronic renal or liver failure,
- vitamin D hypovitaminosis,
- albumin deficiency (nephrotic syndrome, liver cirrhosis),
- treatment with cytostatics,
- acute alkalosis.
Symptoms of calcium metabolism disorders
When calcium levels in the blood increase, the following appears:
- severe weakness,
- rapid physical and emotional exhaustion,
- patients become depressed and drowsy,
- loss of appetite,
- frequent urination,
- constipation,
- pronounced thirst,
- frequent vomiting,
- extrasystole,
- violation of orientation in space.
Hypercalcemia can lead to:
- urolithiasis and cholelithiasis,
- arterial hypertension,
- calcification of blood vessels and heart valves,
- keratitis,
- cataracts,
- gastroesophageal reflux,
- peptic ulcer.
A decrease in calcium in the blood manifests itself:
- spasmodic pain in muscles and abdomen,
- muscle spasms,
- tremor of the limbs,
- tetanic convulsions (spasmophilia),
- numbness of hands,
- baldness,
- brittleness and layering of nails,
- severe dry skin,
- insomnia,
- memory loss,
- clotting disorder,
- frequent allergies,
- osteoporosis,
- lower back pain,
- coronary heart disease,
- frequent fractures.
Important. In pregnant women, low calcium leads to impaired fetal development. In women who are breastfeeding, poor lactation may also be due to calcium deficiency.
However, it is important to understand that not all pregnant women have calcium deficiency, so the question of whether to drink calcium during pregnancy should be decided individually, based on calcium levels in the blood.
If a woman follows a balanced diet (sufficient consumption of dairy products, greens, etc.), has no underlying diseases leading to hypocalcemia, and also has normal test results, additional intake of calcium supplements is not required.
For reference. In young children, calcium deficiency in the blood is usually caused by vitamin D deficiency (rickets).
As a result, calcium absorption in the intestine is impaired. The disease is manifested by sweating, baldness of the back of the head, developmental delays (physical and mental), late teething, and bone deformities.
Calcium deficiency is also observed in women during menopause and the elderly.
What to do if symptoms of hyper- or hypocalcemia appear
Considering that changes in the level of calcium in the blood can be due to many reasons, the appointment of complex treatment
carried out after a final diagnosis has been established.
In case of iatrogenic deficiencies, as well as if hypocalcemia is associated with hormonal imbalance during menopause or due to the patient’s age, drugs containing Ca are prescribed (Calcium D3 Nycomed, Vitrum Calcium).
Also, balanced multivitamin complexes containing microelements can be prescribed (Vitrum Centuri - for patients over fifty years of age, Menopace - for women in the menopausal period).
Taking medications must be agreed with your doctor. It is important to understand that uncontrolled use of calcium supplements can lead to hypercalcemia and its attendant complications.
How to prepare for a calcium blood test
In order for a calcium blood test to give an accurate result, you need to undergo simple preparation for the procedure:
- On the eve of the study, you should not drink alcohol, fried or fatty foods.
- The day before blood sampling, it is advisable to avoid heavy physical and emotional stress.
- Blood is donated on an empty stomach, 8-10 hours after the last meal. It is recommended to drink only still water.
- It is not recommended to donate blood immediately after fluorography, rectal examination, radiography, ultrasound examination or physiotherapeutic procedures.
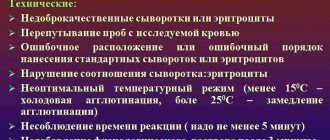
Factors that may distort the analysis result
Taking medications can affect the accuracy of the calcium blood test result. It is advisable to stop taking any medications 1-2 weeks before taking blood for testing. If it is impossible to discontinue the drug, then in the referral for a biochemical blood test for calcium it is necessary to indicate which medications the patient is taking and in what doses. The following medications affect calcium levels in the blood.
Increase calcium levels: vitamin A, vitamin D, testolactone, tamoxifen, parathyroid hormone, progesterone, lithium, isotretinoin, ergocalciferol, dihydrotachysterol, danazol, calusterone, Ca salts, androgens, regular use of diuretics.
Reduce calcium levels: sulfates, oxalates, fluorites, tetracycline, plicamycin, phenytoin, methicillin, magnesium salts, isoniazid, insulin, indapamide, glucose, glucagon, gastrin, fluorites, estrogens, ergocalciferol, corticosteroids, carboplatin, carbenoxolone, carbamazepine, calcitonin, asparaginase , aminoglycosides, alprostadil, albuterol.
Medicines that distort test results
Calcium in the blood increases when treated with drugs containing calcium salts, parathyroid hormone and progesterone, androgens, as well as vitamins A and D, lithium, Tamoxifen, Testolactone, Tamoxifen, Isotretinoin, Ergocalciferol, Dihydrotahysterol , Danazol, Calusterone, diuretics in large quantities.
Ca decreases during treatment with sulfates, corticosteroids, Tetracycline, Methicillin, Insulin, Carboplatin, Plicamycin, Indapamide, Phenytonin, Carbenoxolone, Isoniazid, Calcitonin, Carbamazepine ", "Albuterol", "Alprostadil", as well as drugs with Mg salts, estrogens, glucose, glucagon, gastrin, ergocalciferol (a type of vitamin D) in large quantities, asparaginase, aminoglycosides, calcium oxalates, fluorite (D-Fluoretten 500 IE) .
Norms
The results of the study must be interpreted by a specialist with appropriate qualifications. Only a doctor will be able to properly assess the patient’s condition, the deviation from the normal blood test for calcium and make the correct diagnosis. And accordingly, prescribe adequate treatment in a timely manner.
Reference values for a blood test for total calcium:
- children under 1 year – 2.1-2.7 mmol/l;
- children from 1 to 14 years old – 2.2-2.7 mmol/l;
- children over 14 years old – adults – 2.2-2.65 mmol/l.
What tests need to be taken
In order to determine or clarify the cause of osteoporosis, a general clinical examination is prescribed.
General blood analysis
In secondary osteoporosis due to lifestyle disturbances or hormonal dysfunction, a moderately elevated level of leukocytes can be detected. If bone loss is an age-related process or occurs in women after multiple pregnancies (primary process), then no specific changes are found.
For calcium
Maintains the strength of bones and teeth, ensures the conduction of impulses in muscle tissue, and blood clotting. Its consumption increases with smoking, drinking coffee, and stress. It is not absorbed from food if there is a lack of vitamin D. It is increased in the blood with increased activity of the parathyroid glands, bone metastases, and a long period of immobility. Decreased with protein deficiency, renal and liver failure. Average values for adults are 2.1-2.5 mmol/l.
Biochemical
In addition to calcium determination, the following tests are recommended:
- creatinine to assess kidney function;
- total protein, the activity of calcium ions depends on it, since half of them circulate in the blood as part of protein complexes;
- alkaline phosphatase, the activity of this enzyme increases during bone tissue breakdown, Paget's and Gaucher's diseases, menopause and pregnancy;
- ALT and AST to exclude liver failure;
- C-reactive protein, when elevated, indicates the presence of an inflammatory process.
Blood hormones
To exclude dysfunction of the endocrine system, the level of the following hormones is examined:
- thyroid-stimulating and thyroxine, in thyrotoxicosis, when bone density is impaired, the first is lower and the second is higher than normal;
- ACTH (corticotropin) and cortisol can help in diagnosing Cushing's syndrome and disease, which occur with disorders of mineral metabolism;
- sex hormone binding globulin; the risk of fractures increases many times if estradiol is below normal and this protein is elevated.
Analysis of urine
To clarify calcium metabolism disorders, its level must be examined not only in the blood, but also in the urine. Increased excretion from the body reflects high concentrations in the blood serum, accelerated destruction of bone tissue, and hyperfunction of the parathyroid glands. A general urine test helps determine existing kidney problems, which can change the reliability of biochemical tests.
Increased levels of calcium oxalate in urine
Increased values
Hypercalcemia indicates the following diseases:
- Acute renal failure.
- Sarcoidosis and other granulomatous diseases.
- Iatrogenic hypercalcemia.
- Hereditary hypocalciuric hypercalcemia.
- Williams syndrome (idiopathic hypercalcemia of newborns).
- Hypervitaminosis D.
- Milk-alkali syndrome.
- Hemoblastoses (leukemia, lymphoma, myeloma).
- Adrenal insufficiency.
- Immobilization hypercalcemia (for therapeutic purposes for injuries, congenital hip dislocation, Paget's disease, spinal tuberculosis).
- Malignant tumors
- Primary hyperparathyroidism (adenoma, hyperplasia or carcinoma of the parathyroid glands).
- Thyrotoxicosis.
Reduced values
Hypocalcemia is observed in the following diseases:
- Acute pancreatitis with pancreatic necrosis.
- Chronic renal failure.
- Liver failure.
- Hypovitaminosis D with rickets in children and osteomalacia in adults (as a result of nutritional disorders, reduced insolation, malabsorption).
- Hypoalbuminemia in nephrotic syndrome and liver pathology.
- Hypomagnesemia.
- Pseudohypoparathyroidism (hereditary disease).
- Primary hypoparathyroidism (X-linked, hereditary, DiGeorge syndrome).
- Secondary hypoparathyroidism (autoimmune, as a result of surgery).
Diseases associated with hypocalcemia
If there is not enough Ca in the blood, then a person may be sick:
- chronic renal and liver failure;
- acute pancreatitis with the presence of pancreatic necrosis;
- osteomalacia with malabsorption, malnutrition, decreased insolation (in adults);
- hypovitaminosis D with rickets (in children);
- hypoalbuminemia due to liver disease and nephrotic syndrome;
- hypoparathyroidism primary (hereditary) or secondary (autoimmune, after surgery);
- hereditary pseudohypoparathyroidism;
- hypomagnesemia.
With calcium deficiency, the body initially removes it from its own reserves, so characteristic symptoms do not appear. When the bones lose their mass, the patient’s eyelids and corners of the mouth, wings of the nose begin to twitch, fingers and toes begin to go numb, nails break and become covered with grooves, and teeth decay. Children's growth slows down.