- Reasons for the development of pathology
- Symptoms
- Diagnostic methods
- Methods for treating arrhythmia in old age
- Types of arrhythmias that pose the greatest danger in old age
- Prevention methods
Arrhythmia in older people is the result of acquired pathologies of the cardiovascular system and age-related changes in myocardial tissue. Most often, atrial fibrillation develops in old age. At the age of 65-85 years, pathology occurs in 70% of cases and increases the risk of stroke and death.
Reasons for the development of pathology
The development of arrhythmia, or atrial fibrillation, in old age is caused by cardiovascular disorders, which can be a consequence of increased physical and emotional stress, poor nutrition, and a sedentary lifestyle in youth. The older a person is, the more unfavorable conditions affect his health.
Changes in heart rate in older people are associated not only with dysfunctions of the cardiovascular system, but also with pathologies of other internal organs.
The main reasons for the development of atrial fibrillation in elderly people include the following:
- atherosclerotic disorders of blood vessels;
- hypertension;
- decreased conduction of impulses along the atrioventricular pathways;
- cardiac ischemia;
- heart defects;
- pericarditis of various forms;
- heart failure;
- cardiomyopathy;
- age-related changes in the myocardium;
- damage to the heart muscle of a rheumatic nature;
- degenerative processes of the sinus node;
- violation of coronary blood supply;
- heart attacks.
Factors not associated with dysfunction of the heart muscle and causing arrhythmia in old age are:
- thyrotoxicosis;
- vegetative-vascular dystonia;
- alcohol abuse;
- hormonal disorders;
- severe bacterial and viral infections;
- intoxication of the body with poisons and various poisonous gases;
- prolonged use or overdose of diuretics, antiarrhythmic drugs;
- increased mental stress;
- obstructive pulmonary diseases;
- obesity;
- diabetes.
In 30% of cases, arrhythmia in older people is caused by a hereditary factor. Sometimes the cause of such a pathology cannot be established; in this case, we are talking about idiopathic arrhythmia.
Lifestyle correction
The diet when diagnosed with atrial fibrillation must be completely revised, eliminating foods that contribute to the deposition of excess bad cholesterol. The menu should include citrus fruits, onions and garlic, nuts, honey, cranberries and dried fruits. Fermented milk products and sprouted wheat grains will be beneficial. Chocolate, coffee, alcoholic beverages, fatty meats, flour dishes, and canned food are prohibited.
Treatment of atrial fibrillation in older people determines the presence of vascular atherosclerosis, and in young people it is associated with hormonal changes in the body. The basic rules of treatment after 60 years include constant use of medications under the supervision of a doctor.
The feeling of a missed contraction, periodic disruptions in heart rhythm require qualified medical assistance. Do not self-medicate; only timely started therapy will prevent the occurrence of various complications.
Symptoms
At the initial stages of the pathology, the clinical picture is not clearly expressed. In this case, the deviation can only be detected during diagnostic measures. As the disorder progresses, symptoms begin to appear.
The main signs that indicate atrial fibrillation in older people include the following:
- general weakness;
- frequent dizziness;
- nausea;
- pain, discomfort in the chest area;
- pre-fainting states;
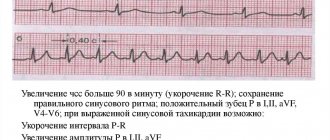
- rapid pulse (more than 100 beats per minute);
- increased heart rate;
- feeling of lack of air;
- tingling in the heart area;
- sharp, chaotic “twitching” of the heart muscle;
- severe sweating;
- feeling of coldness in the lower and upper extremities;
- attacks of panic, fear;
- increase in the amount of urine excreted.
Attacks of arrhythmia in older people are called paroxysms. Depending on the frequency and duration of symptoms, attacks are divided into the following forms:
- paroxysmal: manifestations of arrhythmia can persist from several hours to several days;
- persistent: in this case, signs of deviation are temporary and stable, persisting for 7 days;
- long-term persistent: attacks of arrhythmia appear for a year or more;
- permanent form: symptoms in this case are associated with the presence of persistent causes - for example, heart defects or endocrine disorders.
The chronic type of the disease is expressed in disordered heart sounds, which may not even be felt by the patient.
What to do during an attack?
Attacks of suffocation and other symptoms are a reason to immediately call an ambulance
If you suspect an attack of cardiac arrhythmia in the elderly, you must call an ambulance as soon as possible. After this, the following steps are taken:
- Ventilation of the room. If the patient has shortness of breath, it is advisable to give him a semi-sitting position by unbuttoning the top buttons of the shirt.
- Measurement of blood pressure and pulse rate.
- To prevent an attack, you can alternately change your body position: from sitting to lying and vice versa.
- Gentle pressure on the eyelids can help reduce the patient's tension.
Diagnostic methods
Pathology in old age can be identified using the following diagnostic measures:
- taking anamnesis;
- pulse counting;
- listening to the heart;
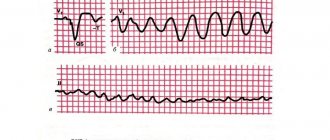
- electrocardiogram;
- Ultrasound of the heart muscle with Doppler sonography;
- chest x-ray;
- tests to determine the level of thyroid hormones;
- MRI or CT;
- Holter monitoring.
After establishing the diagnosis and the cause that causes arrhythmia paroxysms, the specialist selects the optimal course of treatment.
Methods for treating arrhythmia in old age
Depending on the extent of the pathological process, medical or surgical treatment may be chosen.
Drug therapy
Conservative treatment consists of the patient taking the following medications:
- drugs for stabilizing heart rhythm (Cordarone, Ritmonorm, Novocainamide): drugs in this group can cause bradycardia, so when taking them it is important to constantly monitor blood pressure;
- anticoagulants (Warfarin, Aspirin, Finilin, Sinkumar): the need to take them is due to the fact that impaired atrial contraction impairs blood circulation, which increases the risk of blood clots forming in the vessels;
- beta blockers and calcium antagonists (Sotalol, Metoprolol, Diltiazem).
The dosage and duration of the course are determined by the doctor individually. If the patient has a chronic course of the pathology, he should take drugs against arrhythmia on an ongoing basis.
Electrical cardioversion
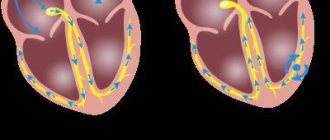
If it is impossible to restore sinus rhythm (correct conduction of the impulse through the conduction system of the heart muscle) with the help of medications, they resort to the method of electrical cardioversion. This is a procedure that involves delivering a shock of electricity through the heart by placing electrodes. It is performed under general anesthesia.
The likely and most common complication after electrical cardioversion in adults is thrombus formation. Also, if the electrodes are placed incorrectly, there is a risk of skin burns.
Elderly people suffering from arrhythmia are rarely prescribed electrical cardioversion, since maintaining sinus rhythm for a long time in this case is almost impossible. This procedure is an emergency or last resort treatment measure.
Surgical intervention
Surgery for atrial fibrillation in elderly people is indicated if there are no results from conservative therapy.
Depending on the general indicators, the following operations can be performed:
- Cauterization (radiofrequency catheter ablation). Specialists identify the area of the myocardium that is the source of the arrhythmia and cauterize it. The guidewire is introduced to the heart muscle through the femoral artery.
- Ablation followed by installation of a pacemaker. This manipulation is performed if the sinus rhythm has been disturbed and attacks of arrhythmia are repeated frequently. Before installing a pacemaker, an atrioventricular node block is caused.
- Defibrillator installation. The device is implanted in the upper chest. It is used to quickly relieve the next paroxysm.
- Operation Labyrinth. This type of intervention is performed on an open heart. Incisions are made in the atria that resemble a labyrinth. This allows you to change the direction of electrical impulses and normalize the functioning of the organ.
Lifestyle
For full treatment, correction of the patient’s general regimen is required. The following rules must be followed:
- completely stop drinking alcohol and smoking;
- do not try to stop paroxysm on your own using folk remedies or medicinal methods without first undergoing the necessary diagnostic measures;
- prevent the likelihood of nervous shocks, avoid stressful situations;
- exclude from the diet foods that contribute to the deposition of cholesterol plaques in blood vessels (fatty, flour), give up acids, salt, foods high in easily digestible carbohydrates, sweets (see nutrition for arrhythmia);
- introduce feasible physical activity into your usual routine;
- observe the work and rest schedule;
- An elderly person suffering from atrial fibrillation should sleep for at least 8 hours.
At home, following the instructions of your doctor, you can supplement the course by taking a decoction of viburnum berries and drinking a nut-honey mixture.
Medicines for atrial fibrillation
The course of extrasystole is determined by the nature of the underlying disease and the degree of heart damage. If the patient has no signs of myocardial damage and the left ventricle fully performs the contractile function, then extrasystole does not pose a danger.
If the patient has organic myocardial damage, the doctor may consider extrasystole as an additional prognostically unfavorable sign.
For this form of arrhythmia, drug treatment usually begins with beta blockers. The effectiveness of amiodarone and sotalol will be evaluated in the future. Therapy with sedatives is also possible. Sodium channel blockers are used only for very frequent extrasystoles, in the absence of effect from treatment with beta blockers, amidoron and sotalol.
In the case of paroxysmal supraventricular tachycardia, antiarrhythmic drugs are prescribed if there is no effect from vagal techniques (massage of the carotid artery, immersing the face in cold water, etc.). The most effective medications for this form of cardiac arrhythmia are verapamil and adenosine.
In the paroxysmal form of the disease, sinus rhythm spontaneously recovers in 50% of patients during the first 24 hours, but it is impossible to predict whether this will happen in the first hours. Usually, when seeking medical help early, specialists try to restore the rhythm with the help of antiarrhythmic drugs.
However, if more than 2 days have passed since the onset of the attack, then returning to the normal rhythm poses a certain danger, since the risk of thromboembolism is high. In cases where atrial fibrillation lasts more than 2 days, the patient is prescribed indirect anticoagulants (phenylin or warfarin).
In the treatment of persistent atrial fibrillation, restoration of normal rhythm is achieved by administering quinidine. Other medications for cardiac arrhythmia (potassium salts, beta blockers, etc.) are used to maintain the restored normal rhythm. According to various data, quinidine is effective in 40-80% of cases.
However, it has a number of contraindications (diseases of the heart muscle, conduction disorders, angina pectoris, patient age over 60 years). Treatment with quinidine usually requires prior preparation.
The patient may be prescribed digitalis preparations, which will reduce the symptoms of circulatory failure. Potassium salts are prescribed to normalize electrolytic metabolism in the myocardium.
Types of arrhythmias that pose the greatest danger in old age
There are several types of arrhythmias that pose a particular danger to elderly patients. These should include:
- arrhythmias causing severe disturbances of the central or peripheral circulation (ventricular fibrillation);
- arrhythmias that can cause the development of acute heart failure and cardiosclerotic changes (ventricular tachycardia, tachysystolic fibrillation or atrial flutter);
- arrhythmias, which are accompanied by attacks of angina or other manifestations of acute coronary insufficiency.
Atrial fibrillation is especially dangerous in old age, as it increases the risk of blood clots. Thrombosis often causes heart attacks and strokes, as well as pulmonary embolism. Such pathologies can cause cardiac arrest.
How to deal with cardiac arrhythmia in older people using cardioversion
The heart pacemaker is the area of the muscle that is responsible for transmitting impulses. It ensures automatic operation of the entire mechanism. Moreover, if there are deviations, they affect the appearance of fibrillation.
Cardioversion is a strong effect on the heart to correct sinus rhythm. That is, doctors force impulses so that they are transmitted synchronously, in the required order. There are two main methods of medical intervention:
- Medication – with the help of drugs.
- Defibrillator.
Indications for recovery
Typically this method is used in the following cases:
- when it is impossible to normalize the rhythm using classical methods, that is, using beta blockers;
- when atrial fibrillation and its symptoms persist even after drug treatment;
- when it is necessary to maintain the normal functioning of the pacemaker for a long period.
Interestingly, the readings are strongly influenced by the size of the atria - this is what doctors look at when assessing the result of EchoCG.
Drug cardioversion of arrhythmia in an elderly person: what to do
If there is no need or opportunity to perform general anesthesia, and this is very common in older patients, only medications have to be used. In parallel, treatment with beta blockers is allowed. This method is less effective, but may be sufficient.
The drug is selected only and exclusively by a doctor. Since all medications have their indications and contraindications. In addition, the first dose (course) of pills must be taken under the supervision of a specialist, because complications are possible. These include:
- low pressure;
- fibrillation;
- sinus node arrest;
- ventricular block.
Electrical cardioversion
The second option is to use special equipment. The main indication for using a defibrillator is a situation when medications simply cannot cope with the condition, and the dynamics of the disease are getting worse. It should be noted that this procedure for older people is always an increased risk; usually no one leaves without complications. But in some cases this is the only way to save life. So, possible consequences for the elderly:
- Embolism of blood clots.
- Prolonged arrest of the sinus node, that is, the impulse simply does not reach the myocardium.
- Ventricular fibrillation.
- The classic complications that occur with general anesthesia are a difficult undertaking in itself at this age.
Prevention methods
The following recommendations will help reduce the risk of developing arrhythmia in old age:
- it is necessary to promptly treat diseases of the cardiovascular system, as well as non-cardiac diseases that can provoke disturbances in the conduction of impulses in the heart muscle;
- it is important to give up junk food, smoking and drinking alcohol as soon as possible;
- you should regularly monitor blood glucose and cholesterol levels, as well as blood pressure levels;
- It is important to eat as much plant food as possible and take vitamin complexes.
Persons who are predisposed to the development of arrhythmia and heart disease in general need to protect themselves from stressful situations, anxiety, and emotional turmoil. If necessary, the specialist will recommend sedatives to patients with increased nervous excitability.
Arrhythmia in old age is especially dangerous, as it creates conditions for the accelerated formation of blood clots. This is fraught with heart attacks and strokes, which often result in death. To prevent the likelihood of severe complications and death, it is necessary to promptly diagnose the type of arrhythmia and take measures to correct the patient’s condition.
How to measure a person’s blood pressure and how is it measured?
It is very important for people suffering from hypertension to regularly monitor their blood pressure levels.
To do this, attending physicians recommend that their patients purchase a special device for measuring blood pressure, which is called a tonometer.
This device is required in every hospital and in any department. The second name for a tonometer is a sphygmomanometer.
Device design for measuring pressure and types of devices
The apparatus for measuring blood pressure consists of a cuff that is placed on the shoulder, a bulb with which air is pumped, two special tubes, one of which connects the cuff to the bulb, and the second with the pressure gauge scale itself, on which you can see numbers and an arrow, indicating the air injection level. All these elements are interconnected, but to take measurements you also need a stethoscope.
Currently, four types of sphygmomanometers are known:
- Mercury;
- Mechanical;
- Semi-automatic device;
- Automatic or electronic device.
Mercury is the most ancient and accurate apparatus. It does not err by more than 3 mmHg. The design of a mercury tonometer differs in that instead of a traditional scale and arrow we will see a glass column with a scale. There are divisions on it, the minimum is 0, the maximum is 260. When pumping air with a pear, the mercury accumulated at the bottom of the column will gradually rise.
The mechanical tonometer is considered standard and is used most often.
A semi-automatic device is more suitable for home use. Instead of a mechanical scale, there is an electronic one, which independently calculates blood pressure and pulse, but the air is still pumped in manually. An automatic or electronic device inflates and determines the pressure completely on its own; you just need to apply a cuff and turn it on.
Most often, they are purchased for home use to regularly measure blood pressure.
Basic rules for measuring human pressure
To take a correct blood pressure measurement, you need to sit quietly for a few minutes, calm down, and relax.
It is worth remembering that drinking coffee, alcohol or nicotine about an hour before the procedure can overestimate the true blood pressure readings. A person should sit or lie down in a comfortable environment.
The hand should be at heart level and completely relaxed. For the readings to be correct, it is better for the patient not to move or talk.
The algorithm for the immediate procedure is as follows:
- When the patient is completely ready, a cuff is placed on his arm approximately two fingers above the elbow. It should not be tightened too much, as there will also be air injection. A finger should fit freely between the cuff and the skin. Do not forget that the hand is located at the level of the heart.
- In the area of the elbow bend, you should feel the pulsation of the ulnar artery and apply the phonendoscope membrane to this place and put it on.
- Next, a special regulator is screwed onto the bulb, which is called an air release valve. Using a bulb, air is pumped into the cuff, up to approximately 220 units.
- The relief valve begins to be slowly and gradually unscrewed, releasing the air. At the same time, you need to monitor the needle on the pressure gauge scale, which will move in proportion to the speed of air release.
- You will hear the pulse beat through the stethoscope. The scale value at which the first beat sounds will indicate the upper, or systolic, pressure. The indicator at which the strokes subside is the lower, or diastolic, pressure.
- A person’s blood pressure is measured three times with an interval of 5-10 minutes; the average value is considered correct.
When using the electronic device yourself, you need to put a cuff on your arm, which will be located at the level of your heart, turn on the tonometer, and at the end it will show you the levels of systolic and diastolic pressure, as well as pulse rate.
The procedure should be repeated two more times.
Normal pressure indicators
Mature and elderly people often complain of headaches, redness of the face, the appearance of spots before the eyes, deterioration in their general condition, and sometimes even swelling in the legs. All these are symptoms of arterial hypertension. So what numbers are considered normal?
Normal pressure is considered to be from 110/70 to 130/90 mm Hg. But, as you know, the concept of norm is individual for everyone. If the systolic pressure is between 140 and 160, then this is stage 1 hypertension. If the indicators rise to 160-180, then this means the second degree. The third is diagnosed when the pressure rises to 200 mmHg. Art. and higher. It is most dangerous due to the occurrence of hypertensive crises, heart attacks and strokes.
It is necessary to measure the blood pressure of a person with high blood pressure several times a day to monitor the effectiveness of antihypertensive therapy and to prevent complications of the disease.
It is optimal to take measurements in the morning and evening.
How to choose the right tonometer?
The meter must be selected taking into account concomitant diseases, such as hypertension, previous heart attacks and strokes, and persistently low blood pressure. Basically, people buy an electronic or semi-automatic device because they are easy to use, rarely make mistakes in measurements, show the presence of arrhythmia, if any, remember about 30 recent pressure readings, and some can even be connected to computers. The device can be purchased at any pharmacy or medical equipment store.
Depending on your body type, age and arm circumference, you can choose a cuff of different sizes. There are three sizes - S, M and L. S is the smallest cuff, the length of which does not exceed 22 cm. M is larger, ranging from 22 to 32 cm in length, and L is the largest, reaching 45 cm.
All electronic and semi-automatic meters are supplied with an AC adapter to allow the device to be charged using electricity. But it is convenient because it can run on batteries.
Automatic blood pressure monitors, unfortunately, are much more expensive than mechanical ones. But the principle “more expensive means better” is not always true. Their disadvantages are that the battery discharges frequently and quickly. Measuring sensors must be tested and adjusted in a special service center, and, as mentioned above, they are very expensive. But despite all this, they are very convenient for home use.
Currently, the products of the following companies are trusted:
- Microlife;
- Frei;
- AND;
- Little Doctor;
- Well;
- NISSEI;
- OMRON;
- Rossmax.
All electronic devices have the advantage that they automatically pump air to the required level, detect rhythm disturbances, and can even announce measurement indicators, which is very important for blind people.
In addition to shoulder tonometers, there are also wrist tonometers. They are preferable for people who lead an active lifestyle and do not have enough time to fully measure blood pressure. In these devices, you can independently set the measurement frequency and save the indicators for further comparison. But they often produce errors, unlike conventional tonometers.
TO THE DOCTOR
how can I call you?:
Email (not published)
Subject of the question:
Question: