Among the various types of heart rhythm disturbances, it stands out in a special way. systolic arrhythmia. What is this known to experienced cardiologists, who, along with ventricular dysfunction, often encounter the presented pathology.
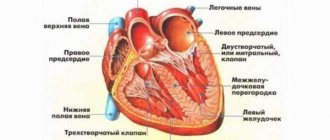
Normally, the cardiac cycle consists of alternating periods: systole (contraction) and diastole (relaxation). During diastole of the atria, blood enters them from the vessels, then they contract (systole) and expel the blood into the ventricles. The latter are also filled with blood in diastole from the atria and then expelled during systole into the general circulation.
The contractility of the heart is assessed precisely by its performance during systole, that is, by the ejection fraction. Normally it is 55-70%
Systolic function is the capacity of the heart, assessed by measuring ejection fraction. This indicator is determined using ultrasound diagnostics of the heart. If less than 40% is determined, then they speak of systolic insufficiency
functions, since less than 40% of the blood volume enters the general blood supply. This pathology is also known as heart failure with left ventricular systolic dysfunction. Systolic arrhythmia may also develop; whether this condition is dangerous can only be understood by considering the presented topic in detail.
Video: Cardiac cycle
Extrasystolic arrhythmia
The most common type of heart rhythm disturbance during myocardial infarction is extrasystolic arrhythmia .
The occurrence of extrasystolic arrhythmia is usually a consequence of increased myocardial excitability, which creates a threat of the development of atrial or ventricular fibrillation. In addition, frequent extrasystole can significantly worsen both the energy resources of the myocardium and the conditions of peripheral and coronary circulation. Thus, the appearance and increase in extrasystolic contractions should be considered an unfavorable prognostic sign, requiring constant ECG control (monitoring) and adequate treatment. In the acute period of myocardial infarction, treatment is necessary for all types of acute arrhythmia, even with rare (3-5 extrasystoles per 1 minute) atrial and ventricular extrasystoles. Polygonal group, “early” (approximation of extrasystolic impulses to the T wave of the previous complex) ventricular extrasystoles are especially dangerous.
For extrasystole, drugs are indicated that reduce myocardial excitability (lidocaine, procainamide, ajmaline, etc.), prolong the time of effective refractoriness (lidocaine, procainamide, quinidine), increase the speed of excitation and eliminate its differences, i.e. prevent (most antiarrhythmic drugs, including β-blockers, atropine), improving coronary blood flow (coronary dilators), tranquilizers, neuroleptics (difenin, phenobarbital, droperidol, etc.).
Lidocaine should be considered the drug of choice. It is used for ventricular extrasystole. Its single dose is 100-200 mg intravenously. Lidocaine is quickly inactivated in the body; with a single use, its effect is short-lived. Therefore, after eliminating the arrhythmia, a more or less long-term drip administration in the amount of 100-150 mg per hour is usually required. With this dosage, no side effects are observed (atriventricular block, convulsions, hypotension).
Procainamide is very effective, which, unlike lidocaine, also affects atrial rhythm disturbances. The drug is administered intravenously or intramuscularly (5-10 ml of 10% solution) at 4-hour intervals and continuously intravenously.
Atropine is indicated for extrasystole combined with bradycardia or conduction disturbances. For persistent extrasystole, beta-blockers (Inderal, Trazicor, Anaprilin, etc.) are recommended. In such cases, patients with myocardial infarction are prescribed drugs orally. For atrial and ventricular extrasystoles, ajmaline (50 mg orally or 1 mg of 5% solution intravenously), verapamil or isoptin (40-80 mg orally or 5 mg intravenously), rhythmodan (disopyramide, 100 mg capsule), pulsnorma (consisting of ajmaline, spartenia, antazoline and phenylethylbarbituric acid), a polarizing mixture (potassium + insulin + glucose) or other potassium preparations in a dose determined by the magnitude of its deficiency in plasma. If necessary, the acid-base balance is corrected.
Elimination of extrasystolic arrhythmia that occurs against the background of overload of the ventricular or atrium myocardium and incipient heart failure is sometimes achieved by prescribing cardiac glycosides (strophanthin, korglykon) and carrying out other measures that reduce the systolic load (diuretics, ganglion blockers, bloodletting, etc.), without the use of specific antiarrhythmic drugs.
For extrasystoles, including allorhythmias, which occur in some cases due to an overdose of cardiac glycosides, potassium preparations are highly effective. The use of other antiarrhythmic drugs (lidocaine, procainamide) in such cases is also often effective, but less desirable due to their more pronounced negative inotropic effect. It is generally accepted for digitalis intoxication to use SH-group donors (unithiol 5 ml intramuscularly 2-4 times a day), but their effect manifests itself rather slowly, which is why it is usually necessary to carry out combined treatment.
Does Anaprilin have any worthy analogues?
What analogues does Anaprilin have? Anaprilin and analogue drugs belong to the group of beta-blockers. They have a beneficial effect on the body. These drugs help in the fight against tachycardia, reduce the need for oxygen in the heart muscle, lower blood pressure, etc. It happens that Anaprilin is not suitable for a particular person, for example, it causes allergies. In this case, you should pay attention to similar drugs. They usually have the same effect, but a different composition. What kind of medicines are these? When is their use indicated?
Total information
As mentioned above, Anaprilin is a drug from the group of beta-blockers. Its main ingredient is propranolol. This substance enters the blood immediately after taking the medicine orally. The highest concentration is observed after 1 or 1.5 hours.
Indications for the use of the drug are considered to be several conditions:
- Unstable form of angina.
- Heart rhythm disturbances. This includes arrhythmia, tachycardia, extrasystole, etc.
- Migraine.
- Hypertension.
- Pheochromocytoma (tumor disease).
- Poisoning of the body with drugs based on the foxglove plant.
- Thyrotoxicosis.
- Ischemia.
Sometimes taking Anaprilin is strictly prohibited.
The list of contraindications looks like this:
- acute myocardial infarction;
- diabetes;
- peripheral arterial blood flow disorders;
- colitis;
- bradycardia;
- hay fever.
In all these cases, it is better to stop treatment with Anaprilin or replace it with similar drugs.
Some of the analogues have the same composition (active substance) as this drug. Others differ in composition, but have the same effect on the human body. If necessary, feel free to replace Anaprilin with them.
Same composition
In first place is the drug “Atobene”. These are tablets that have a composition similar to Anaprilin.
Indications for their use are:
- cardiac ischemia;
- angina pectoris;
- hypertension;
- hypertensive crisis;
- dystonia;
- various types of tremor, for example, senile and essential.
And also this drug is used as part of complex therapy in the treatment of pheochromocytoma (tumor), thyrotoxicosis and migraine.
In some cases, it is better to limit the use of Atobene or completely eliminate it:
- Individual intolerance to the substances included in the composition.
- Allergy to one or more ingredients.
- Bradycardia.
- Blood pressure too low.
- Diabetes.
- Low blood sugar.
- Raynaud's syndrome.
- Liver failure.
- Myasthenia.
- Psoriasis.
- The period of bearing a child.
- Childhood or old age.
It is not recommended to use Atobene without a doctor's prescription.
Another drug that can replace Anaprilin is Lokren. Like Atobene, it comes in tablet form. The instructions for use indicate that this medicine helps normalize the condition of high blood pressure, ischemia, myocardial infarction, tachycardia, arrhythmia and other similar conditions. Contraindications for use are the same as in the previous case.
When using Lokren, side effects may develop:
- Excessive fatigue.
- Weakness and dizziness.
- Headache.
- Myasthenia.
- Trembling of limbs.
- Dry eyes.
- Feeling cold in the legs.
- Pain in the heart area.
- Nausea and vomiting.
- Increase or decrease in blood sugar levels.
- Itching.
- Skin rashes.
- Changes in blood composition.
- In men, deterioration of potency.
- Shortness of breath and difficulty breathing.
If one of these symptoms appears, the drug should be stopped immediately. It is also recommended to seek help from a doctor.
Another medicine from the list of Anaprilin analogues is Propranobene.
It comes in several forms:
- capsules;
- solution for intravenous injection;
- solution for intramuscular administration;
- pills.
Indications for use of this product are:
- high blood pressure;
- angina pectoris;
- tachycardia of various origins;
- myocardial infarction;
- state of anxiety;
- thyrotoxic crisis;
- migraine attacks.
Several conditions can be identified as contraindications for the drug:
- Intolerance to the components included in the product.
- Cardiogenic shock.
- Low blood pressure.
- Severe form of bronchial asthma.
- Breast-feeding.
- Myasthenia.
- Psoriasis.
- Pregnancy period.
- Childhood.
- Advanced age.
Similarity in indications and action
Some modern drugs differ in their composition from Anaprilin.
But they have the same effect on the body. One example is Pumpan.
Indications for the use of these tablets are several diseases:
- Ischemia.
- Hypertension.
- Heart failure.
- Dystonia.
- Pathologies of the heart muscle.
- Arrhythmia.
- High blood cholesterol levels.
It is noteworthy that there are practically no contraindications to the use of Pumpan. The only condition when you should be careful is pregnancy. The drug does not have a harmful effect on the fetus. But it should be prescribed only after careful consideration of the risks and benefits. And there is also no data on overdose and its consequences.
You can replace Anaprilin with Angiovit. This remedy is in tablet form, which is usually used in the complex treatment of circulatory problems, atherosclerosis and ischemia. Angiovitis has virtually no side effects. True, nausea, vomiting and headache are sometimes noted. Its use is contraindicated only for those people who suffer from an allergy to one of the components included in the tablets.
Rimekor is also a good analogue of Anaprilin.
Indications for the use of tablets are:
- ischemia;
- angina attacks;
- dizziness caused by problems with blood vessels;
- noise in ears.
There are few contraindications to treatment with Rimecor:
- allergy to the drug;
- renal failure;
- liver pathologies;
- pregnancy and breastfeeding;
- age up to 18 years.
Side effects include itching, nausea, vomiting and tachycardia. It is worth noting that they appear extremely rarely.
Kudesan drops have a similar effect to Anaprilin.
They are used in the treatment of such conditions:
- ischemia;
- chronic form of heart failure;
- high blood pressure;
- arrhythmia;
- asthenic syndrome in children;
- congenital myopathy.
And drops are also used for excessive physical exertion and to prevent coenzyme Q10 deficiency.
Kudesan should be taken according to the regimen prescribed by your doctor. The dosage and duration of treatment will depend on age, disease and severity of symptoms.
The drug “Kratal” has the same effect on the body as Anaprilin. These are tablets that are used to treat various types of dystonia and chronic forms of coronary heart disease. In most cases, the doctor prescribes taking 1 or 2 tablets three times a day. On average, the course of treatment lasts for a month.
It is not recommended to take Kratal for those patients who suffer from intolerance to the substances that make up the drug.
What is extrasystolic arrhythmia and methods of its treatment
Extrasystolic arrhythmia is a disturbance in the heart rhythm associated with the occurrence of a single or paired premature contraction of the heart, and caused by excitation in the myocardium for a variety of reasons. The clinical picture of the disease is quite serious and it manifests itself in 60-70% of people.
If you do not consult a doctor in a timely manner for diagnosis and treatment, the condition may worsen. Basically, people begin to get used to such short-term attacks, but over time they can lead to sudden cardiac arrest.
Forecast and possible consequences
Since then, when a person is diagnosed with extrasystolic arrhythmia, he needs regular examination by a cardiologist and ECG monitoring to prevent the disease from developing into complex rhythm disturbances. Regular ECG monitoring and Holter monitoring are mandatory studies that help detect asymptomatic rhythm disturbances.
Some forms of extrasystoles can lead to more serious rhythm disturbances such as ventricular tachycardia. Untimely and inadequate assistance with the development of ventricular tachycardia can lead to death.
In situations where drug treatment is ineffective, instrumental and cardiac surgery are used.
With a benign course of ventricular extrasystole, complications do not develop. This type is easy to treat. For malignant PVCs, treatment can be lifelong. Possible complications include sustained tachycardia, ventricular fibrillation, asystole, cardiac arrest and death.
Timely treatment is the key to a favorable outcome. In the later stages of development of PVCs, the prognosis is always the same. The risk of sudden death is very high. Antiarrhythmic drugs and beta blockers will help improve the quality of life and reduce the risk of adverse complications.
Causes
The risk factors for extrasystolic arrhythmia are very serious, just like the clinical picture of the disease, and therefore, when the first symptoms appear, you should immediately consult a doctor. The causes of the disease include the presence of:
- ischemic disease;
- hypomagnesemia;
- hypokalemia;
- thyrotoxicosis;
- high activity from the ANS;
- congenital pathologies in the heart valves;
- previous diseases such as heart attack or myocarditis;
- activities through which muscle mass is gained.
As a rule, the cause can only be determined with a high-quality diagnosis by a professional and experienced specialist.
Useful video
The next video will show an excerpt from the popular TV show “Live Healthy!”, in which the presenters will explain in simple words what cardiac extrasystole is, what symptoms can be used to identify the disorder, how to start treatment in the early stages and share clinical recommendations.
Dr. Myasnikov will tell you what the diagnosis of atrial fibrillation means for a patient, what is the difference and how it differs from other types of arrhythmias, we will hear several typical case histories, and also find out whether it is possible to distinguish atrial fibrillation on your own.
Classification
The types of extrasystole can manifest themselves in very different ways, and each of them depends on a certain factor.
| What determines the type of extrasystolic arrhythmia? | Type of disease |
| Localization of the formation of an ectopic focus of excitation |
|
| Frequency of manifestations |
|
| Frequency of occurrence of extrasystoles |
|
There is a classification of extrasystolic arrhythmia according to etiology.
- Functional. With this type, a disturbance in the rhythm of the heart in a healthy person occurs when consuming alcohol, drugs, or smoking. Provoking factors may include banal tea and coffee, emotional stress or a severe stressful situation.
- Organic. Such a disorder can occur with myocardial damage, including if coronary disease is present, there has been a myocardial infarction, as well as cardiosclerosis, cardiomyopathy, pericarditis, myocarditis, myocardial damage after cardiac surgery.
- Toxic. The occurrence of such a disorder occurs during fever, as well as if thyrotoxicosis occurs. Such extrasystolic arrhythmia can be a side effect after taking certain types of medications, especially antidepressants.
Paroxysmal form of heartbeat
Recurrent ventricular tachycardia manifests itself in the form of short attacks - paroxysms. This type of arrhythmia is characterized by a more active heart than usual.
With paroxysmal tachycardia, the ECG recorded a cycle of 15–20 extrasystoles. Attacks are observed in organic pathology, and their occurrence is provoked by physical and emotional stress, smoking. Drinking alcohol and coffee also causes activation of the sympathetic-adrenal system with the development of paroxysmal palpitations.
In healthy people, tachycardia occurs suddenly, for no apparent reason. In the absence of heart pathology, treatment is not required. It is recommended to follow a daily routine, switch to a balanced diet, and avoid stress and physical overexertion. It is necessary to add foods containing magnesium, potassium and calcium to the diet.
Indications for treatment
Symptoms of extrasystolic arrhythmia can be either striking or almost invisible. In any case, if at least one of the signs of this disease appears, you should immediately contact a doctor for treatment.
Symptoms may include the presence of:
- discomfort or discomfort in the chest area;
- cardiac ischemia;
- extraordinary contraction that can disrupt the heart rhythm;
- a large number of contractions occurring in the ventricles;
- severe myocardial infarction;
- changes in hemodynamic parameters.
Treatment should be prescribed only by a qualified physician, since unauthorized use of drugs can cause a worsening of the condition.
Parasystole: causes, forms, symptoms, diagnosis, therapy
All materials are published under the authorship or editorship of medical professionals (about the authors), but are not a prescription for treatment.
Contact the specialists! © When using materials, a link or indication of the source name is required.
Author: Soldatenkov Ilya Vitalievich, general practitioner
Parasystole is a special type of arrhythmia caused by the presence of an additional source of cardiac impulse generation , which functions independently of the main pacemaker. Parasystole is considered a combined pathology, in which an extraordinary cardiac contraction occurs as a result of an abnormal impulse coming from any part of the heart. A double rhythm occurs: the main one is set by the sinus node, and the additional one is set by other pathological sources of generation from any part of the conduction system.
The paracenter is a pathological pacemaker that can be located in the ventricles of the heart, atria, or atrioventricular junction. It can be combined and multiple. A person may not feel any extraordinary contractions. In some cases, they are perceived as interruptions in the functioning of the heart and discomfort in the chest.
Parasystole occurs in persons with pathology of the cardiovascular system, endocrinopathies, hematological diseases, dysfunction of the nervous system, as well as in athletes.
Parasystole is characterized by the simultaneous and independent appearance of several competing centers of automaticity. Pathology occurs more often in adults than in children. In children, parasystole is not combined with concomitant, severe myocardial lesions, which are associated with the appearance of pathology in adult patients. The disease is difficult to treat with antiarrhythmics. Drug treatment for parasystole should be long-term. In most patients, the pathology is persistent and persistently recurrent. Frequent parasystole, combined with organic or structural heart diseases, has an unfavorable prognosis.
Treatment
Treatment of extrasystolic arrhythmia is preferably carried out in a hospital and under the supervision of doctors who are able to adjust therapy at the right time, if necessary.
- Initially, beta blockers are prescribed, which have a beneficial effect on the cardiovascular system and help reduce the number of contractions per minute.
- When pathology is detected, such as a change in the electrolyte composition of the blood fluid, magnesium and potassium intake is required.
- If the extrasystole is ventricular, then constant ECG and individual selection of drugs are necessary.
- Additionally, glycosides, diuretics, and ganglion blockers can be used.
In any case, the disease is treated by a doctor, and the patient must consume all prescribed medications every day. Otherwise, the condition may deteriorate to the point of cardiac arrest, which is treated in very rare situations.
Extrasystoles. Why do they happen? How to treat?
11. Guest
| 02.06.2014, 18:46:20 [2031746290]
The author, in principle, is Murashko, Kushakovsky, etc. It’s on the internet if you read it.
It's hot right now, maybe they lost K/Na - this is for the simplest reasons. With isolated Mg2+ deficiency, the pressure would most likely be increased.
Mushroom pickers sometimes have frequent extrasystole - as soon as all the botulinum toxins and tetanospasmin are collected, that’s how it begins.
Next - myocarditis (starting with streptococcus, which in rheumatism - while there is little of it and there is no pulmonary edema, and extrasystoles are single; by the way, single without shortness of breath and other sensations / disturbances - a variant of the norm), chlamydial (usually goes into the diagnosis of coronary artery disease / atherosclerosis and patients do not receive etiotropics) and other coronaritis, endocarditis (in IV patients), helminthic and microthromboembolism of the branches of the pulmonary artery, pellagritic and other thrombosis of the coronary sinus, etc.
Of the actual antiarrhythmics, if indicated, allapinine, mexiletine, BMCC, quinidine (see), again extrasystole or parasystole, atrial-nodal-ventricular.
Samples with nitrates, a/b, K, etc. can offer PPEFI
Symptoms and treatment of extrasystolic arrhythmia
Extrasystolic arrhythmia is a disturbance in heart rhythm caused by sudden contractions of the atria and/or ventricles. This disease can lead to the development of atrial fibrillation. The highest risk group is people over 50 years of age. Extrasystole develops due to the fact that in the heart, in addition to the main pacemaker located in the sinus node, other ectopic foci appear. In other words, in addition to the main center, nerve impulses that provoke compression begin to be generated in other places. In this case, the heart begins to pump less blood. This leads to a slowdown in hemodynamics (blood flow).
Parasystole and extrasystole: what are the differences?
In the presence of double rhythm formation, the patient may be misdiagnosed as extrasystole. The resulting treatment will be ineffective, although in some cases the symptoms of arrhythmia may be alleviated. Despite the fact that these two diseases are types of the same pathology, they require different approaches to therapy.
The difference between extrasystole and parasystole is that in the first case, the occurrence of additional impulses occurs in one zone, and therefore there is a stable interval between the extrasystole and the normal heart rhythm. With parasystole, there may be two or more sources of unplanned impulses, which leads to instability of the intervals between them.
Risk factors
Extrasystole can be caused by reasons of a functional, organic or toxic nature.
Functional forms of the disease are caused by neurological problems. In this case, extrasystolic arrhythmia can begin as a result of the development of:
- inflammation of the cervical spine;
- VSD (vegetative-vascular dystonia);
- neurosis;
- severe stress;
Organic extrasystoles are associated with myocardial pathologies:
- ischemia;
- heart attacks;
- heart defects;
- inflammation of the outer and middle lining of the heart;
- circulatory disorders;
- dystrophic processes.
The toxic form of the disease can result from:
- side effects of antidepressants and other drugs;
- hyperfunction of the thyroid gland;
- disturbances in the ratio of basic ions and acid-base balance.
Preventive measures
To prevent the development of parasystole, you must follow the following medical recommendations:
- Maintain a sleep schedule.
- Eliminate stress from everyday life. The patient may be prescribed sedative decoctions and other folk remedies.
- Quit smoking completely.
- Follow a diet and control your body weight.
- Exercise regularly.
- Patients whose development of parasystole was provoked by another disease need to actively treat this disease.
Parasystole is a deviation in the functioning of the heart associated with a change in rhythm. Seemingly harmless, over time it can cause associated pathologies, which creates a risk of death. Therefore, if any symptoms of the disease are detected, the patient should immediately consult a doctor.
Classification
Depending on the location of ectopic foci, the following are distinguished:
- ventricular extrasystoles (65% of all cases).
- atrial (25%).
- atrioventricular. Localized in the atrioventricular node (10%).
In rare cases, the site of the disease sends signals independently of the main (sinus) rhythm. Thus, two separate rhythms arise. This phenomenon is called parasystole.
The frequency of extrasystoles is of great importance. If more than 10 pathological beats per minute occur, this indicates the rapid development of the disease. Allorhythmia is often observed - alternation of additional contraction with normal systoles. Bigemnia is a rhythm in which the extrasystole is repeated after one full compression of the heart; trihemnia is an additional contraction after the usual two, and so on.
Symptoms
Depending on the cause of the disease, patients experience its manifestations differently. For example, people suffering from VSD feel extrasystole more strongly. Most often, patients feel shocks in the chest caused by contraction of the ventricles.
Functional extrasystolic arrhythmia is accompanied by fever, sweating, anxiety, and general weakness of the body. Early and group extrasystoles are characterized by a decrease in hemodynamic speed (blood movement) by 10–25%. If the pathology is complicated by atherosclerosis, the patient experiences dizziness and fainting, and with ischemia, attacks of pressing pain.
The following symptoms may also occur:
- suffocation;
- sense of anxiety;
- feeling of a sinking heart.
In severe forms, the disease may be accompanied by fainting.
What to do during an attack?
If symptoms persist for a long time, you should call an ambulance
An attack of arrhythmia cannot be tolerated. First of all, you should calm down and take a few deep breaths and exhalations. If such a simple technique does not bring your heart rate back to normal, you need to take a tablet of the drug recommended by your doctor for such cases.
If an attack of extrasystolic arrhythmia does not go away within 24 hours, you need to call an ambulance at home.
Diagnostics
The main diagnostic test is an ECG. Daily monitoring of electrical impulses provides a lot of information. In some cases, it may be necessary to take a sample after exercise.
The doctor should also find out the patient’s medical history:
- whether he or his parents had cardiovascular diseases;
- schedule;
- presence of bad habits;
- psychological condition.
Auscultation (listening) allows you to identify premature 1st and 2nd sounds. The first tone sounds stronger because the ventricles are not completely filled with fluid. The second one is heard more silently, because there is also not enough blood flowing into the aorta and pulmonary artery.
When palpating the radial artery, a wave is first observed, after which the pulse drops out. This also indicates that during contraction the ventricles are not completely filled with blood.
To diagnose organic extrasystole, MRI analysis, chest ultrasound and echocardiography may be needed.
Extrasystole
The human heart is designed in such a way that it allows blood to pass through it. This process is carried out through nerve impulses. Blood fluid passes from one atrium to another.
Namely, from right to left. There are cases when the electrical impulses that activate this transition fail. A condition occurs that is called extrasystole. Or, in other words, the cardiac cycle is disrupted.