5 / 5 ( 1 voice )
Tachysystole is a collective concept used to designate disturbances in heart rhythm in the direction of its acceleration. Tachysystole includes several pathologies accompanied by accelerated contraction of the atria or ventricles. Some of them are relatively mild, while others are life-threatening.
Tachysystole is a type of arrhythmia
Characteristics of the concept
What is tachysystole? This concept comes from two words - “tachy” (quickly) and “systole” (contraction). Thus, tachysystole is an acceleration of heart contractions. The normal heart rate is between 60-80 beats per minute. Anything over 80 is called tachyarrhythmia.
These disorders are quite common in cardiology.
The following forms of tachysystole are distinguished:
- sinus tachycardia;
- atrial tachycardia, fibrillation and fibrillation;
- ventricular tachycardia and fibrillation.
Each condition has its own manifestations.
Common deviations from the norm (brady- and tachysystole)
Sometimes the ECG conclusion may include a combination of normosystole and irregular sinus rhythm - “normosystole, irregular rhythm.” The latter can occur, for example, with respiratory or sinus arrhythmia. In this case, the rhythm comes from the sinus node (as it should be normally), but there are minor functional fluctuations in the heart rate due to the phases of inhalation and exhalation (normally, when inhaling, the heartbeat speeds up slightly, and when exhaling, it slows down slightly). Therefore, if a patient sees a conclusion about normosystole with an irregular but sinus rhythm, there is no point in panicking.
When a patient experiences an increase or decrease in heart rate, the doctor describes this as tachycardia or bradycardia. But sometimes he may write about tachysystole or bradysystole, which literally means frequent or rare heartbeats, respectively. In this context (assuming sinus ri and “systole” are synonymous.
Again, tachysystole and bradysystole can occur both in a completely healthy person and in various diseases of the heart or other organs. Here everything depends on other nuances obtained from the ECG. But if a person has a sinus rhythm with a slightly slow heart rate (at least 50 per minute) or increased heart rate (90-100) - especially from excitement, then we can talk about normal indicators.
Sinus tachycardia
This condition is not considered a disease and is not life-threatening. With sinus tachycardia, the heart rate exceeds 100 beats per minute.
There are two types of ST:
- Physiological . Appears with pronounced emotional excitement, physical stress, consumption of large doses of nicotine and caffeine. Physiological tachycardia is observed in young children and athletes.
- Pathological . Caused by certain diseases - anemia, fever, thyrotoxicosis, heart failure.
Symptoms of sinus tachycardia are rarely severe. A person may be bothered by a feeling of rapid heartbeat, interruptions in heart function, dizziness, and shortness of breath.
Sinus tachycardia is diagnosed by auscultation or by electrocardiogram. In the physiological form, it is necessary to avoid provoking factors and take sedatives. In the pathological form, the underlying disease is treated.
Sinus tachycardia is normal for newborns
Sinus rhythm: essence, reflection on the ECG, norm and deviations, features
Sinus rhythm is one of the most important indicators of normal heart function, which indicates that the source of contractions comes from the main, sinus node of the organ. This parameter is one of the first in the ECG conclusion, and patients who have undergone the study are eager to find out what it means and whether they should worry.
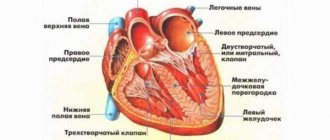
The heart is the main organ that supplies blood to all organs and tissues; the degree of oxygenation and the function of the entire organism depend on its rhythmic and consistent work. To contract a muscle, a push is needed - an impulse emanating from special cells of the conduction system. The characteristics of the rhythm depend on where this signal comes from and what its frequency is.
The sinus node (SU) is located under the inner lining of the right atrium, it is well supplied with blood, receiving blood directly from the coronary arteries, and is richly supplied with fibers of the autonomic nervous system, both parts of which influence it, contributing to both an increase and a decrease in the frequency of impulse generation.
The cells of the sinus node are grouped into bundles; they are smaller than ordinary cardiomyocytes and have a spindle-shaped shape. Their contractile function is extremely weak, but their ability to form an electrical impulse is akin to nerve fibers. The main node is connected to the atrioventricular junction, to which it transmits signals for further excitation of the myocardium.
The sinus node is called the main pacemaker, because it is the one that provides the frequency of heart contractions that gives the organs adequate blood supply, therefore maintaining a regular sinus rhythm is extremely important for assessing the work of the heart when it is damaged.
The control system generates pulses of the highest frequency compared to other parts of the conduction system, and then transmits them further at high speed. The frequency of impulse formation by the sinus node ranges from 60 to 90 per minute, which corresponds to the normal heart rate when they occur due to the main pacemaker.
Electrocardiography is the main method that allows you to quickly and painlessly determine where the heart receives impulses, what their frequency and rhythm are. ECG has become firmly established in the practice of therapists and cardiologists due to its accessibility, ease of implementation and high information content.
Having received the result of electrocardiography, everyone will look at the conclusion left there by the doctor. The first of the indicators will be the assessment of the rhythm - sinus, if it comes from the main node, or non-sinus, indicating its specific source (AV node, atrial tissue, etc.). So, for example, the result “sinus rhythm with heart rate 75” should not worry you, this is the norm, and if a specialist writes about non-sinus ectopic rhythm, increased heart rate (tachycardia) or slowdown (bradycardia), then it’s time to go for further examination.
Also in conclusion, the patient can find information about the position of the EOS (electrical axis of the heart). Normally, it can be either vertical or semi-vertical, or horizontal or semi-horizontal, depending on the individual characteristics of the person. Deviations of the EOS to the left or right, in turn, usually indicate organic pathology of the heart. The EOS and its position options are described in more detail in a separate publication.
Sinus rhythm is normal
Often, patients who detect sinus rhythm in the ECG report begin to worry whether everything is in order, because the term is not known to everyone, and therefore may indicate pathology. However, they can be reassured: sinus rhythm is the norm, which indicates the active functioning of the sinus node.
On the other hand, even with preserved activity of the main pacemaker, some deviations are possible, but they do not always serve as an indicator of pathology. Rhythm fluctuations occur in various physiological conditions that are not caused by a pathological process in the myocardium.
The impact of the vagus nerve and fibers of the sympathetic nervous system on the sinus node often causes a change in its function towards a higher or lower frequency of formation of nerve signals. This is reflected in the heart rate, which is calculated on the same cardiogram.
Normally, the frequency of sinus rhythm lies in the range from 60 to 90 beats per minute, but experts note that there is no clear boundary for determining normality and pathology, that is, with a heart rate of 58 beats per minute, it is too early to talk about bradycardia, as well as tachycardia if it exceeds indicator of 90. All these parameters must be assessed comprehensively, taking into account the general condition of the patient, the characteristics of his metabolism, type of activity, and even what he was doing immediately before the study.
Determining the source of rhythm when analyzing an ECG is a fundamental point, while the following are considered indicators of sinus rhythm:
- Identification of P waves before each ventricular complex;
- Constant configuration of atrial waves in the same lead;
- Constant value of the interval between the P and Q waves (up to 200 ms);
- The P wave is always positive (directed upward) in the second standard lead and negative in aVR.
At the conclusion of the ECG, the subject can find: “sinus rhythm with heart rate 85, normal position of the electrical axis.” We consider this conclusion to be the norm. Another option: “non-sinus rhythm with a frequency of 54, ectopic.” This result should be alarming, since serious myocardial pathology is possible.
The characteristics listed above on the cardiogram indicate the presence of sinus rhythm, which means that the impulse goes from the main node down to the ventricles, which contract after the atria. In all other cases, the rhythm is considered non-sinus, and its source lies outside the sinus system - in the fibers of the ventricular muscle, atrioventricular node, etc. Pulsation is possible from two places of the conduction system at once, in this case we are also talking about arrhythmia.
Correct conclusions about the regulation of heart rhythm can be made by studying long-term ECG recordings, since in the process of life all healthy people change their heart rate: at night the pulse is one, during the day - another. However, even shorter periods of recording ECG signs demonstrate pulse unevenness associated with the peculiarities of autonomic innervation and the functioning of the whole organism as a whole. Pulse assessment is helped by specially developed mathematical processing programs, statistical analysis - cardiointervalography, histography.
In order for the ECG result to be most accurate, all possible causes of changes in heart activity should be excluded. Smoking, quickly climbing stairs or running, or drinking a cup of strong coffee can change cardiac parameters. The rhythm, of course, will remain sinus if the node is working correctly, but at least tachycardia will be recorded. In this regard, before the study you need to calm down, eliminate stress and anxiety, as well as physical activity - everything that directly or indirectly affects the result.
Sinus rhythm and tachycardia
Let us remember again that sinus rhythm corresponds to a frequency of 60 - 90 per minute. But what to do if the parameter goes beyond the established limits while maintaining its “sinus”? It is known that such fluctuations do not always indicate pathology, so there is no need to panic prematurely.
Accelerated sinus rhythm of the heart (sinus tachycardia), which is not an indicator of pathology, is recorded when:
- Emotional experiences, stress, fear;
- Strong physical activity - in the gym, during heavy physical labor, etc.;
- After eating too much, drinking strong coffee or tea.
This physiological tachycardia is reflected in the ECG data:
- The length of the gap between the P waves and the RR interval decreases, the duration of which, with appropriate calculations, makes it possible to determine the exact heart rate figure;
- The P wave remains in its normal place - in front of the ventricular complex, which, in turn, has the correct configuration;
- According to calculations, the heart rate exceeds 90-100 per minute.
Tachycardia, with preserved sinus rhythm under physiological conditions, is aimed at providing blood to tissues that, for various reasons, begin to need it more - playing sports, jogging, for example. It cannot be considered a violation, and in a short period of time the heart itself restores the sinus rhythm to normal frequency.
If, in the absence of any diseases, the subject encounters tachycardia with sinus rhythm on the cardiogram, you should immediately remember how the study took place - whether he was worried, whether he rushed headlong to the cardiography room, or maybe he smoked on the stairs of the clinic just before taking an ECG.
Sinus rhythm and bradycardia
The opposite of sinus tachycardia is the slowing of its contractions (sinus bradycardia), which also does not always indicate pathology.
Physiological bradycardia with a decrease in the frequency of impulses from the sinus node to less than 60 per minute can occur with:
- State of sleep;
- Professional sports;
- Individual constitutional characteristics;
- Wearing clothes with a tight collar and a tightly tightened tie.
It is worth noting that bradycardia more often than an increase in heart rate indicates pathology, so close attention is usually paid to it. With organic lesions of the heart muscle, bradycardia, even if the “sinus” rhythm is maintained, can become a diagnosis requiring drug treatment.
During sleep, there is a significant decrease in heart rate - by about a third of the “daily norm”, which is associated with the predominance of the tone of the vagus nerve, which suppresses the activity of the sinus node. ECG is more often recorded in awake subjects, so such bradycardia is not recorded during routine mass studies, but it can be seen during 24-hour monitoring. If in the conclusion of Holter monitoring there is an indication of a decrease in sinus rhythm during sleep, then it is likely that the indicator will fit into the norm, which the cardiologist will explain to particularly worried patients.
In addition, it has been noted that about 25% of young men have a slower pulse in the range of 50-60, and the rhythm is sinus and regular, there are no symptoms of trouble, that is, this is a variant of the norm. Professional athletes are also prone to bradycardia due to systematic physical activity.
Sinus bradycardia is a condition when the pulse decreases to less than 60, but impulses in the heart continue to be generated by the main node. People with this condition may faint or experience dizziness; often this anomaly accompanies vagotonia (a variant of vegetative-vascular dystonia). Sinus rhythm with bradycardia should be a reason to exclude serious changes in the myocardium or other organs.
Signs of sinus bradycardia on the ECG will be a lengthening of the intervals between the atrial waves and the complexes of ventricular contractions, however, all indicators of the “sinus” rhythm are preserved - the P wave still precedes the QRS and has a constant size and shape.
Thus, sinus rhythm is a normal indicator on the ECG, indicating the preserved activity of the main pacemaker, and with normosystole the rhythm is both sinus and normal frequency - between 60 and 90 beats. In this case, there should be no cause for concern unless there are indications of other changes (ischemia, for example).
When should you worry?
Cardiography findings indicating pathological sinus tachycardia, bradycardia or arrhythmia with instability and irregularity of rhythm should be a cause for concern.
With tachy- and bradyforms, the doctor quickly determines whether the pulse is more or less abnormal than normal, clarifies complaints and refers for additional examinations - ultrasound of the heart, Holter, blood tests for hormones, etc. Having found out the cause, you can begin treatment.
Unstable sinus rhythm on the ECG is manifested by unequal intervals between the main teeth of the ventricular complexes, the fluctuations of which exceed 150-160 ms. This is almost always a sign of pathology, so the patient is not ignored and the cause of instability in the sinus node is found out.
Electrocardiography will also indicate that the heart beats with an irregular sinus rhythm. Irregular contractions can be caused by structural changes in the myocardium - scar, inflammation, as well as heart defects, heart failure, general hypoxia, anemia, smoking, endocrine pathology, abuse of certain groups of drugs and many other reasons.
An irregular sinus rhythm comes from the main pacemaker, but the frequency of the organ’s beats either increases or decreases, losing its constancy and regularity. In this case, they talk about sinus arrhythmia.
Arrhythmia with sinus rhythm can be a variant of the norm, then it is called cyclic, and it is usually associated with breathing - respiratory arrhythmia. With this phenomenon, the heart rate increases as you inhale, and decreases as you exhale. Respiratory arrhythmia can be found in professional athletes, adolescents during periods of increased hormonal changes, and people suffering from autonomic dysfunction or neuroses.
Sinus arrhythmia associated with breathing is diagnosed on an ECG:
- The normal shape and location of the atrial waves, which precede all ventricular complexes, are preserved;
- As you inhale, the intervals between contractions decrease, and as you exhale, they become longer.
Several tests can help distinguish physiological sinus arrhythmia. Many people know that during the examination they may be asked to hold their breath. This simple action helps to neutralize the effect of vegetatives and determine a regular rhythm, if it is associated with functional reasons and is not a reflection of pathology. In addition, taking a beta-blocker increases arrhythmia, and atropine relieves it, but this will not happen with morphological changes in the sinus node or heart muscle.
If the sinus rhythm is irregular and cannot be eliminated by holding your breath and pharmacological tests, then it’s time to think about the presence of pathology. It can be:
- Myocarditis;
- Cardiomyopathies;
- Ischemic disease, diagnosed in most older people;
- Heart failure with expansion of its cavities, which inevitably affects the sinus node;
- Pulmonary pathology - asthma, chronic bronchitis, pneumoconiosis;
- Anemia, including hereditary;
- Neurotic reactions and severe vegetative dystonia;
- Disorders of the internal secretion organs (diabetes, thyrotoxicosis);
- Abuse of diuretics, cardiac glycosides, antiarrhythmics;
- Electrolyte disturbances and intoxications.
Sinus rhythm, when irregular, does not exclude pathology, but, on the contrary, most often indicates it. This means that in addition to “sinus”, the rhythm must also be correct.
If the patient knows about his existing diseases, then the diagnostic process is simplified, because the doctor can act purposefully. In other cases, when an unstable sinus rhythm was found on the ECG, a complex of examinations is required - Holter (24-hour ECG), treadmill, echocardiography, etc.
Features of rhythm in children
Children are a very special part of people whose many parameters are very different from adults. So, any mother will tell you how often the heart of a newborn baby beats, but at the same time she will not worry, because it is known that babies of the first years and, especially newborns, have a pulse much faster than adults.
Sinus rhythm should be recorded in all children without exception, unless there is heart damage. Age-related tachycardia is associated with the small size of the heart, which must provide the growing body with the necessary amount of blood. The smaller the child, the faster his pulse, reaching 140-160 seconds per minute during the newborn period and gradually decreasing to the “adult” norm by the age of 8 years.
An ECG in children records the same signs of the sinus origin of the rhythm - P waves before ventricular contractions of the same size and shape, while tachycardia should fit into age parameters. The lack of activity of the sinus node, when the cardiologist indicates rhythm instability or ectopia of its driver, is a reason for serious concern for doctors and parents and a search for the cause, which in childhood most often becomes a congenital defect.
At the same time, when reading the indication of sinus arrhythmia according to the ECG data, the mother should not immediately panic and faint. It is likely that sinus arrhythmia is related to breathing, which is often observed in childhood. It is also necessary to take into account the conditions for taking an ECG: if the baby is laid on a cold couch, he is scared or confused, then a reflexive holding of breath will increase the manifestations of respiratory arrhythmia, which does not indicate a serious illness.
However, sinus arrhythmia should not be considered normal until its physiological nature is clearly proven. Thus, pathology of sinus rhythm is more often diagnosed in premature infants who have suffered from intrauterine hypoxia of children, with increased intracranial pressure in newborns. It can be provoked by rickets, rapid growth, VSD. As the nervous system matures, rhythm regulation improves, and disturbances may go away on their own.
A third of sinus arrhythmias in children are pathological in nature and are caused by hereditary factors, infection with high fever, rheumatism, myocarditis, and heart defects.
Sports for children with respiratory arrhythmia are not contraindicated, but only under the condition of constant dynamic monitoring and ECG recording. If the cause of unstable sinus rhythm turns out to be non-physiological, then the cardiologist will be forced to limit the child’s sports activities.
It is clear that parents are concerned about an important question: what to do if the sinus rhythm on the ECG is incorrect or an arrhythmia is recorded? First, you need to go to a cardiologist and give your child another cardiogram. If the physiological changes are proven, then observation and an ECG 2 times a year are sufficient.
If the instability of sinus rhythm does not fit within the normal range and is not caused by breathing or functional reasons, then the cardiologist will prescribe treatment in accordance with the true cause of the arrhythmia.
Source: miokard.lechenie-gipertoniya.ru
Supraventricular tachycardia
These conditions are associated with rapid contraction of the atria. There are several forms of pathology.
Table. Characteristics of atrial tachycardias:
| Form | Symptoms | Treatment instructions |
| Paroxysmal tachycardia - regular contractions are observed with a frequency of 150-230 per minute | Starts and stops suddenly. A person complains of an attack of rapid heartbeat and severe weakness. A decrease in pressure may be observed, and with significant hypotension, acute heart failure develops | You can stop the attack by inducing vomiting or coughing, inhaling with straining, and massaging the interclavicular fossa. The drugs used are adenosine or verapamil intravenously |
| Multifocal atrial tachycardia - the appearance of three or more consecutive extrasystoles | Usually not felt sick, numerous extrasystoles can cause weakness and dizziness | Verapamil is used intravenously |
| AV nodal tachycardia - increased frequency of atrial contractions up to 130 per minute | Manifested by dizziness. Usually occurs due to intoxication with glycosides, heart attack, heart surgery | Does not require specific treatment |
These diseases are also not life-threatening. For diagnosis, an electrocardiogram or Holter monitoring is used, where attacks of increased contractions are recorded.
What causes symptoms such as: Sinus arrhythmia, Brady-normosystole
Below are diseases that match your symptoms.
- Euthyroidism is a condition of the thyroid gland in which the levels of thyroid (T3, T4) and thyroid-stimulating hormones do not exceed normal limits. The term is used by endocrinologists to characterize the results of laboratory tests.
- Coronary heart disease (CHD) is a disease that occurs when the supply of oxygen through the coronary arteries to the heart muscle is limited.
- Ehlers-Danlos syndrome is a hereditary systemic connective tissue dysplasia caused by insufficient development of collagen structures.
Depending on the clinical type, Ehlers-Danlos syndrome can manifest itself as hypermobility of the joints, unusual vulnerability and extensibility of the skin, a tendency to hemorrhage and bleeding, deformities of the spine and chest, myopia, strabismus, ptosis of internal organs, etc.
- Graves' disease (diffuse toxic goiter) is an autoimmune endocrine disease and is a type of goiter. The disease can occur in mild and complicated forms.
- Epstein-Barr virus (EBV), a virus from the herpesovirus family, is a type 4 herpes virus. It can be present in the human body for life and cause a number of diseases. Epstein-Barr virus can appear in children at an early age. It has been proven that 80% of the entire world population are carriers of the virus.
- Respiratory failure is a pathological syndrome that occurs as a complication of certain diseases, which is based on a violation of gas exchange in the lungs. Acute and chronic natures of the disease are distinguished.
- Myocardial infarction (heart attack) is an acute form of coronary heart disease in which the blood supply is disrupted and blood does not reach the heart muscle. If blood does not reach the muscle for more than 15 minutes, the area dies (cardiac muscle necrosis). An area of dead heart cells is called a myocardial infarction.
- Cardiosclerosis is a disease of the heart muscle, which is characterized by deformation of the heart valves and replacement of the cardiac muscle tissue with connective tissue. Cardiosclerosis is a heart disease that can occur at any age, but against the background of vascular lesions it is observed mainly in middle-aged and elderly patients.
- The thyroid gland produces a hormone that determines how cells use energy. Hyperthyroidism occurs when the body produces excess amounts of these hormones.
- Paroxysmal supraventricular tachycardia is an increased heart rate. PSVT is a fairly common type of abnormal heart rhythm. It can happen at any age and in people who do not have other heart conditions.
- Wolff-Parkinson-White syndrome (also known as WPW syndrome) is a congenital abnormality of the heart structure, characterized by the presence of an additional pathway (bundle of Kent), which disrupts the heart rhythm. With this disease, cardiac impulses are conducted along the bundle of Kent, which connects the ventricles and atria. As a result, ventricular preexcitation occurs.
- Acute rheumatic fever is a systemic disease of connective tissue with a predominant localization of lesions in the cardiovascular system (carditis, valvular heart disease), the development of articular (arthritis), skin (rheumatic nodules, annular erythema) and neurological (chorea) syndromes that occurs in children 7-15 years against the background of the body’s immune response to group A beta-hemolytic streptococcus antigens and cross-reactivity with similar tissues of the human body.
- A heart attack is the death of part of the heart muscle due to insufficient blood flow to it. It is called a heart attack or coronary thrombosis. An attack occurs when one of the blood vessels supplying the heart muscle becomes blocked by a blood clot.
- Thyrotoxic crisis is the result of untreated hyperthyroidism. A person's pulse, blood pressure and body temperature can reach dangerously high levels.
- Hypocalcemia is a disease that develops when the electrophysiological process is disrupted and is characterized by a decrease in serum calcium levels to below normal levels. Hypocalcemia can occur in humans at any age and is diagnosed even in children at birth. This disease can be acute or chronic.
- According to the National Institute on Drug Abuse, about 15 percent of people in the United States have tried cocaine. Cocaine is a stimulant, meaning it increases alertness and energy. It affects the neural pathways in your brain, making you feel talkative, energetic, and euphoric. Addiction to cocaine can develop quickly, even after several attempts.
- Hypertension is a chronic disease characterized by a long-term and persistent increase in blood pressure (BP), caused by disruption of the heart and regulation of vascular tone and not associated with diseases of the internal organs. Possible symptoms of acute hypertension include sweating and chills.
- Wolff-Parkinson-White syndrome is a birth defect in which the heart develops an additional electrical pathway (bundle of Kent). May cause cardiac arrhythmia.
- Friedreich's ataxia is a genetically determined disease that occurs when iron is not transported properly from the mitochondria.
Never rely solely on search results to make a diagnosis. Be sure to consult a board-certified physician for diagnosis and treatment.
Source: https://healthchecker.net/symptom/%D0%A1%D0%B8%D0%BD%D1%83%D1%81%D0%BE%D0%B2%D0%B0%D1%8F%20 %D0%B0%D1%80%D0%B8%D1%82%D0%BC%D0%B8%D1%8F,%D0%91%D1%80%D0%B0%D0%B4%D0%B8- %D0%BD%D0%BE%D1%80%D0%BC%D0%BE%D1%81%D0%B8%D1%81%D1%82%D0%BE%D0%BB%D0%B8%D1 %8F/
general information
Sinus arrhythmia implies a malfunction of the heart when the difference between heartbeats is more than 10% (if this figure is less, there is no pathology). At the same time, the pulse remains within normal limits (60-80 beats per minute).
Sinus arrhythmia must be present in a person, since in a calm state the heart beats moderately, and in response to excitement or during physical activity, the pulse quickens. It allows you to see the level of adaptation of the heart muscle to stress and is, within certain limits, a sign of good health.
According to statistics, arrhythmias account for 10-15% of all heart diseases. In recent years, the number of cases has been growing. Sinus arrhythmia is most often observed in older people, as well as in those who abuse alcohol or drugs.
In children, sinus arrhythmia is present quite often, but in most cases it is not a pathology, since the nervous system simply cannot keep up with the growing body.
The disease does not require treatment if it develops against the background of severe nervous experiences. As soon as a person relaxes, it goes away on its own. To calm down in this case, you can use herbal remedies (valerian, motherwort).
Symptoms of the disease, especially in the early stages, do not appear clearly. A person may not realize that he has health problems for quite a long time.
Classification
Sinus arrhythmia is divided into the following types, determined by heart rate (HR):
- Tachyarrhythmia, in which a rapid heartbeat of over 80 beats per minute is monitored; blood does not fill the heart in full, which is why all internal organs suffer and blood flow is disrupted.
Identified in people with problems with the thyroid gland and autonomic nervous system;
A decrease in heart rate below 40 beats per minute can lead to fainting or even cardiac arrest and death;
The cause may also be forms of ischemic heart disease and dystrophy of the heart muscle. Cardiac output is unproductive. The patient experiences a feeling of a sinking heart, dull tremors in the heart area, a feeling of anxiety and lack of air;
Inherent in children and adolescents, in adults sinus respiratory arrhythmia sometimes accompanies vegetative-vascular dystonia, brain diseases, and appears after severe infections.
Stages
The following stages of the disease are distinguished:
- Mild (moderate) sinus arrhythmia - for the most part does not manifest itself in any way, can be a specific feature of a particular organism, and can also accompany old age.
It is not a deviation from the norm if it is associated with hormonal changes in the body (in adolescents). It is necessary to consult a doctor to determine the exact cause and nature of the disease.
- Sinus arrhythmia of the first degree - symptoms occur rarely and, as a rule, go away on their own, the patient does not experience discomfort.
Often manifested in breathing disorders (respiratory arrhythmia), detected in adolescents during puberty, in athletes, and in older people. Consultation with a doctor is required, especially if frequent fainting occurs. - Sinus arrhythmia of the second degree - the symptoms are most clearly expressed and coexist with various heart diseases.
A person develops severe weakness, fatigue, and shortness of breath. There is a possibility of developing serious complications. An examination of all internal organs is required. - severe stress, psychological depression;
- intrauterine developmental defects;
- tumors and heart defects;
- pathologies of internal organs;
- heredity;
- poisoning;
- long-term and severe infections;
- myocardial diseases.
Causes
In young and middle-aged people:
- high blood pressure;
- heart defects;
- chronic lung and thyroid diseases;
- alcoholism and smoking;
- viral infections;
- stress;
- heart surgery;
- lack of potassium and magnesium in the body.
In older people, sinus arrhythmia, in addition to the above reasons, is almost always a manifestation of another heart disease, a consequence of other health problems, including age-related ones. Risk factors may include: taking medications, rich fatty foods, abuse of coffee and cigarettes.
Symptoms and signs
Symptoms of sinus arrhythmia are associated with abnormal heart rhythms. A person complains of “fading” of the heart, shortness of breath, lack of air, dizziness, weakness and fainting; he has panic attacks associated with feelings of fear and anxiety.
The first signs of the disease are:
- palpitations; palpitations;
- pain on the left side of the chest, radiating to the arm;
- inability to take a full breath;
- dyspnea;
- pulsation in the temporal region;
- attacks of severe weakness, dizziness, fainting;
- coldness of the extremities.
Diagnostics
The following methods are used to diagnose sinus arrhythmia:
- ECG (electrocardiogram) - as a paramount method;
- EPI (electrophysiological study);
- echocardiogram;
- monitoring (episodic, Holter);
- load test;
- orthostatic test;
- laboratory tests (general blood test, blood test for T3 and T4 hormones);
- determination of heart rate variability.
We figured out what sinus arrhythmia means, but here’s what it looks like on an ECG:
Differential diagnosis is to recognize the disease in time and prevent complications. That is why the doctor always prescribes an ECG for rhythm disturbances and as a preventive therapeutic method, which allows recognizing pathology and works as an initial diagnostic method.
First aid
An attack can take you by surprise; it begins suddenly and ends the same way. The patient should call an ambulance.
Before the team arrives, you need to try to calm the person down, create comfortable conditions, open a window, you can give a sedative (motherwort, valerian, valocordin).
If the patient loses consciousness, you need to tilt your head back and unfasten the collar. If there is no breathing or heartbeat, it is necessary to perform artificial respiration until the ambulance arrives.
Treatment and rehabilitation
Treatment should be strictly under the supervision of a specialist. Basic techniques:
- healthy balanced diet (refusal of coffee, strong tea, alcohol, fatty and sweet foods);
- to give up smoking;
- drug treatment (sedatives, tranquilizers, antiarrhythmic drugs);
- installation of a pacemaker (for severe disease);
- surgery;
- traditional medicine (only together with the main treatment and with the permission of a doctor): treatment with asparagus, lemons, walnuts and honey, hawthorn;
- treatment with leeches.
How to treat sinus arrhythmia in each individual case is determined by the attending physician.
Rehabilitation after an attack of sinus arrhythmia consists of receiving medical care, which will be aimed at restoring the heart rhythm (drug or electrical stimulation), ensuring the most calm conditions.
Learn more about what sinus arrhythmia means in the video:
Atrial fibrillation
This is an uncoordinated contraction of the muscle fibers of the atria, in which the heart rate reaches 700 beats per minute.
There are two forms of fibrillation:
- paroxysmal - lasts no more than two days;
- chronic - lasts more than two days.
Atrial fibrillation is registered in 0.5% of the population, but among people over 65 years of age it occurs in 5%.
Causes
30% of the population has an idiopathic form of the disease, that is, it has no apparent cause.
In the rest, the pathology develops against the background of cardiac and extracardiac diseases:
- heart attack;
- pericarditis or myocarditis;
- heart surgery;
- heart defects;
- hypertension;
- cardiomyopathy;
- alcoholism;
- thyrotoxicosis;
- TELA;
- electrical injury;
- pneumonia.
More often, the pathology develops against the background of heart disease. Many foci appear in the cardiac tissue that generate electrical impulses (photo). As a result, excitation and contraction of individual areas of the myocardium occur.
Mechanism of development of atrial fibrillation
Manifestations
Patients with atrial fibrillation complain of increased fatigue, dizziness, a feeling of rapid heartbeat, shortness of breath, and attacks of loss of consciousness. In some patients with underlying heart disease, signs of heart failure increase. Less commonly, there are no complaints - the asymptomatic form.
The examination reveals characteristic signs of the underlying disease. On auscultation, a rapid heartbeat is recorded.
Diagnostics
The diagnosis is confirmed after instrumental studies:
- ECG . There is an absence of P waves (normal atrial contractions); instead, specific f waves appear. There is an irregular heart rhythm.
- Holter monitoring . It is carried out to determine the number of attacks of fibrillation per day.
- Ultrasound of the heart . Detects heart disease, assesses ventricular function, and detects intracardiac blood clots.
To exclude thyrotoxicosis as a cause of fibrillation, the content of thyroid hormones in the blood is examined.
Therapeutic measures
Treatment goals for atrial fibrillation:
- restoration of normal rhythm;
- prevention of paroxysms of fibrillation;
- prevention of complications, primarily thromboembolic.
If the rhythm is severely disrupted, emergency defibrillation is performed.
Restoring a normal rhythm helps improve the patient’s overall well-being and reduces the risk of thromboembolic complications. For this purpose, first class antiarrhythmic drugs are used - Propafenone or Amiodarone. The drugs are administered orally or intravenously. In case of chronic fibrillation, anticoagulants are prescribed on a regular basis.
Surgical treatment is indicated when conservative methods are ineffective. It consists of destroying the AV connection with a radio knife and installing an artificial pacemaker.
Normosystole, tachysystole and bradysystole on the ECG: what is it, norm and pathology
Tachysystole is a collective concept used to designate disturbances in heart rhythm in the direction of its acceleration. Tachysystole includes several pathologies accompanied by accelerated contraction of the atria or ventricles. Some of them are relatively mild, while others are life-threatening.
Tachysystole is a type of arrhythmia
Types and causes of tachysystole
There are several types of tachysystole: atrial, paroxysmal, supraventricular, nodal, atrial flutter and fibrillation, ventricular tachycardia. Treatment options are selected by the doctor individually, taking into account the type of disease and the individual characteristics of the individual patient.
There are also many reasons why tachysystole can occur. Heart failure may be one of them.
Cardiac glycosides contribute to the conversion of the tachysystolic form of atrial fibrillation to normosystolic, which is achieved with intravenous administration of glycosides.
Prevention of tachysystole
Prevention of attacks of tachysystole has problems in the context of ischemic cardiomyopathy, since it is very difficult to predict in advance the effectiveness of a particular drug. During long-term use of the drug, one must take into account its side effects. It is because of this that those drugs with minimal side effects are preferred.
The most promising drug for the prevention of attacks of tachysystole is Ethmozin. Since with its long-term use it has practically no side effects and at the same time success with its use is achieved in 50% of all identified cases. Also, in a number of cases, a convincing effect was obtained from “Ri and Isotin”.
If you have been diagnosed with this by a qualified specialist, then you first need to follow all his recommendations to improve your health.
In addition, you should not self-medicate, because traditional medicine can only worsen your health condition. After diagnosing tachysystole, constant supervision by the attending physician is necessary.
If new symptoms appear, you should seek advice from a medical institution to avoid a sharp deterioration in health.
The problem of preventing attacks of tachysystole is of great importance in ischemic cardiomyopathy. It is difficult to predict in advance which drugs may be effective.
If you need to take drugs for a long time, you have to take into account their side effects.
Sensitivity to the drug may be different for the same type of arrhythmias. Our employee T.G.
Gomzyakova (1972), who treated a large group of patients with persistent attacks of tachysystole on an outpatient basis, in most cases tested 3 to 5 drugs in succession before finding an effective remedy for each patient.
At the same time, in 75% of patients it was possible to achieve a reduction in the frequency of attacks by 2-3 times or their disappearance. In half of the patients the effect lasted from a year to 3-4 years, in 1/5 - up to a year, in the rest - at least 2 months.
Potassium preparations, in particular potassium chloride (2.0 - 4.0 g per day) and panangin (2 tablets 3 times a day), often in combination with glycosides, maintain sinus rhythm in cases where paroxysms of flutter and flicker appeared for the first time or occurred rarely before treatment and the patients were not actually treated.
Most patients received quinidine before admission to the clinic, and it turned out to be ineffective or stopped working.
Of the 11 patients in whom treatment with quinidine began in our clinic (0.45 - 0.6 g per day), the effect was noted in only one case, which does not agree with the data of other authors on the effectiveness of quinidine in these cases (I.M. Arrigoni, 1968).
Perhaps this is due to the particular persistence of attacks in our patients. Recently, data have appeared on the great promise of using durul quinidine for this purpose.
One of the most promising drugs for the prevention of paroxysmal tachysystoles, especially atrial fibrillation and supraventricular, in patients with coronary artery disease is ethmozin (carbazine).
Its long-term use (0.05 - 0.075 g per day) gives virtually no side effects, and success is achieved in 50% of all cases. Novocainamide (1.5 - 2.0 g per day) is effective only for ventricular tachysystoles in approximately 1/4 of patients.
In some cases of this type of arrhythmia, antithyroid drugs were effective.
"Ischemic heart disease", ed. I.E. Ganelina
The phenomenon of atrial fibrillation is better known to a wide range of people without medical education as atrial fibrillation. This form of pathology refers to supraventricular rhythm disturbances. In this case, the impulses to contract the heart do not come from the sinoatrial node. They are generated by elements of the conduction system located above the ventricles.
Hence another name - supraventricular arrhythmia. The excitation wave can come from the atrioventricular center or from atypical electrically active areas of the atria. In the latter version, we are talking about fibrillation (twitching of myofibrils - contractile fibers of the myocardium).
More detailed information on this topic can be found in this article.
Normosystole: concept, how it is reflected on the ECG, norm and deviations
All materials are published under the authorship or editorship of medical professionals (about the authors), but are not a prescription for treatment. Contact the specialists!
Sazykina Oksana Yurievna, cardiologist
The patient cannot always independently interpret the medical terms read in the electrocardiogram protocol. Of course, only a doctor can decipher the cardiogram itself and the resulting conclusion, but what should you do before your appointment? First, decide on the terminology and try to understand for yourself whether your cardiogram is normal or not.
Forms of atrial fibrillation
Atrial fibrillation is characterized as a failure of the contractile activity of the heart muscle. In this case, individual areas of the atrium are randomly excited, preventing complete normal contraction of the chamber.
The number of flickers reaches 300-600 per minute.
The antrioventricular node conducts only a portion of this large number of electrical impulses, as a result of which the ventricles begin to work asynchronously, with different frequencies and sequences.
During fibrillation, the atria cannot be fully filled with blood, and accordingly, the ventricles do not perform their function normally. The strength and volume of cardiac output decrease, the body does not receive the required amount of nutrients and oxygen.
Atrial fibrillation has several varieties. They can be classified according to the following criteria:
- ventricular rate;
- features of waves on a cardiogram;
- duration of the abnormal rhythm.
Based on frequency, fibrillation is divided into:
The number of ventricular contractions corresponds to normal values (60-90 per minute).
The work of the ventricles is slow, they contract less than 60 times per minute. In this case, the pulse wave passes normally.
The ventricles contract more frequently than normal (more than 100 beats per minute). However, there may be periodic absence of a pulse. This happens because the chambers of the heart are not working at full capacity. Weak contractions do not produce a pulse wave. Sometimes cardiac output is irregular because the ventricles are not filling enough with blood.
The most favorable prognosis is considered for normosystolic and bradysystolic forms of atrial fibrillation.
Wave subtypes of fibrillation:
The cardiogram shows large and rare (from 300 to 500 per minute) contraction waves.
The duration of atrial fibrillation may vary. This serves as a reason to highlight another classification criterion:
- Primary atrial fibrillation.
This is a single rhythm disturbance that was recorded for the first time. It can vary in duration, symptoms and nature of complications.
Source: https://klinika-krovi.ru/bolezni-serdca/tahisistoliya-chto-eto-takoe.html
Atrial flutter
This is a regular contraction of the atrium muscle with a frequency of 250-300 per minute. It is rarely observed, as it is an unstable condition that quickly turns into a normal rhythm or fibrillation. It can be paroxysmal or chronic.
The causes and symptoms of flutter are no different from those of fibrillation. The ECG shows sawtooth F waves at the site of the P waves.
Treatment is similar to fibrillation.
F waves in atrial flutter
Normal heart rate
The concept of normosystole usually also refers to the fact that electrical signals that contribute to the sequential electrical excitation of all parts of the heart are generated in the sinus node, which is normally the first-order pacemaker. In all other cases, they speak of pacemaker migration or non-sinus rhythm. These processes are united by the concept of heart rhythm disturbances, or arrhythmias.
Therefore, usually in the ECG conclusion, in addition to the characteristics of the heart rate (HR), in the first place there is a mention of whether the patient has sinus rhythm or not. If the patient sees the term “normosystole” in the protocol, then most likely this means that he has not only a correct, normal heart rhythm, but also a sinus rhythm - that is, it comes from the sinus node, as it should be normally. (Nevertheless, there are formulations of “normosystole” with an even heart rate, but non-sinus rhythm - more on this at the end of the article).
Paroxysmal ventricular tachycardia
This is a condition that occurs as a result of the appearance of three or more ventricular extrasystoles following each other.
Causes
There is an idiopathic form that occurs for no apparent reason. In other cases, ventricular tachycardia develops against the background of any heart disease. An ectopic focus forming in the ventricle causes its extraordinary contractions.
Symptoms
The clinical picture of paroxysmal tachycardia is poor. The patient complains of dizziness, clouding of consciousness. A decrease in pressure is objectively determined.
Diagnostics
Ventricular tachycardia is determined using an electrocardiogram. There is a deformation of the QRS complex (contraction of the ventricle), overlapping of the atrial and ventricular complexes.
Treatment
In most cases, the condition does not require specific treatment. A persistent attack of VT is treated with intravenous lidocaine. Signs of hemodynamic compromise require defibrillation.
Tachysystole irregular sinus rhythm
Mechanism of heart contractions
The function of regulating the number of heart contractions is performed by the conduction system of the heart, which consists of the following elements and structures:
- sinoatrial (sinoatrial) node;
- muscle tracts;
- internodal atria;
- atrioventricular node;
- atrioventricular bundle.
The impulse that excites cardiac contraction begins from the sinoatrial node.
Then the excitation is transmitted along the internodal pathways of the atria, provoking their depolarization, approaches the atrioventricular node and is transmitted through the atrioventricular bundle to the muscles of the ventricles.
At the slightest failure of the impulse strength in any part of the conduction system, episodic or organic disruptions of the heart rhythm (extrasystoles) may occur.
Extrasystole disease
Extrasystoles (extrasystoles) are atypical depolarization and premature contractions of the heart or its individual chambers.
As a rule, patients diagnosed with extrasystole experience a short-term freezing of the heart rate, lack of air and an intense cardiac impulse.
Such abnormal heartbeats and pauses between contractions provoke an impulse outside the cardiac sinus node.
Differential and etiological diagnosis of extrasystole is difficult in cases where heart rhythm disturbances are a side effect of another cardiovascular disease. When extrasystole occurs, it is imperative to undergo a full diagnosis and evaluate the functional state of the myocardium.
Types of extrasystoles
Premature heart contractions (complexes) according to the mechanism of occurrence are: parasystoles and extrasystoles. The differences between the types are clearly visible on daily ECG monitoring.
In cardiology there are:
1. Functional extrasystoles. Diagnosed in people with signs of neurosis or autonomic dysfunction. Such extrasystoles are recorded at rest; during emotional outbursts or after physical activity, atypical complexes cease.
With a functional malfunction of the heart rhythm, patients may feel extrasystoles: tremors behind the sternum, hot flashes, anxiety, discomfort and lack of air. In most cases, the development of functional extrasystoles is benign.
Gastric monotopic changes are recorded on the ECG.
2. Organic extrasystoles. Typical for elderly patients. As a rule, organic extrasystoles accompany endocrine disorders, heart disease, and chronic intoxication.
Subtle signs of premature heart beats occur after stress or exercise. Such complexes do not prevent patients from leading an active lifestyle. Cardiac contractions of high gradations are organic in 95% of cases.
In this case, ventricular, polytopic, atrial, atrioventricular and group extrasystoles are recorded on the ECG.
Bigeminy
Bigeminy in cardiology refers to a certain type of supraventricular (supraventricular) or ventricular extrasystole. This type of arrhythmia develops due to dysfunction of the autonomic and central nervous system.
The main cause of bigeminy is organic changes in the heart muscle.
Even small deviations in the myocardium with extracardiac origin and associated factors provoke the appearance of an ectopic focus of excitation.
Ventricular bigeminy is characterized by uniform alternations of a normally occurring contraction with a single ventricular extrasystole, which is a type of allorhythmia. Untimely excitation of the right cardiac ventricle is also recorded. Supraventricular bigeminy is a paired alternation of one rhythmic contraction and one extrasystole.
The diagnosis of “bigeminy” is common in rheumatic heart defects (mitral valve prolapse and aortic stenosis). The disease often accompanies cardiomyopathies, myocarditis and thyrotoxicosis.
Classification of extrasystoles
Depending on the area of localization and ectopic foci of excitation, extrasystoles are distinguished:
- Atrial.
- Ventricular
- Atrioventricular and nodal (atrioventricular).
- Sinoatrial (sinus extrasystole).
Extrasystole can have one or more sources of excitation. The following types of extrasystoles are diagnosed:
- Monotopic - with one focus of development and a stable interval in areas of the cardiogram.
- Polytopic - several centers of occurrence and different intervals of linkage.
- Unstable paroxysmal tachycardia is a series of extrasystoles following each other.
Today, several classification systems for arrhythmias are used in medicine. The most common modified version of the “Lown & Wolf” gradation offers the following classification of ventricular extrasystoles:
Source: https://office-gemotest.ru/serdce/normo-bradisistoliya.html
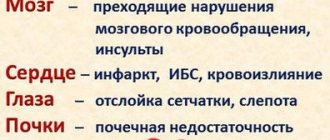
Ventricular fibrillation and flutter
These rhythm disturbances are characterized by uncoordinated contraction of the ventricles at a rate of 250-300 per minute. On the ECG it is recorded as a sinusoidal curve. Leads to cardiac arrest and clinical death.
Emergency defibrillation is required and resuscitation measures are taken. To prevent this condition, patients have a cardioverter-defibrillator installed in the heart area.
Tachysystolic heart rhythm disturbances are a large group of conditions characterized by various types of increased heart rate. Some of them are safe for life and do not cause any clinical manifestations. Some arrhythmias are life-threatening and require urgent treatment.
What is sinus tachysystole?
Tachysystole is a collective concept used to designate disturbances in heart rhythm in the direction of its acceleration. Tachysystole includes several pathologies accompanied by accelerated contraction of the atria or ventricles. Some of them are relatively mild, while others are life-threatening.
Normosystole, tachy- and brady-: the concept of how it is reflected on the ECG, norm and deviations
© Sazykina Oksana Yurievna, cardiologist, especially for SosudInfo.ru (about the authors)
The patient cannot always independently interpret the medical terms read in the electrocardiogram protocol. Of course, only a doctor can decipher the cardiogram itself and the resulting conclusion, but what should you do before your appointment? First, decide on the terminology and try to understand for yourself whether your cardiogram is normal or not.