Order No. 273 of November 23, 2004
Standard of sanatorium-resort care for patients with disorders of the autonomic nervous system and neurotic disorders associated with stress, somatoform disorders
Patient model
Age category: adults, children
Disease class V: mental and behavioral disorders
Group of diseases: neurotic, stress-related and somatoform disorders
ICD-10 code: F45.3. F48.0, F48.8
Types and symptoms of NCD
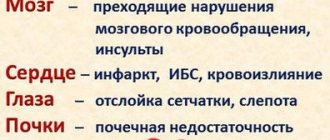
General symptoms of dystonia: neurosis, fatigue, weakness, irritability, decreased memory and attention. The cardiac type is characterized by shortness of breath, irregular heart rhythm, a slight decrease or increase in blood pressure, and pain in the heart. Since neurocirculatory dystonia of the cardiac type does not have precise symptoms, it is difficult to immediately determine the disease. To make it easier to diagnose the pathology, according to the complaints of patients, it was divided into 4 forms:
- Cardialgic. The main symptom is pain in the heart, which can be aching, squeezing, or stabbing.
- Tachycardic. Characterized by an increase in heart rate of more than 100 beats per minute. Accompanied by shortness of breath, headache, panic attacks.
- Arrhythmic. Heart rhythm disturbances in the form of ventricular fibrillation, atrial fibrillation or extrasystole. The arrhythmic form is also manifested by severe fatigue, weakness, pallor of the skin, and shortness of breath.
- Bradycardic. It is characterized by a decrease in heart rate, signs of lack of oxygen: weakness, dizziness, cold extremities.
Depending on the level of pressure, hypotensive, hypertensive, and mixed forms are distinguished. In the first form, systolic pressure decreases to less than 100 mm. rt. Art., dizziness, lightheadedness or loss of consciousness occurs. The hypotensive form is characterized by severe weakness, fatigue, and coldness of the feet and hands. As a rule, patients have a thin build, cold, wet palms, and pale skin.
In the hypertensive form, there is a transient increase in systolic pressure from 130 mm. rt. Art. and higher. More often, this form does not manifest itself as a deterioration in the general condition; sometimes patients complain of periodic headaches, palpitations, and weakness. The manifestations of neurocirculatory dystonia of the hypertensive form are similar to hypertension.
You can distinguish the symptoms of NCD from diseases of the cardiovascular system by the following signs:
- With NCD, pain occurs during physical activity, and with heart pathology afterwards.
- Instability of emotions, moods, and a neurosis-like state are not typical for heart diseases.
- In case of NCD, the symptoms are varied and can manifest themselves in many organs and systems; in case of heart pathology, the symptoms are associated only with it.
- After taking sedatives, symptoms of NCD decrease or disappear. They are not effective for heart pathologies.
With NCD, secondary symptoms may occur in the form of apathy, tremors in the limbs, chills, and sleep disturbances.
Important! Symptoms of dystonia can arise and disappear spontaneously, unlike cardiac pathology.
Vegetative-vascular dystonia code according to ICD-10
Home -> Types of VSD -> Vegetative-vascular dystonia code according to ICD-10
The fact is that the International Classification of Diseases (ICD 10) does not include diseases such as vegetative-vascular dystonia and neurocirculatory dystonia. Official medicine still refuses to recognize VSD as a separate disease.
Therefore, VSD is often defined as part of another disease, the symptoms of which appear in the patient and which is indicated in ICD-10.
For example, with VSD of the hypertensive type, of arterial hypertension (hypertension) can be made . Accordingly, the ICD-10 code will be I10 (primary hypertension) or I15 (secondary hypertension).
Very often, VSD can be defined as a symptom complex characteristic of somatoform dysfunction of the autonomic nervous system . In this case, the ICD-10 code will be F45.3 . Here the diagnosis must be made by a psychiatrist or neuropsychiatrist.
VSD is also often defined as “Other symptoms and signs related to emotional state ” (code R45.8 ). In this case, consultation with a psychiatrist is not necessary.
Non-drug treatment
The main thing in the treatment of NCD is the formation of a correct lifestyle, correction of work and rest schedules, and adequate sleep.
You should refuse overtime and night work, business trips, and if there are occupational hazards, minimize their impact as much as possible or change your type of activity.
It is important to follow a diet, normalize weight, give up alcohol and smoking, take long walks in the fresh air, adequate physical activity, and avoid stress.
Treatment of NDC requires a comprehensive approach and includes psychotherapeutic intervention, physical therapy, physical therapy, and only if absolutely necessary, drug correction of symptoms.
It is important to eliminate foci of chronic infection and correct general somatic disorders. Therapy with multivitamins and adaptogens is prescribed.
Hormonal disorders must be stopped, especially in women.
They use sedatives, often of plant origin - valerian extract, motherwort.
With the participation of a psychotherapist, stronger drugs are prescribed - tranquilizers (phenazepam, diazepam, chlordiazepoxide), which have an anxiolytic and vegetative-stabilizing effect, and a pronounced antiphobic effect.
To relieve sympathoadrenal crises, beta-blockers are prescribed. B vitamins are used in courses.
Therapeutic baths (pine, oxygen), contrast showers, magnetic therapy, laser therapy, thermal procedures, and mud treatment are used.
Acupuncture is prescribed, and massage is extremely effective. Physical therapy is mandatory, as it increases the body’s ability to adapt and trains the circulatory system.
Rational psychotherapy is important to help reduce stress and return to a normal psycho-emotional state.
Relaxation techniques help, which include diaphragmatic breathing, muscle relaxation, training with image building and teaching stress tolerance and problem solving skills.
Vegetative-vascular dystonia in children can manifest itself as cardiac, respiratory, neurotic syndromes, vegetative-vascular crises, and thermoregulation disorder syndrome.
Diagnosis of vegetative-vascular dystonia in children includes a functional examination of the cardiovascular, nervous, and endocrine systems (ECG, EEG, EchoCG, EchoEG, REG, rheovasography, etc.). In the treatment of vegetative-vascular dystonia in children, medication, physiotherapy, and psychological effects are used.
Vegetative-vascular dystonia in children is a secondary syndrome that affects various somato-visceral systems and develops against the background of deviations in the autonomic regulation of the functional state of the body. According to various data, certain signs of vegetative-vascular dystonia are diagnosed in 25-80% of children.
More often, the syndrome is found in children 6-8 years old and in adolescents, predominantly female.
In pediatrics, vegetative-vascular dystonia is not considered as an independent nosological form, therefore, various narrow disciplines are studying its manifestations: pediatric neurology, pediatric cardiology, pediatric endocrinology, pediatric gastroenterology, etc. Autonomic disorders in children can give impetus to the development of serious pathological conditions - arterial hypertension, bronchial asthma, gastric ulcer, etc. On the other hand, somatic and infectious diseases can aggravate vegetative changes.
toxicosis of the pregnant woman, fetal hypoxia, intrauterine infections, rapid or protracted labor, birth injuries, encephalopathy, etc. A special role in the development of vegetative-vascular dystonia in children belongs to various psychotraumatic influences - conflicts in the family and school, pedagogical neglect of the child, overprotection, chronic or acute stress, increased school loads.
Predisposing factors for vegetative-vascular dystonia in children can be somatic, infectious, endocrine diseases, neuroinfections, allergies, focal infections (chronic tonsillitis, caries, pharyngitis, sinusitis), constitutional abnormalities, anemia, traumatic brain injuries. The direct triggers of autonomic dysfunction in most cases are unfavorable weather conditions, climatic features, unfavorable environmental conditions, physical inactivity, imbalance of microelements, excessive physical activity, poor nutrition, violation of the daily routine, insufficient sleep, hormonal changes during the puberty period.
Autonomic disorders are accompanied by various reactions of the sympathetic and parasympathetic systems, caused by impaired production of corticosteroids, mediators (acetylcholine, norepinephrine), biologically active substances (prostaglandins, polypeptides, etc.), impaired sensitivity of vascular receptors.
When diagnosing vegetative-vascular dystonia in children, a number of criteria are taken into account, which are decisive in distinguishing the forms of the syndrome. According to the predominant etiological signs, vegetative-vascular dystonia in children can be psychogenic (neurotic), infectious-toxic, dyshormonal, essential (constitutional-hereditary), mixed in nature.
Depending on the nature of autonomic disorders, sympathicotonic, vagotonic and mixed variants of vegetative-vascular dystonia in children are distinguished. Taking into account the prevalence of vegetative reactions, vegetative-vascular dystonia in children can be generalized, systemic or local.
According to the syndromological approach during vegetative-vascular dystonia in children, they distinguish between cardiac, respiratory, neurotic syndromes, thermoregulation disorder syndrome, vegetative-vascular crises, etc. According to the severity, vegetative-vascular dystonia in children can be mild, moderate and severe; according to the type of flow - latent, permanent and paroxysmal.
The clinical picture of vegetative-vascular dystonia in a child is largely determined by the direction of autonomic disorders - the predominance of vagotonia or sympathicotonia. About 30 syndromes and more than 150 complaints accompanying the course of vegetative-vascular dystonia in children have been described. Cardiac syndrome of vegetative-vascular dystonia in children is characterized by the development of paroxysmal cardialgia, arrhythmia (sinus tachycardia, bradycardia, irregular extrasystole), arterial hypotension or hypertension.
In the case of a predominance of cardiovascular disorders in the structure of vegetative-vascular dystonia, they speak of the presence of neurocirculatory dystonia in children. Neurotic syndrome with vegetative-vascular dystonia in children is the most constant. Typically, the child complains of fatigue, sleep disturbances, poor memory, dizziness, headaches, and vestibular disorders.
Children with vegetative-vascular dystonia experience low mood, anxiety, suspiciousness, phobias, emotional lability, and sometimes hysterical reactions or depression. With leading respiratory syndrome, shortness of breath develops at rest and during physical stress, periodic deep sighs and a feeling of lack of air are noted.
Reactions of the digestive system can be characterized by nausea, increased or decreased appetite, unmotivated abdominal pain, and spastic constipation.
The urinary system is characterized by a tendency to fluid retention, swelling under the eyes, and frequent urination.
Children with vegetative-vascular dystonia often have marbled coloration and increased greasiness of the skin, red dermographism, and sweating.
Children with vegetative-vascular dystonia need consultation with a pediatrician, as well as (in accordance with the leading causes and manifestations) a pediatric neurologist, pediatric cardiologist, pediatric endocrinologist, pediatric gastroenterologist, pediatric otolaryngologist, and pediatric ophthalmologist. The initial autonomic tone and autonomic reactivity are assessed using the analysis of subjective complaints and objective indicators - ECG data, Holter monitoring, orthostatic, pharmacological tests, etc. To assess the functional state of the central nervous system in children with vegetative-vascular dystonia, EEG, REG, EchoEG, and rheovasography are performed.
During the diagnosis, other pathologies that have similar clinical manifestations are excluded: rheumatism, infective endocarditis, juvenile arterial hypertension, bronchial asthma, mental disorders, etc.
When choosing methods for treating vegetative-vascular dystonia in children, the etiology and nature of autonomic disorders are taken into account. Preference is given to non-drug therapy. General recommendations include normalizing the daily routine, rest and sleep; dosed physical activity; limiting traumatic influences, consulting a family and child psychologist, etc.
For vegetative-vascular dystonia in children, courses of general massage and massage of the cervical-collar zone, IRT, physiotherapy (electrophoresis on the collar zone, endonasal electrophoresis, galvanization, electrosleep), exercise therapy have a positive effect.
Water procedures are useful: swimming, therapeutic showers (circular, fan, Charcot shower), general baths (turpentine, radon, pine, carbon dioxide). An important role in the complex therapy of vegetative-vascular dystonia in children is given to the treatment of focal infection, somatic, endocrine, etc. diseases.
If it is necessary to include drug therapy, sedatives, nootropics, multivitamin complexes are used, and, according to the indications of a pediatric psychoneurologist, antidepressants or tranquilizers are used.
Diagnostics
The variety of symptoms and similarity with the signs of many diseases makes it difficult to make a diagnosis, so a careful differential diagnosis is necessary. Dystonia can be suspected based on the following signs, which are observed for about 2 months:
- heartbeat;
- periodic sensations of lack of air;
- increased fatigue, weakness;
- irritability;
- anxiety;
- sleep disturbance;
- heartache;
- dizziness;
- cold extremities.
These symptoms have a clear connection with the emotional state. The disease has a period of exacerbations and remissions, and progression is not observed, as with cardiac pathologies. One of the criteria indicating NCD is instability of the heart, a tendency to increase its rhythm, which occurs unexpectedly in stressful situations. The most informative research methods:
- ECG. Extrasystole, pacemaker migration, arrhythmia, and changes in the T wave are detected.
- Hyperventilation test. Alternating forced inhalations and exhalations for 25-35 minutes to record changes on the ECG.
- Orthostatic test. After taking an ECG while lying down, the person is asked to stand up for 15 minutes, and then the readings are taken again.
- Samples with drugs. Used to distinguish dystonia from heart disease.
When examining blood, an increase in the level of lactic acid, metabolic substances, adrenaline, and norepinephrine is noted.
Diagnosis of NCD by mixed type
Although the causes of VSD lie in a person’s head, physical health should not be neglected. If there are signs of dystonia, it is recommended to make a primary diagnosis, which includes:
- General blood and urine analysis.
- Blood chemistry.
- Ultrasound of vital organs.
- ECG.
- Rheoencephalography.
It is necessary to consult a neurologist, endocrinologist, cardiologist, gynecologist (for women), and urologist. Other specialists and studies are assigned as needed.
The main problem of modern doctors is that they do not consider the disease as a single whole of soul and body. Each specialist begins to treat a person exclusively in his own field, which ultimately leads to the prescription of a bunch of useless medications and a lot of wasted nerves and money. Therefore, when identifying NCD, it is recommended to immediately find a competent psychotherapist who can help the patient look at his body as a single system, and at his illness as a single problem, and find the underlying causes of the “failure.”