Features of children's extrasystole
Previously, doctors believed that children mainly experienced ventricular arrhythmia.
But the results of modern research prove that all types of extrasystoles occur with almost identical frequency. The reason for this phenomenon is quite simple: the child’s body is rapidly growing and developing, the heart cannot cope with the additional functional load, so it begins to compensate for the “lag” with extrasystoles. As a rule, as soon as the period of active growth ends, the arrhythmia disappears without drug intervention.
Why is extrasystole dangerous in children: this pathological phenomenon can be a consequence of various pathologies of the thyroid gland, lungs, and myocardium
At the same time, young patients complain of the same symptoms as adults - frequent dizziness, weakness, cardiac “thrusts” in the chest. Important: drug treatment of ventricular arrhythmia is indicated only when the daily number of extrasystoles reaches 15,000 (children are prescribed metabolic, antiarrhythmic therapy). Such patients must be registered with a dispensary and undergo a comprehensive examination at least once a year.
What symptoms accompany the disease?
Extrasystole, which is within the normal range, is not characterized by any symptoms; people often learn about it only when reading the ECG results.
Standards:
- up to 960 per day is considered the norm for healthy people
- from 960 to 1200 is the norm for patients with diagnosed polymorphic extrasystoles
- more than 1200 per day is a sign of pathology
However, not all people have a hidden nature; they can manifest themselves in the following symptoms:
- Sensation of tremors in the chest area
- The feeling that the tremors are separated by pauses
- After shocks, a slow or rapid heartbeat is felt
- Darkness in the eyes, dizziness
- Shortness of breath, difficulty breathing,
- Increased sweating, chills
- Pallor of the skin,
- Anxiety, discomfort, panic attacks
Usually, extrasystoles are described as “the heart turned over”, “stopped”; the symptoms are very varied and subjective, especially if this is a manifestation of neurological problems. The most common symptom is a strong shock in the chest area, which is explained by a sharp contraction of the ventricles.
Irregular contractions can occur during moments of fear, causing a feeling of tightness inside the chest, followed by a rapid heartbeat.
If there is a disappearance of symptoms during the period of observation by a doctor or with the arrival of emergency assistance, or while being in a calm environment, then the probability that such arrhythmia has a functional origin tends to one hundred percent.
In such cases, taking antidepressants quickly improves the patient’s condition, and the arrhythmia attacks end after the start of treatment.
Bibliography
- Doshchitsin V.L. Clinical electrocardiography. - M.: Medical Information Agency, 1999. - 373 p.
- Cook-Soup So Clinical interpretation of ECG. Introduction to electrocardiography. - M.: MEDpress-inform, 2020. - P. 179-188.
- Kushakovsky M.S. Cardiac arrhythmias. - St. Petersburg: Foliot, 2007. - pp. 241-331.
- Mazur N.A. Paroxysmal tachycardias of the heart. M.: Medpraktika-M, 2005. - P. 24-105.
- Nedostup A.V., Blagova O.V. How to treat arrhythmias. Rhythm and conduction disorders in clinical practice. - M.: MEDpress-inform, 2013. - P. 10-22.
- Okorokov A.N. Diagnosis of diseases of internal organs: T 6. Diagnosis of diseases of the heart and blood vessels. — M.: Med. lit., 2002. - 449 p.
- Orlov V.N. Guide to electrocardiography. - M.: Medical Information Agency, 2003. - P. 354-367.
- Suvorov A.V. Clinical electrocardiography. - Nizhny Novgorod: NMI, 1993. - pp. 45-47.
- Fomina I.G. Heart rhythm disturbances. - M.: Russian doctor, 2003. - 192 p.
- Shevchenko N.M., Grosu A.A., Olishevko S.V. Extrasystole // Cardiology, 1990. - No. 8. - P. 109-111.
- Vaughan Williams EM Classification of antiarrhythmic action / Williams EM Vaughan, ed. // Handbook of Experimental Pharmacology: Antiarrhythmic Drugs. - Berlin: Springer-Verlag, 1989. - P. 45-76.
Classification and differences between species, stages
The gradation and danger to health and life during ventricular extrasystole is determined according to the Lown classification. The following classes of PVCs are distinguished:
- 0 – complete absence of ventricular extrasystoles;
- 1 – single contractions caused by an impulse from the same source;
- 2 – the impulse is also monomorphic, but their number is more than 30 per hour;
- 3 – extrasystoles from different foci;
- 4 – divided into two types: A – paired extrasystoles, B – group extrasystoles, which are also called short runs of ventricular tachycardia;
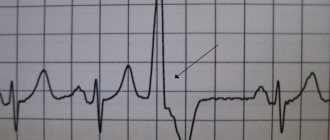
- 5 – PVC, in which the ventricular complex “overlaps” the T wave of the previous cycle. Such extrasystole is the most dangerous and can lead to arrhythmia, which significantly affects hemodynamics, causes shock and death.
Based on the time of occurrence, three types are distinguished:
- early - ventricular contractions occur during the passage of an impulse through the atria;
- interpolated ventricular extrasystoles - simultaneously with contraction of the upper chambers of the heart;
- late - occurring during diastole.
Ordered ventricular extrasystoles are called allorhythmia. When cardiac arrhythmia (CHD) such as ventricular extrasystole occurs after each normal complex, they speak of bigeminy, when after two normal complexes, they speak of trigeminy, and so on.
Folk recipes
The list of folk remedies for the treatment of vagal extrasystole is quite large. But they are applicable only as auxiliary methods as part of complex treatment. After consulting with a specialist, you can use “grandmother’s” recipes:
- Hawthorn – use dried flowers as tea leaves (a tablespoon per 200 ml of boiling water). Drink three glasses every day. You can prepare a tincture: per tablespoon of flowers - 200 ml of vodka. After leaving for 10 days in a dark place, drink a teaspoon three times a day;
- Calendula - pour a teaspoon of flowers into a glass of boiling water, let it brew, strain. Drink 100 ml four times a day;
- Horsetail - pour a tablespoon of horsetail into 600 ml of boiling water, leave for three hours. Strain, drink a tablespoon six times a day;
- Cornflower - add a teaspoon of dried flowers to 200 ml of boiling water and leave. Strain, drink on an empty stomach three times a day;
- Lumbago – add two teaspoons of dried flowers to 200 ml of boiling water and let it brew. Drink a third of a glass three times a day;
- Honey and chopped radish - mix in equal proportions, drink a tablespoon three times a day.
For the most part, patients with extrasystole do not need antiarrhythmic treatment. The reticence of specialists when prescribing rhythm stabilizers is understandable: complications associated with their use are often more dangerous than manifestations of extraordinary impulses.
Diagnosis of the disease
To diagnose the disease, general clinical and instrumental methods are used. First of all, complaints are carefully collected, this will help to establish when the extrasystoles first appeared, under what conditions certain symptoms occur, and what the child feels.
General examination and complaints
Children do not immediately begin to complain of discomfort in the heart area. Often, they first go to doctors of other specialties; children are examined by pediatric neurologists or gastroenterologists. A neurologist complains of dizziness, headaches, nocturnal enuresis, weather dependence, and a gastroenterologist examines him for biliary dyskinesia and gastrointestinal dyspepsia. And only after an ECG, these specialists send the child for a consultation with a cardiologist.
Normally, the pulse wave corresponds to heart contractions, but with arrhythmia, a loss of beats is noted. Auscultation can be heard in pairs, the first is loud and clear, and the second is muffled. In addition, it is necessary to conduct a blood test for electrolytes and thyroid hormones. Rule out past infections that can cause heart complications.
Instrumental examination
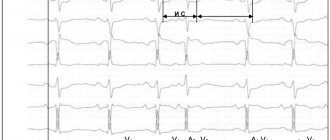
You can instrumentally confirm or refute the presence of a disease in a child using an ECG. This pathology is determined by characteristic signs:
- the presence of premature heart contractions with a deformed QRS complex;
- absence of P waves;
- the appearance of drainage complexes;
- the presence of a complete compensatory pause after the ventricular extrasystole passes.
Holter monitoring is a study that allows you to determine when ventricular extrasystole occurs during the day. The essence of the study is that the child is attached to a special monitor, with which he walks for 24 hours or more (the duration is indicated by the doctor).
Keeps a special diary. Based on the decoding results, it is possible to determine the circadian rhythm of the extrasystole (it occurred during the day or at night), detect life-threatening forms of arrhythmia, carry out differential diagnosis with other types of diseases, and evaluate the effectiveness of the treatment.
Any treatment for children depends on the overall picture of the patient’s condition. If the extrasystoles are single and not accompanied by additional complaints, then treatment is not required, and the patient undergoes dispensary observation. An ECG is performed every 6 months. In newborn babies, this disease occurs as a result of hypoxia.
Therefore, it is important to feed the baby breast milk to obtain all the necessary elements for normal heart function.
Drug treatment is selected individually, depending on the patient’s age and severity of the condition. In addition to cardiogenic drugs, sedatives and nootropic drugs are also actively used. The goal of treatment is to normalize the heart rate. Antiarrhythmic drugs are divided into 4 groups. The choice is determined by the etiology of extrasystole. Most antiarrhythmic drugs cause bradyarrhythmia.
Extrasystole: 6 groups of causes, main symptoms, treatment features
https://pixabay.com/illustrations/heart-curve-crack-ecg-health-66892/
What are extrasystoles in the heart? In a healthy person, the heart contracts rhythmically. The impulses are generated by the pacemaker - the sinus node.
Electrical signals travel from top to bottom to the ventricles. But sometimes, due to certain reasons, this system undergoes changes.
Below in the ventricles an extraordinary electrical impulse occurs, and the heart muscle contracts ahead of schedule.
This is an extrasystole, after which there is a short pause, and then the heart begins to beat rhythmically again. The main purpose of heart contraction is the release of blood.
Extrasystoles occur during diastole, when the heart is resting and filling with blood.
So, the heart does not have time to fill with a sufficient amount of blood; accordingly, little blood is ejected, as a result of which less blood flows to all organs and tissues.
https://pixabay.com/illustrations/heart-care-medical-care-heart-1040227/
The main causes of extrasystole
We need to figure out what is the cause of extrasystole? We must understand that extrasystole is a secondary disease, a symptom of some problem. It is necessary to find the cause and its elimination will lead to success in the treatment of extrasystole. Etiology of extrasystole:
- Idiopathic form (20%) - when it is impossible to find an obvious cause of extrasystole. Usually, this form hides previous myocarditis.
- Electrolyte imbalance.
- Pathology of the cardiovascular system:
- Pathology of internal organs:
- problems with the spine,
- pathology of the gastrointestinal tract,
- oncological diseases,
- endocrine diseases,
- anemia.
- Acute and chronic intoxication.
- Taking medications.
https://pixabay.com/photos/woman-person-desktop-work-aerial-3187087/
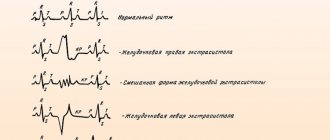
There are ventricular, atrial (supraventricular) extrasystole and extrasystole from the atrioventricular junction.
Extrasystoles are single, paired and salvo. According to their rhythm, extrasystoles are divided into periodic (bigymenia, trihymenia) and non-periodic.
According to the number of foci - monotopic and polytopic. The Lown classification, based on the quantitative characteristics of extrasystoles, is quite popular in Russia. But I want to emphasize that it can only be used in relation to patients who have suffered a myocardial infarction.
We should be afraid not of the quantity of extrasystoles, but of their quality.
The fact is that a person can have 20-30 thousand extrasystoles, but absolutely safe, and 10 extrasystoles, but with poor characteristics. But Bigger’s classification, proposed back in 1984, is still quite relevant today.
Here are the types of arrhythmias he offers:
- prognostically safe arrhythmias (functional) - rare, single extrasystoles with good characteristics, are effectively treated and resolve quickly;
- potentially dangerous arrhythmias are a huge number of extrasystoles, safe in their characteristics. But they can lead to unpleasant consequences in the future;
- prognostically life-threatening ari) are arrhythmias in those who already have coronary heart disease, have had tachycardia in the past, suffered clinical death, or unclear loss of consciousness. Or reduced ejection fraction, dilation of the heart cavities and significant bradycardia.
Many people do not feel extrasystole in any way, that is, it can be asymptomatic. In this case, it is first detected on an electrocardiogram. In some people, extrasystole still occurs. What worries the patient during extrasystole?
These are interruptions, single or frequent pauses in the work of the heart, attacks of rapid irregular heartbeat, a feeling of “a fist in the chest.” When extrasystoles occur at night, the person, accordingly, sleeps poorly and is anxious. All this is sometimes accompanied by shortness of breath, dizziness, weakness, pain in the heart region of various types.
Auscultation of the heart
During the general examination, the patient showed no special changes. When auscultating the heart, the usual regular rhythm is heard and against this background a premature contraction. This is the extrasystole. It is characterized by a loud 1st tone and a weakened 2nd tone. Palpation of the pulse is necessary. Extrasystole is characterized by irregularity and pulse deficiency.
To diagnose extrasystole, it is enough to undergo electrocardiography and Holter ECG monitoring. When examining a patient's electrocardiogram, it is possible to determine the presence of extrasystole, its localization, morphology, density and rhythm.
Characteristic signs of extrasystoles on an ECG:
- atrial: altered P wave, normal ventricular QRS complex;
- ventricular: the QRS complex is widened and changed;
- extrasystoles from the atrioventricular junction: normal QRS complex, the P wave is absent or appears after the QRS complex in an altered form.
Holter
Holter monitoring is carried out over 24 or 48 hours and provides a more detailed analysis of extrasystoles.
Determines their number during the day, type, connection with various factors and at what time of day they predominantly occur. Additionally, echocardiography and stress tests are recommended.
Echocardiography reveals organic pathology of the heart in humans. Stress tests are performed to exclude ischemic heart pathology.
In more rare cases, MRI of the heart is recommended when the cause of the occurrence is unclear or there is a suspicion of hereditary extrasystoles. An electrophysiological study of the heart is carried out in certain situations when there is already coronary heart disease and unfavorable echocardiographic signs.
https://pixabay.com/photos/ambulance-emergency-medic-health-3592155/
Treatment of extrasystole
If extrasystoles are detected, there is no need to self-medicate. First of all, you need to find out the reason. During the interview, it is found out what diseases the patient has, heredity, and the presence of heart disease.
If extrasystole can not be treated, then it is advisable not to treat it.
The choice of treatment for extrasystoles depends on which heart they occurred on. If a person does not have organic heart pathology, this is one case. If extrasystoles occur due to heart disease, the approach is completely different.
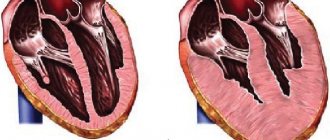
Therefore, the most important thing is to determine whether there is heart disease or not. What is organic heart pathology? These are a history of myocardial infarction, low ejection fraction, and valvular heart disease.
When treating extrasystoles, you need to take into account the type of extrasystoles (ventricular or supraventricular).
Recommendations from Academician A. Revishvili
Here are the approaches to treatment offered by the famous academician A. Revishvili:
- it is considered dangerous and therapy is necessary for extrasystole more than 20,000/day and if there is heart disease;
- no treatment is required for extrasystole less than 20,000/day and the person does not feel them;
- Treatment is required if there are 100 extrasystoles per day. A person feels each of them as a “blow to the chest.”
- also, treatment is not required if 200 extrasystoles per day are detected and when there is no heart disease.
Treatment of extrasystole in patients without cardiovascular pathology
So, let's consider the treatment of extrasystoles in a person without heart pathology. Most of these extrasystoles are safe. With functional extrasystoles, treatment of the underlying disease is important.
Observation by a doctor and monitoring of extrasystoles using echocardiographic examination twice a year are recommended. Sedatives can be used. If symptoms are severe, antiarrhythmic drugs .
These are mainly 2 classes of antiarrhythmic drugs - beta-blockers and class I drugs (Propafenone, Allapinin). The main role of beta-blockers is their effect on the characteristics of extrasystoles, but they do not eliminate the symptoms of the disease.
And class I drugs reduce the number of extrasystoles.
Treatment of extrasystole due to heart disease
If extrasystole is associated with heart disease, then potassium, magnesium, and metabolic agents (omega-3 PUFAs) are used.
Among the antiarrhythmic drugs for the treatment of ventricular extrasystoles, beta-blockers (Metoprolol, Bisoprolol) in combination with Amiodarone are used. Amiodarone may be recommended to relieve symptoms of arrhythmia.
It must be remembered that patients after myocardial infarction should not take class I drugs.
Calcium antagonists (Verapamil, Diltiazem) are used primarily for supraventricular arrhythmias. Also, beta-blockers and class I drugs (Allapinin, Propafenone) are effective for supraventricular extrasystole. If the patient has bradycardia, then the dosage of drugs must be carefully selected.
Surgery
If drug treatment does not help, then the question of surgical treatment . This is the so-called radiofrequency ablation of ectopic sites. In later stages of the disease, heart transplantation is necessary.
https://pixabay.com/illustrations/pill-capsule-medicine-medical-1884775/
Complications of extrasystole
- Atrial fibrillation;
- ventricular tachycardia;
- heart failure;
- threat of sudden death.
Forecast
The prognosis for functional extrasystoles is favorable. Malignant extrasystoles, if treated incorrectly and untimely, can lead to serious complications and sudden death.
Prevention
The basis for the prevention of all diseases is a healthy lifestyle.
This is a proper balanced diet, enriched with potassium and magnesium; giving up bad habits (smoking, drinking alcoholic beverages), strong tea, the ability to deal with stress.
Regular moderate physical activity and walks in the fresh air are beneficial. Control of blood sugar and cholesterol levels is also necessary.
https://pixabay.com/photos/a-change-in-lifestyle-banana-diet-1430599/
Conclusion
Treat your heart with care. Do not self-medicate. Any rhythm disturbances require an individual approach. Only a doctor will be able to find out the cause of extrasystole and determine the treatment that is right for you. The earlier treatment is started, the better the prognosis of the disease.
Literature
- Belenkov Yu. N., Oganov R. N. Cardiology. National leadership.//M., 2012 – 569 p.
- Belyalov F.I. Cardiac arrhythmias.// Irkutsk, 2014 – 182 p.
- Strutynsky A.V.
Electrocardiogram: analysis and interpretation//M., 2012- p.100. - Kiyakbaev G.K. Cardiac arrhythmias. Fundamentals of electrophysiology, diagnosis, treatment and modern recommendations.//M., 2014 – p. 99.
Article rating
We have put a lot of effort into making sure you can read this article and would welcome your feedback in the form of a rating. The author will be pleased to see that you were interested in this material. Thank you!
(1 5,00 of 5) Loading...
If you liked the article, share it with your friends!
You might be interested
Source: https://UstamiVrachey.ru/kardiologiya/ekstrasistoliya
Basic principles of treatment of extrasystole after eating
An attack of premature heart contractions during and after eating may not always be life-threatening for the patient: in some cases it is a physiological norm. To alleviate an attack of labile extrasystole, the patient needs to take a horizontal position and relax as much as possible. You should lie with the foot end of the bed elevated (for better blood flow to the heart). You can normalize the condition by drinking sweet tea, as well as doing self-massage.
In the treatment of extrasystoles, it is necessary to eliminate the root cause that caused the pathological process in the body. So, if the factor contributing to the development of attacks is coronary artery disease and other cardiogenic diseases, the specialist should prescribe drugs that relieve this condition.
The main principle of therapy for tachycardic extrasystoles is the use of sedative medications that reduce the heart rate and have a beneficial effect on the functioning of the organ. Such drugs include “Valerian”, “Motherwort”. The drugs “Novopasit” and “Persen” have a good effect.
In some cases, when severe attacks occur, a specialist may prescribe the use of tranquilizers Sebazon and Seduxen. Such drugs will help not only relieve stress, but also prevent vascular spasm - the main complication of the disease.
To stop an attack of a bradycardic type, the doctor has the right to prescribe the administration of atropine. This substance will normalize the heart rhythm, strengthening the work of the muscle wall.
In the treatment of extrasystole, it is important to mention adrenergic blockers. These drugs are prescribed by a doctor to slow down accelerated heart contractions, by dilating blood vessels, reducing myocardial excitation and lowering blood pressure.
When using drugs in this group, it is necessary to follow strict rules of dosage and time of administration in order to prevent the development of complications.
If the cause of intercalary systolic complexes is not associated with any cardiac pathology, you should think about the correctness of your diet and lifestyle. Fatty, spicy, fried, smoked foods are considered difficult to digest. Strong black tea or coffee, carbonated drinks, and alcohol are also not beneficial. Cigarettes are also not the best friend for the heart muscle. Low physical activity also does not contribute to the smooth functioning of the digestive organs. All this can cause heart rhythm disturbances. At first they will be one-time, but then they can develop into a permanent severe arrhythmia with all the ensuing consequences.
Even an ordinary daily half-hour walk in the open air will be useful for the normal movement of food through the gastrointestinal tract, and will also easily eliminate oxygen starvation of the myocardium.
Can extrasystole occur after eating and why?
Extrasystole, which debuts after eating, is distinguished by frequent heart contractions, causing severe discomfort to the patient. The mechanism of their occurrence is temporary myocardial hypoxia due to increased blood supply to the gastrointestinal tract. Extrasystoles after eating are divided into organic and functional, the provoking factors for which are presented in the table.
- myocarditis;
- myocardial infarction;
- stroke;
- cardiomyopathy.
- prolonged depression;
- stress;
- smoking;
- alcohol and drug use;
- systematic overeating;
- physical stress.
The causes of extrasystole during meals may be associated with professional sports, menstruation, and failure to comply with nighttime sleep patterns.
Extrasystole itself after eating does not pose a threat to life. But with pathologically altered heart structures and the absence of adequate treatment, the risk of its transformation into atrial fibrillation (atrial fibrillation) increases.
Heart rhythm disturbances are recorded after eating, including arrhythmia in the form of extrasystole, and during pregnancy. Its etiology lies in natural gestational modifications during this period associated with an increase in circulating blood volume and changes in hormonal levels.
Read also: Myocardial dystrophy
Extrasystole in pregnant women is associated with the following reasons:
- increased load on the heart;
- pressure of the pregnant uterus on the stomach;
- restless emotional state of a woman.
Functional extrasystoles do not aggravate the course of pregnancy and disappear after childbirth.
The influence of gastroesophageal reflux disease (GERD) on the occurrence of cardiac symptoms is now recognized, requiring a careful differential diagnosis. Heart rhythm disturbances in this pathology occur through viscerocardiac reflexes. Disorders of this origin are always neurogenic (functional) in nature.
Such arrhythmias are considered to resolve independently with remission of the provoking disease. The main difficulty is that GERD does not tend to cure, and rhythm disturbances with it are very variable.
Causes of rhythm disturbances
Normally, the appearance of sudden contractions of the heart is recorded from 10-20 to 100-250 times a day. Such data were obtained using Holter monitoring. Often, food intake is directly related to these deviations from the normal rhythm. The physiological reasons for the appearance of such a disorder as extrasystoles during or after meals are:
- drinking large amounts of alcohol;
- smoking;
- abuse of strong coffee or tea;
- taking energy drinks;
- experiences and fears;
- stressful situation;
- pregnancy (hormonal changes and pressure of the growing uterus on the mediastinal organs);
- consumption of fatty heavy foods;
- binge eating;
- weakness of the heart muscle due to physical inactivity.
Pathological causes of extrasystoles after eating may be associated with the following conditions or diseases:
- myocarditis;
- dystrophic changes in the heart muscle;
- cardiac failure;
- high pressure;
- impairment of kidney and liver function;
- reflux with the backflow of stomach contents into the esophagus;
- vascular diseases;
- conditions with electrolyte imbalance;
- intoxication or poisoning;
- irradiation;
- vegetative-vascular dystonia;
- dysfunction of the thyroid gland;
- hormonal changes (puberty, menopause).
The mechanism for the occurrence of extrasystole during a meal is the increased flow of oxygen to the stomach. At this moment, the heart experiences a lack of it, which leads to an intensification of the excitation process. If at the same time a person consumes little liquid in the form of pure water, then a relative thickening of the blood occurs, and the work of pumping it becomes more difficult. Compensatory mechanisms are forced to increase the frequency of myocardial contractions by increasing the excitation of conduction.
When the body begins the digestion process, the influence of the sympathetic nervous system decreases at this time. The pressure drops, the pulse becomes less frequent, and the activity of the cerebral cortex slows down. This is how vagal extrasystole develops. The mechanism of its appearance is accompanied by excitation of sections of the conduction system under the influence of temporary myocardial ischemia. It can be relieved with atropine or regular exercise.
Origin and classification of extrasystoles
By origin, extrasystoles are organic and functional. The former are a consequence of various cardiac pathologies. If extraordinary systoles are not associated with heart disease, they are classified as functional. The latter occur against the background of complete health of the body (idiopathic), or are a consequence of various conditions not related to the condition of the heart. The following pathologies and conditions can provoke the appearance of extrasystole:
- osteochondrosis;
- cardiopsychoneurosis;
- hormonal disorders (especially thyroid dysfunction);
- psycho-emotional stress and physical overload;
- disorders of salt metabolism (hypercalcemia, hypokalemia).
It has been proven that the use of certain pharmacological agents (osmotic diuretics, ephedrine, glucocorticoids, digitalis preparations (digitalis), tricyclic antidepressants) stimulate the occurrence of extrasystoles. Alcohol and caffeine-containing drinks (energy drinks, strong coffee and black tea) provoke extrasystole. Eating, especially large meals, also contributes to rhythm disturbances.
Depending on the part of the heart that contracts prematurely, extrasystoles are divided into three most common types:
- atrial;
- ventricular;
- atrioventricular (atrioventricular).
Extraordinary ventricular systoles occur most often (about 60%), 25% of recorded cases occur during atrial contractions, and atrioventricular extrasystole is observed less often than others (10%). The remaining 5% is distributed to rare and atypical mechanisms for the occurrence of extraordinary contractions (for example, when an extrasystole occurs simultaneously with a normal contraction of the heart muscle). After eating, during special studies, extraordinary contractions of the ventricles are predominantly recorded, and much less often - of the atria.
Types of extrasystole
Depending on the area in which the formation of ectopic foci of excitation occurs, ventricular extrasystoles, atrioventricular extrasystoles and atrial extrasystoles are determined. In addition, there are also some options for their combination. Exceptionally rare cases indicate that extraordinary impulses appear from the sinoatrial node, that is, from the physiological pacemaker.
In some cases, two simultaneous rhythms are noted, that is, sinus and extrasystolic rhythms, which is defined as parasystoles.
The next pair of extrasystoles are called paired, but if there are more than two, then the extrasystoles are called group (or volley).
They also distinguish between a rhythm in which normal systoles alternate with extrasystoles (that is, bigeminy), a rhythm in which two normal systoles alternate with an extrasystole (trigeminy) and a rhythm in which an extrasystole follows every third normal contraction. Regular repetition of bigeminy, trigeminy and quadrigeminy defines these conditions as allorhythmia.
Depending on the frequency of formation of extrasystoles, rare extrasystoles (up to 5 per 1 minute), medium extrasystoles (from 6 to 15 per 1 minute), as well as frequent extrasystoles (more than 15 times per minute) are determined. Depending on the number of ectopic foci that arise, extrasystoles with one foci (monotopic) and extrasystoles with several foci (polytopic) are determined.
Depending on the etiological factors, such types of extrasystoles are determined as functional extrasystoles, toxic extrasystoles and organic extrasystoles.
Functional extrasystoles
They represent disturbances in the rhythm of psychogenic (neurogenic) origin. They are associated with chemical exposure factors, alcohol and drug use, smoking, etc. Functional extrasystole is also recorded in patients diagnosed with vegetative dystonia, osteochondrosis, neuroses and other conditions.
As an example of the type of extrasystole under consideration, arrhythmia that occurs in trained and completely healthy individuals involved in sports can be noted. You can also note the frequency of development of functional extrasystole in women during the onset of menstruation. Functional extrasystoles are provoked, among other things, by stress and the consumption of strong drinks such as coffee and tea.
In the case of the development of functional extrasystole without any predisposing factors to it in healthy people, it is defined as idiopathic functional extrasystole.
Organic extrasystoles
The relevance of this type of extrasystole is determined by the damage that occurs in the myocardium, which occurs in particular in such conditions as myocardial infarction, coronary heart disease, myocarditis, cardiosclerosis, pericarditis, heart defects, myocardial damage due to sarcoidosis, hemochromatosis, amyloidosis, as well as during surgical interventions. In athletes, the formation of extrasystole can in some cases occur due to myocardial dystrophy, which is formed due to physical overexertion.
Treatment
To achieve a good therapeutic effect, you must adhere to a healthy diet and regimen.
Requirements that a patient suffering from cardiac pathology must comply with:
- give up nicotine, alcoholic beverages, strong tea and coffee;
- eat foods with a high concentration of potassium - potatoes, bananas, carrots, prunes, raisins, peanuts, walnuts, rye bread, oatmeal;
- in many cases, the doctor prescribes the drug “Panangin”, which contains “heart” microelements;
- give up physical training and hard work;
- during treatment, do not adhere to strict diets for weight loss;
- if the patient is faced with stress or has restless and intermittent sleep, then light sedatives (motherwort, lemon balm, peony tincture), as well as sedatives (valerian extract, Relanium) are recommended.
Medicines to restore rhythm
The treatment regimen is prescribed on an individual basis and depends entirely on morphological data, the frequency of arrhythmias and other concomitant cardiac diseases.
Antiarrhythmic drugs used in practice for PVCs are divided into the following categories:
- sodium channel blockers - “Novocainamide” (usually used for first aid), “Giluri”;
- beta-blockers - “Cordinorm”, “Carvedilol”, “Anaprilin”, “Atenolol”;
- potassium channel blockers - Amiodarone, Sotalol;
- calcium channel blockers - Amlodipine, Verapamil, Cinnarizine;
- if the patient’s extrasystole is accompanied by high blood pressure, then antihypertensive drugs are prescribed - “Enaprilin”, “Captopril”, “Ramipril”;
- to prevent blood clots - Aspirin, Clopidogrel.
A patient who has started treatment is recommended to have a control electrocardiogram after 2 months. If extrasystoles become rare or disappear altogether, then the therapeutic course is canceled. In cases where the result has improved slightly during treatment, treatment is continued for several more months. In the case of a malignant course of extrasystole, drugs are taken for life.
Surgical methods of treatment
Surgery is prescribed only in cases of ineffective drug therapy. Often this type of treatment is recommended for patients who have organic ventricular extrasystole.
Types of cardiac surgery:
- Radiofrequency ablation (RFA). A small catheter is inserted through a large vessel into the cavity of the heart (in our case, these are the lower chambers) and using radio waves, problem areas are cauterized. The search for the “operated” zone is determined using electrophysiological monitoring. The effectiveness of RFA in many cases is 75-90%.
- Installation of a pacemaker. The device is a box equipped with electronics, as well as a battery that lasts ten years. Electrodes extend from the pacemaker and are attached to the ventricle and atrium during surgery. They send electronic impulses that cause the myocardium to contract. The pacemaker essentially replaces the sinus node, which is responsible for rhythm. An electronic device allows the patient to get rid of extrasystole and return to a full life.
Complications of supraventricular extrasystole
Supraventricular extrasystole can provoke the development of supraventricular tachycardia, which is characterized by sudden onset and cessation of pathologically rapid cardiac activity. During an attack, the heart rate rises to 220-250 beats per minute. If at this moment it is possible to take an ECG, then a paroxysm (attack) of supraventricular tachycardia can be recorded.
One of the consequences of this disease can be atrial fibrillation (atrial fibrillation). These are chaotic and frequent excitations and contractions of the atria, as well as twitching of certain groups of atrial muscle fibers. During an attack, the heart rate increases significantly and the correct heart rhythm is disrupted. The risk of atrial fibrillation should serve as a criterion for the malignancy of supraventricular extrasystole (high risk of sudden death). A harbinger of atrial fibrillation is frequent group supraventricular extrasystole with episodes of paroxysmal (paroxysmal) supraventricular tachycardia.
Symptoms and treatment
Discomfort after eating manifests itself as follows:
- Dyspnea. It occurs because more oxygen is required by the gastrointestinal tract for digestion.
- Pain in the chest and a feeling that the heart is doing somersaults, turning over. stops - these are signals about extrasystole.
- Dizziness. It also occurs due to a lack of oxygen for the brain to function. One may note a decline in brain activity and a reluctance to perform complex intellectual work.
- Low blood pressure. At the time of digestion, a decrease in blood pressure can be diagnosed due to increased blood flow into the gastrointestinal tract.
It was previously noted that extrasystoles after eating are not always dangerous to health, as they are associated with physiological aspects of digestion. In such cases, do not resort to drug treatment.
But if a person is constantly bothered by the symptoms described above, then he tries to eliminate them. To do this, it is recommended to do the following:
- To refuse from bad habits.
- Eat a healthy diet (especially regarding fat content).
- Instead of strong coffee or black tea, drink green tea.
- Reduce physical activity.
It is recommended to take specialized dietary supplements, foods rich in potassium and magnesium, to support the functioning of the heart muscle.
If a patient has interruptions in the functioning of the heart due to overeating, then first aid can be provided to him in the following form. Prepare an infusion of plants that stabilize blood pressure and improve blood circulation. For example, it could be an equal combination of lemon balm, motherwort and mint. An infusion of these remedies will allow you to relax and relieve psychological and physiological stress.
You can also use valerian tincture and motherwort drops. These methods will help relieve stress and prevent spasm of blood vessels, which can aggravate the usual extrasystole after eating.
What else you can’t do after eating, watch the video. For example, in the evening after eating you can go to bed only 2 hours later.
Extrasystole after eating is a type of arrhythmia, which is characterized by extraordinary contractions of the heart or its individual parts. During such contractions, a person feels a dull push, a blow from inside the chest, and a short spasm. The heart seems to freeze for 2-3 seconds, and then resumes its function.
Stomach pain and extrasystoles
Rhythm disturbances are often associated with various diseases of the gastrointestinal tract, which in such cases act as the primary disease. Research in this direction has been ongoing for many years and today a clear connection has been identified between gastrointestinal disorders such as GERD and the cardiovascular system.
Arrhythmia is a rhythm disorder that can be asymptomatic and without threat to the patient’s life, or contribute to the development of dangerous conditions such as atrial and ventricular fibrillation. There are various reasons for the development of arrhythmia, and many of them are diseases of the gastrointestinal tract (GIT).
According to statistics, 10% of deaths in the United States are due to pathologies of the digestive system, which in such cases are the main cause of concomitant diseases. [1 - Peery AF, Dellon ES, Lund J, Crockett SD, McGowan CE, et al. (2012) Burden of gastrointestinal disease in the United States: 2012 update. Gastroenterology 143: 1179-1187]
Many of these patients have cardiovascular symptoms that appear to be related to their primary disorder. To make a correct diagnosis, the relationship between the cardiovascular and gastrointestinal systems is under intensive research.
: Polyps in the intestines; arrhythmia | Doctor Myasnikov “About the Most Important Thing”
Features of the connection between the heart and the gastrointestinal tract
In a normal state, an adult has from 60 to 90 beats/min. In children, the heart rate is slightly different, especially in the first months of life, when the pulse can reach 140 beats/min. Around the age of 18, heart function begins to correspond to adult norms.
When determining a rhythm disorder against the background of gastrointestinal pathologies, they speak of functional arrhythmias.
The pathogenesis of the development of functional arrhythmias lies in the interaction of all organs and systems of the body through the autonomic nervous system. Its tasks include monitoring the work of all internal organs. Since it consists of two main sections, which are in antagonistic action with each other, the heart and gastrointestinal tract are affected differently by nervous regulation.
Manifestations of the influence of the autonomic nervous system in accordance with the departments:
1. Sympathetic nervous system:
1.1 Heart - heartbeat increases, heart rate amplitude increases
1.2 Intestines - peristalsis is inhibited, the amount of digestive juices decreases, and the force of contraction of the anus increases.
2. Parasympathetic nervous system (vagus nerve):
2.1 Heart - heartbeat decreases, heart rate amplitude decreases
2.2 Intestines - peristalsis increases, the amount of digestive juices increases, the force of contraction of the anus decreases.
It is important to note that the sympathetic division of the nervous system is primarily active during the day, while the parasympathetic division is active at night.
Thus, it turns out that if a person has a gastrointestinal disease, the sympathetic part of the nervous system is excited due to constant pain or high temperature, which contributes to a reflex increase in amplitude and increase in heart rate. In such cases, in addition to the symptoms of the underlying gastrointestinal disease, a person may experience changes in the functioning of the heart.
The main forms of arrhythmia arising from gastrointestinal pathologies
The term “arrhythmia” refers to a group of diseases associated with heart rhythm disturbances. These disorders may differ in the mechanism of arrhythmia development, frequency and order of heart contractions. As already mentioned, with gastrointestinal diseases, functional arrhythmias most often develop, which in most cases take the form of:
- Tachycardia
- Extrasystoles
- Atrial fibrillation
People with inflammatory bowel disease (IBD) are 20% more likely to develop heart disease than the general population, with the risk being higher in women and people under 40, according to a study published in March 2014 by Clinical Gastroenterology and Hepatology.
Tachycardia is the definition of a heart rate above 90 beats/min (in an adult). In this case, the patient may feel other symptoms of the disorder:
- weakness;
- fatigue;
- dizziness;
- anxiety;
- tinnitus;
- feeling of palpitations or “heart jumping out of the chest”;
- chest pressure;
- change in skin color;
- nausea;
- cold extremities, etc.
Extrasystole is an extraordinary contraction, which can be single, paired, or group.
Their formation is due to the presence in the myocardium of an ectopic focus of excitation, which sends intermediate impulses that are not consistent with the main pacemaker - the sinus node.
With functional rhythm disorders, similar extraordinary contractions can also form, which is associated with periodic overexcitation of the autonomic nervous system and, accordingly, acceleration of the heart rate.
Gastroesophageal reflux disease and atrial fibrillation
Atrial fibrillation (AF) is the most common clinically significant arrhythmia in the general population, and gastroesophageal reflux disease (GERD) is the most diagnosed gastrointestinal disease in outpatient clinics in the United States and around the world. When no structural heart disease can be detected, the heart disease is called secondary, and careful evaluation of the patient may help identify other underlying conditions, including GERD.
Source: //ohansk-city.ru/bolit-zheludok-i-jekstrasistoly/
Causes
Extrasystole occurs for various reasons and therefore has various consequences. There are several groups of factors that increase the risk of arrhythmias.
Factors provoking extrasystole:
- Structural heart diseases: coronary heart disease, cardiomyopathy, pericarditis, heart failure, heart defects, heart attack, acute coronary syndromes, ventricular myocardial hypertrophy.
- Extracardiac diseases: defects of the respiratory system, digestive organs, thyroid gland, spine, systemic allergic reactions, neoplastic processes, electrolyte metabolism disorders, arterial hypertension.
- Toxic effects of certain groups of drugs, such as cardiac glycosides, tricyclic antidepressants, glucocorticosteroids, sypatolytics, diuretics. As well as the effect of thyrotoxicosis on the body, intoxication in infectious diseases.
- Reasons of a functional nature are daily stress, psycho-emotional and autonomic disorders, increased physical activity, abuse of alcohol, strong tea, coffee, smoking.
- Idiopathic causes are the spontaneous occurrence of disruptions in the normal heart rhythm of unexplained etiology for no apparent reason.
Symptoms of gastroesophageal reflux disease (GERD)
- Heartburn
- Belching of air or gastric contents (regurgitation), which increases in a horizontal position of the body, is one of the main signs of gastroesophageal reflux disease.
- Dysphagia – disturbances in the movement of food through the esophagus and associated discomfort
- Periodic nausea, discomfort in the chest
- Sore throat, dry cough, hoarseness, choking (due to irritation of the mucous membrane of the pharynx, larynx, esophagus by acidic gastric contents and irritation of the vagus nerve fibers)
- There may be pain in the heart area, palpitations, dizziness, and a feeling of weakness.
Types of extrasystoles
Extrasytolia after eating are usually divided into atrial, atrioventricular and ventricular types.
The development of these forms of the disease depends on the influence of the parasympathetic and sympathetic autonomic parts of the nervous system (NS). The influence of NS is key in the development of extrasystoles after eating. To a certain extent, changes in heart rhythm characterize the balance between parts of the autonomic nervous system.
When the balance is disturbed, the dominant influence of one of the sections of the NS is revealed, which, in turn, leads to the development of arrhythmias. In this regard, there are two types of extrasystoles:
- Bradycardic. Occurs with the dominant influence of the parasympathetic department. Arrhythmias can occur at rest and after eating. With physical activity, an upright position and the administration of atropine, the symptoms of extrasystole disappear.
- Tachycardic. Occurs under the dominant influence of the sympathetic division of the NS. After using antiarrhythmic drug therapy, this type of arrhythmia disappears.
From the point of view of theoretical and practical medicine, the greatest attention should be paid to ventricular extrasystole, since it is associated with a high risk of death. This is especially true when there is an underlying disease, in particular coronary heart disease (CHD)
Ventricular arrhythmia, which is not related to severe pathology of internal organs, has no prognostic significance and is often safe. There are two large groups of extrasystoles:
- benign or labile;
- life-threatening or stable.
Benign arrhythmias are represented by rare or frequent single extrasystoles, which become significantly smaller or disappear if physical activity is present. They are a sign of functional changes in the heart. The occurrence of such arrhythmias is usually not associated with concomitant cardiac or any other pathology. Such extrasystoles often develop during meals.
Extrasystole and pregnancy
Heart rhythm disturbances, in particular arrhythmia in the form of extrasystole, are a common pathology during pregnancy. Natural gestational changes in the body during this period cause hemodynamic, neurohumoral and electrophysiological fluctuations.
Atrial, atrioventricular and ventricular extrasystoles occur in approximately 20% of women. Of these 20%, in almost half of the cases functional reflex extraordinary contractile complexes are recorded after or during meals. Their reasons are:
- increased load on the heart;
- the influence of the growing uterus, squeezing the stomach;
- constant fear of the upcoming birth in recent months.
The absence of organic heart damage in the presence of this type of arrhythmia does not require treatment and does not significantly affect pregnancy.
Emotional excitement at any stage contributes to the appearance of extrasystole. Symptoms usually go away after delivery.
Of all types of arrhythmia, extrasystole is the most common, although it is not always recorded. Rare and one-time manifestations of such disorders are not dangerous; they can be considered a variant of the norm. Still, if you notice symptoms of extraordinary myocardial contractions after eating, you should consult a doctor so that labile arrhythmia does not cause the development of a more serious pathology of the cardiovascular system.
Traditional methods of treatment
Is it possible to help yourself if you are diagnosed with extrasystole? Traditional treatment is possible, and herbalists offer a huge number of recipes.
- You can adjust your heart rhythm using a regular infusion of valerian root (it can be purchased at the pharmacy). This remedy is most effective if the extrasystole is neurogenic and caused by stress.
- Good results can be achieved using a decoction of blue cornflowers. The flowers of this plant (about a teaspoon) should be poured with a glass of boiling water. Close the container, let it brew, and then strain. You need to take a quarter glass three times a day (it is better to drink the decoction 15 minutes before meals).
- Calendula infusion will also help cope with heart rhythm disturbances. A tablespoon of dry herb should be poured with two glasses of boiling water, cover with a lid and leave for an hour. After the mixture has infused, you need to strain it. It is recommended to drink 100 ml four times a day.
- Alcohol tincture of hawthorn also helps with extrasystole. You can buy it at the pharmacy or prepare it yourself.
Of course, you should not use the above-mentioned medications without permission. First, be sure to consult with your doctor - a specialist will help you choose the appropriate medications and the appropriate dosage.
Categories and risks
Currently, VES is most often detected in people over fifty years of age. On average, according to medical statistics, this age group accounts for from half of all patients with PVC to 75% of cases.
A classification system has been developed that allows dividing all patients into several groups. This simplifies the selection of the optimal treatment format. One of the well-known and popular systems is called RYAN. Ventricular extrasystole according to this categorization involves the identification of mono-, polymorphic cases of paired, as well as three or more impulses initiated at the stage of atrium rest
If you pay attention to the qualification according to Lown, then such cases belong to categories 4A, 4B, 5. The current gradation of ventricular extrasystole according to RYAN involves assessing the source of impulse initiation
If there is only one of these, they speak of a monomorphic form; a polymorphic form is identified if there are several foci of impulse emission.
Another case classification system was named after its developer, Dr. Mayerburg, a distinguished author and cardiologist. He proposed dividing all cases according to frequency into very rarely manifested, rarely noticeable and infrequently noticeable. It was also proposed to distinguish between the level of moderate rarity, frequent cases and very frequent cases. Additional classification according to Mayerburg involves assessing the type of violation: single or paired, poly- or monomorphic, stable or without such a feature.
Diagnosis of reflux esophagitis
- Analysis of complaints, clinical manifestations of gastroesophageal reflux disease
- A simple test can be performed on an outpatient basis, which consists of taking omeprazole 40 mg per day daily for 5 days. If the patient's condition improves significantly, this indicates the possible presence of gastroesophageal reflux disease.
- Fibroesophagogastroduodenoscopy (FEGDS) is the main method for diagnosing reflux esophagitis (if there are changes in the esophageal mucosa, a biopsy is performed)
- X-ray, computed tomography of the esophagus
- If necessary, esophageal manometry, pH-metry and other studies can be additionally performed
Classification
Types of extrasystole (criterion – place of formation of ectopic foci):
- ventricular;
- atrial;
- atrioventricular;
- various combinations of the above extrasystoles.
Sometimes (no more than 0.2% of the total) extraordinary impulses come from the sinoatrial node.
The focus of the ectopic rhythm can function independently of the main (sinus) rhythm - this phenomenon is called parasystole.
Another classification of extrasystole (criterion - time of occurrence of arrhythmia on the electrocardiogram):
- early;
- average;
- late.
By frequency of occurrence:
- rare (single) (less than 5/minute);
- medium (multiple) (5–15/minute);
- frequent extrasystole (group) (more than 15/minute);
- steam room (two in a row).
By nature (etiology), there are also several types of extrasystole:
- organic;
- functional;
- toxic origin.
The most dangerous type of arrhythmia - ventricular - is usually divided into 5 classes (determined only after a 24-hour ECG):
- I – transient extrasystoles are not registered.
- II – up to 30 monotopic extraordinary impulses are recorded in 60 minutes.
- III – 30 or more extrasystoles per hour (time of day is not taken into account).
- IV – both mono- and polytopic impulses are noted (subclass “a” – paired ventricular extrasystoles are present, subclass “b” – runs of ventricular tachycardia).
- V – early ventricular extrasystoles.
There are also the following types of ventricular arrhythmia:
- benign (not associated with the risk of cardiac arrest, the muscle is not damaged);
- potentially malignant (it is accompanied by problems with blood circulation, as well as organic damage to the myocardium);
- malignant (numerous extrasystoles, significant probability of patient death).
What treatment regimen can modern medicine offer?
What should a patient do if an extrasystole is detected? Treatment in this case directly depends on the causes of extraordinary heart contractions. If the extrasystoles are isolated and do not pose a particular threat, then therapy may not be required at all.
In cases of neurogenic extrasystole, patients are prescribed sedatives and tranquilizers. Patients are also advised to give up bad habits, temporarily reduce physical activity, monitor their diet more carefully and, of course, undergo regular medical examinations.
If cardiac arrhythmias are associated with the use of certain drugs, then they must be urgently discontinued and safer drugs must be selected.
Therapy for extrasystole that occurs against the background of diseases of the digestive, nervous, and endocrine systems comes down to the treatment of the underlying diseases. Sometimes patients are also prescribed antiarrhythmic drugs. Such products as Amiodarone, Cordarone, and Novocainamide are considered good. The dosage and schedule of administration are determined individually.
The most dangerous is the ventricular form of extrasystole if the daily frequency of extraordinary heart contractions reaches 20–30 thousand. If antiarrhythmic therapy does not relieve symptoms, then surgery is performed.
Possible consequences of the disease
This condition can be dangerous only if it has become a sign of other serious diseases, both cardiac and non-cardiac.
If attacks become more frequent and haunt the patient even for no apparent reason, there is a threat to life as a result of serious complications - tachycardia, fibrillation, cardiac arrest. Increased excitability of a person and a feeling of fear during extraordinary contractions of the myocardium can contribute to the occurrence of panic attacks, as well as the appearance of a hypotensive crisis.
When cases become more frequent, it is important to quickly undergo a full examination by a specialist who can accurately determine the root cause and prescribe medications to alleviate the condition and treat concomitant pathologies.
It is important to carefully monitor your health. After all, even a seemingly minor disease can cause irreparable damage and change a person’s life forever.