An electrocardiograph (ECG) is a device for assessing the electrical activity of the heart muscle. In cardiology, it is most in demand, as it allows you to detect any changes in the heartbeat, organic lesions and electrolyte imbalances. When interpreting the cardiogram, sinus rhythm is detected in the absence of pathological abnormalities. An experienced specialist evaluates the final results. To an ordinary person, Latin letters and curved lines will not say anything. Generally accepted standards and definitions will help you figure out the decoding yourself.
Sinus rhythm on a cardiac cardiogram - what is it?
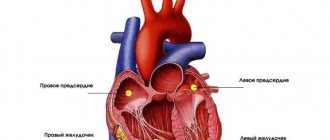
The sinus rhythm detected on the electrocardiogram is displayed by identical teeth at equal intervals of time and indicates the correct functioning of the heart. The source of impulses is set by the natural pacemaker, the sinus (sinusoidal) node. It is localized in the angle of the right atrium and serves to generate signals that cause sections of the heart muscle to contract one by one.
A feature of the sinus node is its abundant blood supply. The number of impulses it sends is influenced by the divisions (sympathetic, parasympathetic) of the autonomic nervous system. If there is a malfunction in their balance, the rhythm is disturbed, which is manifested by an increase in heart rate (tachycardia) or slowdown (bradycardia).
Normally, the number of pulses generated should not exceed 60-80 per minute.
Maintaining sinus rhythm is important for stable circulation. Under the influence of external and internal factors, disruption of the regulation or conduction of impulses may occur, which will lead to disruptions in hemodynamics and dysfunction of internal organs. Against this background, the development of signal blockade or weakening of the sinusoidal node is possible. On the electrocardiogram, the resulting disorder is displayed as the presence of a focus of replacement (ectopic) impulses in a certain part of the heart muscle:
- atrioventricular node;
- atria;
- ventricles.
When the signal source is located anywhere other than the sinus node, we are talking about heart pathology. The patient will have to undergo a series of examinations (24-hour ECG monitoring, stress tests, ultrasound) to identify the causative factor of the disorder. Treatment will be aimed at eliminating it and restoring sinus rhythm.
What do heart rate indicators mean?
Heart rhythm is the main indicator of heart function; thanks to it, it is possible to determine the presence of a particular organ pathology. Rhythm is determined by the frequency of contractions of the heart muscle (HR) at certain time intervals.
Normally, the heart muscle contracts equally, with sequential contraction and relaxation occurring at equal intervals. If the duration of several cycles becomes different, a heart rhythm disturbance is determined.
Impulses arising in the sinus node (Keith-Fluck node) are transmitted to myocytes, thereby causing them to contract and then relax. Due to the high ability of muscle cells to contract, impulses affect the entire heart, causing it to contract rhythmically and pump blood.
Decoding the cardiogram of the heart: sinus rhythm
Panic when a “sinus rhythm” recording is detected is typical for people unfamiliar with medical terms. Usually the cardiologist prescribes a series of examinations, so you will be able to see him again only after receiving all the results. The patient can only wait patiently and familiarize himself with publicly available sources of information.
In fact, sinus rhythm is the generally accepted norm, therefore, there is no point in worrying. Deviations are possible only in heart rate (HR). It is affected by various physiological factors, the influence of the vagus nerve and autonomic failures. The number of heart beats per minute may become higher or lower than normal for age, despite sending signals from the natural pacemaker.
A diagnosis of “tachycardia” or “bradycardia” of sinus type is made only after a comprehensive assessment of all the nuances. The doctor will pay attention to the patient’s condition and ask about the actions performed immediately before the study. If the decrease or increase in heart rate is insignificant and is associated with the influence of external factors, then the procedure will be repeated a little later or on another day.
Identification of the natural pacemaker during electrocardiography occurs according to generally accepted criteria:
- the presence of a positive P wave in the second lead;
- there is an equal interval between the P and Q waves, not exceeding 0.2 seconds;
- negative P wave in lead aVR.
If the transcript indicates that the patient has sinus rhythm and a normal position of the electrical axis of the heart (EOS), then they are afraid of nothing. The rhythm is set by its natural driver, that is, it comes from the sinus node into the atria, and then into the atrioventricular node and ventricles, causing alternate contractions.
Respiratory and non-respiratory types
Sinus arrhythmia in children is also divided into two types:
- respiratory;
- non-respiratory.
Respiratory arrhythmia , as the name implies, is associated with breathing - the heart rate involuntarily increases during inhalation, and decreases when exhaling.
If, for example, during an ECG, a child is placed on a couch with cool oilcloth, he will reflexively hold his breath, which will lead to a reduction in heart rate. This condition is not dangerous for children, as it does not create problems in the heart pumping blood.
Non-respiratory arrhythmia is caused by disturbances in the conduction system of the heart. Impulses occur in the sinus node at the correct frequency, but as they travel through the cardiocytes (muscle cells of the heart), problems arise that lead to arrhythmia. Such changes are usually transient, and they are not always associated with heart disease, but possibly with diseases of other systems or organs. Non-respiratory arrhythmia can be constant or paroxysmal - from a couple of attacks per year to several per day.
Acceptable standards
Whether the cardiogram readings are normal can be determined by the position of the teeth. Heart rhythm is assessed by the interval between the RR waves. They are the highest and should normally be the same. A slight deviation is acceptable, but not more than 10%. Otherwise, we are talking about a slowdown or increase in heart rate.
The following criteria are typical for a healthy adult:
- PQ interval varies within 0.12-0.2 seconds;
- Heart rate is 60-80 beats per minute;
- the distance between the Q and S teeth remains in the range from 0.06 to 0.1 sec;
- the P wave is 0.1 sec;
- The QT interval varies from 0.4 to 0.45 seconds.
In children, the indicators are slightly different from adults, which is due to the characteristics of the child’s body:
- QRS interval does not exceed 0.1 second;
- Heart rate varies depending on age;
- the distance between the Q and T teeth is no more than 0.4 seconds;
- PQ interval 0.2 sec.
- the P wave does not exceed 0.1 sec.
In adults, as in children, in the absence of pathologies, there should be a normal position of the electrical axis of the heart and sinus rhythm. You can see the permissible frequency of reductions by age in the table:
| Age | Number of contractions in 1 minute (minimum/maximum) |
| Up to 30 days | 120-160 |
| 1-6 months | 110-152 |
| 6-12 months | 100-148 |
| 1-2 years | 95-145 |
| 2-4 years | 92-139 |
| 4-8 years | 80-120 |
| 8-12 years | 65-110 |
| 12-16 years old | 70-100 |
| 20 years and older | 60-80 |
Normal indicators
Heart rates are not the same in children and adults. In children under one year old, it ranges from 140 to 160 beats per minute. With age, heart rate decreases; by the age of 15, healthy rates reach 60-90 beats and are equal to the norm for an adult.
In older people over 70 years of age, it is closer to the upper limit of normal, which is associated with age-related changes in the heart. Women's pulse is 6-8 beats less than men's.
The pulse rate may differ from the norm, but is not considered a pathology:
- in pregnant women - the heart adapts to the increased load, thus providing the mother and growing fetus with oxygen, the pulse may be slightly increased;
- in people who exercise daily and lead an active lifestyle, the heart works in economy mode, the heart rate is near the lower limit of normal;
- In professional athletes, at rest the heart can contract at a frequency of 45-50 beats.
If a person does not belong to one of these categories, then any pronounced deviation of heart rate from the norm requires identification of the cause and treatment.
Reasons for deviation from the norm
Heart rate varies depending on the time of day, psycho-emotional state and other external and internal factors. To obtain reliable data, you will need to take into account many nuances:
| Factor | Influence |
| Equipment malfunction | Any technical glitches will distort the results |
| Inrush currents | Occur due to insufficient adherence of the electrodes to the patient’s skin |
| Trembling muscle tissue | Will appear on the electrocardiogram as asymmetrical oscillations |
| Insufficiently prepared surface for attaching electrodes | Poorly cleansed skin from creams and other external products or the presence of thick hair can cause incomplete adhesion of the electrodes |
| Medical errors | Incorrectly joined diagrams or cutting them in the wrong place will lead to a loss of the complete picture of the heart's function. |
Equally important is careful preparation for the procedure:
- It is prohibited to consume alcohol and drugs a couple of days before the ECG.
- It is better to forget about smoking, coffee and energy drinks on the day of the procedure.
- Immediately a couple of hours before the examination, it is not recommended to transfer, stay in stressful situations and become overtired.
If you were unable to follow all the rules, then upon arrival at the diagnostic room you should tell the specialist about it. He will take this nuance into account and, if necessary, schedule an examination for another day.
A general list of factors that can affect the frequency and rhythm of the heart rhythm is as follows:
- mental disorders;
- overwork (psycho-emotional, physical);
- developmental defects (congenital, acquired);
- taking medications with antiarrhythmic effect;
- disruption of the valve apparatus (insufficiency, prolapse);
- dysfunction of the endocrine glands;
- advanced stage of heart failure;
- pathological changes in the myocardium;
- inflammatory heart diseases.
The use of medications, especially for stabilizing blood pressure (Mexari) and improving metabolic processes (Metonate, Adenosine), must be reported before the procedure. Many heart medications can slightly distort the results.
Causes and risk factors
Arrhythmia is caused by cardiac dysfunction:
- Malfunctions in the system that conducts impulses. Violations may relate to the rate of formation and conduction of the impulse.
- Irregular structure of the heart. If abnormalities interfere with normal contraction of the heart muscle.
- Disorders of the autonomic nervous system.
Also, an abnormal heart rhythm may be one of the manifestations of the disease:
- congenital or acquired heart disease;
- inflammatory heart diseases;
- severe intoxication of the body (including drugs);
- neoplasms (benign or malignant tumors);
- severe cases of infectious or viral diseases;
- nervous tension and stress;
- disruptions during embryonic development;
- hereditary diseases;
- dehydration of the body;
- excessive physical activity, especially against the background of vitamin deficiency or general weakness.
Temporary disruptions in heart rhythm cause hormonal surges as a result of strong emotions.
In childhood and adolescence, there are several periods when the risk of arrhythmia is increased due to physiological characteristics:
- Infants from 4 to 8 months;
- preschool children from 4 to 5 years old;
- junior schoolchildren from 6 to 8 years old;
- teenagers from 12 years old.
During these periods, it is better to conduct an ECG (electrocardiography) and visit a cardiologist. You can read about deciphering ECG in children in a separate article.
Features of deciphering an electrocardiogram
Based on the electrocardiogram, the cardiologist will be able to assess the electrical potential of the heart muscle during systole (contraction) and diastole (relaxation). Displays data in 12 curves. Each of them demonstrates the passage of an impulse through a specific part of the heart. Waveforms are recorded on 12 leads:
- 6 leads on the arms and legs designed to assess vibrations in the frontal plane.
- 6 leads in the chest area for recording potentials in the horizontal plane.
Each curve has its own elements:
- The teeth in appearance resemble bulges directed up and down. They are designated by Latin letters.
- Segments are the distance between several teeth located nearby.
- An interval is a gap consisting of several teeth or segments.
General principles of decoding
Evaluating the electrocardiogram is a complex process. The doctor carries it out step by step so as not to miss the slightest changes:
| Stage name | Description |
| Determination of the rhythm of contractions | Sinus rhythm is characterized by an equal distance between the R waves. If differences are detected when measuring the intervals, then we are talking about arrhythmia |
| Heart rate measurement | The doctor counts all the cells between the adjacent R waves. Normally, the heart rate should not exceed 60-80 beats per minute |
| Identifying the pacemaker | The doctor, focusing on the overall picture, looks for the source of the signals that cause the heart to contract. Particular attention is paid to the P wave, which is responsible for atrial contraction. In the absence of pathologies, the natural pacemaker is the sinus node. Detection of ectopic signals in the atria, atrioventricular node and ventricles indicates conduction failures |
| Conductor System Assessment | Impaired impulse conduction is detected by the length of the teeth and certain segments, focusing on acceptable standards |
| Study of the electrical axis of the heart muscle | It is generally accepted that the EOS in thin people has a vertical location. If you are overweight, horizontal. If the displacement is noticeable, the doctor will suspect the presence of pathology. A simple way to determine it is to study the amplitude of the R wave in 3 basic leads. The normal position is detected at the largest interval in the second lead. If it is 1 or 3, then the patient’s axis is shifted to the right or left. |
| Detailed study of all curve elements | If the ECG machine is old, then the doctor records the length of intervals, waves and segments manually. New devices do everything automatically. The doctor remains to evaluate the final results |
| Writing a conclusion | After the diagnosis, the patient needs to wait a little and pick up the report. In it, the doctor will describe the rhythm, its source, contraction frequency, and the position of the electrical axis. If deviations are detected (arrhythmias, blockades, changes in the myocardium, overload of individual chambers), then they will also be written about |
To better understand the information, it is advisable to familiarize yourself with various options for expert opinions:
- A healthy person is characterized by sinus rhythm, 60-80 heartbeats per minute, EOS in a normal position and the absence of pathologies.
- With an increased or decreased heart rate, sinus tachycardia or bradycardia is indicated in conclusion. The patient will be advised to undergo several more examinations or repeat the procedure on another day if the result was influenced by external factors.
- In elderly patients and people who do not lead a healthy lifestyle, pathological changes in the myocardium of a diffuse or metabolic nature are often detected.
- A record of the presence of nonspecific changes in the ST-T interval indicates the need for additional examinations. In this case, it is not possible to find out the true cause only with the help of electrocardiography.
- The detected repolarization disorder indicates incomplete recovery of the ventricles after contraction. Usually, various pathologies and hormonal imbalances affect the process. To detect them, several more examinations will be required.
For the most part, the conclusions are positive. Changes can be overcome with lifestyle changes and medications. An unfavorable prognosis is usually when coronary artery disease, proliferation (hypertrophy) of the chambers of the heart muscle, arrhythmia and failures in the conduction of impulses are detected.
How to recognize sinus arrhythmia in a child
You and your child may not be aware that they have a heart rhythm disorder. Often sinus arrhythmia is discovered by chance, as happened with my patient.
According to the classification of O.A. Kozyrev and R.S. Bogacheva in 1998, according to the clinical course, heart rhythm disturbances are divided into:
- insignificant;
- significant.
The first ones “do not bother” the patient. The general condition does not suffer, there are no complaints or clinical symptoms. The latter significantly complicate life and have an unfavorable prognostic value. This group of arrhythmias requires careful examination and timely treatment.
Complaints and symptoms, or when it’s time to see a doctor
The child may have complaints of a feeling of “interruptions” in the heart area, unexplained weakness, and dizziness. It is important to understand that preschoolers will not always describe their condition. If you suddenly notice that your baby, who usually runs, sits down to rest, or is experiencing unreasonable fatigue, immediately take him to the pediatrician. This will help you not to miss time in case of any illness.
The doctor will suspect sinus arrhythmia on auscultation if he hears different lengths of pauses between heart sounds. The pulse will correspond to age, but will be characterized by inconstancy: within one minute, too rapid repetition of beats will be replaced by a slow pace.
ECG signs
The main diagnostic method for rhythm disturbances is electrocardiography. An ECG allows you to clarify the type of change in automatism, conductivity, and identify non-physiological foci of excitation.
Sinus arrhythmia is characterized by:
- constancy of the P wave;
- a gradual increase in the distances between neighboring P or T, and then the same gradual decrease;
- stability of the PQ interval;
- normal EGC curve if you ask the patient to hold his breath.
With Holter monitoring, pronounced sinus arrhythmia in a child will be observed during sleep and physical activity. It is under these conditions that the activity of the vagus increases.
Causes of deviations in sinus rhythm
Abnormal sinus rhythm appears under the influence of pathologies or physiological factors. The forms of failure differ depending on the frequency and rhythm of contractions:
- sinus arrhythmia;
- sinus bradycardia;
- sinus tachycardia.
Despite the correct source of signals, the problem that has arisen must be dealt with. If no action is taken, a more severe form of arrhythmia may develop and dangerous symptoms of hemodynamic disturbances may appear.
Sinus tachycardia
The sinus form of tachycardia can be pathological or physiological. In the first case, it occurs due to other diseases, and in the second, after stress and overwork. The electrocardiogram usually reveals an increased frequency of contractions from 100 to 220 per minute and a short P-P interval.
The following symptoms are characteristic of an attack of sinus tachycardia:
- feeling of heartbeat;
- lack of air;
- general weakness;
- dizziness;
- sleep disturbance;
- chest pain;
- noise in ears.
Sinus bradycardia
Attacks of sinus bradycardia, like tachycardia, occur as a symptom of other diseases or as a reaction to physiological factors. They are characterized by a decrease in heart rate to 60 beats per minute or less. The electrocardiogram shows a noticeable increase in the distance between the P-P waves.
In addition to a slow heartbeat, during an attack of bradycardia the following symptoms appear:
- dizziness;
- fainting state;
- pain in the heart area;
- pale skin;
- tinnitus;
- fast fatiguability.
Sinus arrhythmia
The sinus variety of arrhythmia usually results in an irregular rhythm. The heart rate can increase or decrease sharply under the influence of various stimuli. The length of the P-P interval varies.
An attack of sinus arrhythmia is characterized by the following symptoms:
- feeling of fading and heart failure;
- change in skin color (blueness, redness);
- feeling of lack of air;
- panic attacks;
- pain in the heart area;
- tremor of the limbs;
- faintness or loss of consciousness.
What affects heart contractions?
When a doctor deciphers data, he takes into account not only what value he sees on paper, but also the patient’s lifestyle. Negatively affects cardiac activity:
- stress,
- smoking,
- alcohol consumption,
- taking antiarrhythmic drugs,
- physical overload.
Often the situation normalizes when a person finds himself in a calm environment. More than half of heart rate problems go away after stress relief. As a percentage, this figure is 62%. It is important to understand that due to busy work, most patients feel discomfort. Regardless of the reasons, if there are clear signs of a disorder, it is recommended to visit a doctor.
The number of beats per minute also depends on age. So, for children the norm may be 160 beats per minute, while for adults (over 12) this figure should be 75 beats per minute.
Sometimes, to clarify the details of the rhythm, doctors prescribe a daily study. In this case, sensors and a memory device are attached to the patient, which he must wear all day. This allows you to track the behavior of the heart muscle throughout the day under different conditions.
Features of ECG interpretation in children
Electrocardiography is performed in children in the same way as in adults. Problems can only arise with hyperactive kids. They must first be reassured and the importance of the procedure explained. The results obtained differ only in heart rate. During active growth, the heart has to work harder to supply all tissues of the body in full. As the child develops, the heartbeat gradually returns to normal.
Signs of sinus rhythm in children are similar to adults. The increase in heart rate must be within the acceptable age limit. If a focus of ectopic impulses is detected, then we can talk about a congenital malformation of the heart. It can only be completely removed through surgery.
Cases of mild sinus arrhythmia are most often associated with the respiratory system. During inhalation, the heart rate increases and stabilizes as you exhale. Such failures are typical for children and go away over time. When conducting an ECG, respiratory arrhythmia must be taken into account, since a cold couch, fear and other factors provoke its aggravation.
The sinus form of arrhythmia can be provoked by more dangerous causes:
- hypoxia that occurred in the womb;
- high pressure inside the skull, detected immediately after birth;
- rheumatism;
- myocarditis;
- infectious diseases;
- heart defects.
Due to the voiced pathological processes, the likelihood of developing complications that can lead to death and disability increases. Less severe causes include active growth, rickets and vegetative-vascular dystonia. In most cases, they go away on their own. It is enough for parents to give their child vitamin complexes and diversify his diet.
Treatment
It is not rhythm disturbance that requires therapy, it is a symptomatic measure. The basis is the elimination of the underlying pathological process.
The etiotropic approach simultaneously solves another problem - the prevention of complications and progression of the disorder.
Irregular rhythm requires conservative care, using groups of drugs.
Since the list of causes is huge, it is impossible to thoroughly describe all treatment options. There would be enough information for many scientific studies.
In short:
- Endocrine pathologies are eliminated by diet and hormone replacement therapy.
- Functional disorders of the heart require the use of glycosides (Digoxin), antiarrhythmics (Quinidine or Amiodarone, but with caution).
- Hypertension involves taking special groups of medications: ACE inhibitors (Perindopril, Prestarium), beta blockers (Metoprolol, Carvedilol), calcium antagonists (Diltiazem), centrally acting agents (Moxonidine), and mild diuretics (Veroshpiron and its analogues).
- Neurological functional disorders require the prescription of cerebrovascular (Piracetam, Actovegin) and/or nootropic mixed drugs (Cavinton, Vestibo, Glycine).
As part of stopping the attack of tachycardia itself, beta blockers are used. Anaprilin is ideal for these purposes (in the amount of a quarter or half of a tablet, a whole tablet is taken in exceptional cases).
Surgery is required when dangerous heart defects are detected. Prosthetics are performed on damaged areas (more often than other methods), plastic, and restoration of the anatomical integrity of tissues.
In case of vascular anomalies, stenting and ballooning (mechanical expansion of the lumen) are possible.
If excessive electrical activity of the heart develops due to the formation of excess conductive fibers, radiofrequency ablation (cauterization) of the altered lesion is performed.
This is a minimally invasive intervention with virtually no complications.
Dangerous types of disorders such as group extrasytolia, atrial fibrillation, fibrillation and flutter require the installation of a pacemaker, which itself sets the correct rhythm.
In the future, cardioprotectors must be used. Riboxin or Mildronate to normalize metabolic processes in the heart.
Universal recommendations for patients during and after treatment are to stop smoking, alcohol, and unauthorized use of any medications, avoid stress, get proper rest (at least 7 hours per night), and adhere to adequate physical activity (hiking and swimming, no more).
Also adjust your diet. Less animal fat, more plant foods. But there should not be a complete refusal, so as not to encounter protein deficiency.
Attention:
A vegetarian diet requires a certain level of health and is absolutely not suitable for a person with heart problems.
Decoding the electrocardiogram during pregnancy
During pregnancy, significant changes occur in a woman’s body that affect the results of electrocardiography:
- An increase in circulating blood volume contributes to the development of tachycardia and the manifestation of signs of overload in certain parts of the heart muscle.
- The growing uterus provokes displacement of internal organs, which is manifested by a change in the location of the electrical axis of the heart.
- Hormonal surges affect all systems in the body, especially the nervous and cardiovascular systems. A woman experiences attacks of tachycardia after any physical exertion. Heart rate usually increases by no more than 10-20 beats per minute from normal.
The changes that occur go away on their own after the birth of the child, but in some cases they develop into a full-fledged pathological process. To prevent it, it is necessary to be observed by a doctor throughout the entire pregnancy.
Dangerous and non-hazardous forms
Depending on the cause, heart rhythm failure is classified as respiratory, functional or organic.
Respiratory
The respiratory form is considered the most harmless type of the disease . It is expressed in increased heart rate when inhaling and decreased when exhaling.
A common cause is the immaturity of the baby’s nervous system. Heart rhythm disturbances go away with age, but you need to see a doctor so as not to miss possible complications.
Pathological causes of respiratory sinus arrhythmia include:
- increased intracranial pressure;
- brain damage of a non-inflammatory nature in infants, which is caused by oxygen starvation of the fetus during intrauterine development;
- immaturity of the child’s body as a result of premature birth;
- metabolic disorders in the body, rickets.
Functional
The functional form is less common than the respiratory form, but is also rarely dangerous . The cause may be disturbances in the functioning of the nervous, immune, and endocrine systems. It occurs as a consequence of an infectious or viral disease or as a manifestation of thyroid disease.
After eliminating the cause, the arrhythmia goes away.
Organic
The organic form is the most dangerous . Indicates pathological malfunctions in the impulse conducting system and other disturbances in the functioning of the heart.
This form is characterized by pronounced symptoms of arrhythmia. The condition requires immediate examination and long-term treatment.
The meaning of letters and numbers on an electrocardiogram
The definitions of the Latin letters that label the teeth will help you understand what is being said in the electrocardiogram:
| Name | Description |
| Q | Shows the degree of excitation of the left septum. ¼ of the length of the R wave is allowed. Exceeding the norm may indicate the development of necrotic changes in the myocardium |
| R | Visualizes the activity of all ventricular walls. Must be shown on all curves. If at least 1 is absent, there is a possibility of ventricular hypertrophy |
| S | Displays the moment of excitation of the ventricles and the partition between them. Normally, it should be negative and amount to 1/3 of the length of the R wave. The duration varies from 0.02 to 0.03 seconds. Exceeding the permissible limit indicates intraventricular blockade |
| P | Shows the moment of atrial excitation. Located above the isoline. The length does not exceed 0.1 seconds. The amplitude varies from 1.5 to 2.5 mm. With hypertrophy of the right atrium, characteristic of “pulmonary heart”, the P wave increases and acquires a pointed end. The growth of the left atrium is manifested by the splitting of its apex into 2 parts |
| T | Detected positive on the first 2 lines. The VR lead is negative. Too sharp apex at the T wave is characteristic of excessive levels of potassium in the body. If there is a shortage of an element, it is flat and long |
| U | Appears in rare cases near the T wave. Shows the degree of excitation of the ventricles after contraction |
It is equally important to find out the meaning of certain segments and intervals:
- The PQ interval shows how long it takes for an electrical impulse to travel through the heart muscle (from the atria to the ventricles). In the absence of irritating factors, the length does not exceed 0.2 seconds. Based on this indicator, the doctor will assess the general condition of the conduction system. If there is a lengthening of the distance between the P and Q waves, then the problem may be the development of heart block.
- Based on the space between the RR teeth, the doctor will determine the regularity of contractions and count them.
- The QRS complex helps you see how the signal is conducted through the ventricles.
- The segment between the S and T waves shows the moment the excitation wave passes through the ventricles. Its permissible length is 0.1-0.2 seconds. The segment is located on an isoline. If it is slightly displaced, then certain pathological processes can be suspected: higher by 1 mm or more – myocardial infarction;
- lower by 0.5 or more – ischemic disease;
- saddle-shaped segment – pericarditis.
It will not be easy for an ordinary person to decipher an electrocardiogram. First, you will have to familiarize yourself with the definition of the Latin symbols that indicate the teeth, and the features of the intervals between them. Then you need to study the types of heart rhythm and generally accepted heart rate norms. Finally, it is advisable to review the options for expert opinions and the general principles of decoding. Based on the information studied, even a person far from medicine will be able to understand the cardiogram.
Possible complications and prevention
Why is childhood SA dangerous? Sinus respiratory arrhythmia does not pose any threat to the child’s health. Typically, such failures of the cardiac system cause children to hold their breath instinctively. But severe or moderate SA, independent of breathing, is not a physiological variant of the norm; it is a clear symptom of disturbances in the functioning of the heart, endocrine system or other body functions. Such sinus arrhythmia in children is a reason for an immediate visit to a cardiologist. Thus, severe SA in adolescents is not only accompanied by severe clinical symptoms, but is also usually a “companion” of cardiosclerosis and rheumatism. Particularly dangerous is bradycardia, a consequence of neurosis, since it often becomes chronic and leads to serious dysfunction of the myocardium. Preventive measures aimed at preventing SA are as follows:
- organizing the correct regime, creating a balanced diet;
moderate regular physical activity;
eliminating stress, hypothermia, overheating;
hardening;
timely treatment of acute (chronic) diseases, especially infectious and viral ones.
Sinus rhythm disturbances affect the overall performance of the heart muscle, which, in turn, sooner or later will affect the amount of blood pumped by the myocardium. A deficiency of oxygen and nutrients supplied to the internal organs, tissues, and cells leads to disruptions in the functioning of the entire body. As a result, in addition to general weakness, decreased ability to work, dizziness and other unpleasant symptoms, over time, SA can lead to impaired coronary circulation and cardiac insufficiency. Only timely diagnosis and treatment (if necessary) of sinus arrhythmia will help avoid consequences for the child’s growing body.
What it is
Heart contractions occur due to sinus rhythm. A collection of nerve fibers in the right atrium is capable of generating electrical impulses, which are then transmitted to the ventricle and stimulate contraction. The number of impulses that originate in the heart depends on the age of the patient. The entire conduction system works like a large motor, which is necessary to obtain energy and provide blood circulation.
Normally, sinus rhythm should occur at regular intervals, and in case of disturbances, cardiologists diagnose the condition of arrhythmia.
The number of heartbeats (beats/minute) for children of different ages is:
- First month of life – up to 150
- Up to a year – 120-130
- 1-3 years – 110-120
- 3-8 years – 100
- 8-12 – 80-90
- Over 12 – 60-80
With arrhythmia, the number of heart beats can remain within normal limits, but their rhythm becomes confused and the intervals become unequal.
Depending on whether the electrical impulse is formed with a delay or advance, several types of arrhythmias are distinguished:
- the number of strokes remains within the normal range
- the number of contractions increases - tachycardia
- the number of rhythms decreases – bradycardia
Symptoms of sinus arrhythmia in children and adolescents
Typically, sinus arrhythmia has no obvious symptoms. The child feels normal and does not feel any discomfort. Physical and mental development are normal.
Sometimes, however, the pathology manifests itself with symptoms characteristic of other diseases. To find out the cause of the malaise, you should consult a doctor. This must be done in the following cases:
- if the baby is not gaining enough weight;
- the child’s lips turn blue, arms and legs turn pale or blue;
- the baby sleeps poorly, often worries for no apparent reason;
- the child’s appetite has decreased;
- Shortness of breath is noticeable during physical activity.
Such signs occur with heart disease, but other causes are possible. Early seeking medical help increases the chances of coping with pathology.
In older children, 4-6 years old, arrhythmia manifests itself differently. The child is able to complain about discomfort:
- fatigue, reluctance to play, especially outdoor games;
- pain, feeling of heaviness in the heart area;
- dizziness, darkness in the eyes.
The desire to avoid physical activity and complaints of weakness should not be attributed to laziness. This means that the child has reasons for such behavior. If poor health is accompanied by fainting, measures should be taken immediately.