Anatomy
Rice.
1. Schematic representation of the conduction system of the heart: 1 - branches of the right leg of the atrioventricular bundle; 2 - right leg of the atrioventricular bundle; 3 - atrioventricular node; 4 - anterior internodal bundle; 5 - posterior internodal bundle; 6 - bundles directed to the right atrium and inferior vena cava; 7 - sinoatrial node; 8 - bundle going to the superior vena cava; 9 - posterior intervenous bundle (indicated by a dotted line); 10 - bundle going to the left atrium and the mouths of the pulmonary veins; 11 - bundle going to the left atrial appendage; 12 - atrioventricular bundle; 13 - left leg of the atrioventricular bundle. In P. s. With. There are two interconnected parts: the sinus-atrial and atrioventricular (atrioventricular). The sinoatrial part includes the sinoatrial node (nodus sinuatrialis) with bundles of cardiac conductive myocytes extending from it. The atrioventricular part is represented by the atrioventricular node (nodus atrioventricularis), the His bundle, or the atrioventricular bundle (atrioventricular bundle, T.; fasc. atrioventricularis) with its left and right legs and peripheral branches - Purkinje conductive fibers (myofibrae conducentes purkinjienses). In Fig. Figure 1 shows a diagram of the conduction system of the heart.
Types of additional pathways
The following bundles of muscle fibers extend from the atria:
- James - goes to the terminal part of the AVN from the sinus node;
- Kenta-Palladino - connects the atria with the ventricles (there are right and left) bypassing the conduction system of the AVU;
- Breschenmash - from the right atrium to the bundle of His.
The Mahaim bundle unites the His trunk and AVU, the right ventricle and the septum. Sometimes additional paths are called nodal shunts, since they help bypass the AVU; short fibers in the node itself also belong to this group. There are also options with multiple paths.
Embryology
Formation of the basic elements of P. s. With. in the embryo it begins at the stage of the tubular heart, in which, according to Wenink (A. S. G. Wenink, 1976), in addition to the future contractile myocardium, there are four more morphologically specialized muscle rings: bulboventricular, atrioventricular, sinoatrial and truncobulbar . From these rings, in the process of loop formation and the formation of heart chambers, all components of the heart develop. With. The bulboventricular ring is involved in the formation of the atrioventricular bundle and its legs, the atrioventricular ring is involved in the formation of the atrioventricular node and bundle, the sinoatrial ring gives rise to the sinoatrial and atrioventricular nodes. The truncobulbar ring forms structures that function only in the heart of embryos.
The previously widespread theory of Mall (FP Mall, 1912), according to P.’s cut. With. represents the remnant of the auricular canal, currently recognized as incompetent.
The sinoatrial node (nodus sinuatrialis), described in 1906 by Keys and Fleck (A. Keith, M. Flack), is a generator of pulses to excite heart contractions (see Automation). It is located on the superior surface of the right atrium between the opening of the superior vena cava and the appendage of the right atrium. The node is always detected macroscopically. Its length is 8-26 mm, width 4-13 mm, thickness 1-3 mm. The bundles of cardiac conductive myocytes associated with the node conduct excitation to the myocardium of various parts of the atria and the atrioventricular node. There are bundles directed to the superior and inferior vena cava, the posterior intervenous bundle, described in 1906-1907. Wenckebach (K. F. Wenckebach), anterior and posterior internodal bundles, the latter was described in 1909 by Ch. Thorel. The beam conducting excitation from the node to the left atrium and the mouths of the pulmonary veins was described in 1913 by J. Tandler, and the beam directed to the appendage of the left atrium was discovered in 1916 by JG Bachmann. The sizes and position of the beams are individually variable; they are not always detected macroscopically, although they can always be detected using histological methods of examination (see).
Rice. 2. Macropreparation of the heart with the prepared left bundle branch (the cavity of the left ventricle is opened): the left bundle branch (1) is divided into anterior (2), two intermediate (3) and posterior (4) branches.
The atrioventricular node (nodus atrioventricularis) was described in 1906 by S. Tawara and L. Aschoff. It is located in the right fibrous triangle at the anterosuperior part of the mouth of the sinus of the vena cava, below the attachment of the septal cusp of the tricuspid valve. The atrioventricular node, as well as the His bundle and its branches, is always detected macroscopically (Fig. 2). The shape of the node is often round. Its length is 3-15 mm, width 1-7 mm, thickness 0.5-2 mm. The bundle of His departs from the node, which penetrates through the right fibrous triangle into the membranous part of the interventricular septum, dividing at the upper edge of its muscular part into the left and right legs. The part of the bundle extending from the node to the beginning of division into legs is called the trunk (truncus), its length is 3-20 mm. The position of the bundle in the interventricular septum is individually variable. The left leg (crus sinistrum) of the His bundle, 5-27 mm long and 1.5-15 mm wide at the point of origin from the trunk, is located under the endocardium on the left surface of the interventricular septum and is divided at the same level into 2-4 branches (rr. cruris), which pass into conducting Purkinje muscle fibers. The right leg (crus dextrum) is located under the endocardium on the right surface of the interventricular septum in the form of one trunk, much thinner than the left leg, from which branches extend all the way to the myocardium of the right ventricle.
Additional conductive tracts are also described - bundles of Kent, James, Maheim fibers, which are not macroscopically detected.
Conservative treatment
If patients do not have manifestations of rhythm disturbances (shortness of breath, fainting, heart pain, circulatory disorders), then specific treatment is not required. Such patients require periodic examination (at least once a year) and prophylactic administration of drugs to improve metabolic processes in the myocardium (Panangin, Riboxin, Magne B6).
Particular vigilance is needed in case of familial forms of arrhythmia, especially in cases of sudden cardiac arrest in close relatives, as well as persons whose professions involve physical (athletes) or neuro-emotional (drivers, pilots) overload.
They first try to relieve an attack of arrhythmia by massaging the carotid sinus (near the angle of the lower jaw), pressing on the eyeballs, holding the breath while inhaling and straining, inducing a cough or gag reflex. If ineffective, intravenous administration of Aymalin, Novocainamide, Cordarone, Ritmonorm is used. Subsequently, patients are transferred to maintenance antiarrhythmic therapy with tablets.
The use of medications from the group of calcium antagonists, cardiac glycosides and beta blockers is contraindicated, as they improve conduction along the accessory pathway, which increases the frequency of ventricular contractions and the possibility of developing ventricular fibrillation.
Blood supply
The sinoatrial node receives arterial blood from the branch of the sinoatrial node (r. nodi sinuatrialis), which often departs from the right coronary (coronary, T.) artery, less often from the circumflex branch (r. circumflexus) of the left coronary artery. The capillary network formed by arterioles extending from the branch of the sinoatrial node is oriented along the fibers. Postcapillary venules, forming a dense network, form 1-3 veins with a diameter of up to 0.5 mm, flowing into the veins of the wall of the superior vena cava, into the veins of the right atrium appendage. Bundles of cardiac conducting myocytes associated with the sinoatrial node are vascularized from nearby branches of the coronary arteries. Blood enters the atrioventricular node from the branch of the atrioventricular node (r. nodi atrioventricularis), which often departs from the right coronary artery and very rarely from the circumflex branch (r. circumflexus) of the left coronary artery. The outflow of venous blood from the node occurs through postcapillaries and venules into draining veins going to the coronary sinus of the heart (sinus coronarius) and to the middle vein of the heart (v. cordis media). Small arteries and arterioles approach the trunk of the atrioventricular bundle and its legs, coming from the artery supplying blood to the atrioventricular node, as well as from the first septal interventricular branch (r. mterventricularis septalis I) and the anterior interventricular branch (r. interventricularis anterior) of the left coronary artery. The density of arterioles in the atrioventricular node is 10 times less than in the bundle. Venous outflow from the node and bundle is carried out through small veins to the great vein of the heart (v. cordis magna). Arterioles and venules in the atrioventricular bundle are located parallel to cardiac conduction myocytes. According to Van der Hauwaert, Stroobandt, Verhaeghe (LG Van der Hauwaert, R. Stroobandt, L. Verhaeghe, 1972), anastomoses between the vascular formations of P. s. With. and vessels of the interventricular septum are absent.
Syndrome and sudden death
Cardiac pathologies are considered so dangerous because they can lead to death. Premature excitation of the ventricles of the heart, although rare, is a dangerous disease. A retrospective analysis of electrocardiograms taken from patients who suffered cardiac arrest proves that in half of the victims an increased rate of impulse transmission to the cardiac chambers was recorded after restoration of normal rhythm.
People who suffer from tachyarrhythmias and Ebstein's disease are at greatest risk of complications. The chances of sudden cardiac arrest are also high in patients whose ECG revealed a shortening of the RR interval.
The opinion regarding the dependence of the prognosis on gender and age is erroneous. Blood cholesterol levels also do not affect the risk of developing unpleasant consequences of the disease.
Histology
The composition of the formations of P. s. pp., in addition to specialized cardiomyocytes, includes nerve elements (nerve trunks of varying thickness, consisting of myelinated and non-myelinated nerve fibers, nerve endings), connective tissue with vessels. Unlike the contractile myocardium for P. s. With. characterized by a quantitative predominance of connective tissue and nerve elements over muscle and vascular elements. According to Truex (R. Truex) et al. (1974), cardiomyocytes P. s. With. with generally accepted histol. colors look lighter than the cells of the contractile myocardium and differ from them in size. Using electron microscopic studies, it has been established that in these cells the Golgi complex (see Golgi complex), localized near the nucleus or subsarcolemmal, granular and non-granular endoplasmic reticulum (see Endoplasmic reticulum), ribosomes (see); there are small round mitochondria (see), a small number of lysosomes (see), and glycogen granules. A characteristic feature of specialized cardiomyocytes is the presence of tunnel-like invaginations of the sarcolemma containing connective tissue and neural elements, pronounced subsarcolemmal cisterns, and a complex of myofilaments with polyribosomes. Depending on the size, shape of cells, number and position of myofibrils, four types of specialized cardiomyocytes are distinguished. Cells of types I, II, III were found in the composition of P. s. With. in almost all mammals, including humans. They are smaller in size than the cells of the contractile myocardium. Type I cells include spindle-shaped cardiomyocytes, which, compared to cardiomyocytes of the contractile myocardium, contain a smaller number of incorrectly oriented myofibrils. Type II cardiomyocytes have an irregular process shape and contain approximately the same number of myofibrils as the cells of the contractile myocardium, but unlike the latter, the myofibrils in type II cardiomyocytes are arranged randomly.
Type III cardiomyocytes include spindle-shaped cells with a small number of myofibrils ordered along the long axis of the cell and a large number of glycogen granules. Type IV cells (Purkinje cells) are found only in some animal species. Most mammals and humans have Purkinje cell-like cells, which are functionally similar to Purkinje cells.
Different parts of P. s. With. contain various types of specialized cardiomyocytes. The sinoatrial node consists of cells of types I and II, the atrioventricular node - of cells of types II and III, the bundle of His contains cells of all types, the legs of this bundle and its terminal branches consist of cells of type III and cells similar to Purkinje cells, or only from the latest.
There are several types of contacts between P.'s cardiomyocytes. With. With the help of insertion disks and nexuses, the heads are in contact with each other. arr. type II cells, as well as type III cells. Between type I cells, these contacts are rare; they are characterized by simple contacts. Simple contacts also occur between all other types of cardiomyocytes of P. s. With.
Spread of excitation throughout the heart muscle
⇐ PreviousPage 3 of 7Next ⇒Depolarization occurring in the sinoatrial node spreads radially through the atria and then converges at the AV junction. Atrial depolarization is completely completed within 0.1 s. Since conduction in the AV node is slower than conduction in the atria and ventricles in the myocardium, an atrioventricular (AV) delay occurs lasting 0.1 s, after which excitation spreads to the ventricular myocardium. The duration of atrioventricular delay is reduced by stimulation of the sympathetic nerves of the heart, while under the influence of irritation of the vagus nerve its duration increases.
From the base of the interventricular septum, a wave of depolarization propagates at high speed along the Purkinje fiber system to all parts of the ventricle within 0.08–0.1 s. Depolarization of the ventricular myocardium begins on the left side of the interventricular septum and spreads primarily to the right through the middle part of the septum. A wave of depolarization then travels along the septum down to the apex of the heart. Along the ventricular wall it returns to the AV node, moving from the subendocardial surface of the myocardium to the subepicardial.
Bundle of His. The cardiomyocytes of this bundle conduct excitation from the AV junction to the Purkinje fibers. Conducting cardiomyocytes of the His bundle are also part of the sinoatrial and atrioventricular nodes.
Purkinje fibers . Conducting cardiomyocytes of Purkinje fibers are the largest cells of the myocardium. Cardiomyocytes of Purkinje fibers do not have T-tubules and do not form intercalary discs. They are connected by desmosomes and gap junctions. The latter occupy a significant area of contacting cells, which ensures the highest speed of excitation through the ventricular myocardium.
Additional cardiac pathways
The Bachmann bundle starts from the sinoatrial node, some of the fibers are located between the atria (interatrial bundle to the left atrial appendage), some of the fibers are directed to the atrioventricular node (anterior internodal tract).
The Wenckebach bundle starts from the sinoatrial node, its fibers are directed to the left atrium and to the atrioventricular node (middle internodal tract).
The James bundle connects one of the atria to the AV junction or passes within this junction; along this bundle, excitation can prematurely spread to the ventricles. The James bundle is important for understanding the pathogenesis of Lown–Guenon–Levine syndrome. The faster propagation of the impulse in this syndrome through the accessory pathway leads to a shortening of the PR (PQ) interval, but there is no widening of the QRS complex, since excitation spreads from the AV junction in the usual way.
Kent's bundle - accessory atrioventricular connection - an abnormal bundle between the left atrium and one of the ventricles. This bundle plays an important role in the pathogenesis of Wolff–Parkinson–White syndrome. Faster propagation of the impulse through this additional pathway leads to: 1) shortening of the PR interval (PQ); 2) earlier excitation of part of the ventricles - wave D occurs, causing expansion of the QRS complex.
Maheima bundle (atriofascicular tract). The pathogenesis of Maheim syndrome is explained by the presence of an additional pathway connecting the His bundle with the ventricles. When excitation is carried out through the Maheim bundle, the impulse propagates through the atria to the ventricles in the usual way, and in the ventricles part of their myocardium is excited prematurely due to the presence of an additional conduction pathway. The PR (PQ) interval is normal, and the QRS complex is widened due to the D wave.
Extrasystole is a premature (extraordinary) contraction of the heart, initiated by excitation emanating from the myocardium of the atria, AV junction or ventricles. The extrasystole interrupts the dominant (usually sinus) rhythm. During extrasystole, patients usually experience interruptions in the functioning of the heart.
The property of myocardial contractility is provided by the contractile apparatus of cardiomyocytes connected into a functional syncytium using ion-permeable gap junctions. This circumstance synchronizes the spread of excitation from cell to cell and the contraction of cardiomyocytes. An increase in the force of contraction of the ventricular myocardium - the positive inotropic effect of catecholamines - is mediated by β1-adrenergic receptors (sympathetic innervation also acts through these receptors) and cAMP. Cardiac glycosides also increase contractions of the heart muscle, exerting an inhibitory effect on Na+,K+ - ATPase in the cell membranes of cardiomyocytes.
• Required initial level of knowledge:
1. Location and structural features of the automation nodes and conduction system of the human heart.
2. Membrane-ionic mechanisms of origin of PP and PD in excitable structures.
3. Mechanisms and nature of information transfer in muscle tissue.
4. Ultrastructure of skeletal muscle tissue and the role of cellular-subcellular formations involved in contraction.
5. Structure and function of the main contractile and regulatory proteins.
6. Basics of electromechanical coupling in skeletal muscle tissue.
7. Energy supply for the process of excitation - contraction - relaxation in the muscles.
Lesson plan:
1. Introductory word from the teacher about the purpose of the lesson and the scheme of its implementation. Answers to student questions - 10 minutes.
2. Oral survey - 30 minutes.
3. Educational, practical and research work of students - 70 minutes.
4. Students complete individual control tasks - 10 minutes.
Questions for self-preparation for the lesson:
1. Physiological properties and characteristics of the heart muscle.
2. Automaticity of the heart muscle, its causes. Parts of the conduction system of the heart. The main pacemaker of the heart, the mechanisms of its rhythm-forming function. Features of the occurrence of PD in the cells of the sinus node.
3. Automatic gradient, the role of the atrioventricular node and other parts of the conduction system of the heart.
4. Action potential of working cardiomyocytes, its features.
5. Analysis of the spread of excitation throughout the heart.
6. Excitability of the heart muscle.
7. Contractility of the heart muscle. The “all or nothing” law. Homeo- and heterometric mechanisms of regulation of myocardial contractility.
8. The ratio of excitation, contraction and excitability during the cardiac cycle. Extrasystoles, mechanisms of its formation.
9. Age characteristics in children.
Educational, practical and research work:
Task No. 1.
Watch the video “Properties of the heart muscle.”
Task No. 2.
Look at the slides “Origin and propagation of excitation in the cardiac muscle.” Draw in a notebook (for memorization) the location of the main elements of the conduction system. Note the features of the propagation of excitation in it. Draw and remember the features of the action potential of working cardiomyocytes and pacemaker cells.
Task No. 3.
After studying the theoretical material and watching (slides, films), answer the following questions:
1. What is the ionic basis of the membrane action potential of myocardial cells?
2. What phases does the action potential of myocardial cells consist of?
3. How did the representation of myocardial cells develop?
4. What is the significance of diastolic depolarization and threshold potential in maintaining cardiac automaticity?
5. What are the main elements of the conduction system of the heart?
6. What are the features of the propagation of excitation in the conduction system of the heart?
7. What is refractoriness? What is the difference between periods of absolute and relative refractoriness?
8. How does the initial length of myocardial fibers affect the strength of contractions?
Task No. 4.
Analyze situational tasks.
1. The membrane potential of the pacemaker cell of the heart increased by
20 mV. How will this affect the frequency of automatic pulse generation?
2. The membrane potential of the pacemaker cell of the heart decreased by 20 mV. How will this affect the frequency of automatic pulse generation?
3. Under the influence of the pharmacological drug, phase 2 (plateau) of the action potentials of working cardiomyocytes was shortened. What physiological properties of the myocardium will change and why?
Task No. 5.
Watch videos introducing experimental techniques. Discuss what you saw with your teacher.
Task No. 6.
Perform experiments. Analyze and discuss your results. Draw conclusions.
1. Analysis of the conduction system of the heart by applying ligatures (Stannius ligatures), (see workshop, pp. 62-64).
2. Excitability of the heart, extrasystole and reaction to rhythmic stimulation. (see Workshop pp. 67-69).
Recommended reading:
1. Lecture material.
2. Human physiology: Textbook/Ed. V.M.Smirnova
3. Normal physiology. Textbook./ V.P. Degtyarev, V.A. Korotich, R.P. Fenkina,
4. Human physiology: In 3 volumes. Per. from English/Under. Ed. R. Schmidt and G. Tevs
5. Workshop on physiology / Ed. M.A. Medvedev.
6. Physiology. Fundamentals and functional systems: Course of lectures / Ed. K. V. Sudakova.
7. Normal physiology: Course of physiology of functional systems. /Ed. K.V. Sudakova
8. Normal physiology: Textbook / Nozdrachev A.D., Orlov R.S.
9. Normal physiology: textbook: 3 volumes. V. N. Yakovlev et al.
10. Yurina M.A. Normal physiology (educational manual).
11. Yurina M.A. Normal physiology (short course of lectures)
12. Human physiology / Edited by A.V. Kositsky.-M.: Medicine, 1985.
13. Normal physiology / Ed. A.V. Korobkova.-M.; Higher school, 1980.
14. Fundamentals of human physiology / Ed. B.I. Tkachenko.-St. Petersburg; 1994.
⇐ Previous3Next ⇒
Functional meaning
P.S. With. determines the frequency, sequence and strength of heart contractions. The triggering mechanism for myocardial contraction is an excitation impulse that occurs in specialized pacemaker (see Pacemaker) type I cardiomyocytes that are part of the sinoatrial node. This impulse occurs in the node at regular intervals from 60 to 80 times per 1 minute. Normally, the sinoatrial node is the pacemaker of the heart. From the node, the excitation impulse propagates at a speed of 0.8-1 m/sec along the bundles of cardiac conductive myocytes to the cardiomyocytes of the contractile atrial myocardium and to the atrioventricular node. Slow-conducting type II cardiomyocytes participate in the conduction of impulses through the bundles. From the atrioventricular node, the excitation impulse travels at a speed of 1-1.5 m/sec through fast-conducting cardiomyocytes of type III and Purkinje-like cells of the His bundle and its branches and then at a speed of 3-5 m/sec through their branches and conducting Purkinje fibers to the contractile cardiomyocytes myocardium of the ventricles of the heart (see also Heart, physiology).
Diagnosis of additional pathways in the myocardium
An ECG study is used to detect abnormal conduction pathways.
Wolff-Parkinson-White syndrome
It is characterized by accelerated conduction of impulses bypassing the AVU along the Kent, Breshenmache pathways or simultaneous movement along the James and Mahaim beams. It can be obvious and hidden (only in the opposite direction), constant or periodic. In the latter case, the signal passes normally, but if there is a significant delay, an additional path is switched on in the AVU.
It manifests itself as arrhythmia - supraventricular tachycardia, flutter and atrial fibrillation. The attacks are felt as fainting, dizziness, shortness of breath.
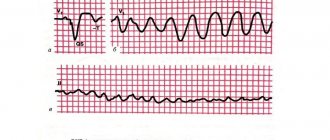
The ECG reveals:
- short PQ up to 0.1;
- additional wave (delta);
- altered QRS complex;
- leg block;
- normal atrial waves;
- attacks of tachycardia or atrial fibrillation.
Clerk-Levy-Christesco syndrome
Associated with activation of the James beam. Most patients have no clinical manifestations. During physical or emotional stress, strong heart palpitations and shortness of breath may occasionally occur. On the ECG it appears as a shortening of the PQ interval, while the ventricular complex is of normal shape, there is no delta wave. In the absence of symptoms, it has a benign course.
Activating the Mahaim Beam
In this case, the impulse almost completely passes the atrioventricular node, but then quickly moves along an additional path to the His bundle. This causes blockade of the right (more often) or left leg, widening of the QRS and formation of a delta wave. The atrial wave and the distance from it to the ventricular complex do not change. Patients often develop supraventricular tachycardia.
Pathology
Malformations of P. s. With. may arise due to disruption of the formation of the interventricular septum, while double contact of the bulboventricular and atrioventricular rings can lead to the formation of two (anterior and posterior) separate atrioventricular nodes. Abnormal connections between other specialized muscle rings lead to the emergence of a number of additional conducting structures described in 1976 by Wenink in some animals and humans: the retroaortic node, node-like structures in the interatrial septum, conducting elements of the atrioventricular ring. Research by R. N. Anderson et al. (1977) showed that disruption of the normal connection of the atrial and ventricular myocardium when the atrioventricular node is separated from the bundle of the same name can lead to congenital complete heart block, and the presence of additional pathways (bundle of Kent) between the atria and ventricles, bypassing the atrioventricular bundle, can contribute to development of Wolff-Parkinson-White syndrome (see Wolff-Parkinson-White syndrome). In the presence of the James bundle, connecting the atrial myocardium to the trunk of the atrioventricular bundle, or the Maheim fibers, connecting the trunk of the atrioventricular bundle to the ventricular myocardium, various forms of ventricular preexcitation syndrome may develop.
Acquired pathology P. s. With. may occur with functional or organic damage (inflammation, ischemia, necrosis, dystrophy). Depending on the level, degree and nature of P.’s lesion. With. various types of disturbances in the normal coordination of contractions develop between different parts of the myocardium or parts of the heart (see Heart arrhythmias, Heart block, Atrial fibrillation, Paroxysmal tachycardia, Heart, pathology, Extrasystole),
Bibliography:
Bratanov V. S. Individual and age-related features of the topography of the human atrioventricular conduction system, Vestn. chir., t. 105, no. 10, p. 22, 1970; Mikhailov S.S. and Chukbar A.V. Topography of elements of the conduction system of the human heart, Arkh. anat., gistol, and embryol., t. 44, no. 6, p. 56, 1982; U m o-v and t V. N. Conducting system for congenital defects of the heart septa, Kyiv, 1973, bibliogr.; X u b u-tiya B.I., Ermolova Z.S. and Telyatnikov S.S. Surgical anatomy of the conduction system of the heart, Grudn. hir., No. 1, p. 41, 1975; Cher in the island I. A. and Pavlovich E. R. Morphology of the main parts of the conduction system of the rat heart, Arkh. anat., gistol, and embryol., t. 77, no. 8, p. 67, 1979; A p-d er son R. N. a. O. Congenitally complete heart block, developmental aspects, Circulation, v. 56, p. 90, 1977; In 1 about about g S. M. Cardiac pathology, Philadelphia, 1978; Brechenmacher C. Atrio-His bundle tracts, Brit. Heart J.* v. 37, p. 853, 1975; In u g with he 1 1 HB In support of Kent, J. thorac. cardiovasc. Surg., v. 79, p. 637, 1980; The conduction system of the heart, Structure, function and clinical implications, ed. by HJ Wel-lens ao, p. 55, Leiden, 1976; D av ies MJ Pathology of conducting tissue of the heart, L., 1971; E 1 iska O. a. E 1 isk about y a M. Venous circulation of the human cardiac conduction system, Brit. Heart J., v. 42, p. 508, 1979; they e, Lymphatic drainage of the ventricular conduction system in man and in the dog, Acta anat., v. 107, p. 205, 1980; Gardner E. a. O' R ahi 1 1 y R. The nerve supply and conducting system of the human heart at the end of the embryonic period proper, J. Anat., v. 121, p. 571, 1976; Michailow S. Neue anatomische Forschungsergebnisse vom Nerven- und Reizleitungssystem des Herzens, S. 84, Stuttgart, 1974; Navaratnam V. The human heart and circulation, L.—NY, 1975; Osterwalder B. a. Schneider J. Morphologische Untersuchungen am menschlichen Reizleitungs, in the book: Probleme der Medizin in der Ud SSR, hrsg. v. V. Parin u. L. Staroselsij, system, Schweiz, med. Wschr., S. 953, 1976; Sherf L. a. James Th. N. Fine structure of cells and their histologic organization within internodal pathways of the heart, clinical and electrocardiographic implications, Amer. J. Cardiol., v. 44, p. 345, 1979; Van der Hauwaert LG, Stroobandt R. a. Yerhaeghe L. Arterial blood supply of the atrioventricular node and main bundle, Brit. Heart J., v. 34, p. 1045, 1972; Wenink ACG Development of the human cardiac conduction system, J. Anat., v. 121, p. 617, 1976.
S. S. Mikhailov, I. A. Chervova.
Endovascular destruction of accessory pathways
To destroy additional pathways, laser radiation, cold cauterization, or electric current can be used. Radiofrequency targeted treatment of the myocardium – radioablation – is recognized as the most effective. Its advantages include:
- good tolerance;
- short rehabilitation period;
- the ability to refuse to take antiarrhythmic drugs that are highly toxic.
If there are additional conduction pathways, before surgery, in addition to standard ECG, 24-hour Holter monitoring, and stress tests, it is necessary to conduct an electrophysiological study of the heart. Sometimes ultrasound with Doppler sonography and MRI are also required.
Indications and contraindications
Cauterization of the myocardium with radio waves is carried out when a patient has:
- attacks of loss of consciousness, vascular collapse;
- reduction in cardiac output;
- direct and reverse impulse conduction with paroxysmal tachycardia;
- latent form of Wolff-Parkinson-White syndrome with a burdened hereditary history, high occupational risk;
- poor tolerance to medications or resistance to them, the presence of contraindications;
- atrial fibrillation and flutter;
- reciprocal (associated with impulse circulation) tachycardia;
- several accessory pathways with complex rhythm disturbances.
The operation is not recommended for cancer, acute myocardial infarction, cardiomyopathy, rhythm disturbances with multiple ectopic foci, unstable angina, venous or arterial thrombosis, vascular aneurysms.