“Jellyfish head” is one of the symptoms of portal hypertension developing in various pathologies, which is manifested by the appearance of visible, convoluted and dilated veins on the anterior surface of the abdominal wall, diverging in different directions from the navel. The appearance of the blood vessels visible through the skin resembles the head of the character from the myths of Ancient Greece, Medusa the Gorgon, who had snakes on her head instead of hair.
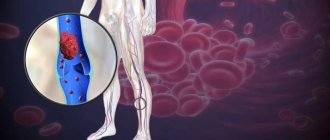
The appearance of the symptom in question may indicate the development of various pathologies, which are accompanied by an increase in pressure in the portal vein and its branches. This vessel collects blood from all organs of the abdominal cavity, and disruption of its outflow provokes the appearance of multiple additional collateral vessels. They branch in different directions, expand and become visible on the skin of the abdomen. Due to increased pressure in the portal vein, the patient develops ascites, in which the skin on the anterior abdominal wall becomes thinner due to overstretching. As a result, the network of dilated vessels becomes even more noticeable.
Causes
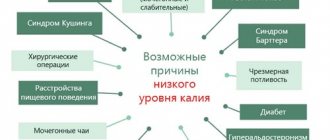
Many severe heart diseases lead to portal hypertension, including myocarditis and cardiomyopathies.
“Jellyfish head” can be detected in patients with various pathologies of the liver and other organs:
- liver pathologies: alcoholic, acute or chronic hepatitis, hepatosis, primary or secondary biliary cirrhosis, sarcoidosis, carbohydrate liver degeneration, amyloidosis, polyps and liver tumors, metastases from other organs;
- pancreatic tumors;
- cholelithiasis;
- schistosomiasis;
- pathologies of the cardiovascular system: heart defects (congenital and acquired), restrictive cardiomyopathy, phlebothrombosis of the liver veins in Budd-Chiari syndrome, constrictive pericarditis;
- chronic poisoning with hepatotropic poisons;
- complications of surgical interventions, injuries and burns;
- taking chemotherapy drugs;
- bleeding from the stomach and intestines;
- infectious diseases of the digestive system;
- taking high doses of diuretics and tranquilizers;
- intrauterine thrombosis of the liver veins.
Jellyfish head in medicine: symptoms, causes of the syndrome, treatment
© Soldatenkov Ilya Vitalievich, general practitioner, especially for SosudInfo.ru (about the authors)
“Jellyfish head” is a clinical sign of portal hypertension caused by increased pressure in the portal vein and its branches.
This symptom got its name due to its external resemblance to the mythical character - Medusa the Gorgon, who had not hair growing on her head, but snakes.
Dilated saphenous veins run along the anterior surface of the abdomen and meander in the umbilical region. In medicine, “jellyfish head” is a clinical manifestation of liver cirrhosis and other diseases.
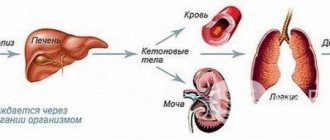
The portal vein (portal vein) is a blood vessel that collects blood from the abdominal organs and approaches the “gate” of the liver, which is how it got its name. In the liver tissue, the portal vein branches, the blood is filtered from toxins and metabolic products. Purified blood in the lungs is enriched with oxygen and distributed to internal organs and tissues.
Portal hypertension is a symptom complex manifested by dyspeptic symptoms, dilated abdominal veins, hepatosplenomegaly, and ascites.
Diagnosis of pathology consists of X-ray and ultrasound examinations, percutaneous splenomanometry, and gastroduodenoscopy. To get rid of the “jellyfish head”, it is necessary to create a bypass path for the blood flow by performing an anastomosis.
Portal hypertension complicates the course of gastroenterological, cardiovascular and hematological diseases.
abdominal vessels forming the “head of the jellyfish” syndrome
Etiology
When the outflow of venous blood from the unpaired internal organs of the abdominal cavity is disrupted, a “jellyfish head” appears on the abdomen. Obstacles that arise in the bloodstream of the portal system lead to the appearance of bypass paths - collaterals. Through them, the blood goes around the existing barrier.
The collaterals expand, grow and become clearly visible on the abdomen, resembling the “head of a jellyfish”. In the presence of ascites, the skin on the abdomen becomes thinner and translucent, as a result of which the vascular network acquires a clear outline.
Ascites in this pathology is a pathognomonic sign that persists for a long time and is difficult to treat.
direction of blood flow through the veins of the abdominal wall with obstruction of the portal vein (left), with obstruction of the inferior vena cava (right).
“Jellyfish head” appears in various conditions:
- Liver dysfunction – cirrhosis, hepatosis, hepatitis, sarcoidosis,
- Pathologies of the heart and blood vessels - endophlebitis and portal vein thrombosis, pericarditis, cardiomyopathy, congenital and acquired heart defects;
- Metabolic disorders - amyloidosis, carbohydrate liver dystrophy;
- Helminthiasis;
- Oncopathologies - liver tumors and polyps, cancer and liver metastases;
- Long-term exposure to toxic substances – hepatotropic poisons;
- Chemotherapy - treatment with cytostatics;
- Complications of operations, consequences of injuries and burns;
- Infectious diseases of the digestive system;
- Intrauterine hepatic vein thrombosis;
- Bleeding from the stomach and intestines;
- Treatment with loading doses of tranquilizers and diuretics;
- Regular consumption of strong drinks
Symptoms
“Jellyfish head” is not the only symptom of pathology. Portal hypertension manifests itself with a variety of clinical signs.
Dyspeptic disorders are the earliest clinical signs of portal hypertension. These include:
- Loss of appetite,
- Bloating,
- Constipation followed by diarrhea
- Feeling full when eating small amounts of food
- Abdominal pain.
manifestations of the “head of Medusa”
Signs of asthenia and intoxication:
- Dizziness,
- lethargy,
- Insomnia,
- Fluctuations in blood pressure,
- Muscle weakness
- Arthralgia and myalgia,
- Hair loss, brittle nails,
- Weight loss,
- Fever.
Signs of obstructive jaundice:
- Dark colored urine
- Light feces,
- Yellow skin tone and icteric sclera,
- Itchy skin
- Pain in the right hypochondrium.
Symptoms of multiple organ failure:
- Hepatosplenomegaly,
- Nervous system dysfunction
- Dyspnea,
- Bleeding of the mucous membranes of the nose and mouth,
- Cough,
- Arrhythmia,
- Dropsy of the abdomen with swelling of the ankles.
Symptoms
An increase in pressure in the portal vein is accompanied not only by the appearance of the “head of jellyfish” symptom. Usually the first signs of this condition are digestive disorders:
- feeling of fullness in the stomach when eating small portions of food;
- constipation alternating with diarrhea;
- stomach ache;
- loss of appetite;
- bloating.
When the hepatic ducts are compressed, the patient develops obstructive jaundice:
- yellowness of the skin and mucous membranes;
- darkening of urine;
- discoloration of stool;
- skin itching;
- pain in the right hypochondrium.
Portal hypertension causes asthenia in the patient and is accompanied by intoxication:
- frequent feeling of weakness;
- dizziness;
- instability of blood pressure;
- weight loss;
- pain in muscles and joints;
- muscle weakness;
- fever;
- hair loss and brittle nails;
- sleep disorders.
Changes in blood circulation lead to multiple organ failure:
- increase in the size of the liver and spleen;
- tendency to nosebleeds;
- dyspnea;
- rhythm disturbances;
- swelling in the ankles;
- cough;
- ascites;
- disorders of the nervous system.
A prolonged increase in pressure in the portal vein leads to the development of varicose veins of the esophagus, stomach and rectum. Because of this, the patient may experience bleeding, which can cause posthemorrhagic anemia.
If untreated, portal hypertension is complicated by encephalopathy and the patient has complaints of drowsiness, memory impairment, decreased concentration and excessive irritability.
What is the head of a jellyfish in liver cirrhosis?
Cirrhosis is a pathological change in the liver when healthy tissue is replaced by connective scar tissue. One of the clinical manifestations of the disease is “jellyfish head”, when the vessels of the portal system protrude under the skin of the abdomen. The pattern of dilated saphenous veins on the abdomen resembles the writhing snakes on the head of the mythical character - Medusa the Gorgon.
In medicine, this symptom is used to identify one of the complications of cirrhosis, which occurs at stage 3 of the disease. What is the “head of a jellyfish” in liver cirrhosis? This is a manifestation of portal varicose veins, a symptom of pathology of the portal vein, a blood vessel entering the parenchyma.
Reasons for the formation of “jellyfish head”
The liver is an organ that filters venous blood and utilizes decay products from it. After passing through the parenchyma, the blood is directed to the lungs and again distributed through the vascular system to the internal organs. Then it again enters the portal vein - the entrance vessel of the parenchyma. There it spreads along small vascular branches that penetrate the lobules of the largest gland in the body.
When the function of the parenchyma fades due to cirrhosis, foci of connective tissue form and blood flow is disrupted. The connective tissue tightens the parenchyma, small vessels are pinched, and excess pressure is created in the portal vein system.
Against the background of portal hypertension in cirrhosis, the veins located under the skin of the abdomen dilate. They begin to bulge entirely, form venous nodes - a “jellyfish head” is formed. A pressure of up to 12 mm Hg is created in the veins. Art., the normal value is almost half less - 7 mm Hg. Art. Over time, new vessels are formed - collaterals.
The body creates bypass pathways that go around the liver. All of them are concentrated in the abdomen and connect to the umbilical vein. With ascites, a complication of cirrhosis, the vessels in the abdomen bulge even more. When exudate accumulates in the abdominal cavity, the abdomen increases in volume and the skin becomes tense.
The manifestation of the “jellyfish head” begins with the vascular network, small stars, and nodules. When the walls of the subcutaneous vessels are stretched, cavities are formed - hernias, in which blood stagnates. With increased blood pressure, the process of vasodilation accelerates.
How does the head of a jellyfish appear?
The photo shows the intricate pattern formed by the dilated vessels. It's called "jellyfish head". Sometimes pineal venous formations are observed, which protrude into large tubercles on the abdomen. The protruding vessels resemble a ball of snakes; they are concentrated in the navel area and diverge from it in different directions.
Sometimes a varicose node forms right in the area of the umbilical hollow. Externally, the stomach of a patient with cirrhosis with dilation of the saphenous veins resembles a ball of snakes. Doctors gave the symptom a sonorous name due to its resemblance to the head of the Gorgon, a character in the myths of Ancient Greece. This houria had thin living snakes growing on its head instead of hair.
Diagnosis of causes
“Jellyfish head” most often occurs with cirrhosis, but there may be other causes of varicose pathology of the subcutaneous vessels located on the abdomen. To confirm or refute necrotic lesions of the parenchyma, the patient is thoroughly examined. Urine and blood tests are required.
In cirrhosis, elevated levels of bilirubin, ALT and AST enzymes, albumin, and alkaline phosphatase are diagnosed. A CT scan with contrast injection reveals pathology of the hepatic portal vein. Ultrasound allows you to determine the degree of development of cirrhosis. The “jellyfish” symptom occurs only at stages 3 and 4; it signals the development of portal hypertension.
Other signs of cirrhosis and ascites are revealed: jaundice appears, extremities become severely swollen, loss of muscle mass is observed, and the patient’s general condition worsens due to increasing intoxication.
: Is it possible to get cirrhosis of the liver from a patient?
Complications and prognosis
The appearance of a “jellyfish head” is dangerous for bleeding of internal organs. Varicose veins of the esophagus develop, the functioning of internal organs deteriorates, and ascites (dropsy) develops more intensively.
The severity of the symptom depends on the morphological form of cirrhosis and the causes of its occurrence. Typically, the symptom is diagnosed at the stage when liver destruction can actually be stopped; with timely treatment, the patient maintains quality of life for 10–15 years. Strict adherence to doctor's instructions and a long course of treatment are required.
Surgery minimizes portal hypertension, the “head of the jellyfish” appears less, and the risk of bleeding is reduced. With the first one, 60% of patients survive; after the second one, no more than 20 patients out of a hundred survive. The head of a jellyfish is a reason to take your health seriously, give up bad habits, and lead a measured lifestyle.
Source: https://progepatity.ru/tsirroz/golova-meduzy-pri-tsirroze
Diagnostics
Ultrasound will help detect liver disease, which has led to portal hypertension and varicose veins of the anterior abdominal wall.
“The head of a jellyfish” is detected when examining the anterior abdominal wall - dilated, tortuous veins protruding above the surface of the skin are visible on the abdomen. In addition, the patient has swelling in the ankles and signs of ascites (increased abdominal volume). When palpating the liver, its increase is determined. The organ becomes lumpy and dense.
To identify the cause of the appearance of the “jellyfish head”, the patient is prescribed the following studies:
- blood tests: clinical, biochemistry, serum immunoglobulins, coagulogram;
- Ultrasound of the abdominal organs;
- Dopplerometry of liver vessels;
- radiographic techniques: angiography of mesenteric vessels, celiacography, portography, cavography, splenoportography;
- CT;
- MRI;
- liver scintigraphy;
- esophagoscopy;
- fibrogastroduodenoscopy;
- sigmoidoscopy.
In some cases, the examination of the patient is supplemented by a liver biopsy followed by histological analysis.
What diseases may this indicate?
Enlarged veins in the abdomen can occur due to diseases such as:
- Hepatosis. It develops due to the entry of excess fat into the liver or difficulty in its exit from the liver. The fat accumulates and ruptures the hepatocyte (liver cells). Adipose tissue replaces liver tissue.
- Amyloidosis. A systemic disease in which the functioning of the immune system is disrupted and insoluble protein is deposited in the wall of the hepatic vessels and bile ducts. In this case, the condensed vessels cannot function normally, and portal hypertension occurs.
- Carbohydrate liver dystrophy. In this case, glycogen accumulates in the nucleus of hepatocytes, and they significantly increase in size and die.
- Hepatitis. A viral disease that affects the liver and causes inflammation,
- Helminthic infestations. Once in the liver, helminths live there for a long time and multiply unhindered. They can compress the hepatic vessels and contribute to bile stagnation, which leads to portal hypertension,
- Sarcoidosis. A systemic inflammatory disease in which white blood cells become very active and produce substances that form granulomas (inflammatories).
- Thrombosis of the portal or inferior genital vein,
- Cirrhosis of the liver. A disease in which liver tissue dies and is gradually replaced by scar tissue,
- Pericarditis,
- Cardiomyopathy,
- Malformations of heart valves.
- Cruvelier-Baumgarten disease. This is a developmental defect in which the umbilical vein (which supplies the fetus in the womb with nutrients) does not heal, combined with congenital hypoplasia of the portal vein.
- Cruvelier-Baumgarten syndrome. Unlike the disease, the syndrome is not a congenital condition, but develops in adult patients due to cirrhosis of the liver. It is more common in young women.
- Liver cancer and metastases. Cancer cells grow and compress hepatocytes, and the liver cannot perform its functions.
Treatment
To eliminate the “head of the jellyfish”, the underlying disease and the portal hypertension that provokes the appearance of this symptom must be treated.
The following medications are used to reduce pressure in the portal vein:
- vasoconstrictors (vasopressin, somatostatin) - used to narrow arterioles and reduce pressure in the portal vein;
- organic nitrates (nitroglycerin, isosorbide, etc.) – help reduce blood volume in the portal vein by increasing its volume in small vessels;
- ACE inhibitors (fosinopril, lisinopril, enalapril, captopril, etc.) – are used to eliminate arterial hypertension and improve blood flow in peripheral vessels;
- beta-blockers (propranolol, metroprolol, etc.) – reduce the number of heart contractions, lower blood pressure and increase tissue resistance to lack of oxygen;
- diuretics (furosemide, etc.) – eliminate swelling and promote the elimination of toxic substances along with urine;
- lactulose – helps eliminate toxic substances from the intestines;
- hepatoprotectors;
- B vitamins.
With portal hypertension, the patient must follow a diet that involves limiting the consumption of salt and protein foods.
If conservative therapy is ineffective, the patient is prescribed surgical treatment. In case of bleeding from varicose veins of the esophagus or stomach, endoscopic operations can be performed to ligate or sclerosis the affected vessels. If these minimally invasive techniques are ineffective, then the varicose veins are stitched through the mucous membrane.
When portal hypertension is complicated by gastrointestinal bleeding, splenomegaly and accumulation of fluid in the abdominal cavity, it is recommended to perform operations aimed at creating a bypass anastomosis, which will ensure the outflow of blood from the portal vein into the inferior vena cava or renal vein. Depending on the clinical case, the following types of bypass surgery are performed:
- mesentericocaval - portocaval anastomosis is created between the inferior vena cava and the superior mesenteric vein;
- portocaval - a shunt is performed between the portal and cava veins;
- selective splenorenal - distal vascular anastomosis is applied between the splenic and left renal veins;
- transjugular intrahepatic portosystemic - a stent is implanted through the jugular vein, which creates an anastomosis between the portal and hepatic veins;
- reduction of splenic arterial blood flow - a spiral is introduced endovascularly (through the femoral artery) into the splenic artery, which reduces the volume of arterial blood flow and prevents venous outflow into the portal vein.
In case of decompensated or complicated portal hypertension, laparocentesis or drainage of the abdominal cavity is performed. In some advanced cases, the patient may be recommended liver transplantation and splenectomy.
Which doctor should I contact?
If a “jellyfish head” appears (visible convoluted dilated veins on the abdomen), signs of indigestion, jaundice, deterioration in general condition and an increase in the abdomen in volume, you should consult a physician. After conducting a series of studies (ultrasound of the abdominal organs, Doppler ultrasound of liver vessels, CT, MRI, portography, liver scintigraphy, etc.) and identifying signs of portal hypertension, the doctor may prescribe a consultation with a specialized specialist (cardiologist, hepatologist, etc.) and treatment with a vascular surgeon
“Jellyfish head” is a symptom of portal hypertension and manifests itself in the form of dilated and tortuous veins on the anterior abdominal wall. It can occur with various diseases and conditions and always requires immediate treatment of the underlying ailment. To reduce pressure in the portal vein, conservative therapy and surgical treatment are prescribed.
About portal hypertension in the program “Live Healthy!” with Elena Malysheva:
Jellyfish head in medicine: causes and symptoms of the syndrome, treatment
Cirrhosis is a pathological change in the liver when healthy tissue is replaced by connective scar tissue. One of the clinical manifestations of the disease is “jellyfish head”, when the vessels of the portal system protrude under the skin of the abdomen. The pattern of dilated saphenous veins on the abdomen resembles the writhing snakes on the head of the mythical character - Medusa the Gorgon.
In medicine, this symptom is used to identify one of the complications of cirrhosis, which occurs at stage 3 of the disease. What is the “head of a jellyfish” in liver cirrhosis? This is a manifestation of portal varicose veins, a symptom of pathology of the portal vein, a blood vessel entering the parenchyma.
Anatomy of the structure of the abdominal veins
The main vein that participates in the formation of the jellyfish’s head is the portal vein and its branches. This vein is a blood vessel that takes blood from organs located in the abdominal cavity.
This vessel approaches the entrance to the liver, hence the name “portal”. Once in the epithelium of the liver, this vein sends out its branches, and the blood is cleansed of toxins and decay products.
Next, the blood follows to the lungs, where it is saturated with oxygen and again enters the general bloodstream.
Medicine identifies the meaning of portal hypertension - this is a complex of symptoms that are manifested by nausea, vomiting, constipation, venous enlargement of the abdominal cavity, fluid concentration in the abdominal cavity and a simultaneous increase in the size of the spleen and liver.
The head of the jellyfish manifests itself as a complication of diseases from the field of hematology and gastroenterology, pathological cardiac and vascular conditions.
Consequences
Since dilation of the veins of the abdominal wall is a serious symptom, the consequences of the diseases that cause it can be severe:
- Cirrhosis of the liver;
- Malignant neoplasms;
- Bleeding;
- Ascites;
- Death.
Therefore, if this symptom is detected, you must immediately consult a doctor and begin treatment. In most cases, such diseases require the patient to be in a hospital.
Reasons for the progression of pathology
If a person has a disturbance in the outflow of blood flowing in the veins from the abdominal organs, a symptom such as the head of a jellyfish appears. The factors causing this condition are disturbances in the collateral outflow of blood.
This situation occurs when barriers to healthy blood flow form in the portal vein. Most often, the severity of the pathology of the head of the jellyfish occurs during the period of death of liver tissue.
If the patient has ascites, the skin becomes thinner and becomes more translucent, which leads to the appearance of a clear outline of the network of blood vessels.
The appearance of a jellyfish head is characteristic of the following pathological conditions:
- Impaired liver function - death of liver tissue, hepatitis, etc.;
- Tumor formations in the liver, tumor formation in the liver, or metastasis to it;
- Metabolic disorders – carbohydrate thinning of the liver, amyloidosis;
- Thrombosis of the hepatic veins inside the womb;
- Gastric and intestinal hemorrhages;
- Therapy with large dosages of tranquilizers and diuretics;
- Pathologies of the cardiovascular system - congenital or acquired heart defects, thrombosis of the portal vein, pericarditis, cardiomyopathy;
- Chemotherapy (cytostatic therapy);
- Burdens after surgical interventions, burns, or injuries;
- Infectious diseases of the gastrointestinal tract;
- Constant consumption of alcoholic beverages.
The occurrence of portal hypertension due to liver disorders
Which doctor should I contact?
If a “jellyfish head” appears (visible convoluted dilated veins on the abdomen), signs of indigestion, jaundice, deterioration in general condition and an increase in the abdomen in volume, you should consult a physician.
After a series of studies (ultrasound of the abdominal organs, Doppler of liver vessels, CT, MRI, portography, liver scintigraphy, etc.
) and identifying signs of portal hypertension, the doctor may prescribe a consultation with a specialized specialist (cardiologist, hepatologist, etc.) and treatment with a vascular surgeon.
“Jellyfish head” is a symptom of portal hypertension and manifests itself in the form of dilated and tortuous veins on the anterior abdominal wall. It can occur with various diseases and conditions and always requires immediate treatment of the underlying ailment. To reduce pressure in the portal vein, conservative therapy and surgical treatment are prescribed.
About portal hypertension in the program “Live Healthy!” with Elena Malysheva:
Jellyfish head
(lat. caput medusae
) is the name given to the dilated convoluted saphenous veins on the anterior abdominal wall, meaning a roundabout route for the outflow of venous blood from the portal vein system (
vena portae
). This name is given because in such cases, the veins around the navel, expanding, resemble the image of the head of the mythological Medusa - the most famous of the three Gorgon sisters, a monster with a woman's face, who had writhing snakes growing from her head instead of hair.
The expansion of venous blood vessels on the anterior abdominal wall develops as a result of the redistribution of venous blood into the bypass portacaval and cavo-caval anastomoses, which have the value of a roundabout outflow path from the portal vein system when obstacles arise to its normal passage in the portal vein itself. Such disturbances in the outflow of venous blood through the portal vein most often develop in pathologies that impede the passage of blood through the liver: cirrhosis of the liver, including alcoholic cirrhosis of the liver, as well as cancer of the liver.
Normally, venous blood flows into the portal vein from all unpaired organs of the abdominal cavity (stomach, small and large intestines, spleen and pancreas), with the exception of the liver and the lower third of the rectum. From these organs, venous blood enters the liver through the portal vein, and from it through the hepatic veins into the inferior vena cava.
In the venous system, additional routes for the outflow of blood, in addition to the main deep veins and their tributaries, are also the superficial or saphenous veins, as well as the venous plexus, which is widely developed in humans. Of greatest importance in clinical practice are intersystem venous anastomoses, through which the systems of the superior and inferior vena cava and portal veins are interconnected.
As a result, porto-caval, cavo-caval, and cavo-cavoportal anastomoses are formed. All of them have the meaning of a collateral (roundabout) path of blood outflow, bypassing the main veins. Porto-caval anastomoses are normally poorly developed in humans, but when the outflow of blood through the portal vein system is impaired, they expand significantly.
In this case, they provide the process of “dumping” blood bypassing the liver from the portal vein system into the system of the superior and inferior vena cava.
Symptoms of head jellyfish
The appearance of jellyfish head pathology is not the only sign of venous disease. Hypertensive portal vein disease is characterized by a variety of clinical signs.
The main symptoms that appear are:
- Feeling of nausea;
- Vomiting;
- Yellowing of the skin;
- Hemorrhages;
- Disturbances in the rhythm of heart contractions;
- Deviations from normal blood pressure;
- Darkening of urine;
- Lethargy;
- Dyspnea;
- Dizziness;
- Cough;
- Disturbances in the nervous system;
- Loss of body weight;
- Sleep problems;
- General weakness;
- Increased body temperature;
- Itchy skin;
- Pathological enlargement of the liver;
- Dropsy with swelling of ankles;
- Pain in the right hypochondrium;
- Accumulation of fluid in the abdominal cavity.
Other causes of symptoms
This symptom can occur not only in liver cirrhosis. It also accompanies other pathological conditions leading to the development of the same hypertension. These conditions include:
- acute liver diseases (alcoholic hepatitis, failure);
- chronic liver diseases (malignant tumors, sarcoidosis);
- thrombosis of the portal and inferior vena cava;
- abnormalities in the cardiovascular system.
Diagnostics
At the first visit, the doctor examines the patient, studies the medical history and listens to his complaints.
After an initial examination and detection of signs of a jellyfish head, the doctor will send the patient for laboratory and hardware tests that will help accurately diagnose the root cause that caused this sign.
The main research methods are:
- Complete blood count – helps determine the general condition of the patient’s blood;
- General urine analysis - possible pathologies of the kidneys and urinary tract are determined;
- Coagulogram - analysis of blood clotting;
- Blood test for hepatitis ;
- Skin biopsy - examination of the skin at the site of the lesion to determine the processes occurring in the tissues;
- Liver scintigraphy is a radioisotope scan of the liver. During the study, a series of images is taken after the introduction of a radioisotope into a vein, acting as a contrast agent;
- Ultrasound examination of blood vessels - helps to determine the condition of blood vessels at the site of the lesion, identify damage to the walls of blood vessels and possible overlaps and narrowings;
- X-ray – irradiation of the body to determine pathological foci;
- Angiography – x-ray with contrast agent;
- MRI and CT scans detect nodules in the liver tissue and other neoplasms. The methods are quite expensive compared to the above.
At the first visit, the doctor examines the patient, studies the medical history and listens to his complaints.
What diseases may this indicate?
Enlarged veins in the abdomen can occur due to diseases such as:
- Hepatosis. It develops due to the entry of excess fat into the liver or difficulty in its exit from the liver. The fat accumulates and ruptures the hepatocyte (liver cells). Adipose tissue replaces liver tissue.
- Amyloidosis. A systemic disease in which the functioning of the immune system is disrupted and insoluble protein is deposited in the wall of the hepatic vessels and bile ducts. In this case, the condensed vessels cannot function normally, and portal hypertension occurs.
- Carbohydrate liver dystrophy. In this case, glycogen accumulates in the nucleus of hepatocytes, and they significantly increase in size and die.
- Hepatitis. A viral disease that affects the liver and causes inflammation;
- Helminthic infestations. Once in the liver, helminths live there for a long time and multiply unhindered. They can compress the hepatic vessels and contribute to bile stagnation, which leads to portal hypertension;
- Sarcoidosis. A systemic inflammatory disease in which white blood cells become very active and produce substances that form granulomas (inflammatories).
- Thrombosis of the portal or inferior genital vein;
- Cirrhosis of the liver. A disease in which liver tissue dies and is gradually replaced by scar tissue;
- Pericarditis;
- Cardiomyopathy;
- Malformations of heart valves.
- Cruvelier-Baumgarten disease. This is a developmental defect in which the umbilical vein (which supplies the fetus in the womb with nutrients) does not heal, combined with congenital hypoplasia of the portal vein.
- Cruvelier-Baumgarten syndrome. Unlike the disease, the syndrome is not a congenital condition, but develops in adult patients due to cirrhosis of the liver. It is more common in young women.
- Liver cancer and metastases. Cancer cells grow and compress hepatocytes, and the liver cannot perform its functions.
Jellyfish head treatment
Drug therapy is aimed at reducing pressure on the walls of the portal vein vessels during the initial stages of the disease.
The main medications are:
| Beta blockers (Anaprilin, Metoprolol) | They help reduce the number of heart contractions, lower blood pressure, and increase tissue resistance to oxygen starvation. |
| Diuretics (Lasix, Furosemide) | Relieves swelling and helps remove toxins from the body. |
| Vasoconstrictors (Somatostatin, Vasopressin) | They help narrow arterioles and reduce pressure on the walls of the portal vein. |
| Nitrates (Nitroglycerin) | They influence the accumulation of blood in small vessels, which helps relieve the load on the liver. |
| ACE inhibitors (Captopril, Lisinopril) | They lower blood pressure and activate blood flow in the vessels of the whole body. |
| Hepatoprotectors (Karsil) | For maintenance therapy of a patient with chronic liver inflammation. |
| Vitamin complexes (with essential vitamin B) | Saturate the body with the necessary vitamins and minerals. |
| Lactulose | Helps cleanse the intestines of toxins and waste products. |
Surgical intervention is used in extreme and advanced stages of development of the pathology of the head of the jellyfish. During the operation, a path is artificially created between the vessels, which helps reduce pressure on the walls of the portal vein .
During surgery, an anamostosis is created, creating a bypass for circulating blood. In addition, pathological sections of blood vessels are stitched or bandaged, and electrocoagulation is performed.
In the absence of effectiveness of drug treatment and surgical interventions, liver transplantation is performed.
Treatment with traditional medicine
The use of medical folk remedies can only be used as an additional therapy, but not as the main treatment for the pathology of the Head of the Medusa.
Source: https://MedBur.ru/rekomendacii/golova-meduzy-v-medicine.html