Thrombosis of the inferior vena cava is a type of severe pathological process, which is accompanied by partial or complete disruption of blood flow and requires emergency medical care. The tasks of the hollow inferior duct include transporting blood between the lower extremities, a number of pelvic organs and the right atrium.
To establish the clinical picture, it is necessary to determine the level of thrombosis, indicators of narrowing of the lumen, and also to identify which segment is “under attack.”
Causes
Varicose veins are a serious risk factor for the development of acute phlebothrombosis.
So far, the exact reasons for the development of thrombosis have not been established. It is known that the following triad of factors can contribute to clogging of venous vessels:
- high blood clotting;
- slowing blood flow;
- damage to the venous wall.
Various diseases and conditions can contribute to the occurrence of the above factors:
- varicose veins;
- smoking;
- long bed rest;
- pregnancy and childbirth;
- C-section;
- taking certain medications that increase blood viscosity (for example, oral contraceptives);
- atherosclerosis;
- injuries of vascular walls (including those associated with frequent venous punctures);
- compound fractures;
- surgical interventions on joints and abdominal operations;
- obesity;
- infections;
- long trips or air flights;
- physical inactivity;
- alcohol abuse;
- malignant neoplasms;
- heart valve pathologies;
- arrhythmias;
- heart failure;
- old age.
Prevention
To prevent blood clots, a comprehensive approach of preventive measures is necessary.
If a person is at risk and suffers from varicose veins, he needs to be especially careful about his health.
To maintain venous walls in tone, venotonics are used.
Be sure to establish a healthy diet and monitor your drinking regime. These measures are aimed at reducing blood viscosity.
Controlling body weight is important. Obesity and overweight should not be allowed to occur.
If possible, prolonged stress on the legs in one position should be avoided.
Cycling, water aerobics and swimming help maintain blood vessels in proper tone.
List of mandatory preventive measures:
- avoiding dehydration and overheating;
- wearing compression garments;
- performing a daily set of gymnastic exercises;
- wearing orthopedic shoes;
- avoiding heavy physical activity and static positions;
- avoiding prolonged immobility.
Treatment and prevention will be ineffective if the patient does not give up bad habits, primarily smoking.
Classification and stages
Depending on the location of the blockage of the venous vessel, experts distinguish the following types of thrombosis:
- subcutaneous – damage to the superficial veins occurs;
- deep – blockage develops in deep veins;
- ascending - in addition to blockage of the venous vessels, the patient develops additional pathologies in the lymphatic system (lymphostasis, limangoitis), it is very difficult and without treatment in 90% of cases causes death.
Depending on the type of blood clot, the following types of vein thrombosis are distinguished:
- parietal - the blood clot is located near the venous wall;
- occlusive - a thrombus completely blocks the lumen of the vein;
- floating - a blood clot is attached to the venous wall on one side only, and the other end is in motion and can come off;
- mixed - combines the characteristics of previous varieties.
During acute venous thrombosis, two stages are distinguished:
- compensation – no pronounced hemodynamic disturbances are observed, pain and discomfort occur periodically, sometimes the temperature rises for no apparent reason, the duration of this stage can vary from 24 hours to 1 month;
- decompensation – hemodynamic disturbances occur, pain becomes intense, swelling appears, skin color changes and limb mobility becomes difficult.
How dangerous is the disease?
As a result of this condition, the following pathologies develop:
If a clot breaks away from the venous wall, it can travel through the bloodstream into the pulmonary artery and block it.
- Blockage of large, medium and small veins of the lower extremities. This condition ends in gangrene.
- Pulmonary embolism. Appears if a thrombotic formation breaks away from its place of origin and enters the veins of the lungs through the systemic circulation.
- Heart attack. When a migrating thrombus enters the coronary vessels, necrosis of the cardiac myocardium occurs.
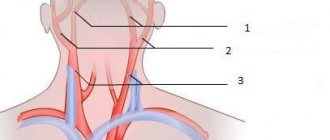
- Stroke. Brain disorders occur when thrombotic formations travel through the jugular veins into the choroid plexuses of the head.
Symptoms
In the initial stages of development, vein thrombosis can manifest itself as minor and rare pain, sensations of fullness in the muscles and heaviness in the legs. Sometimes pain occurs in the lumbosacral region or lower abdomen on the side of the thrombosis. Usually these symptoms do not cause much concern, and the patient consults a doctor only at the beginning of the acute stage of the disease.
As thrombosis progresses, the following symptoms suddenly occur:
- sharp pain in the leg;
- stiffness and difficulty in movements;
- swelling (the leg increases in size, its soft tissues become denser);
- the skin on the leg turns blue (sometimes becomes blackish or pale milky);
- local increase in temperature (fever in the leg);
- noticeable visual expansion of the saphenous veins;
- low-grade fever, weakness, adynamia.
All of the above manifestations are caused by stagnation of venous blood below the site of thrombus formation. If the vessel is completely blocked, the patient's hemodynamics are disrupted, swelling increases and gangrene may develop. At all stages of the disease, when a blood clot breaks off, the development of pulmonary embolism, stroke, and thromboemolius of other organs is likely.
Acute venous thrombosis always develops suddenly, and its manifestations can become maximal from the first day of the disease. The nature and severity of symptoms depend on the following factors:
- location of the blocked vessel;
- diameter of the affected vein;
- type of blood clot;
- rate of blood clot formation;
- the likelihood of a reflex circulatory disorder in neighboring vessels;
- tissue sensitivity to hypoxia;
- severity of collateral circulation.
Symptoms of iliac vein thrombosis
Symptoms indicating iliac vein thrombosis have a number of features:
- The pain is most often localized in the groin area, in the area of the inner thigh.
- The pain may radiate to the calf muscle.
- Character of pain: bursting, pulling, dull. With iliac vein thrombosis, acute pain never occurs.
- Pain first bothers a person only during physical activity, and then begins to appear at rest.
- Pain is associated with a number of factors:
- Development of periphlebitis in the iliac region (inflammation of the tissue surrounding the iliac vein);
- Stretching of the walls of the affected vein by formed blood clots;
- Stretching of the walls of the tributary veins due to increased blood circulation;
- Increased venous pressure;
- Increased blood circulation in the arteries that are connected to the iliac vein that has undergone thrombosis;
- Overexertion of the limbs.
- Swelling of the leg on the affected side. A characteristic feature of iliac vein thrombosis is that tissue swelling extends not only to the thigh and leg, but also to the genitals and buttock. Of course, it is the thigh that swells the most. When you press on the affected tissue, there is no hole left. The reason for its absence comes down to the fact that the veins are filled with blood during thrombosis, so water is contained not only in the subcutaneous fat layer, but also in the soft tissues. Edema always occurs, but the degree of its severity varies in all patients.
Ileofemoral venous thrombosis
This type of venous thrombosis is distinguished separately, since this disease is very severe, progresses quickly and is associated with a high risk of developing pulmonary embolism. Ileofemoral phlebothrombosis is caused by blockage of the iliofemoral segment and is characterized by intense pain, severe swelling of the entire leg and severe general condition of the patient. The affected limb turns blue and the saphenous veins dilate. When the outflow of blood completely stops, the patient quickly develops gangrene.
About veins
The vena cava and its system consist of vessels that collect blood from the walls and organs of the abdominal cavity, pelvis and legs.
The inferior vena cava is the largest vessel in the human body. There is not a single valve in it.
Appears by the confluence of the iliac veins, the origin is located in the anterior lateral right surface of the lumbar region.
It is worth noting that the breathing process changes the diameter of the lumen of the vessel: when inhaling, it contracts, and when exhaling, it becomes wider. The normal fluctuation range is from two to three centimeters. The vena cava collects blood waste. Behind it are the kidney artery and the right lumbar artery.
Thrombosis of the inferior vena cava
This type of thrombosis is also characterized by a severe course and a high risk of complications. When the inferior vena cava is blocked by thrombotic masses, both legs of the patient swell, and 80% of patients develop renal failure, accompanied by the appearance of blood in the urine. In cases of blockage of the liver segment, liver failure develops, complicated by Budd-Chiari syndrome. In the future, the patient may develop severe inferior vena cava syndrome.
Symptoms
If a blood clot has formed in the inferior vena cava, then a person experiences pain in the affected area, swelling of the lower extremities, and vessels protrude in the abdominal cavity. But such signs rarely appear, since a blood clot most often forms not in the vena cava, but in its segments.
In the case of thrombus formation in the infrarenal area and blockage of the inferior vena cava, the patient feels severe pain in the lumbar region and abdomen. In addition, the legs swell, the skin becomes bluish or red, and all the vessels are clearly visible in the lower abdomen.
When thrombosis forms in the liver segment, the following signs appear:
- Severe pain syndrome that occurs in the area of the ribs and shoulder blades.
- Swelling of the peritoneum.
- Yellowness of the skin.
- Enlargement of the liver and spleen, which is felt upon palpation.
- Dilated vessels are clearly visible on the abdomen.
If thrombus formation occurs in the renal segment, the patient may not feel any symptoms. This is possible when the vein is not completely blocked by a blood clot. Sometimes a person has symptoms that do not indicate thrombosis. The patient complains of a general deterioration in condition, increased temperature and pressure, weakness, pale skin and other unpleasant signs.
If a blood clot blocks the renal segment of the vein, pain occurs in the lumbar and abdominal area, nausea, vomiting, digestive organ upset, and the volume of urine excreted decreases. These symptoms of thrombosis of the inferior vena cava are characteristic of signs of intoxication of the body, so people rarely pay attention to them.
Diagnostics
Duplex scanning of veins plays an important role in the diagnosis of acute venous thrombosis.
To detect venous thrombosis, the following studies are performed:
- Dopplerography and duplex scanning of veins - allows you to identify the location and extent of thrombosis, assesses the quality of blood flow and the condition of the venous walls;
- X-ray contrast venography – performed if the results of an ultrasound scan are questionable or if a blood clot is located above the groin;
- MR angiography – performed when the results of previous studies are questionable;
- impedance plethysmography - performed when thrombosis of veins above the knee is suspected, carried out using a cuff that is inflated with air and provides temporary occlusion of the veins to measure changes in their filling before and after deflation of the cuff;
- X-ray of the lungs – performed if pulmonary embolism is suspected;
- blood tests (coagulogram, D-dimer, culture for sterility) - are carried out to determine blood clotting indicators and identify infections.
Diagnosing the problem
To determine the diagnosis, you should undergo a series of examinations. Initially, the patient's medical history is collected. After it is collected, the doctor carries out an examination - the level of the pain threshold and the shade of the skin are assessed.
The second stage of diagnosis is laboratory tests, urine and blood tests.
Sometimes additional examinations are prescribed:
- Reactive protein assay.
- Thromboelastogram.
- Coagulogram.
- Blood test to determine the prothrombin level index.
Diagnosis using instruments consists of duplex angio scanning. Using Doppler mapping. This is the most popular method for locating a blood clot.
If an acute situation is observed, additional instrumental examination is prescribed:
- Phlebography.
- Cavagraphy.
- Photoplethysmography.
- Vascular ultrasound.
It is worth realizing that this disease is fraught with the appearance of acute disorders and often leads to the death of the patient. It is important to find signs of a problem in a timely manner and get a full examination. If the treatment is chosen correctly, the growth of the blood clot can be stopped.
Treatment
The main objectives in the treatment of acute venous thrombosis are aimed at restoring blood flow in the affected vessel, preventing the progression of edema, the development of gangrene of the limb, preventing pulmonary embolism and other complications. If damage to the deep veins is detected, the patient is urgently hospitalized in a specialized angiosurgical hospital or general surgery department. Patients with superficial vein thrombosis can be observed on an outpatient basis.
Depending on the clinical case, treatment can be conservative or surgical. If the risk of thromboembolism is high, bed rest is prescribed. All patients with venous thrombosis are recommended to wear compression stockings (the tightness of the stockings should be determined by the attending physician) and follow a diet.
All patients with venous thrombosis are advised to take anticoagulants. These medications are the most effective at preventing progression of the disease. Patients are sequentially prescribed direct (nadroparin, dalteparin, enoxaparin and other low molecular weight and unfractionated heparins) and indirect (phenyline, acenocoumarol, warfarin, ethyl biscoumacetate) anticoagulants. When choosing a drug, contraindications to its use must be taken into account.
To improve blood circulation and thin the blood, patients with venous thrombosis are prescribed:
- clopidogrel;
- rheopolyglucin;
- ticlopedin;
- pentoxifylline;
- phleboactive agents: Troxevasin, Escusan, Detralex, etc.
To eliminate pain and reduce platelet aggregation, it is recommended to take non-steroidal anti-inflammatory drugs:
- diclofenac;
- ketoprofen;
- ibuprofen, etc.
If infections are detected or there is a high risk of developing (for example, AIDS, diabetes, etc.), antibiotic therapy is indicated for the patient.
To eliminate venous thrombosis, hirudotherapy may be recommended as an addition to treatment. The saliva of medicinal leeches contains substances that help eliminate inflammation of the venous walls, destroy blood clots and prevent the formation of new blood clots. When prescribing hirudotherapy, the doctor must take into account possible contraindications to this method of treatment. The number of sessions is determined by the clinical case.
Sometimes conservative measures are not enough to eliminate thrombosis and prevent its complications, and then patients undergo surgical operations, which can be performed either planned or urgently. The following methods can be used for this:
- installation of a vena cava filter - a special metal device in the form of an umbrella is installed in the lumen of the inferior vena cava temporarily or permanently, the operation is performed endovascularly (through the lumen of a venous vessel) and is carried out to prevent thromboembolism (for example, with floating blood clots);
- thrombolysis - intervention is performed when it is necessary to remove large blood clots (prescribed infrequently due to the high risk of bleeding), carried out using a special catheter into which a drug that destroys the clot is injected;
- venous angioplasty - a balloon is inserted into the area of narrowing of the vessel, which, after inflating, expands its lumen; a stent is installed in the place of narrowing of the vein;
- venous bypass - during the intervention, incisions are made outside the narrowed part of the venous vessel, to which a venous graft (taken from the patient’s thigh or synthetic) is sutured, ensuring blood flow in the area affected by thrombosis;
- thrombectomy - the operation is performed classically or endovascularly; under angiography control, the doctor identifies the location of the blood clot, makes a small incision and removes the blood clot using a special catheter.
After the operation, the patient is prescribed drug therapy.
Femoral vein thrombosis: causes, symptoms and treatment
Femoral vein thrombosis is the most dangerous of all types of deep vein blockages. The disease poses a threat to human life. The problem is further aggravated by the fact that in the early stages the disease is asymptomatic, and it can be very difficult to diagnose it in a timely manner.
Definition
Deep vein thrombosis (DVT) is the formation of blood clots that block (partially or completely) the internal lumen. Most often, the process is localized in the lower extremities, for example, in the femoral vein. Classic signs of DVT:
- swelling;
- pain;
- redness of the skin in the affected area.
The disease occurs in approximately 20% of the population and, if untreated, often causes death from pulmonary embolism. The main risk group is men. In women, DVT is common if they are taking hormonal birth control.
Femoral vein thrombosis is the most dangerous of all localizations of blood clots. When complications develop in the form of pulmonary embolism, death occurs in 60% of cases.
Thrombosis of the femoral vein is also dangerous due to the risk of clot rupture and penetration into the heart. In most cases, embolism of this organ is fatal.
With the development of thrombosis of the iliac and femoral veins, the following symptoms are characteristic:
- severe swelling and pain in the legs, starting from the groin area;
- cyanosis of the skin of the lower extremities;
- petechial rash (small hemorrhages in the form of dots);
- increase in temperature due to the addition of phlebitis.
Phlebologists distinguish two stages of acute thrombosis of the deep veins of the thigh. They differ in the color of the skin of the lower extremities: white and blue phlegmasia. The initial stage of thrombosis is characterized by a pale coloration of the skin: due to a reflex spasm of small arteries, blood circulation is disrupted. At this stage you can observe the following:
- The pulsation of the arteries of the feet decreases.
- Extremities are cold to the touch.
- Patients often complain of severe pain.
Important! Blueness of the legs indicates that venous vessels of various sizes are overflowing with blood and is accompanied by darkening of the skin, severe bursting pain and blisters containing hemorrhagic fluid protruding to the surface. At this stage, thrombosis can progress to gangrene.
Clinical manifestations
In 50% of patients there are no signs of thrombosis. A complete clinical picture can be provided not so much by DVT itself, but by its complications caused by the addition of an internal infection. The walls of the vein around the blood clot become inflamed. In this case, the patient's body temperature may increase.
Very often, when making a diagnosis, doctors confuse thrombosis with thrombophlebitis. This is explained by the almost simultaneous occurrence and course of both processes. Symptoms manifest differently and depend on the location of the vessel affected by the thrombus. So, with DVT of the lower leg the following are observed:
- swelling in the lower part of the limb (ankle);
- pain that occurs when bending the leg at the knee joint;
- sensory disturbances in the foot (numbness or fever).
Treatment
Treatment methods for deep vein thrombosis depend on the causes of the disease and the presence/absence of complications. The age of the patient, as well as his general health, are also important.
Conservative therapy is indicated in cases where the blood clot does not completely block the vessel, sits “firmly” in place and is unlikely to break off. Treatment goal:
- restoration of normal vein patency;
- preventing the destruction of a blood clot and preventing the possibility of embolism of blood vessels of vital organs;
- eliminating tissue damage.
Thrombolytic therapy is a type of drug treatment. The main objective of this method is to restore blood flow in the vascular bed. Achieved by dissolving the blood clot. The method consists of activating the fibrinolytic properties of blood by converting plasminogen into plasmin, the active form.
The drugs used in the thrombolytic method of treatment differ from heparins in the principle of action. While heparins only inhibit the formation of clots, thrombolytics destroy existing blockages in the veins.
This method of treating DVT is most effective in the first three days after the formation of a blood clot.
Anticoagulant therapy is indicated for all patients with deep vein thrombosis. Treatment should begin with injections of blood thinning drugs. It is preferable to use low molecular weight heparins (LMWH) or fondaparinux with a gradual transition to indirect drugs (Warfarin).
Elastic compression involves wearing compression stockings (class 2-3). If a patient has obliterating diseases of the leg arteries, compression stockings should be used with caution.
Compression therapy is contraindicated if tibial posterior artery systolic pressure is less than 80 mmHg. Art. It is often used as concomitant therapy during surgical interventions to remove blood clots.
Surgical methods
If the patient’s condition allows, then in emergency cases or in case of individual intolerance to drugs, blood clots are removed through surgery. Also during the operation, the patency of the vein cavity is restored while maintaining the functions of the valves.
Important! The cause of PE (pulmonary embolism) in most cases is untreated deep vein thrombosis.
Considering the high percentage of deaths from the penetration of detached blood clots into the lungs, the prevention of their formation during surgery is given great importance.
So, for several days before surgery and in the postoperative period, the doctor prescribes the patient to wear compression stockings or apply elastic bandages. On the second day after surgery, exercise therapy is prescribed. If the patient is paralyzed, he is prescribed massage.
Nutrition
The substances we get from foods can affect blood thickness in different ways. In case of increased coagulability, in order to avoid the formation of blood clots, the following should be limited or completely eliminated from the diet:
- lard, fatty meat and sausages, canned meat, butter;
- white pastries;
- legumes (beans, peas, soybeans, lentils);
- rosehip, black currant, chokeberry;
- bananas and pomegranates;
- walnuts.
Useful foods for those with a tendency to develop blood clots include boiled lean meat, fish, cottage cheese and kefir, and vegetable oil. Fresh herbs (dill, parsley, onions), garlic, tomatoes are very useful. You can eat all fruits and berries except those that are prohibited. If the patient does not have diabetes and is not overweight, chocolate is allowed.
In addition to diet, it is very important to maintain a drinking regime. In addition to tea, coffee, juices, compotes and other drinks, you need to drink an average of about 2 liters of plain drinking water per day. A sufficient amount of fluid in the body can have a positive effect on blood viscosity, preventing blood clots from forming.
Source: //vseonogah.ru/zabolevaniya-sosudov/tromboz/bedrennoj-veny.html
Diet
To improve the rheological properties of blood, a patient with venous thrombosis should drink up to 2.5 liters of water per day.
All patients with venous thrombosis are advised to follow a special diet and take a sufficient amount of fluid (up to 2.5 liters per day). Proper nutrition can improve the rheological properties of blood, reduce swelling and improve the condition of vascular walls.
The following foods that increase blood clotting should be excluded from the menu:
- foods high in vitamin K and C: green vegetables and fruits, spinach, nettle, sorrel, walnuts, rose hips, currants, citrus fruits, bell peppers, chokeberries, etc.;
- fatty meats;
- sausages;
- canned meat;
- fatty dairy products;
- mayonnaise;
- spicy, fried, smoked, sweet and salty dishes;
- confectionery products with margarine, butter and cream;
- pastry products;
- coffee;
- alcoholic drinks.
Products rich in polyunsaturated fatty acids (Omega 3 and Omega 6) and vitamin E have a beneficial effect on the condition of blood vessels and blood. In addition, the diet should include foods that prevent flatulence and constipation, in which blood stagnation in the lower part of the body increases.
For vein thrombosis, the following products should be included in the daily menu:
- fish fat;
- fatty fish: salmon, pike perch, mackerel, cod;
- lean meat (1-2 times a week);
- seafood: squid, mussels, crabs;
- low-fat fermented milk products;
- cashew nuts;
- cereals;
- legumes;
- vegetable oils: olive, cedar, flaxseed, corn, soybean, wheat germ, etc.
- asparagus;
- corn;
- onion;
- garlic;
- horseradish;
- pepper;
- pumpkin and sunflower seeds;
- melons and watermelons;
- foods rich in fiber: cabbage, carrots, etc.
For vein thrombosis, it is recommended to prepare dishes by boiling or steaming.