Causes of the problem
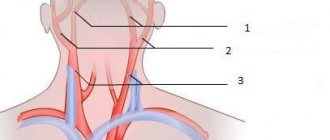
The “head of a jellyfish” appears due to the appearance of a barrier in the vein, as a result of which the blood begins to move along “back-up routes”.
If the cause of this phenomenon is not eliminated, the veins will begin to expand, which will soon be noticeable to the naked eye. However, pathology is dangerous not only because of aesthetic imperfections, but also because of real health problems. At the same time, enlarged veins in the abdominal area pose the greatest danger to women during pregnancy. Portal hypertension is not a separate disease, but a syndrome that accompanies other pathologies associated with increased pressure in the portal vein. To find out the cause of this phenomenon, you need to undergo a full examination prescribed by a doctor. Possible prerequisites for portal hypertension include:
- cirrhosis of the liver;
- congenital anomalies;
- umbilical sepsis;
- suppuration in the abdominal area;
- endophlebitis (hepatic vein thrombosis);
- pericarditis (inflammation of the pericardial sac);
- tumor-like and cystic neoplasms;
- tricuspid valve insufficiency;
- inflammation in the abdominal cavity;
- complications after operations;
- hepatosis (metabolic disorders in liver cells);
- amyloidosis (protein metabolism disorder);
- carbohydrate liver dystrophy;
- hepatitis;
- helminth infection;
- sarcoidosis (increased levels of enzymes in the liver);
- cardiomyopathy (primary damage to the heart muscle);
- cancer or metastases in the liver.
The list of causes of portal hypertension is quite extensive, but diagnosis is simplified by the fact that there are several types of this disease, each of which is associated with certain pathologies. There is intrahepatic, suprahepatic, subhepatic or combined portal hypertension. Only a doctor can determine the type of pathology and identify the cause of its formation, since for the patient the symptoms will be the same in different cases.
Causes
There are a number of factors that lead to the expansion of veins in the abdominal area:
- Pregnancy. During this period, the veins of the legs, uterus, and small pelvis begin to expand. The changes are triggered by hormonal imbalances and poor nutrition. To alleviate your condition, you need to lead a healthy lifestyle and eat a balanced diet. If cosmetic defects persist after childbirth, it is necessary to use venotonics. In severe cases, photocoagulation and sclerotherapy are used.
- Women who lift heavy things, take hormones for a long time, or sit constantly have problems with their veins. Over time, a network of blood vessels becomes noticeable on their abdomen. Venous congestion in the pelvis is especially dangerous; it leads to the development of varicose veins of the pelvic organs and uterus.
- Physical inactivity in men leads to varicocele and inhibits sexual function due to problems with blood circulation.
When a woman loses weight sharply, her subcutaneous tissue becomes thinner, and veins become visible through it. If the vessels are visible, but without nodes, this is normal. A venous vascular network on the abdomen appears in those who like to play sports, especially in security forces and bodybuilders. In this case, the venous pattern begins to sharply intensify, while the vessels are large and thickened. The condition is not dangerous, but it spoils the appearance if you suddenly stop training.
Primary varicose veins are a pathological condition in which venous vessels enlarge and, over time, become deformed and blood flow is disrupted. As a rule, the disease is caused by genetic causes, weak vessel walls, vascular diseases, and heart disease.
It is dangerous when veins in the abdomen appear as a result of portal hypertension, and the “head of the jellyfish” syndrome develops, the abdomen noticeably enlarges, ascites is observed, and swelling increases. Portal hypertension is provoked by pylephlebitis, thrombosis, as well as fatty hepatosis, hepatic cirrhosis, and dystrophy.
Symptoms of the disease
The primary symptoms of the disease are directly related to the disease that caused the appearance of the “jellyfish head”. This may include the occurrence of pain, nausea, vomiting, shortness of breath, cough, change in color of stool and urine, etc. There may also be a general deterioration in the condition: weakness, insomnia, decreased appetite, increased body temperature, lethargy, dizziness, irregular heart rhythm, etc. d.
Gradually, symptoms characteristic of portal hypertension appear, these include:
- a sharp increase in the size of the spleen;
- varicose veins in the abdominal area;
- accumulation of fluid in the abdominal cavity (ascites);
- digestive disorders;
- venous bleeding;
- lack of appetite;
- formation of spider veins.
Veins on the abdomen - description
Brightly visible veins in the abdominal area are a reason to make an appointment with a doctor. Often this process is a sign of an emerging disease. Phlebologists believe that the appearance of veins on the abdomen is, as a rule, a clinical symptom of varicose veins.
Varicose veins are a pathology characteristic of both adults and children. Initially, the appearance of stars and nodules is observed on the body, and then the venous network is already visible. Most often this pathological disease is observed on the lower extremities. During the examination, the doctor may also detect enlarged veins in the abdominal area, on the back, arms and other parts of the body.
Rarely, varicose veins affect larger vessels. Intradermal vessels are the first to be affected. The larger the affected area, the more often the patient experiences discomfort accompanied by swelling. For advice, you should contact a phlebologist, who can establish a course of treatment and tell you whether the patient needs surgical intervention. To eliminate such a skin defect, laser therapy or photocoagulation is prescribed.
Enlarged veins in the abdomen can lead to serious illnesses. Pregnant women should be especially careful. Failure of hormones and an increase in the volume of circulating blood can lead to an increase in the load on the venous system and an increase in veins on the skin. As a rule, this pathology is more often observed in females than males. Most often, varicose veins are observed on the abdomen in overweight people and in people who frequently consume alcoholic beverages and tobacco products. In such people, the blood is thicker, and the blood vessels and abdominal muscles are weaker. It is these processes that contribute to the formation of the disease.
If the symptoms of the pathology are identified in a timely manner and a course of therapy is started, eliminating varicose veins on the skin of the abdomen will not be difficult.
Diagnostic methods
To treat the disease faster and with less effort and money, you need to contact a gastroenterologist as soon as the first symptoms of the problem appear. It is especially important to recognize portal hypertension during pregnancy, since in this case an individual approach from an obstetrician-gynecologist will be required.
Diagnosis of the disease begins with a general examination of the patient by a doctor, collecting medical history data and drawing up a picture of the course of the pathology. After this, the symptoms are examined and if portal hypertension is suspected, general blood and urine tests, biochemical examination of venous blood, examination for the presence of hepatitis, etc. are prescribed.
Also, along with laboratory tests, instrumental examination procedures can be prescribed - ultrasound, x-ray examination of potentially blocked veins, splenoportography, etc.
Once the doctor has determined that the patient's symptoms indicate varicose veins due to portal hypertension, treatment can begin. It must be comprehensive and include medications and surgical procedures. Treatment with folk remedies is also possible, but only after consultation with the doctor and only as additional methods of alleviating the patient’s condition.
Diagnostics
If varicose veins are the cause of a specific disease, it is necessary to contact a vascular surgeon, phlebologist, and a pregnant woman should consult an obstetrician-gynecologist.
After the doctor listens to all the complaints, collects anamnesis, he prescribes:
- Blood test for viruses, liver enzymes.
- Ultrasound of internal organs, blood vessels, liver to evaluate the portal vein and learn about sclerotic changes.
- Puncture of the spleen and liver.
- Venography of the affected veins.
- Additional methods are sigmoidoscopy, esophagography, laparoscopy.
Conservative treatment
Often, in the early stages of the disease, you can only get by with drug treatment, since the problem is not advanced. At later stages, conservative therapy is combined with medical procedures and surgeries to achieve the desired result. The doctor needs to be especially careful when treating portal hypertension in a woman during pregnancy, since this disease can have a very serious impact on both her and the child.
The following groups of drugs can be prescribed for therapy:
- Pituitary hormones. These drugs help normalize blood flow, as they reduce hepatic blood flow and reduce pressure in the portal vein.
- Nitrates. They reduce blood flow in the liver due to the accumulation of blood in small vessels.
- Beta blockers. Reduce blood flow to the liver by reducing heart contractions.
- Synthetic analogues of somatostatin. I promote narrowing of arterioles in the perihepatic area, which helps reduce pressure.
- Diuretics. Promote the removal of excess fluid and harmful substances naturally through urination.
- Synthetic analogues of lactose. They help cleanse the intestines of harmful substances that have accumulated in it due to the development of the disease.
- Antibiotics. Prescribed on the condition that the disease causing varicose veins in the abdomen is caused by pathogenic microorganisms. Antibiotics help destroy them and prevent further development.
All of these medications have a serious effect on the human body and have an impressive list of contraindications. For this reason, you cannot prescribe certain drugs on your own; this can lead to irreparable consequences, especially when treating abdominal varicose veins during pregnancy. Only a doctor should prescribe this or that remedy after the patient has passed all the tests and compiled a medical history.
Treatment
In order for dilated veins in the abdomen to disappear, it is necessary to treat the diseases that caused their appearance. Conservative treatment is indicated in the initial stages, when the problem has not yet started. As the pathology progresses, drug therapy is combined with surgery. Complex treatment helps to achieve a positive therapeutic result.
Medicines intended for patients who have swollen veins in the abdomen:
- Venotonics and angioprotectors are the main drugs for the treatment of varicose veins in the abdomen. Patients are prescribed Detralex, Venoruton, Venarus.
- Drugs that improve blood microcirculation - “Curantil”, “Cavinton”, “Pentoxifylline”.
- Diuretics remove excess fluid from the body - Furosemide, Lasix, Veroshpiron.
- Hormonal drugs regulate the functioning of vascular smooth muscles - Prednisolone.
- Drugs from the NSAID group relieve spasms and general inflammation - Ketorol, Ibuprofen.
- Medicines that improve metabolism - Wobenzym, Phlogenzyme.
- Vitamins of group B, P, C.
- Hepatoprotectors for restoring the function of hepatocytes in liver diseases - “Essentiale”, “Lipoid”, “Karsil”, “Phosphogliv”.
- Thrombolytics for thrombosis - “Streptokinase”, “Urokinase”.
Treatment of pregnant women with varicose veins on the abdomen is more gentle. They are prescribed mainly topical medications - safe gels and ointments with a venotonic effect (basically the same as those used for varicose veins of the legs). Such drugs will not have a detrimental effect on the development of the fetus. In the absence of contraindications, tableted venotonics, including herbal ones, are also used.
In the absence of effect from conservative treatment, surgical intervention is indicated for persons who have pathological dilated veins on the abdomen. Types of manipulations for varicose veins on the abdomen:
vein sclerosisSclerosis of veins that create a cosmetic defect.
- Laser vein obliteration.
- Phlebectomy is the surgical removal of a varicose vein.
- Miniphlebectomy – partial removal of an enlarged vein.
- Stripping - pulling out the inflamed vein through two punctures.
- Ligation - ligation of a vein.
- Transluminal phlebectomy - removal of affected veins by injecting a special liquid.
Surgery is contraindicated for elderly people, patients in the late stages of tuberculosis, pregnant women, patients with decompensated diseases of internal organs, and cancer patients.
Traditional medicine has a huge number of recipes that can improve the condition of patients with dilated veins in the abdomen. The effectiveness of treatment will increase if you combine traditional medicine with traditional:
- Pour a glass of boiling water over a spoonful of crushed dandelion roots, leave for an hour and take the warm remedy internally.
- A decoction of medicinal herbs - nettle, chamomile, rosehip - is taken during the day between main meals. The raw materials are poured with hot boiled water and boiled in a water bath for half an hour.
- Green walnuts are infused in olive oil for forty days and lubricated on the skin of the abdomen.
- Add a teaspoon of apple cider vinegar to a glass of water and mix well. Drink this remedy before every meal. It is also recommended to wipe the skin of the abdomen with this solution.
- Shredded raw potatoes are applied to the affected areas.
- An alcohol infusion of Kalanchoe and birch buds is used to rub the skin of the abdomen.
- Carrot juice mixed with flaxseed oil is taken on an empty stomach for three weeks.
If obvious pathology is not treated, severe complications may develop: thrombophlebitis, and in severe cases, thrombosis and thromboembolism. At the same time, the general condition of the patients worsens significantly: pain, swelling, and periodic convulsions appear.
Surgical intervention
Even during pregnancy, some people perceive varicose veins in the abdominal area as normal, but this is not at all the case. This phenomenon indicates an advanced stage of portal hypertension and is one of the indications for surgical intervention. In most cases, bypass surgery is performed, but in serious situations, spleen removal or liver transplantation may be prescribed.
Specialized medical measures can be taken in relation to dilated veins. These include suturing or ligation of pathological areas, endoscopic sclerotherapy, endoscopic installation of tightening rings and other operations.
Reasons for appearance
Veins on the skin of the abdomen increase in physiological and pathological conditions in the following cases:
- In pregnant women, there is an increase in the veins in the abdominal area if there were previously problems with the legs: varicose veins of the lower extremities. Often capillaries located under the skin or venules can also be called veins. In addition, during pregnancy the veins of the uterus and small pelvis become enlarged. As a rule, such changes are caused by weakening of the vascular wall, hormonal failure, increased stress on the body, irrational food intake and lifestyle;
- Women who constantly lift heavy things, use hormonal medications, as well as females who lead a sedentary lifestyle. With such processes, the functioning of venous stagnation in the small pelvis is observed, which contributes to the appearance of uterine varicose veins and pelvic varicose veins. In males, venous congestion is also observed. However, in men it manifests itself as a result of physical inactivity. This contributes to the appearance of varicocele and decline in sexual functioning as a result of insufficient blood supply;
- Sharp weight loss is accompanied by the release of subcutaneous tissue, through which veins can become visible. If the veins do not protrude and do not have a nodular shape, this is a normal condition of the vessels;
- The appearance of a network of veins in the abdomen is also observed in people who regularly visit gyms. This is especially evident in bodybuilders and strength athletes. The pattern of veins increases during training, because at this moment the muscular basis of the vessel wall develops. The vessels become larger, wider and better visible. This structure does not pose a threat to health, but it spoils the appearance of the body if you suddenly stop exercising, or, conversely, increase the number of workouts;
- Varicose veins can appear as a result of a hereditary tendency, which is expressed by a weakening of the vascular wall, complex cardiovascular diseases;
- The most dangerous process in which this pathology is formed is portal hypertension. This disease is accompanied by an enlargement of the abdominal cavity, ascites, and the appearance of swelling (cap jellyfish syndrome).
Signs of the risk of varicose veins on the skin of the abdomen include sudden weight gain, a hereditary predisposition to the disease, bad habits, and physical inactivity.
In pregnant women, the veins in the skin of the abdomen enlarge due to hormonal imbalance, which is caused by excessive release of progesterone, which can influence androgens and estrogens. During this process, the elasticity of the veins and skin changes, the valves become weaker, the blood stagnates, and the veins enlarge. In the early stages of pregnancy, this process is explained by a sharp increase in weight, and after that – by a sedentary lifestyle.
Important!
You should not self-medicate. At the first symptoms, you should immediately seek help from a medical specialist.
Folk remedies
Traditional therapy is still used in the treatment of many diseases, but in the case of portal hypertension it can only complement the effect of conservative and traditional medicine. Before using any prescription that affects the severity of symptoms, you should consult your doctor, especially for women during pregnancy. There are several most common remedies used for varicose veins in the abdominal area.
First, a dandelion decoction is used, for the preparation of which you need to pour a glass of boiling water into 1 tablespoon of powder prepared from the dried roots of this plant. The resulting mixture should be infused for 10-20 minutes and drunk without diluting with water. The product should be used several times a day in a warm form.
Secondly, beet juice has a good effect; it should be taken 100 ml 2-3 times a day 30 minutes before eating. Thirdly, you can make an herbal mixture consisting of nettle leaves, rose hips, chamomile and yarrow inflorescences, mixed in a ratio of 2:4:2:1. It is necessary to pour 2 tablespoons of the resulting mixture into 0.5 liters of hot boiled water and boil over low heat for 20 minutes. The resulting decoction should be taken 2 tablespoons three times a day between meals.
Other folk remedies may also be used to relieve specific symptoms.
Traditional treatment
To make you feel better, we use our grandmothers’ recipes:
- Prepare the dandelion root (chop it), pour boiling water (a glass) over everything, wait about an hour until the product infuses.
- A decoction of chamomile, nettle, and rosehip helps a lot. Take an equal amount of herbs, add water, and boil for 30 minutes.
- Green walnuts need to be poured with olive oil. Wait 40 days for everything to brew well. Then lubricate the skin.
- Add apple cider vinegar (a teaspoon) to 200 ml of water. Mix everything and drink before meals. The solution is also used to wipe the skin.
- Apply finely chopped raw potatoes to the affected area.
So, veins on the stomach not only spoil your appearance, but can also have a serious impact on your health. Pay close attention to your health!
The content of the article:
Varicose veins are a pathology characteristic of both adults and children. Initially, the appearance of stars and nodules is observed on the body, and then the venous network is already visible.
Varicose veins of the abdomen during pregnancy
Women during pregnancy need to carefully monitor their own health, since any negative manifestations will affect not only her, but also the child. At the first signs of the appearance of varicose veins on the abdomen, you should consult a doctor. The danger is that in advanced cases, in which timely treatment was not carried out or the wrong therapy was used, an artificial termination of pregnancy may be prescribed in order to save the mother.
A pregnant woman with portal hypertension needs to be constantly monitored by a doctor and undergo the necessary tests. Regular monitoring of blood composition, liver and spleen condition is carried out.
At the same time, a woman must be informed about all possible complications for herself and the child during pregnancy and childbirth.
If portal hypertension is not advanced and can be treated, childbirth can proceed without complications. Moreover, due to the nature of the disease, not only obstetricians-gynecologists, but also surgeons and hematologists should be present. Varicose veins, which arise as a result of portal hypertension, are not an absolute indication for a Caesarean section, so in most cases the woman gives birth on her own.
Etiology
Physiological and pathological conditions in which the veins in the abdomen dilate:
translucent but unchanged veins on the abdomen during pregnancy are a normal variantVaricose veins on the abdomen are often observed in pregnant women who have suffered from varicose veins in the legs in the past. Small subcutaneous capillaries (including burst ones), venules and microvasculature vessels are also often mistaken for “veins” on the abdomen. Also, during pregnancy, the veins of the uterus, pelvis and abdominal vessels may dilate. Such changes are usually caused by weakness of the vascular wall, hormonal levels, increased stress on the body and an increase in BCC (circulating blood volume), poor nutrition and lifestyle. The solution is the maximum normalization of factors affecting the patient’s overall health and maintaining a healthy and balanced lifestyle. If a cosmetic defect persists after childbirth, the use of venotonics and treatment in phlebological clinics with modern minimally invasive methods - sclerotherapy, photocoagulation, etc. are indicated.
- The risk group also includes healthy women who regularly lift excessive weights, take hormonal contraceptives, and lead a sedentary lifestyle. Visible spider veins on the abdomen may also appear in them. More dangerous is the possible development of venous stagnation in the pelvis - it is fraught with the development of varicose veins of the uterus and pelvic organs. In men, blood stagnation is also possible, but primarily due to physical inactivity. The result is the risk of developing varicocele, suppression of sexual function due to insufficient blood supply.
- visible veins on the abdomen due to weight loss, which are not a pathology
Sharp weight loss is accompanied by thinning of the subcutaneous tissue, through which the veins are visible, making them very noticeable. If the vessels are simply visible and do not have nodes or protrusions, this condition is normal.
- In children, a pronounced subcutaneous vascular pattern may be perceived by parents as dilated veins. In fact, this is also a variant of the norm or a constitutional feature due to genetic predisposition. If the venous pattern still worries the parents, the child should be shown to specialists who, based on the results of Dopplerography of blood vessels, ECG, ECHO KG, blood tests and coagulogram, etc. will determine the general condition of the cardiovascular system.
- The appearance of a venous vascular network on the abdomen is a characteristic phenomenon observed in women and men who regularly visit the gym. This is especially noticeable among bodybuilders and strength athletes. The venous pattern intensifies during sports, as it develops the muscular framework of the vascular wall. The vessels thicken, become larger and more noticeable. This condition is usually not dangerous, but can spoil the appearance if you suddenly stop training or, on the contrary, with excessive intensity of exercise.
veins in the abdomen that appear during excessive force loads - Obvious primary varicose veins on the abdomen are pathological changes that are accompanied by an increase in the length and saccular deformation of the venous vessels, which often leads to impaired blood flow and valve failure. This may be caused by a hereditary predisposition, severe weakness of the vascular wall, systemic cardiovascular diseases (venous stagnation, cardiac and chronic venous insufficiency).
- The most striking and truly dangerous condition in which clearly visible veins protrude on the abdomen is portal hypertension, accompanied by the “head of the jellyfish” syndrome with a clear enlargement of the abdomen, ascites, and increasing swelling. Among the main causes of portal hypertension are pathologies of the venous bed (for example, thrombosis of the abdominal veins, Budd-Chiari syndrome, appendicular pylephlebitis), diseases of the abdominal organs - cirrhosis of the liver, fatty hepatosis, carbohydrate degeneration of the liver, etc.
pathological veins in the abdomen that occur in dangerous conditions - in particular, portal hypertension
Risk factors or precursors of varicose veins on the abdomen are: obesity, bad habits, physical inactivity, hereditary predisposition, long-term hormone therapy or chemotherapy.
During pregnancy, the veins in the abdomen dilate due to hormonal imbalance caused by excessive secretion of progesterone by the placenta, which affects estrogens and androgens. At the same time, the strength and elasticity of blood vessels and skin changes, valves weaken, blood stagnates, veins dilate. In the early stages, this process is associated with rapid weight gain, and in later stages it is due to a sedentary lifestyle.
Other reasons
Pathological changes in the form of spider veins may be a harbinger of systemic connective tissue damage. Doctors call this disease scleroderma, and it is characterized by abnormal thickening of the skin, leading to poor circulation. The pressure created for the passage of blood through compressed capillaries stretches their walls, forming a kind of vascular “spiders”.
A similar process of formation of telangiectasia is characteristic of diseases associated with the liver and gall bladder. In case of cirrhosis or liver cancer, they appear on the skin of the anterior abdominal wall (“head of the jellyfish”) and indicate sclerosis of the liver structures.
Spider veins can also be caused by other factors:
- cardiovascular diseases;
- decreased vascular tone due to lack of vitamins C and P;
- constant exposure to heat on the body;
- blood clotting disorder;
- hereditary predisposition;
- exposure to UV and radiation on the body.
Significantly increased blood pressure, at which small vessels can simply burst from stress, can also contribute to the formation of single telangiectasias.
The appearance of telangiectasia on the body may indicate the onset of connective tissue damage. In medicine, this phenomenon is called scleroderma and manifests itself in the form of seals on the skin, leading to disruption of normal blood circulation. Spider veins on the abdomen near the liver may indicate the presence of a cancerous tumor.
In most cases, the appearance of spider veins on the body does not cause any inconvenience other than aesthetic ones. The defect is easily eliminated using modern hardware techniques. But still, in addition to the cosmetologist’s office, it is advisable to visit a therapist, who, if necessary, will refer you for examination to specialized specialists.
How to remove
Treatment of telangiectasia on the skin is quite difficult and requires patience. When venous pathology develops, its elimination is required. Patients are advised to attend several therapy sessions to improve the appearance of their skin.
The doctor prescribes a treatment regimen only after determining the cause of the skin problem.
Medicinal methods
The most important component of the drug treatment of asterisks is taking medications containing venotonics, primarily vitamin P.
Rutin preparations have angioprotective, anti-edematous and anti-inflammatory effects.
Products containing rutin are used topically and in tablet form. The course of treatment is at least 4 weeks with periodic repetition throughout the year at least 3 times.
Troxerutin gives a good effect. It relieves the patient of spider veins and lines on the legs and arms.
Troxerutin has a good effect, which relieves the patient of spider veins and lines on the legs and arms.
Troxerutin prevents the formation of telangiectasia. The product eliminates increased fragility of blood vessels and swelling of the extremities. The antioxidant activity of Troxerutin has been proven.
Venorutinol is an effective antivaricose and angioprotective agent for topical use. It is recommended to apply the gel to the affected areas of the skin every day for at least 4 weeks. Other drugs against asterisks:
- Ointment with calendula extract effectively strengthens blood vessels.
- Gel Doctor Wen contains a leech extract, which eliminates blood clots and fights vasodilation.
- Venolife includes active ingredients: dexpanthenol, troxerutin, sodium heparin. All of them prevent the appearance of stars, as well as various manifestations of changes in the condition of blood vessels.
- Lyoton contains heparin, which resolves blood clots and has an anti-edematous effect.
- Venozol is a gel with herbal active ingredients.
Lyoton contains heparin, which resolves blood clots and has an anti-edematous effect.
Folk remedies
There are effective and harmless folk ways to get rid of skin defects at home caused by the formation of capillary lines:
- Cold and hot shower. This is a classic way to train blood vessels, allowing you to remove the mesh and strengthen the capillaries and veins. Showers are taken regularly, starting with a slight temperature difference. It is gradually increased.
- Turpentine baths help improve blood flow throughout the body. The endurance of blood vessels from this procedure increases significantly.
- Green tomato therapy. They are cut and applied to the area of redness for 10 minutes. Mesh therapy on the face is especially effective. After removing the tomato, the skin must be treated with a nourishing cream to prevent burns. The course of treatment is at least 10 days.
- Applying natural apple cider vinegar to your feet several times a day helps remove stars. The course of treatment is 4 weeks.
- Cabbage juice contains a high amount of vitamins and microelements necessary for the body. All of them improve the condition of the walls of blood vessels. It is recommended to drink a glass of juice a day for a month. Sometimes people don't like its taste, you can add carrot juice to the drink.
- Every day you need to consume 1 tbsp. l. olive oil. It significantly improves the strength of the vessel wall and prevents the formation of telangiectasia.
- It is beneficial to consume spinach. The vegetable contains potassium and folic acid, which strengthen capillaries and prevent the appearance of stars.
- Grapefruits are rich in pectin and magnesium. These substances strengthen the vascular wall and myocardium.
- It is useful to consume 1 tsp. grape seed oils.
Radio wave method
Using this method, it is possible to remove stars on the face and other parts of the body without contact. The doctor makes a radio wave incision in the skin and removes the star using high-frequency waves.
The main advantage of the method is almost complete painlessness and high efficiency.
The radio wave method completely eliminates the formation of edema, scars and other types of skin changes.
The disadvantage of this method is that only small capillary networks can be removed. Sometimes the method is combined with laser removal of defects.
Electrocoagulation
The area of pathological skin changes is affected by a thin electrode through which a specially tuned electric current flows.
The electrocoagulation method is associated with the risk of damage to healthy skin. Side effects include scarring, changes in skin pigmentation. Today, the method of electrocoagulation is used less and less. It is being replaced by more advanced methods of removing telangiectasia.
The electrocoagulation method is associated with the risk of damage to healthy skin.
Sclerotherapy
Another name for the procedure is compression phlebosclerosis, which is effective in getting rid of venous networks. A special sclerosing substance is injected into the venous vessels, which seals the walls of the blood vessels.
During the procedure, the patient may experience some soreness, swelling, or swelling.
This is a normal reaction of the body to the medicine. The injection site is treated with ointments and tied with an elastic bandage.
Tight bandaging after the procedure promotes stronger sealing of the vessels. If all steps are done correctly, then the patient will not have any scars or other changes.
The technique is best suited for treating leg veins. It may not be effective on other parts of the body.
Ozone therapy
This method of treating asterisks involves injecting an oxygen-ozone mixture into the blood.
Ozone therapy activates oxidative and reduction processes, which lead to the destruction of the mesh.
The ozone contained in it has high biological and chemical activity. In the affected vessels, oxidative and reduction processes are activated, which lead to the destruction of the mesh.
The technique has a large number of advantages. The main thing is the absence of swelling, scars and other negative phenomena. The introduction of ozone does not cause poisoning; hyper- or hypopigmentation or swelling does not appear at the injection site. The effect after the first procedure is visible immediately and lasts for a long time.
Spider veins on the body: cause and symptoms
Spider veins on the body are manifestations in the form of a thin cobweb that arise due to the thinning of the capillary wall and the penetration of blood through it.
In medicine, the pathological condition is also called rosacea, or telangiectasia. The location of stars on the body can be very different. Most often they are observed on the lower extremities and face, but sometimes they also appear on the skin of the arms, back, chest, and abdomen.
Wherever such elements appear, first of all you need to find out why the stars appear on the body, and only then proceed to choosing a method of elimination.
It is difficult to clearly name the cause of a cosmetic defect. The mechanism for the development of a capillary star on the body lies in the disruption of the functionality of the vascular system, which is accompanied by congestion. However, sometimes rosacea is a purely cosmetic problem and develops against the background of absolute human health.
The following unfavorable factors can provoke the appearance of a capillary network on the body:
- consumption of alcohol, nicotine;
- vascular diseases: venous insufficiency, thrombophlebitis, varicose veins;
- hormonal imbalance that develops during pregnancy, menopause, use of contraceptives, and during puberty in adolescents;
- lifting weights;
- standing on your feet for a long time can cause rosacea on the lower extremities;
- hereditary predisposition;
- obesity;
- exposure to frequent temperature changes, frostbite;
- prolonged exposure to open sun;
- frequent visits to the sauna, bathhouse, solarium;
- congenital defects, in particular, Klippel-Trenaunay syndrome, Louis-Bar syndrome and others.
Against the background of Louis-Bar syndrome, damage to the capillaries of internal organs develops. Therefore, women with this diagnosis are often diagnosed with a vascular network in the uterus, on the external genitalia.
The appearance of such elements on the body is necessarily due to the influence of unfavorable factors. These can be both external irritants and diseases of internal organs that lead to disruption of the vascular system. If spider veins appear throughout the body, consulting a doctor is necessary. With such extensive damage, the patient must undergo a comprehensive examination of the body.
The etiological reason why stars cover the body is a violation of blood circulation. Therefore, the fight against the problem should be aimed primarily at eliminating the root cause.
Couperosis appears only as nets or stars on the body, photos of which are given in this article. The pathological elements do not cause any unpleasant sensations; in rare cases, itching and peeling of the skin may occur.
This manifestation of rosacea occurs most often among patients. In most cases, meshes of such localization indicate the development of varicose veins, chronic venous insufficiency and other vascular ailments. Also, capillary stars can be provoked by prolonged standing on your feet, heavy physical work, and lack of activity.
Removal of pathological lesions on the legs is carried out using various methods, ranging from drug treatment and physical exercise to minimally invasive surgical interventions.
Often rosacea is detected on the lateral surfaces of the thighs; the mesh is red or purple in color and takes the form of lines, dots and tree branches. As a rule, such a manifestation also indicates congestion in the capillaries and requires specialized treatment. Sometimes spider veins on the thighs occur during pregnancy due to the increased load on the lower limbs during this period.
As for treatment methods, they depend on the degree of neglect of the disease. Both surgical and conservative techniques are used. Minimally invasive therapy is contraindicated if telangiectasias developed during pregnancy.
The appearance of red capillaries on the skin of the face is a significant cosmetic defect that almost every patient wants to get rid of. Networks of such localization often develop under the influence of external unfavorable factors, for example, exposure to cold air and sun. Couperosis often affects the cheeks, nose, and less often the chin and forehead.
You can remove the vascular network on the head using different methods. The most effective are radio wave therapy, ozone therapy, photorejuvenation, and laser coagulation. Such techniques do not cause discomfort and are not accompanied by adverse reactions. Spider veins on the lip can be eliminated in one procedure using one of the above methods. If a vascular network has developed in the throat, then only an experienced doctor should select a technique.
The reason for the appearance of telangiectasias of such localization can be very diverse, but in most cases, rosacea is caused by hormonal changes in the body. Spider veins on the neck can appear when using hormonal contraceptives or other drugs that are used to treat endocrinological pathologies.
Treatment should be carried out by a specialist, since the skin in this area is quite sensitive. To remove rosacea, techniques such as radio wave exposure, ozone therapy, and laser coagulation can be used.
Sometimes patients wonder: what causes spider veins on the stomach? The main reason for the development of such a defect on the anterior abdominal wall is diseases of the liver and biliary structures. A red mesh in the form of a “jellyfish head” is characteristic of cirrhosis of the liver. In this case, blood passes through the vessels under high pressure, as a result of which such changes appear.
To cope with the problem, therapeutic measures should be aimed primarily at eliminating the underlying pathology, since telangiectasias are only a consequence of the development of a serious illness.
Pregnancy can also provoke the occurrence of rosacea on the stomach. Venous networks appear due to severe stretching of the skin and damage to small vessels. It is recommended to remove such elements after childbirth.
Why do telangiectasias appear on the skin of the back? It’s not easy to answer unequivocally. A variety of reasons can provoke such an illness. Couperosis with this localization can occur against the background of hormonal imbalance, impaired blood flow, prolonged tanning or staying in a solarium.
Often, spider veins on the back are only a cosmetic defect and do not require serious treatment. It is possible to eliminate such manifestations by using local agents. For example, a good effect is achieved when treating telangiectasias with Troxevasin and Venolife cream.
The appearance of rosacea on the side surfaces of the body is also often only a cosmetic defect and is easily eliminated after the influence of external negative factors on the body ceases.
Also, spider veins on the ribs can be caused by hormonal changes in the body, for example, during pregnancy, puberty, or the decline of childbearing function. In men, it is more difficult to accurately determine the cause of the pathology. Removal is carried out using any of the methods. Laser and radio wave treatment and electrocoagulation are especially popular.
According to statistics, spider veins on the palms occur in every second patient. There can be many reasons for such changes, namely:
- chemical, mechanical or thermal effects on the skin of the hands;
- allergic reactions;
- vascular diseases;
- hypertension;
- history of heart attack or stroke.
Spider veins on the shoulder and arms do not cause discomfort, but they create a significant cosmetic defect. That is why, when telangiectasias appear, many rush to get rid of them. This can be done by electrocoagulation, laser, radio wave removal, or by darsonvalization.
If spider veins appear in the upper part of the body, you should not hesitate to visit a doctor, since there are many causes of the disease. In addition, capillary networks on the chest may indicate the onset of an oncological process in the mammary gland.
If rosacea is at the initial stage of development and there are small lesions on the body, then they can be dealt with by using medications. The following medications are prescribed for the treatment of telangiectasias:
- venotonics: Phlebodia, Troxevasin, Venoruton, Aescusan - they help strengthen the vascular wall and normalize blood flow;
- anti-inflammatory: Lyoton, Indomethacin - indicated in the presence of significant hyperemia and discomfort at the site of the mesh.
Patients are also recommended to take Ascorutin. It strengthens the vascular wall and thereby reduces the signs of rosacea. It can be taken orally in tablets or used topically as an ointment. It is necessary to grind several tablets into powder, mix with baby cream and periodically treat the affected areas with this composition.
If spider veins appear on the arms, ankles or other parts of the body, do not hesitate to contact a specialist. Depending on the location, such changes may indicate serious health problems, so timely treatment will help prevent their progression and the formation of unpleasant consequences.
Ksenia Strizhenko: “How did I get rid of varicose veins on my legs in 1 week? This inexpensive product works wonders, it's a common one. "
Spider veins (telangiectasia) are pathologically altered vessels that are visible through thinned skin. They can be single, or they can merge into a vascular network.
The appearance of spider veins on the body always indicates diseases of the internal organs. The only exceptions are spider veins on the body, which are discovered during pregnancy.
I recently read an article that talks about the drug Choledol for cleaning blood vessels and getting rid of CHOLESTEROL. This drug improves the general condition of the body, normalizes the tone of the veins, prevents the deposition of cholesterol plaques, cleanses the blood and lymph, and also protects against hypertension, strokes and heart attacks.
- consumption of alcohol, nicotine;
- vascular diseases: venous insufficiency, thrombophlebitis, varicose veins;
- hormonal imbalance that develops during pregnancy, menopause, use of contraceptives, and during puberty in adolescents;
- lifting weights;
- standing on your feet for a long time can cause rosacea on the lower extremities;
- hereditary predisposition;
- obesity;
- exposure to frequent temperature changes, frostbite;
- prolonged exposure to open sun;
- frequent visits to the sauna, bathhouse, solarium;
- congenital defects, in particular, Klippel-Trenaunay syndrome, Louis-Bar syndrome and others.
Why are varicose veins dangerous for men?
If the pathology is neglected, in addition to pronounced symptoms, various complications may appear.
Depending on the location, varicose veins can lead to:
- thrombophlebitis, which increases the likelihood of patient death;
- venous ulcers;
- hemorrhages due to rupture of blood vessels;
- infertility;
- mesenteric thrombosis;
- purulent paraproctitis;
- tissue necrosis.
By allowing the disease to progress significantly, a man risks becoming disabled. In severe cases, death cannot be ruled out.
Diagnostics
If the veins on the skin of the abdomen begin to enlarge as a result of the appearance of varicose veins or some other disease, you should seek help from a specialist - a phlebologist or a vascular surgeon. When examining pregnant women, it is also important to contact an obstetrician-gynecologist.
After the patient talks about the symptoms that bother him, the specialist doctor should prescribe a blood test (for general clinical standards, infectious diseases), and an ultrasound examination of the vascular system in order to make an accurate diagnosis.
Main reasons
Stagnation of blood creates increased pressure on the vascular walls, causing the vessels to become deformed and become visible on the surface of the skin. Red meshes indicate damage to the arterioles, and a blue tint indicates an increase in venules. Vascular patterns can take linear, tree-like and stellate forms. Such stars appear on the stomach, back, chest or neck. There are several reasons for this:
- liver diseases;
- genetic characteristics;
- hormonal diseases;
- excessive physical activity;
- cardiovascular diseases;
- deficiency of vitamins P and C;
- age-related changes leading to gradual thinning of the walls of blood vessels;
- alcohol abuse;
- smoking;
- diseases of the vascular system;
- frequent visits to the bathhouse;
- sudden changes in temperature;
- high blood pressure.
The appearance of spider veins on the skin is not only an aesthetic problem. In some cases, burning and itching are added to the external symptoms. Pain occurs quite rarely; most often, painful telangiectasias appear not on the body, but on the legs.
- liver diseases;
- genetic characteristics;
- hormonal diseases;
- cardiovascular diseases;
- deficiency of vitamins P and C;
- age-related changes leading to gradual thinning of the walls of blood vessels;
- alcohol abuse;
- smoking;
- diseases of the vascular system;
- frequent visits to the bathhouse;
- sudden changes in temperature;
- high blood pressure.
Varicose veins in men: enlarged veins, does it happen, treatment, on the stomach, causes, signs, symptoms
According to statistics, a tenth of patients who turn to gynecologists complain of pelvic pain. Female misfortune Varicose veins of the small pelvis occur in both men (varicocele - dilatation of the veins of the spermatic cord) and women. Moreover, the latter suffer three times more often.
And if in the first case varicose veins are relatively easy to diagnose (the problem, as they say, is in plain sight), then in the second it is much more difficult. In women, this pathology is “hidden” inside. “Pelvic varicose veins are a violation of venous blood flow, stagnation of blood in the pelvis,” comments Mikhail Khotchenkov, director of the regional Center for Microsurgery.
— Its clinical manifestations are quite diverse. The leading symptom is the occurrence of chronic pain in the lower abdomen. The patient characterizes these pains as pulling, aching, dull, burning, radiating to the lower back or legs. Women also complain of painful menstruation, frequent urination and pain during sexual intercourse.
The problem with such varicose veins, according to the vascular surgeon, is that many diseases, including infectious ones, occur with a similar “picture”. Therefore, it is sometimes difficult for gynecologists to make an accurate diagnosis, and they begin to look for the reasons for this feeling. For example, they treat women for infections and inflammation of the appendages by prescribing antibiotics.
Or they prescribe hormonal drugs to correct hormonal disorders, such as ovarian cysts or uterine fibroids. And with pelvic varicose veins, such treatment can only worsen the situation. Because the same hormones contribute to even greater blood thickening and exacerbation of varicose veins. But this problem cannot be ignored.
Because it is the pelvic veins that are one of the main sources of thrombus formation. In addition, venous stasis can lead to obstetric disorders: infertility, miscarriage and termination of pregnancy. Occlusion versus varicose veins Enlarged varicose veins are clearly visible during routine pelvic ultrasound.
After an accurate diagnosis is made, treatment begins. Depending on the stage of varicose veins, one or another method is chosen. At the initial stage, taking medications to thin the blood and agents that strengthen the walls of blood vessels helps. If the disease is already in the acute stage or has become chronic, then you will have to resort to surgical methods.
For example, using laparoscopy, “ligate” diseased veins, that is, completely block the blood flow in them. “Today we offer an alternative method of treating varicose veins of the small pelvis - intravascular occlusion of the ovarian vein,” continues Mikhail Vyacheslavovich. - This is not an operation, but rather a procedure.
Just as with UAE, under the control of an X-ray machine, the vascular surgeon makes a puncture in the groin area and inserts a catheter into the venous bed. Through it, a nitenol or steel spiral is installed into the lumen of the vein, which blocks the blood flow in the affected area.
Its size depends on the diameter of the varicose vein and ranges from eight millimeters to one and a half centimeters. Sometimes a gluing agent, a sclerosant, is injected into the lumen of the diseased vein. It burns the vein wall from the inside, and it sticks together. But in our center they use metal spirals.
According to the surgeon, intravascular occlusion of the ovarian vein is a virtually painless procedure and is performed under local anesthesia. In its nature, it resembles uterine artery embolization, but with the difference that the specialist works with the ovarian rather than the uterine venous bed. At the same time, blood circulation in the lower abdomen does not stop.
The work of the “blocked” vessels is taken over by neighboring veins.
CAUSES OF VARICOSIS: congenital weakness of the venous wall, vascular defects, impaired elasticity of the muscle layer, insufficiency of valves, venous thrombosis, frequent constipation, compression of the pelvic veins by a tumor or large fetus, bending of the uterus for a long time, long-term use of oral contraceptives if there are already dilated veins in the legs or hemorrhoids are diagnosed, flat feet, heavy physical labor or long stay on your feet (surgeons, hairdressers, waitresses) sedentary lifestyle * * * Test yourself If you observe symptoms of varicose veins of the small pelvis, arrange a test. Lie on your back with a pillow under your butt and lie there for 15-20 minutes. If the pain in the lower abdomen has gone, it means that you may indeed have problems with the blood supply to the vessels of the small pelvis.
Age category of materials: 18+
- Larisa Makovetskaya.
- Amurskaya Pravda dated 10/25/2007
The benefits of ointments and creams for varicose veins
The therapeutic value of such drugs is determined by the substances they contain. Therefore, before using an external remedy, you should consult a doctor.
To obtain the maximum effect, it is better to use ointments at the first manifestations of the disorder.
Thanks to them:
- fatigue, painful discomfort and swelling go away;
- blood vessels become stronger;
- small blood clots dissolve;
- the skin is moisturized;
- muscle and vascular tone increases.
The use of the cream is prohibited for patients with:
- trophic ulcers, open skin lesions;
- individual intolerance to components.
Some phlebologists confidently say that external medications are absolutely useless for varicose veins. They claim that if the veins are stretched, the situation can only be corrected through surgery.
Treatment methods
When treating ARVMT, the following tasks are set:
- normalize vascular tone;
- improve tissue nutrition;
- prevent stagnation and possible complications.
Treatment of varicose veins of the pelvic vessels can simultaneously proceed in several directions, while surgical intervention is necessary only at stage 3 of the disease .
| Medical direction | Specific events |
| Non-drug therapy |
|
| Drug therapy |
|
| Surgical intervention |
|
| Treatment with traditional methods | use of herbal remedies based on dandelion, chaga and horse chestnut |
Find out more about the treatment of pelvic varicose veins in another article.