Eye diseases today affect 60% of the population. If the symptoms of some pathologies can be detected in the early stages, through experiencing unpleasant sensations, then some anomalies are painless, which makes their timely diagnosis difficult.
Despite this, these types of diseases are not at all harmless and can lead to lasting consequences.
Eye retinopathy is one of these pathologies, which involves the destruction of retinal vessels, leading to problems in the blood flow of the retina. Let's look at the concept of a disease, its types and symptoms, and talk about diagnostic methods and therapy.
The essence of pathology
Retinopathy is an abnormal deformation of the retina caused by destruction of the retinal vessels. Disruption of blood flow in the retina causes its changes, which subsequently has the risk of leading to nerve dystrophy.
As a result, a person may completely lose vision. The danger of the anomaly lies in its painless course, which makes timely diagnosis difficult.
The concept of retinopathy includes quite a few ophthalmic eye diseases. The anomaly affects the patient's visual system from infancy to old age, regardless of gender. Retinopathy is mainly provoked by the presence of other problems in the functioning of the human body, but there are cases of spontaneous development of an anomaly.
| Previously, the disease was characterized as a sudden onset of blindness, manifested as a result of trauma to the skull. |
Primary type of pathology
The group includes changes in the retina that are not accompanied by an inflammatory process. Deformations have not yet been fully studied by specialists. The cause of the lesions often cannot be diagnosed even after a thorough examination of the patient's health status.
The disease has 3 types:
- Central serous;
- Acute posterior multifocal pigment epitheliopathy;
- External exudative.
To fully understand the picture of the disease, each subtype of anomaly should be characterized in detail.
Central serous
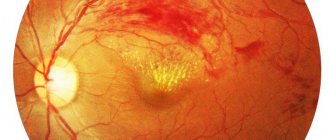
A form of retinopathy manifested as retinal detachment in the macular area. The pigment epithelium of the macula is affected, forming a darkish oval-shaped edema. The disease involves a temporary deterioration in the ability to clearly perceive objects.
Most often, the pathology is localized only in one eye. The anomaly predominantly affects men in the age range from 20 to 40 years.
Precursors to the onset of pathology are chronic stress and headaches for a long time.
Acute posterior multifocal pigment epitheliopathy
The disease consists of lesions of a grayish hue and a flat shape, formed under the influence of a large number of hemorrhages under the retina. Vitreous opacities and inflammation around the iris are often diagnosed. The pathology is located in both one and both eyes.
External exudative
A form of retinopathy is characterized by the presence of accumulations of blood located between the retina and the apple of the eye. They are generated due to the abnormal development of retinal vessels. At the site of the rupture, connective tissue begins to grow, accompanied by disruption of the visual system.
External exudative retinopathy is diagnosed in men under 30 years of age. Mainly one eye is affected.
| Abnormal development occurs slowly and often leads to complete loss of vision. |
What is the danger of retinopathy?
Eye retinopathy is a dangerous disease that, if not treated in a timely manner, leads to irreversible changes in the structure of the retina, causing vision loss. Damage to the retinal vessels in adults without adequate therapy can lead to the following serious complications:
- inflammatory processes;
- loss of visual fields;
- violation of the outflow of intraocular fluid;
- increased intraocular pressure;
- vein thrombosis;
- cataract;
- vitreous deformation;
- blockade of retinal vessels;
- episcleritis;
- iridocyclitis;
- hemophthalmos.
Any form of retinopathy at an advanced stage can lead to atrophy of the optic nerve and retinal detachment, which in turn provokes the development of blindness. Secondary forms of pathology also provoke aggravation of the underlying pathology, negatively affecting the overall health.
Retinopathy in children
Retinopathy in children can lead to the following negative consequences:
- astigmatism;
- myopia;
- strabismus;
- cataract;
- reduction in the size of the eyeball;
- underdevelopment of the optic nerve.
The development of such complications can be prevented if you consult a doctor in a timely manner and undergo a course of adequate therapy.
How to treat this pathological process? Treatment of retinopathy depends on the cause of its origin and can be conservative or surgical.
Author of the article: Kvasha Anastasia Pavlovna, specialist for the website glazalik.ru Share your experience and opinion in the comments.
Secondary type of pathology
A type of retinopathy that occurs together with other diseases in the human body. Often the pathology develops in people who have:
- Eye injury;
- High blood pressure;
- Diabetes type 1 and 2;
- Bruises and fractures of the chest;
- Systemic atherosclerosis;
- Toxicosis;
- Blood diseases.
Let's consider the types of pathologies of the secondary group
Atherosclerotic
It is formed due to a lack of oxygen in the blood vessels. The result is damage to the retina. Character for patients diagnosed with atherosclerosis. Untimely treatment of the disease provokes atrophy of the eye nerve.
Hypertensive
Formed due to deformation of the retina caused by high blood pressure. Due to the compression of small arteries located in the fundus of the eye, rupture and leakage of fluid occurs.
Hypertensive retinopathy is typical for patients suffering from high blood pressure and renal failure. Often affects pregnant women during toxicosis.
| The disease of this form is common and has consequences in the form of a stable deterioration in the ability to clearly perceive objects, up to complete blindness. |
The pathology occurs in 4 stages:
- Agniopathy (beginning of the course of the anomaly);
- Agniosclerosis (damage to the eye vessels);
- Retinopathy (swelling of the retina);
- Neuroretinopathy (nerve swelling, retinal detachment).
Diabetic
A form of retinopathy that affects people with type 1 or type 2 diabetes. Other causes of the abnormality are excess weight, anemia, nephropathy and hypertension. The disease involves loss of elasticity of the blood vessels in the eye and retinal hemorrhage.
The diabetic form of the disease can lead to complete loss of vision if not treated promptly.
Pathology has a three-stage development:
- Background (dilatation of retinal veins);
- Preproliferative (formation of small and medium-sized hemorrhages);
- Proliferative (changes in the vitreous body).
Retinopathy caused by diseases of the circulatory system.
Occurs against the background of various circulatory pathologies:
- Anemia;
- Leukemia;
- Myeloma;
- Bone marrow tumor.
| Each of the subtypes of the disease is characterized by its own clinical picture, but they are all united by the possibility of complete loss of the ability to see. |
Traumatic
It is formed against the background of a strong shaking of the apple of the eye as a result of sudden compression of the chest. Due to compression of the arteries caused by injury, hypoxia forms in the tissues of the retina. From the point of view of ophthalmologists, the pathology looks like a white clouding localized on the side of the affected area or on the other side of the eyeball.
| Often this type of pathology leads to atrophy of the eye nerve. |
Postthrombotic
Occurs due to eye injury, tumors and the development of glaucoma. The pathology manifests itself some time after thrombosis of the vessels that provide blood flow to the retinal area. The result is severe damage to the retina, resulting in significant loss of clear vision.
The postthrombotic form of the pathology is diagnosed in older people with hypertension and coronary artery disease.
Return to contents
Background retinopathy in blood diseases
Blood diseases accompanied by retinopathy include polycythemia, myeloma, anemia, leukemia, etc. At the same time, retinopathy has a certain specific clinical picture. For example, if the pathology occurs against the background of polycythemia, examination of the fundus reveals a particularly bright color of the veins (rich red color), and the fundus has a cyanotic tint. There are signs of vascular thrombosis, as well as papilledema.
In case of anemia, the fundus of the eye is pale, the vessels are pathologically dilated. Retinopathy occurs with frequent hemorrhages (hemophthalmos) under the retina or into the vitreous body. Often the condition of the retina is complicated by a “wet” type detachment.
When retinopathy occurs against the background of leukemia, high vascular tortuosity, swelling of the retina and optic nerve head, small hemorrhages, and accumulation of exudate under the retinal tissue are observed.
Multiple myeloma, like Waldenström's macroglobulinemia, can be accompanied by dilation of retinal vessels (veins and arteries) due to blood thickening, blockage of veins, the appearance of microaneurysms and hemorrhages under the retina.
Treatment of background retinopathy in blood diseases consists of compensating for the malignant process of the underlying pathology and performing a laser coagulation procedure of the retina. The prognosis for the outcome of the disease is usually unfavorable.
Retinopathy of prematurity
The second name is “fibrolental dysplasia”. The anomaly progresses due to the underdevelopment of the eye structure during gestation. It mainly manifests itself in premature babies weighing 1500 grams, who are in incubators for 1-2 months. The reason for the progression of the disease is the excessive level of oxygen that the child breathes.
The anomaly appears on days 14-21. The pathology may disappear on its own or negatively affect the quality of the baby’s vision.
Symptoms
Retinopathy, depending on its type and form, has its own symptoms. The central serous form manifests itself in the form of a decrease in the visual area covered by the eye, involuntary distortion of the dimensions of objects, the appearance of invisible areas in the horizon, and a decrease in the functions of the visual apparatus.
| In the case of using lenses with a slight plus, the quality of the ability to clearly see objects is noticeably improved. |
Symptoms of acute posterior multifocal retinopathy are impaired central vision and the presence of blind spots in the horizon. As the pathology progresses, damage to the veins and swelling of the optic nerve appear.
Signs of hypertensive retinopathy:
- Compaction of the walls of the fundus vessels;
- Deterioration in the ability to clearly see objects and objects;
- Retinal disinsertion;
- Scotomas;
- Venous deformations of the eye.
| The same symptoms appear in the atherosclerotic form of the disease. |
Diabetic retinopathy initially makes itself felt by deteriorating visual acuity, the appearance of fog in the vision, and spots before the eyes. The patient experiences discomfort when reading and working with small objects.
| At the third stage of development of the disease, a complete loss of the ability to see occurs. |
Other symptoms of diabetic form:
- Hemorrhage in the optic organ;
- Deformation of the apple of the eye;
- Increase in glial cells.
Retinopania, caused by pathologies in the circulatory system, manifests itself in the formation of blood clots in the veins located in the retina and its detachment, vasodilation, swelling of the optic disc.
The traumatic form of the disease has its own symptoms:
- Hemorrhage;
- Decreased ability to see;
- Spasm of arterioles;
- Retinal clouding.
Postthrombotic retinopathy makes itself felt by decreased quality of vision and acute retinal hypoxia, as well as hemorrhages in this area.
| If not treated in a timely manner, the pathology leads to complete loss of vision. |
Causes of retinitis pigmentosa
Retinitis pigmentosa, also known as pigmentary abiotrophy, is one of the degenerative diseases of the retina of the eye that is hereditary in nature. This pathology is accompanied by the occurrence of severe visual impairment and most often ends in complete blindness.
This disease has been known since ancient times as one of the causes of complete loss of vision at different ages. However, its name, “retinitis pigmentosa,” was proposed by the Dutch ophthalmologist F. Donders in 1857. The development of scientific thought and the emergence of genetics made it possible to prove that this disease includes a whole set of retinal pathologies with similar pathogenesis and completely different etiology.
To date, several dozen genes have been identified that, in hundreds of mutations, can lead to retinitis pigmentosa. The mechanism of inheritance of this disease is also different. Currently, autosomal dominant forms of the pathology, autosomal recessive, and X-linked forms have been described. The latter include both recessive varieties (only men are carriers) and dominant varieties (when both sexes are affected).
The incidence of retinitis pigmentosa in the population is on average approximately 1 case per 5 thousand people. Moreover, some forms of the disease are more common, others are very rare. There are medical statistics according to which almost 100-120 million people on the planet are carriers of genetic abnormalities (including asymptomatic carriers).
Due to the genetic heterogeneity of retinitis pigmentosa, the etiology of the disease is very diverse. Today, a huge number of its forms are known, which is caused by mutations of various genes. However, it has been reliably proven that the cause of its occurrence is metabolic disorders in the pigment epithelium and photoreceptors of the retina, which lead to the accumulation of decay products and harmful toxins.
How to find out about the disease?
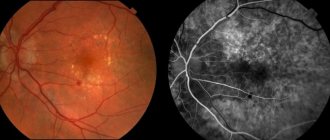
Diagnosis of retinopathy is primarily expressed in a visual examination of the eye for deformations. Ophthalmoscopy is also used to identify pathological changes in the area of the eyeball. Already at this stage, a competent doctor will be able to diagnose retinopathy.
If the presence of the disease is suspected, the patient may be referred for OCT and electrophysiological studies to carefully study the deformities. As prescribed by the ophthalmologist, you should visit a number of other doctors: endocrinologist, cardiologist, therapist and others.
If you have concomitant diseases - diabetes mellitus, atherosclerosis, etc., be sure to visit an ophthalmologist for a preventive examination of the vision apparatus.
To make a diagnosis and combat the disease, comprehensive treatment of both ophthalmological and other pathologies in the patient’s body is required.
Return to contents
Prevention of various forms of retinopathy
Retinopathy can be prevented through regular preventive screenings. Patients with hypertension, diabetes mellitus, atherosclerosis, kidney and blood diseases, those who have suffered injuries and pregnant women need medical supervision by an ophthalmologist.
Prevention of retinopathy in infants involves proper management of pregnancy, especially in women at risk for premature birth. Children who have had retinopathy should have an eye examination annually until age 18.
Sources used:
- Kvasova M. D. Vision and heredity. - Moscow / St. Petersburg: Dilya, 2002.
- Diseases of the lens of the eye in children / A.V. Khvatova. - M.: Medicine, 1982.
- Pediatric ophthalmology. In 2 volumes. Volume 1 / Craig S. Hoyt, David Taylor. - M.: Panfilov Publishing House, 2020.
- National Eye Institute
Therapy
Treatment of retinopathy begins with eliminating its root causes. In the presence of diabetes, the emphasis is on reducing glucose. Hypertension requires normalization of blood pressure. Patients are prescribed medications aimed at strengthening the blood vessels of the eye, stabilizing blood circulation and metabolism in the tissues of the eye.
| It is recommended to take a vitamin-mineral complex. |
In severe forms of the disease that have a risk of causing retinal detachment, patients are advised to undergo laser coagulation. If this happens, then treatment is carried out surgically.
It is not possible to overcome the disease with folk remedies, but some methods can help improve the symptoms that appear.
For example, for diabetic retinopathy, it is recommended to take 1 glass of nettle juice daily. To normalize metabolism and obtain a complex of vitamins, you can drop 2-3 drops of aloe juice into your eyes.
| Remember that before self-treatment, you should definitely consult your doctor. |
Diagnosis of the disease
Diagnosis of the disease includes visits to several highly specialized specialists - ophthalmologist, neurologist, cardiologist, endocrinologist. The attending physician writes out a referral for a comprehensive examination, which is carried out using high-precision equipment. Ophthalmology offers the following methods:
- visual acuity test;
- perimetry - study and analysis of the visual field;
- tonometry - measurement of intraocular pressure;
- electrophysiological study, which helps determine the level of viability of the nerve cells of the retina and optic nerve;
- laser scanning of the retina;
- ultrasound examination of the internal structures of the eye;
- ophthalmoscopy - examination of the fundus of the eye, which helps to accurately assess the condition of the retina and retinal vessels, as well as the vitreous body;
- fluorescein retinal angiography.
Diagnostics is selected for each patient individually based on anamnesis and examinations performed.
Patients suffering from diabetes are examined every six months. Women during pregnancy - once every trimester. For children, an examination by an ophthalmologist is mandatory at the age of one month and then every two weeks until the retina completes its formation.
Preventive actions
First of all, measures to prevent the risk of developing the disease should be aimed at ensuring that the body receives a sufficient amount of vitamins and minerals. To prevent primary type retinopathy, you should avoid stress and chronic fatigue, and also do not ignore frequent headaches.
To reduce the risk of the secondary group, you should pay special attention to the treatment of concomitant diseases and avoid injury to the chest and visual organs.
Proper nutrition, an active lifestyle, weight control and proper rest will help prevent the development of other pathologies that can cause ophthalmic diseases.