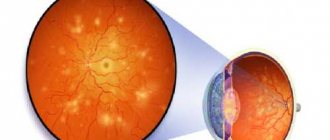
Uveitis – this is not just one disease, but a whole complex of them. This pathology means an inflamed uveal tract - the so-called choroid of the eyes.
What kind of disease is this?
Among eye lesions with an inflammatory course, uveitis is diagnosed in almost half of the cases.
Uveitis: photo
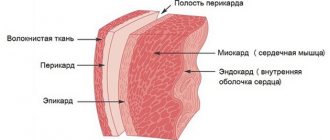
Anatomically, the uveal tract is considered the middle layer of the eye and is located under the sclera. Its structure is formed by the iris, ciliary (ciliary) body and choroid (choroid):
Uveal tract of the eye
ICD-10 code
The international classification classifies uveitis as diseases of the eye and its adnexa (classes H00-H59), diseases of the sclera, cornea, and iris of the ciliary body (classes H15-H22).
Uveitis belongs to class H20.0 , which stands for acute and subacute iridocyclitis. In addition to uveitis, this group includes cyclitis and iritis.
Causes
There are many possible factors for the development of uveitis:
- infection;
- impaired metabolism;
- burn;
- hypothermia;
- reduced immunity;
- autoimmune pathology;
- penetrating trauma;
- psoriasis;
- virus (hepatitis, cytomegalovirus, etc.);
- chronic diseases (for example, diabetes);
- consequences of surgery;
- systemic inflammatory process.
Uveitis in children most often occurs:
- after injury;
- for infections;
- against the background of impaired metabolism or weak immunity;
- with acute allergies.
Video:
Classification
Uveitis is classified according to several criteria:
Localization
To distinguish uveitis by location, they are divided into anterior, median, posterior and generalized.
- Anterior uveitis, meaning pathology in the anterior parts of the uveal tract, respectively, includes iritis, anterior cyclitis and iridocyclitis. It is in this vein that the disease manifests itself more often. Inflammation affects the iris and ciliary body.
- Median inflammation is also known as intermediate inflammation. Posterior cyclitis, parsplanitis and peripheral uveitis are attributed to it. In this clinical picture, not only the choroid is affected, but also the retina with the vitreous and ciliary body.
- Posterior uveitis affects the retina, optic nerve and choroid. This type of inflammation may mean choroiditis, chorioretinitis, retinitis or neurouveitis.
- generalized occurs , that is, panuveitis.
Nature of inflammation
According to the nature of the inflammatory process, it can be of the serous, fibrinous-lamellar, purulent, hemorrhagic or mixed type.
Causes
The causes of uveitis are exogenous and endogenous .
- An exogenous disease means that its causes are external. Usually this is an injury, a burn, or an unsuccessful operation.
- Endogenous causes of inflammation mean that it was caused by internal factors, such as infection.
Depending on the causes of occurrence, uveitis can be primary or secondary . Primary inflammation occurs independently, and secondary inflammation occurs against the background of another ophthalmological disease (as a complication).
Features of the course
According to the time course, uveitis is acute, chronic and recurrent.
- Acute lasts no more than three months.
- A longer duration of inflammation means chronic uveitis.
- recurrent when it occurs again after complete recovery.
Mechanism of development and typical pathogens
The basis for the development of a pathological process is damage to the structures of the eye or two at once by infectious agents.
There are many options here. Bacteria are not always involved, although they make up the bulk of pathogens.
- The likelihood of damage to the choroid is especially high in the presence of sexually transmitted agents, such as syphilitic spirochetes, gonococcus, when they enter the structures of the optic tract.
- Slightly less common are infections by viruses (herpes as one of the leaders, others), and fungi (candida).
- A disorder due to parasitic eggs entering the eye tissue is also possible. Helminthiases of this kind are not as rare as you might think.
- Flukes are especially dangerous in this regard. The so-called opisthorchiasis. Most often, the disease develops in people who do not disdain raw or insufficiently heat-treated river fish.
Normally, a certain number of infectious agents of different types are present in the eye of any person.
The body is able to keep foreign aggressive structures in check and does not allow them to become active. But as soon as you give your immune system some slack, the problem immediately becomes actualized.
Thus, the basis of the mechanism of uveitis is a dual process: damage to the structures of the choroid by an infectious agent, as well as a decrease in local immunity with a drop in blood flow speed, deterioration of microcirculation and general defenses, and inability to give an adequate response.
There is another option. Although uveitis is an inflammatory pathology in all cases, it is not always infectious.
There is a non-septic variety - autoimmune. As the name suggests, the process develops as a result of a spontaneous failure of the patient’s body’s defenses.
Often does not become a primary lesion. It turns out to be a secondary pathological process against the background of rheumatoid arthritis, psoriasis, and systemic disorders of an autoimmune nature.
Taking control of this condition is more difficult than an infectious one, because there is a tendency for frequent relapses. Long-term, complex treatment and adherence to the doctor’s lifestyle recommendations are required so as not to provoke exacerbations.
The mechanism is being studied to develop a clear strategy to help preserve vision.
Classification
The division of the pathological process is possible according to different criteria; all typing methods are used by practitioners to describe the disorder, its precise coding according to the classifier, specifying the diagnosis and identifying a clear vector for medical correction of the condition.
Uveitis can be divided according to its origin:
- Primary. As an independent disorder. For example, after an infectious disease, due to a decrease in general and local immunity. It is relatively rare. Such cases account for up to 25% of the total clinical situations.
- Secondary. Particularly common. It is defined as uveitis formed as a result of other eye diseases. Even banal conjunctivitis, as well as minimal trauma, can play a role here. For example, a cut or scratch to the organ of vision while performing duties, interacting with animals, etc.
Both options are equally dangerous.
Depending on the location, a large group of pathologies is distinguished. It must be borne in mind that the uveal tract “stretches” over the entire eye and is represented by a group of structures: the ciliary (ciliary) body, the iris, and the choroid (choroid).
Based on anatomical features, three regions are distinguished: anterior, median and posterior, which is closest to the retina and optic nerve.
Anterior uveitis
This includes two types of inflammation:
- Iritis. Inflammatory lesion of the iris itself. In isolated form, it is extremely rare due to the general innervation and local circulatory system with surrounding structures. Identification is difficult and requires a comprehensive assessment.
- Iridocyclitis. A much more common problem. In addition to the iris, part of the ciliary body is involved. Without quality medical care, it quickly leads to the formation of adhesions, areas connected to each other by special fibrin strands that prevent the eye from functioning normally.
These two forms are variants of damage to the anterior region of the uveal tract.
Complications
With untimely or inadequate treatment, various complications of uveitis can develop:
- Secondary glaucoma;
- Cataract;
- Overgrowth of the pupil and changes in the structure of the lens;
- The appearance of synechiae (adhesions), leading to disruption of the normal circulation of tear fluid;
- Persistent vitreous opacification;
- Damage to optic nerve tissue;
- Neovascularization (pathological proliferation of blood vessels) of the retina, which ultimately leads to retinal detachment.
Middle type
Regarding the middle structures:
- Posterior cyclitis. The ciliary body has an oblong shape. Covers the eye beyond the initial sections. Otherwise, the pathological process is practically no different from its “brother”, except for the lower intensity of the symptoms, and even then not always.
- Peripheral uveitis. Accompanied by damage to the ciliary body and choroid - the choroid located in the back of the eye: this structure nourishes the retina. If damaged, there is a high risk of catastrophe and complete loss of the ability to perceive visual information.
Prevention of uveitis
Uveitis, the symptoms and treatments for which are described above, can be prevented. In order to reduce the likelihood of developing the disease to a minimum, the following recommendations must be followed:
- observe the work and rest schedule, do not overstrain your eyes;
- When working at a computer, take periodic breaks and give your eyes a rest;
- avoid hypothermia;
- increase the body’s immune defense, engage in hardening;
- observe the rules of hygiene;
- do not injure the eye;
- avoid the development of allergic reactions;
- promptly sanitize foci of chronic infection in the body and treat eye diseases;
- periodically undergo preventive examinations with an ophthalmologist for early diagnosis of possible eye diseases, which significantly facilitates subsequent treatment and significantly improves the prognosis.
Health to you!
Posterior uveitis
The most dangerous lesions of the posterior part of the organ of vision seem to be:
- Choroiditis. The actual involvement of the choroid in a poorly visible area. Diagnosis is difficult due to the unfortunate location and lack of pain, as with damage to the same ciliary body. Therefore, spontaneous and sluggish development of uveitis is possible, a decrease in visual acuity and a visit to the doctor, when little can be done to help.
- Chorioretinitis. An even more dangerous variety. In addition to inflammation of the choroid, the retina is also involved in the disorder. In such a situation, the probability of its detachment is enormous. The disease requires hospitalization and constant monitoring in order to prevent irreparable things or quickly take corrective measures.
- Retinitis. It is quite rare, if we talk about an isolated inflammatory form, only the retina is affected.
- Neuroveitis. It is a lesion of the optic nerve structures. This option is no less dangerous than the previous ones. Because disc degeneration in the fundus leads to a rapid and irreversible decrease in visual acuity.
As a “bonus”, the patient receives adhesions, areas of vascular degeneration, which leads to a decrease in the intensity of nerve nutrition and the constant preservation of decreased vision.
A more general classification based on the same criterion is also possible:
- Posterior uveitis. It carries a much greater danger in terms of critical complications due to the proximity of important anatomical structures: the retina and the nerve disc. Restorative measures are always carried out in the hospital in order to notice negative changes in time and adjust the course of treatment.
- Anterior uveitis. Damage to the iris or ciliary body. A complex process is possible. Despite the relatively lower risks, it is also not recommended to delay consulting a doctor. Because it is possible for the lens to become clouded and involve the retina and choroid in distant parts in the disease.
- Panuveitis. As the name suggests, the anterior and posterior sections of the tract are affected simultaneously.
There are acute and chronic variants of the disease.
There are other ways to classify the pathological process: by the nature of the course, by the type of predominant changes in the choroid. But they are of greater interest to doctors. Little understood by patients.
They are used to assess the severity of the pathological process and develop treatment tactics.
Dispensary observation
Patients suffering from inflammation of the choroid need to undergo regular medical examination. A patient who has already been diagnosed with uveitis should undergo annual medical monitoring.
Purpose of medical examination:
- full examination;
- control of the course of uveitis;
- relapse prevention;
- carrying out preventive measures.
Patients with a previous acute form of uveitis need medical supervision to avoid the development of complications and correct further lifestyle.
Symptoms and signs
The clinical picture depends on the type of disorder and the location of the disorder. However, some common features can be identified:
- Pain syndrome in the eye area. A serious reservation needs to be made here. The intensity of discomfort depends on the specific location of the inflammatory process. So, the iris, and especially the ciliary body, react most actively, so the intensity of the pain will be extremely high.
At the same time, the retina and posterior structures are practically incapable of causing such discomfort. Other manifestations need to be assessed.
- Tearing. Increased secretion production is due to the body’s attempts to get rid of a foreign object, waste products of bacteria. In this regard, redness of the white of the eye is also detected, a change in its shade to pale, cloudy.
- Photophobia. The patient should not be outdoors or in high-impact areas.
- The most characteristic symptoms of ocular uveitis of any localization are decreased visual acuity and a feeling of fullness, a foreign body somewhere inside. The drop in image quality varies.
The more intense the inflammatory process, the worse the situation is.
Attention:
Damage to the posterior portion, retina, or nerve generally leads to rapid deterioration, up to complete blindness within a matter of days.
- Stable glaucoma. Or the development of such attacks. With jumps in the tonometer reading in the eye. The increase in pressure is due to an increase in the amount of fluid produced when its drainage is disrupted naturally due to edema.
The drainage system is not working well and requires outside help to restore it. If the condition is not normalized, an additional damaging factor will arise and degeneration of the optic nerve will begin.
- Change in pupil size, unequal width when visually assessed on both sides (anisorchia). Atypical manifestation. May be missing.
- The same optional, optional sign is a change in the color of the iris. Its lightening. As bleeding develops, the area may fill with blood, which is clearly noticeable even during a routine examination.
There are also specific manifestations. For example, when the posterior parts of the choroid and retina are damaged, scotomas appear; they look like black spots, static, covering part of the picture.
Attention:
These areas of loss of the visual field may also indicate detachment, so you need to carefully monitor your own sensations.
The number of floating opacities increases, which look like spirals, skeins of translucent color, worms, cobwebs. Flickering floaters also occur spontaneously.
Photopsies are possible - false light images, lightning flashes in the form of dots, lines, simple geometric shapes in the field of view. This is the result of irritation of the retina.
Causes
Partially the issue has already been addressed. There are two main provocateurs: the penetration of infectious agents of a certain type into the structures of the eye, a decrease in local and general immunity, often in the system.
In addition, a drop in blood microcirculation is detected. In addition, an autoimmune process is possible. Negative reaction of the body to its own cells.
If we talk about provocateurs in more detail, such a result, the formation of one or more of these moments can lead to:
- Peak hormonal states. Puberty, the beginning of the menstrual cycle. Especially pregnancy. Transition to menopause to a lesser extent.
- Allergic reactions.
- Endocrine diseases and metabolic problems. Diabetes mellitus plays a special role as a pathology that primarily affects the vascular system everywhere, regardless of location.
- Traumas suffered in the recent past. A certain role belongs to pathologies such as hypertension or a symptomatic rise in blood pressure.
The causes of uveitis are determined by damage to the eyes by infectious agents or the immune response to false threats as a result of third-party pathologies: from rheumatoid arthritis to psoriasis and lupus erythematosus.
Knowing this, it is possible to develop high-quality general methods for preventing the disorder.
Causes of uveitis in adults and children
The most common (up to 45%) are infectious uveitis. Diseases that are associated with the circulation of microbes and viruses in the blood can be complicated by damage to the eye membranes. The most common among them are:
- tuberculosis,
- toxoplasmosis,
- syphilis,
- cytomegalovirus and herpes infection,
- streptococcal and fungal infections.
Allergic and autoimmune diseases are accompanied by an inflammatory process. This can be a reaction to taking medications, foods, serums, vaccinations, as well as one of the symptoms of diseases:
- rheumatism,
- scleroderma,
- rheumatoid arthritis,
- Reiter's syndrome,
- psoriasis,
- jade,
- multiple sclerosis,
- diabetes mellitus,
- nonspecific ulcerative colitis,
- autoimmune thyroiditis
- meningoencephalitis.
Eye lesions - retinal detachment, burns and injuries, foreign bodies, keratitis, blepharitis and conjunctivitis can occur with uveitis.
We recommend reading the article about retinal angiopathy. From it you will learn about the types of pathology and the reasons for its development, the danger of the disease, symptoms, diagnosis and treatment.
And here is more information about urticarial vasculitis.
Diagnostics
The examination is urgent, the ability to see is at stake. The problem is solved by an ophthalmologist.
When complications develop, real or suspected, more specialized doctors are involved: a vitreosurgeon (a specialist in the internal parts of the organ of vision), others.
List of events:
- Oral survey. What complaints do you have and when did they arise? Anamnesis collection. Briefly to understand the origin of the pathological process.
- Measuring intraocular pressure. As a rule, it is increased. How much depends on the type and location of the disorder.
- Assessment of visual acuity using standard methods. Using a table. On the side affected by uveitis, the indicators are significantly lower.
- Perimetry. Evaluation of fields of visibility. Some scotomas and defects are invisible to either doctors or the patient until an assessment is carried out.
- Ophthalmoscopy. Fundus examinations using a special apparatus. It is possible to use a Goldmann lens to visually determine changes in the far periphery of the retina. An important condition is the dilation of the pupil, which is carried out using drops.
- Ultrasound. Shown relatively rarely.
- Goniospokia. Inspection of the anterior chamber of the organ.
- Ophthalmography. Used as part of assessing the quality of blood flow in the eye.
- Tomography. In order to differentiate various diseases.
It is possible to conduct laboratory tests:
- General and biochemical blood tests with determination of the concentration of C-reactive protein.
- Specific tests like the Wasserman reaction and a more modern analogue - the anticardiolipin test. Mainly as part of the diagnosis of syphilis, if there is suspicion.
- PCR. Identification of viral agents.
Treatment of uveitis and choice of drops
Drug therapy is used to treat the disease. Most often it consists of the following groups of drugs:
- Mydriatics (Tropicamide, Phenylephrine) to dilate the pupils, prevent adhesions or rupture of existing ones.
- Steroids (Betamethasone, Dexamethasone, Hydrocortisone) are the basis of treatment and have an anti-inflammatory effect. They are instilled in the form of eye drops, the ointment is placed behind the lower eyelid, injections are made under the eyeball, conjunctiva, and into the vitreous body. Combine local and systemic use.
- To lower the pressure of the intraocular fluid, glaucoma medications are recommended - Timolol, Pilocarpine, Fotil, Xalatan.
If no result is obtained from corticosteroid therapy, then immunosuppressants are prescribed. If uveitis is of microbial or viral origin, appropriate medications are used; for allergies, antihistamines are used. After the elimination of the acute inflammatory process, physiotherapy with absorbable enzymes is indicated.
In children with severe cases, it is recommended to add extracorporeal detoxification methods to drug therapy. These include plasmapheresis, hemosorption and quantum autohemotherapy. They allow you to remove immune complexes and antigens from the blood.
If uveitis cannot be treated with pharmacological methods, then surgical treatment is prescribed to dissect adhesions, replace the lens, restore normal intraocular pressure, and retinal hemorrhage. In case of generalized damage, the vitreous body is removed; if this does not help to save the eye, then it must be removed to prevent the process from spreading to the brain.
Treatment
Mostly conservative. Aimed at eliminating the key cause of the disease and correcting its manifestations.
Drugs used:
- Anti-inflammatory non-steroidal origin. Their task is clear. Diclofenac and others, in tablets and drops.
- Antibiotics. Of necessity. If the disorder is provoked by other agents - antifungal drugs, interferon-based drugs or names that can induce the production of antibodies (antiviral).
- Hormonal medications (if the cause is allergies). In the form of drops or ointments. Hydrocortisone, Prednisolone and others.
- Means for relief of increased intraocular pressure. Pilocarpine, Xalatan and the like.
- Mydriatics. They dilate the pupil and prevent the formation of adhesions. Atropine, Scopolamine (drops).
At the end of the acute period, physiotherapy is indicated: electrophonophoresis, other procedures at the discretion of the specialist.
Attention:
Folk remedies are not used. This is a waste of time due to its low effectiveness and high allergy risks.
Medicines for the treatment of ocular uveitis are not always prescribed; in severe cases, they are not sufficiently effective.
If complications develop, such as retinal detachment or the formation of adhesions, surgical assistance is required.
If the eye cannot be saved, the internal media of the organ are excised or completely removed with the installation of a prosthesis for cosmetic purposes.
With the development of a secondary form of the process, when the primary diagnosis is of venereal or other origin, treatment of the underlying disease is indicated. This will prevent relapses.
Clinical recommendations and prognosis
Treatment of uveitis at home should be timely, then the patient can avoid complications, because this is a complex inflammatory process that requires special attention and an integrated drug approach. The initial stage can be determined by characteristic symptoms (blurred vision, decreased clarity of vision, pain, redness and other signs).
Clinical recommendations:
- timely consultation with an ophthalmologist;
- regular monitoring of uveitis;
- use of protective measures when in contact with damaging elements;
- strengthening the immune system;
- taking vitamin complexes;
- proper care of contact lenses;
- timely treatment of infectious diseases;
- limiting contact with allergens.
The prognosis for the further course and dynamics of uveitis is influenced by the timeliness of the therapy started. The acute form, with adequate treatment, goes away within a month. The chronic course requires longer-term use of medications; the fight against the disease sometimes lasts up to six months.
If a secondary lesion is added to uveitis, then treatment at home will not give positive dynamics. For example, retinal detachment, cataract formation, or glaucoma have a poor prognosis. In such situations, operations are prescribed, and the result is individual, as it depends on the severity and form of the disease.
Forecast
With a simple flow, it is almost always favorable. Complications occur in 10-13% of cases, without therapy in 35-40% of situations.
- Posterior forms of uveitis must be corrected in a hospital; in this situation, the chances of complete recovery are more than 85%.
- Forms that occur with other phenomena are much more unfavorable, the probability of total normalization is about 20% or lower
In any case, regardless of the type of disorder, treatment of uveitis is the only way to ensure a positive prognosis.