Kinds
Vasospasm is divided into the following types:
- Expressed;
- Moderate;
- Peripheral.
With severe vasospasm, the heart artery narrows and angina occurs; this condition is characterized by the appearance of heart attacks with severe chest pain. Attacks most often occur at night, they are long-lasting, and are associated with recent physical activity.
Moderate vasospasm is typical for the lower extremities and great vessels, so a moderate spasm may occur in the retina of the eye. When the legs are affected, the skin tends to become pale, followed by redness. When the eye is damaged, its nutrition is slightly disrupted.
Peripheral spasm is the most common form; it is usually associated with vegetative-vascular dystonia. This type of vasospasm is divided into the following subtypes:
- hand spasm;
- acrocyanosis occurs when there is poor blood supply to the capillaries, the skin acquires a blue tint;
- livedo reticularis is characterized by bluish skin with the appearance of a characteristic pattern on it;
- accompanied by lung pathology;
- accompanied by chronic heart failure;
- Raynaud's disease is characterized by damage to the small arteries and narrowing of the lumen of the capillaries, sensitivity is impaired.
- chills are accompanied by bluish skin.
What is retinal vasospasm? Delivery of contact lenses and glasses in Moscow and Russia
Retinal angiospasm in ophthalmology is considered an urgent condition requiring emergency medical intervention. As practice shows, this disease can appear at any age, but most often it is diagnosed in patients over 40 years of age. Moreover, men are more susceptible to retinal vasospasm than women.
Angiospasm of the retina - what is it?
Retinal angiospasm is a dysfunction of the human visual apparatus, which is preceded by an atypical sharp narrowing of the central artery of the retina, as well as the vessels branching from it. In this case, there are no changes at the organic level in the vascular wall.
There are a number of clinical symptoms characteristic of this pathology, namely:
- The appearance of dots before the eyes, which patients often call “spots”;
- Blurred vision, difficulty focusing;
- Discomfort appearing in the periorbital region;
- Distorted perception of color, shape and size of nearby or distant objects.
In more than 90% of cases, such disorders are caused by insufficiently good blood flow in the central artery. They occur due to improper functioning of the human cardiovascular system. Most often, the disease begins to progress against the background of arterial hypertension or atherosclerosis. In approximately 25% of cases, doctors cannot determine the etiology of vascular spasms in the retina.
Ophthalmologists diagnose vasospasm in patients at any age, but in most cases in people over 40 years of age. It has been scientifically proven that men are 2 times more likely to go to medical institutions with a similar problem than women.
Spastic contraction in the middle layers of the retinal arteries in children is usually caused by pathologies in the structure of the peripheral nervous system, including autonomic dysfunction. In the matter of the etiology of this disease, modern medicine is practically powerless - there is no reliably proven assumption regarding the nature and causes of this pathology.
Angiospasm is a disease of the retina, which in adults in the vast majority of cases occurs against the background of other diseases, such as:
- Diabetes mellitus is a disruption of the endocrine system, which is caused by a relative or absolute deficiency of the pancreatic hormone insulin, as a result of which an increase in the level of glucose in the patient’s blood is observed.
- Hypertension is a malfunction of the cardiovascular system. The disease occurs against the background of dysfunction of vascular regulation centers.
- Atherosclerosis is a chronic artery disease caused by disturbances in a wide group of different compounds, i.e. lipids (fatty acids are among them), and is accompanied by an increased content of cholesterol in the inner lining of blood vessels.
Angiospasm of the retina can occur as a result of intoxication, in which an unregulated increase in the tone of the vascular wall occurs. This is possible in case of poisoning with heavy elements such as lead or carbon disulfide.
Corresponding reactions are not uncommon among people employed in hazardous work environments who are diagnosed with chronic intoxication syndrome.
The pathology is characterized by bilateral damage to the paired organs of vision (angiospasm of the retina of both eyes also often indicates a disorder of the nervous regulation of tone).
Adherence to bad habits is another point that is highlighted by doctors as one of the fundamental factors in the development of functional disorders of the central nervous system.
Narrowing of the retinal artery can occur due to exposure to nicotine and tar in smokers, as well as alcohol in those who abuse alcoholic beverages.
These harmful substances lead to temporary deformation of the walls of blood vessels, but gradually such effects provoke dilatation.
Diagnosis of retinal vasospasm
Anamnestic data, the results of a visual examination in combination with additional diagnostic methods allow the ophthalmologist to establish vasospasm of the retinal vessels as a diagnosis. The list of studies within the framework of pathology detection includes:
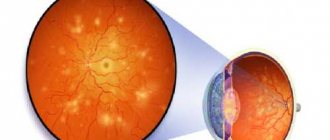
- Ophthalmoscopy. After examining the fundus of the eye, the doctor visually determines a sharp narrowing of the veins in the retina. The vessels are full of blood, but a somewhat swollen, pale pink optic disc is visible. The foveal reflex, like the macular reflex, is not diagnosed during vasospasm.
- OCT. During scanning of the central part of the retina, thickening is visible. In this case, the foveal recess is greatly smoothed, and retinal reactivity is reduced, while the shape of the curve is atypically straight.
- Non-contact tonometry method. During an attack, the specialist observes a slight increase in IOP (intraocular pressure), and after its relief, a normalization of ophthalmotonus.
- Angiography. The ophthalmologist visualizes the changes taking place in the retinal vessels. Diagnosis occurs as part of studying the characteristics of fluorescein circulation. During vasospasm, the internal blood-retinal barrier for contrast remains impenetrable.
Angiospasm of the retina: treatment
For vasospasm, etiotropic therapy is not carried out, since it has not yet been developed in modern medicine. Methods of pathogenetic treatment of the disease are used, which are aimed at reducing pressure and dilating blood vessels undergoing spasms, as well as restoring impaired blood flow in the ischemic zone.
If the unfavorable manifestations of vasospasm are not eliminated in a timely manner, this can lead to a severe decrease in vision and, as a consequence, to a partial or complete loss of the ability to see.
Therefore, the doctor, having diagnosed the corresponding pathology in the patient, immediately after the examination prescribes antispasmodics to the patient. As part of treatment, electrophoresis and vasodilators are recommended.
Carbonic anhydrase inhibitors, as well as saluretics, help reduce intraocular pressure. In cases where the desired effect does not occur, a special irrigation system can be installed in the retrobulbar space.
The pathology is also stopped by instillation of solutions of special drugs: beta-adrenergic receptor blockers.
Sometimes medications are administered intramuscularly (this mainly happens when the disease is accompanied by high blood pressure).
Short-term narrowing of small branches of the central nervous system is not considered dangerous, but if the attack lasts more than 10-15 minutes, irreversible serious changes occur in the retina due to lack of trophism.
Therefore, the prognosis for the treatment of the disease varies - it all depends on the form of the pathology.
As for the prevention of vasospasm, it usually comes down to enhanced monitoring of blood pressure, as well as blood glucose levels.
On the Ochkov.Net website you can view a large selection of contact lenses from popular manufacturers and order them in a few clicks.
Source: https://www.ochkov.net/informaciya/stati/chto-takoe-angiospazm-setchatki.htm
Retinal angiopathy of both eyes
A phenomenon such as retinal angiopathy is detected as a symptom in various diseases. This is not an independent disease, which means that when it appears, it is necessary to identify the source of the problem; this determines how successful the treatment of the disease will be.
Angiopathy is an abnormal process in the blood vessels that occurs due to a violation of nervous regulation. The size of the veins and arteries changes, they become twisting. Ultimately, the blood supply deteriorates and the functioning of organs is disrupted.
Retinal angiopathy is a vascular lesion (hemorrhage, dilatation, spasm) and is quite pronounced in both eyes.
In this case, the patient complains of:
- Deterioration of vision;
- Veils or flickering in the eyes;
- The appearance of blood in the urine;
- Leg pain;
- Nosebleeds.
By consulting a doctor at the first stages of pathological changes, the patient can completely get rid of the disease. If the condition is left to chance, it can lead to serious consequences, and even blindness.
In modern life, a person experiences a constant and quite significant load on the visual analyzer. This is primarily due to frequent use of the computer, forced reading in transport, chronic lack of sleep and many other factors.
Important Unfortunately, very few people have the habit of visiting an ophthalmologist for preventive purposes. But in vain - regular examinations could save vision from such serious pathologies as glaucoma, dry eye syndrome, hypermetropia, presbyopia, astigmatism and retinal angiopathy of both eyes
In medicine, angiopathy refers to pathological processes in blood vessels that occur due to a violation of nervous regulation. At the same time, the caliber and course of the veins and arteries change. They expand or contract and become tortuous.
As a result, blood supply deteriorates, congestion occurs, and the functioning of organs is disrupted. Retinal vascular angiopathy always develops as a symptom of diseases affecting the vascular system of the entire body, including the eyes. These are atherosclerosis, hypertension, diabetes and others.
In the early stages, eye diseases rarely make themselves felt and often proceed without visible changes or discomfort. At the same time, the disease detected at this stage can be corrected with the help of medications and prevent its further progression.
All of the above applies equally to such a pathology as angiopathy of the retinal vessels of the retina of both eyes, which usually occurs against the background of other internal diseases.
In some cases, detected angiopathy helps to timely recognize diseases such as diabetes mellitus, hypertension, neurocirculatory dystonia and prescribe appropriate treatment.
Retinal angiopathy of both eyes (both eyes) is not an independent disease; it is always a sign of other diseases that affect the vascular system of the body, including the eyes. It occurs in people of all ages, but is more often observed in those over 30 years of age.
Detection of angiopathy contributes to the timely recognition of certain ailments: diabetes mellitus, hypertension, carcinoid tumors, head and spine injuries, diseases of blood vessels with the formation of cholesterol on their walls. This helps to determine the necessary treatment in time.
Clinical picture of the disease
Angiopathy is not an independent disease. This is a manifestation of diseases that affect blood vessels, including those supplying blood to the retina of the eye. This disruption of blood supply is a consequence of a violation of nervous regulation. Angiopathy can lead to extremely dangerous consequences for the body, including complete loss of vision.
Today, ophthalmologists classify the disease depending on the factors that led to its development. So, retinal angiopathy happens:
- Diabetic.
- Hypertensive.
- Hypotonic.
- Traumatic.
- Youthful.
Common symptoms for all types of pathology are nosebleeds, blurred vision, the appearance of so-called floaters or lightning in the eyes, and progression of myopia.
It should be noted that in addition to the above ailments, the development of this ophthalmological pathology can be caused by bad habits and working conditions, old age, intoxication of the body, and fragility of the vascular walls.
Causes
Fundus vascular spasms can occur for many reasons, among them the following can be distinguished:
| Adequate sleep is the key to health. A person who sleeps less than 7 hours a day cannot rest fully. The eyes do not get rid of tension, their functioning is impaired. |
| Poor lighting has a direct impact on the visual organs. They become tense, dryness and irritation appear. |
| Frequent work at the computer has a negative impact on the entire human body, primarily regarding vision. It is recommended to take breaks every hour. |
| Frequent conflicts and depression can provoke deterioration in health, the nervous system, blood vessels, and eyes suffer. |
| The harm of addictions is obvious; when they enter the body, toxins are carried through the blood, causing destructive harm. Blood vessels, heart, lungs, kidneys - all of these suffer first. |
| Intoxication | In acute intoxication, a person suffers from elevated body temperature, mental and vision impairment, and convulsions. |
Doctors say that all eye diseases depend on their adequate blood supply. With muscle contractions of the vascular walls, the lumen of the vessel narrows. The membranes of vascular cells do not receive potassium, sodium, or calcium. The muscles do not contract as expected and do not relax.
Interesting! Vegetative-vascular dystonia can provoke vasospasm.
Impaired blood circulation in the eyes can lead to retinal dystrophy, vascular embolism, and glaucoma. Human health directly depends on the condition of the blood vessels, or rather on how passable and clean they are.
Treatment of pathology
The cause of this condition can be eliminated with the help of Papaverine.
Angiospasm of the retina of both eyes requires urgent treatment, as it can lead to necrosis of the macula and loss of vision. For emergency treatment, vasodilators or antispasmodics are used. The most common among them are the drugs “No-shpa”, “Papaverine” and “Cavinton”. They help normalize blood circulation and restore nutrition to the eyeball. The use of sedatives and dehydrating agents that reduce blood pressure and blood supply to the vascular bed is also indicated.
To improve the trophism of macular tissue, Nootropil is used, which increases the ability of cells to take oxygen from tissues. To restore vascular resistance, Nicotinamide is used, and Trental will help improve blood flow. It is also necessary to prescribe vitamin and mineral complexes. Retrobulbar injections of Atropine will help eliminate unpleasant symptoms. If drug treatment is ineffective, surgical intervention is resorted to. It consists of laser coagulation of the affected vessel and subsequent strengthening of the retina.
To prevent the recurrence of the disease, it is necessary to eliminate the cause that provoked vasospasm. To do this, correction of blood glucose levels is carried out, constant monitoring of blood pressure for hypertension and normalization of the diet with the exception of fatty, fried and spicy foods, which provoke high blood cholesterol and, as a result, the development of atherosclerosis. In combination with traditional methods, you can use traditional methods of treatment. Most often these are decoctions of medicinal herbs and their infusions. During the recovery period, it is possible to use physiotherapeutic methods.
Complications
If the disease is not treated, it can lead to the following complications:
- farsightedness;
- glaucoma;
- retinal dystrophy:
- ischemic optic neuropathy;
- retinal stroke;
- thrombosis and embolism of arteries.
The most dangerous consequence is complete loss of vision without the possibility of recovery.
If treatment was carried out in a timely manner, the prognosis is favorable. To avoid recurrence of symptoms, you must strictly follow your doctor's recommendations.
Prolonged vasospasm causes a sharp irreversible decrease or complete loss of vision. Frequent attacks lead to severe discomfort and impairment of performance, because patients cannot predict the time of development of the next episode. Recurrent vasospasm contributes to an increase in intraocular pressure.
Prolonged spasm and poor circulation lead to irreversible loss of vision. Periodic spasms of capillaries provoke constant eye pain.
Frequent acute attacks cause discomfort and reduce ability to work. The situation is complicated by the fact that a person cannot predict the progression of an attack; symptoms appear suddenly and sharply. Relapses contribute to stable intraocular pressure. This is how ocular hypertension develops above 20 mmHg. Art., while there are no changes in the fundus, as with glaucoma.
Short-term attacks of vasospasm do not cause complications.
The prognosis of the disease directly depends on the severity of the clinical picture. Adverse effects are observed in patients with attacks lasting more than 15 minutes. This time is enough for destructive processes to begin in the retina.
These have already been named. In addition to necrosis of the tissues of the heart and brain, intestinal obstruction and sensory disturbances in the extremities occur.
Death of the patient and severe disability are also possible options. When the disorder and the root cause are stopped, the likelihood of consequences is close to zero.
Symptoms
Angiopathy of the arteries located in the retinal area is characterized by symptoms such as pathological changes in the elements of the circulatory network, which determines treatment tactics. The affected vessels dilate because the vascular wall loses its elasticity and tone. The vascular bed becomes tortuous, which, together with impaired patency, leads to a change in the speed and volume of blood flow.
Manifestations of angiopathy of the elements of the blood supply to the eyes include loss of vision, which can be partial or complete, affecting one or both organs of vision. Typically, disorders develop under the influence of provoking factors - psycho-emotional stress, physical stress. Often severe symptoms appear in the morning after waking up.
A decrease in visual acuity is often preceded by symptoms - transient visual dysfunction, short-term loss of visual fields, the appearance of foreign objects (dots, spots, sparks) within the boundaries of the visual field. Angiopathy of the vessels located in the retinal area in adults and children is manifested by the following symptoms:
- The presence of a pink, cherry-colored spot in the retinal area. The spot clearly appears against the background of the retina of a white-gray color, caused by edema of ischemic origin.
- Narrowing of arterioles (small arteries preceding capillaries) of the inner lining of the organs of vision.
- Formation of foci of intraretinal (located inside the retinal nerve sheath) hemorrhage.
In the early stages of the pathology, the disc at the base of the optic nerve is pale pink with blurry, indistinct boundaries. Later, the disc becomes pale, the borders are not visible due to swelling in the peripapillary zone of the inner eye membrane. If ischemic processes affect the entire inner membrane, the color of the papillomacular area may remain unchanged.
If the patency of the central artery or its branches is impaired, pathological changes of ischemic origin occur in the areas that supply the affected vessels. If ischemia does not extend to the macula (the central point of the retina where light rays are refracted), loss of visual fields is detected in accordance with the localization of the ischemic focus.
In cases of damage to the macular area, deterioration in visual acuity is observed. As a consequence of destructive processes, atrophy of the optic nerve tissue develops. You need to make an appointment with an ophthalmologist in cases where the following symptoms are observed:
- Frequent redness of the mucous membrane of the eyes.
- Cloudiness of the visible image.
- Feeling of pulsation and swelling inside the eyes.
- Loss of field of view.
- Pain in the visual area.
- The appearance of foreign objects and blind spots within the field of view.
If these signs appear, then you need to consult a specialist who will conduct a diagnostic examination and develop a treatment program.
Vascular spasm of the eye: main symptoms and treatment methods
The purpose of blood vessels is to provide the eyeballs with the necessary microelements, primarily oxygen.
In order to prevent the occurrence of spasms, you need to know the causes of their occurrence. Vasospasm of the eye, symptoms and treatment are the key to successful health. Only timely detection of pathology will help to avoid consequences, and the patient will be able to maintain vision.
The lumen of the artery narrows significantly
Features of the vessels of the eye
Without adequate blood supply, the eyes will not be able to perform their functions. The necessary “food” for the nerve cells that are located in the retina, nutrients and oxygen, comes from the bloodstream. If at least one vessel does not cope with its work, others come to the rescue, they bring the necessary elements. This can explain the fact that the vessels of the eye are branched.
Blood flow in the eyes begins from the carotid artery. From here the blood goes to the central retinal artery and passes into the posterior ciliary arteries. The central artery is located inside the optic nerve; it is from there that the eye is fed. A small portion of the optic nerves exiting the eye supplies small arteries. All together they form a circle, numbering from 6 to 12.
The venous network has the same structure as the arterial network. However, there is still a small feature: there are no valves. They are needed to prevent the reverse flow of blood. Inflammatory processes can trigger the release of infection into the blood, thereby easily penetrating the brain.
Multiple vessels in the eyes are responsible for the functioning of a specific nerve or muscle; without this, the organs of vision will not be able to fully function. If you experience spasm of the ocular arteries, you should go to the hospital as soon as possible.
Causes
Fundus vascular spasms can occur for many reasons, among them the following can be distinguished:
| No established sleep pattern | Adequate sleep is the key to health. A person who sleeps less than 7 hours a day cannot rest fully. The eyes do not get rid of tension, their functioning is impaired. |
| The workplace is not well lit | Poor lighting has a direct impact on the visual organs. They become tense, dryness and irritation appear. |
| Spending a long time at the computer | Frequent work at the computer has a negative impact on the entire human body, primarily regarding vision. It is recommended to take breaks every hour. |
| Frequent conflicts and depression can provoke deterioration in health, the nervous system, blood vessels, and eyes suffer. | |
| Abuse of bad habits | The harm of addictions is obvious; when they enter the body, toxins are carried through the blood, causing destructive harm. Blood vessels, heart, lungs, kidneys - all of these suffer first. |
| In acute intoxication, a person suffers from elevated body temperature, mental and vision impairment, and convulsions. |
Doctors say that all eye diseases depend on their adequate blood supply. With muscle contractions of the vascular walls, the lumen of the vessel narrows. The membranes of vascular cells do not receive potassium, sodium, or calcium. The muscles do not contract as expected and do not relax.
Interesting! Vegetative-vascular dystonia can provoke vasospasm.
Impaired blood circulation in the eyes can lead to retinal dystrophy, vascular embolism, and glaucoma. Human health directly depends on the condition of the blood vessels, or rather on how passable and clean they are.
Symptoms
As mentioned above, otherwise spasm of the retinal vessels is called vasospasm.
A typical complaint of all patients is distortion of visual perception, discomfort, namely:
- Vision periodically seems to blur. The duration of the symptom varies and may go away in five minutes or several hours.
- Floaters appear before the eyes. It is felt especially strongly at the moment when the patient tries to stand up sharply.
- Photomorphopsia.
When conducting diagnostics, you can see that the branches of the retinal artery are in a narrowed state. Spasms of the ocular vessels can lead to pallor of the fundus tissues.
Diagnostics
Since vasospasm does not manifest itself, the first thing you need to do is find out what triggered the development of the pathology. Diagnosis and treatment are carried out by a therapist and an ophthalmologist.
Before prescribing treatment, the ophthalmologist conducts a complete examination of the retinal vessels. With ophthalmoscopy, the doctor can assess the condition of the arteries and capillaries of the eye, as well as the fundus of the eye. To examine the full picture, drops with a dilating effect are first instilled into the patient.
A distinctive feature of spasms is hemorrhages in the retina, as well as the presence of cholesterol deposits. At a late stage of development, the tissues are swollen and can be seen with the naked eye.
Types of angiopathy
Depending on the underlying disease, vasospasm can be divided into several types:
- Diabetic angiopathy is a common form. In 40% of cases it occurs in patients with diabetes mellitus. From the onset of the disease, angiopathy manifests itself after 5-7 years. Large vessels are affected and become blocked.
- Hypertensive - with increased pressure, the arteries narrow and the veins dilate. If left untreated, vascular sclerosis will begin to form.
- Hypotonic angiopathy - arteries dilate, intraocular pressure increases. Vessels that cannot withstand the load burst and hemorrhage appears.
- Angiopathy during pregnancy is temporary; after childbirth, the pathology goes away on its own within a few weeks. However, if there was another form of the disease previously, after the birth of the baby it will begin to progress.
Angiopathy is dangerous because it is difficult to notice at an early stage of development, since there are no symptoms (see Vessels burst in the eyes: why does this happen?).
Clinical picture depending on the type of pathology:
| View | Symptoms |
| There is a feeling of pulsation in the eyes, the arteries are clearly visible, the retinal tissue swells, and vein thrombosis occurs. | |
| The vision becomes blurred and the veins dilate. The arteries narrow. | |
| Yellow spots appear on the fundus, diabetes mellitus, and the walls of the capillaries swell. |
This article talks about other possible symptoms.
Treatment methods
How the retina changes during the development of the disease
Treatment of vasospasm is an important process. An individual course of treatment is selected for each patient. It is necessary to take into account the age of the patient, the type of pathology, the reasons that caused it, etc.
Interesting! Therapy is aimed primarily at relieving symptoms and eliminating factors that provoked the development of the disease.
Conservative methods
This includes the use of drugs from several groups, with their help you can eliminate the pathological process:
- Vitamin complexes: B15,12, 1;
- Preparations to reduce vascular permeability: Gingko, Parmidine;
- Strengthening preparations: Vazonit, Kaviton;
- Improving microcirculation: Emoxipin;
- Prevents the formation of blood clots: Trombonet.
Conservative therapy is rarely used to treat pregnant women, since side effects can negatively affect the condition of the fetus.
Physiotherapy
How to relieve vascular spasm in the organ of vision using physiotherapy:
- Laser irradiation purifies the blood. It becomes less toxic, the immune system is strengthened.
- Magnetotherapy improves blood circulation, cells become more permeable, inflammation and pain are relieved.
- Acupuncture – recommended for the treatment of angiopathy that occurs after injury.
The price of such treatment varies.
Traditional methods
Arterial spasm can be relieved not only by traditional methods, but also by traditional medicine.
The methods do not completely eliminate the pathology, but improve the patient’s condition. The safest recipes:
- Take half a tablespoon of St. John's wort, chamomile and hot water. Mix, leave for half an hour, strain. Every morning on an empty stomach, drink 1/5 of the resulting product.
- Take fifteen grams of lemon balm, yarrow, and valerian. Separate two spoons, pour a glass of boiling water, let it brew for three hours. Boil in a water bath for fifteen minutes, strain. Add water, the total volume should be 0.25 liters. Drink the prepared product throughout the day.
You can use folk remedies only after visiting a doctor. It is unacceptable to use such methods as the main treatment.
Proper nutrition
During diabetic and hypertensive angiopathy, a special diet is required. You need to avoid foods that contain a lot of cholesterol.
Important! A doctor should prescribe proper nutrition.
If you are diabetic, avoid the following foods:
- Mustard;
- Alcohol;
- Spicy dishes;
- Sweet fruits;
- Sugar.
For hypertensive angiopathy, the following restrictions are provided:
- No strong tea or coffee;
- Fatty dishes and broths are not allowed;
- Spicy dishes;
- Smoked sausages or fish;
- It is too salty.
You need to stick to this diet exactly as much as your doctor recommends.
Complications and prognosis
Result of treatment of complications
If the disease was detected in a timely manner and treatment was completed, the prognosis is favorable. The underlying disease should be given as much attention as possible. The recurrence of pathology can be avoided only by following the recommendations of a specialist.
If left untreated, the patient is at risk of developing glaucoma and cataracts. The juvenile form of the disease carries the greatest danger, since it is difficult to treat.
Complications are extremely serious:
- There is hemorrhage in the vitreous glass;
- Development of cataracts;
- The number of vessels increases;
- The retina detaches.
The photo below is an example of complications
Example of healthy and pathological retina
Prevention
The goal of prevention is to prevent complications from the main disease: high blood pressure, diabetes mellitus.
All patients must follow the following rules:
- Visit an ophthalmologist several times a year and undergo preventive examinations;
- Complete cessation of bad habits;
- Pay due attention to sleep and rest;
- Watch your diet;
- Distribute physical activity correctly;
- Diseases that have a negative impact on blood vessels must be treated promptly.
Treatment of fundus vasospasm is lengthy and difficult. There is no need to panic or despair, as timely treatment starts gives a high chance of recovery. When the first signs of pathology appear, you should immediately visit the hospital and undergo a full examination.
Source: https://uFlebologa.ru/lechenie/metody/spazm-sosudov-glaza-simptomy-lechenie-658
Diagnostics
The doctor checks the fundus of the eye with a special apparatus and evaluates the condition of the retina and blood vessels in both eyes. If you suspect angiopathy, you will also need an ultrasound, magnetic resonance imaging, and x-ray of blood vessels (angiography).
An ophthalmologist makes a diagnosis taking into account the patient’s complaints after examining him. To clarify the diagnosis, eye doctors use ultrasound scanning of blood vessels. This procedure helps to obtain information about the speed of blood circulation and the condition of the vascular walls.
Sometimes, if necessary, the doctor injects an X-ray contrast agent to assess the patency of the capillaries. Another diagnostic method used to establish an accurate diagnosis is magnetic resonance imaging. It allows the eye doctor to assess the condition of the soft tissues of the eye.
Typically, when the diagnosis is confirmed, patients are prescribed medications that improve blood circulation. These are Trental, Emoxipin, Solcoseryl, Vazonit, Arbiflex. Such medications normalize blood flow in the capillaries.
If the patient has vascular fragility, he is prescribed a course of calcium dobesilate. The medicine thins the blood, improves its circulation and the permeability of the vascular walls.
Sometimes physiotherapeutic methods are used in the treatment of this eye disorder, for example, acupuncture, magnetic influence, laser irradiation. They improve the general condition of the patient.
If we are talking about hypertensive angiopathy, then there is no way to do without normalizing blood pressure, its constant monitoring and lowering the level of cholesterol in the blood. And with a hypotonic type of pathology, the first priority is to normalize blood pressure.
When it comes to diabetic diabetes, in addition to medications that improve blood circulation, it is mandatory to follow a diet that excludes an abundance of carbohydrates. Patients with diabetes benefit from moderate physical activity - it will improve the functioning of the cardiovascular system and hematopoiesis.
So, angiopathy is a reversible pathology that simply needs to be promptly detected and treated by a qualified ophthalmologist.
Treatment methods
How the retina changes during the development of the disease
Treatment of vasospasm is an important process. An individual course of treatment is selected for each patient. It is necessary to take into account the age of the patient, the type of pathology, the reasons that caused it, etc.
Interesting! Therapy is aimed primarily at relieving symptoms and eliminating factors that provoked the development of the disease.
Conservative methods
This includes the use of drugs from several groups, with their help you can eliminate the pathological process:
- Vitamin complexes: B15,12, 1;
- Preparations to reduce vascular permeability: Gingko, Parmidine;
- Strengthening preparations: Vazonit, Kaviton;
- Improving microcirculation: Emoxipin;
- Prevents the formation of blood clots: Trombonet.
Conservative therapy is rarely used to treat pregnant women, since side effects can negatively affect the condition of the fetus.
Physiotherapy
Hemorrhage
How to relieve vascular spasm in the organ of vision using physiotherapy:
- Laser irradiation purifies the blood. It becomes less toxic, the immune system is strengthened.
- Magnetotherapy improves blood circulation, cells become more permeable, inflammation and pain are relieved.
- Acupuncture – recommended for the treatment of angiopathy that occurs after injury.
The price of such treatment varies.
Traditional methods
Arterial spasm can be relieved not only by traditional methods, but also by traditional medicine.
The methods do not completely eliminate the pathology, but improve the patient’s condition. The safest recipes:
- Take half a tablespoon of St. John's wort, chamomile and hot water. Mix, leave for half an hour, strain. Every morning on an empty stomach, drink 1/5 of the resulting product.
- Take fifteen grams of lemon balm, yarrow, and valerian. Separate two spoons, pour a glass of boiling water, let it brew for three hours. Boil in a water bath for fifteen minutes, strain. Add water, the total volume should be 0.25 liters. Drink the prepared product throughout the day.
You can use folk remedies only after visiting a doctor. It is unacceptable to use such methods as the main treatment.
Proper nutrition
During diabetic and hypertensive angiopathy, a special diet is required. You need to avoid foods that contain a lot of cholesterol.
Important! A doctor should prescribe proper nutrition.
If you are diabetic, avoid the following foods:
- Mustard;
- Alcohol;
- Spicy dishes;
- Sweet fruits;
- Sugar.
For hypertensive angiopathy, the following restrictions are provided:
- No strong tea or coffee;
- Fatty dishes and broths are not allowed;
- Spicy dishes;
- Smoked sausages or fish;
- It is too salty.
You need to stick to this diet exactly as much as your doctor recommends.
Peripheral vasospasm
The most common vasospasm is peripheral vasospasm.
Peripheral vascular spasm is one of the most important mechanisms in acute blood loss. Blood flows from the periphery to the center, where vital organs that are more sensitive to hypoxia (brain, heart, endocrine glands) are located.
On the lower extremities, spasm is visible to the naked eye and is expressed by pallor of the skin, which then turns blue. The pallor is explained by the outflow of blood into the central vessels, and the blue color is due to a lack of oxygen. Ultimately, lack of oxygen in the tissues leads to their gradual death. If you notice such symptoms, you should immediately seek advice and treatment from a doctor.
Causes of retinal vasospasm
The etiology of the disease is not fully understood. Idiopathic forms of the disease are often observed, when it is not possible to determine the genesis of the pathology. In children, spastic contraction of the middle layer of arteries is caused by autonomic dysfunction and the peculiarities of the formation of the peripheral nervous system. In adulthood, the main causes of retinal vasospasm include:
- Hypertension
. In response to an increase in blood pressure, a reflex spasm of blood vessels occurs, including in the orbital region. This phenomenon is associated with the release of catecholamines, which have a pressor effect on the receptors of the vascular wall. - Diabetes
. People with decompensated diabetes have a high risk of progression of diabetic retinopathy. This pathology is accompanied by frequent episodes of vasospasm. - Atherosclerosis
. With atherosclerotic damage to the endothelium, blood pressure increases and perfusion is impaired. The response to hypoxia is represented by a spastic contraction of the muscle layer of the central nervous system. - Bad habits
. Narrowing of the retinal artery is a consequence of excessive exposure to nicotine in smokers and ethyl alcohol in people who abuse alcoholic beverages. These substances lead to a temporary narrowing of the lumen of blood vessels, which is replaced by dilatation. - Intoxication.
The tone of the vascular wall increases with poisoning with carbon disulfide and lead compounds. Such reactions are typical for people working in hazardous production conditions and suffering from chronic intoxication.
Forecasts for the course and treatment of the disease
Angiopathy during pregnancy has a much more favorable prognosis compared to the development of this pathology in an ordinary person, for example, in hypertensive patients, etc.
In most situations for pregnant women, the disease is a temporary side effect that causes abnormalities in the woman’s body
But you should not be negligent about this violation; it is important to get consultation and advice from your doctor.
(No votes yet) Loading ...VKontakteFacebookOdnoklassnikiNEW
- Causes of development, symptoms and treatment features of chronic bronchitis
- How does thoracic chondrosis manifest and how can the patient be helped?
- The most effective exercises for the lower back, methods of performing them and massage
- Indications, contraindications and implementation of uterine artery embolization
- Unconditioned and conditioned reflex: classification and mechanism
Complications and prognosis
If the disease was detected in a timely manner and treatment was completed, the prognosis is favorable. The underlying disease should be given as much attention as possible. The recurrence of pathology can be avoided only by following the recommendations of a specialist.
If left untreated, the patient is at risk of developing glaucoma and cataracts. The juvenile form of the disease carries the greatest danger, since it is difficult to treat.
Complications are extremely serious:
- There is hemorrhage in the vitreous glass;
- Development of cataracts;
- The number of vessels increases;
- The retina detaches.
The photo below is an example of complications
Types of vasospasm
Vasospasm of the extremities
Quite often, vasospasm of the upper and lower extremities is recorded. The upper extremities are affected much more often.
Symptoms of vasospasm of the extremities:
- A sharp appearance of pallor on the fingers, caused by the outflow of blood.
- Blue extremities are due to lack of oxygen;
- Feeling of coldness in the extremities;
- The appearance of lameness and sharp pain in the lower extremities.
- Or, on the contrary, a complete lack of tactile sensitivity.
The attack stops after about 20 minutes, after which the limbs become very red, as the blood rushes to them again.
Peripheral vasospasm
This is the most common type of this disease. As a result, peripheral blood vessels suffer.
Varieties:
- The upper extremities are subject to spasms;
- Livedo reticularis – it affects girls and women. The affected area turns blue and the surrounding skin turns pale.
- Acrocyanosis - manifests itself during puberty, symptoms: numbness of the limbs, severe sweating. Acrocyanosis
- Lung diseases;
- Chronic heart failure;
- In the cold season it manifests itself in the form of bluish spots on the upper and lower extremities;
- Raynaud's syndrome. This disease has three stages of development: ischemia - small arteries undergo spasm, capillaries narrow;
- Cyanosis - stagnation of blood in the veins, artery-venous anastomosis and capillaries;
- Hyperemia is vasodilation, accompanied by impaired sensitivity.
It appears against the background of weak tone of the walls of the capillaries located on the skin. Which is a consequence of negative factors such as stress, sudden changes in lifestyle and weather conditions.
Cerebral vasospasm
Cerebral vasospasm - expressed in the narrowing of blood vessels in the brain. Has a variety of all possible severe symptoms. They can appear simultaneously or in turn, and intensify when you feel unwell. Signs:
- Headache;
- Whistling in the ears;
- Loss of consciousness, fainting;
- Decreased pressure;
- Memory losses;
- Deterioration of speech function;
- Reduced tactile sensitivity or, conversely, a pain symptom is pronounced, but only in one half of the body;
- Feeling of pressure in the head, as well as heaviness and compression, when the weather changes.
Angiospasm of retinal vessels
Retinal vasospasm is a disease accompanied by dysfunction of the retina and caused by narrowing of the central artery or its branches. This disease can lead to serious vision problems. As a rule, patients complain not of pain, but of vision. For example:
- Short-term blurred vision;
- "Floaters" before the eyes;
- An abnormality of the eyes, manifested in the appearance of light effects in front of the eyes: sparks, shine, luminous rings and lines.
Coronary vasospasm
Coronary vasospasm is a spasm of the blood vessels of the heart. It is characterized by a sharp narrowing of the lumen of the coronary arteries. The reasons for its occurrence are different, but mainly: severe stress, bad habits, platelet activity, angina pectoris. The nature of this disease is still unclear. Since, despite slight deviations in the patients’ cardiogram, the coronary arteries are not blocked and signs of oxygen starvation are not noticed. The symptom is a sharp, severe pain in the chest, usually at night or early in the morning when the person is in a horizontal position.
Angiospasm of the retina: what is it, symptoms and treatment
Under the influence of a number of factors, vascular walls lose their elasticity and ability to adapt to changes in blood pressure.
This causes the central retinal vein, as well as the capillaries branching from it, to become unusually sharply narrowed. Angiospasm of the retina is not accompanied by changes at the organic level in the vascular wall, but it leads to disruption of the blood supply to the eye tissues, causing visual impairment.
In this condition, there is a need for surgical intervention by a specialist.
What it is?
Retinal vasospasm is a functional disorder of the retina, in which a sudden narrowing of the central vein or its branches occurs against the background of intense contraction.
The narrowing of the lumen of the vessel occurs sharply, as a result of which trophism is disrupted; retinal tissue does not receive access to the oxygen and nutrients necessary for their normal functioning.
This condition is emergency and requires immediate surgical intervention.
Causes
The etiology of the disease has not been fully studied to date, and often the cause of the pathology cannot be established.
In childhood, this pathological condition develops quite rarely, against the background of structural features of the peripheral nervous system or due to a violation of autonomic function.
In adulthood, the main cause of the development of retinal vasospasm is problems with the cardiovascular system.
Most often, the disease appears against the background of high blood pressure. And for this it is not at all necessary that the jump in blood pressure be huge.
Even a slight but sharp increase in pressure can cause vasospasm of the retinal vessels, since microcirculation is disrupted, hypertrophy of the muscle layer occurs and the speed of blood flow is disrupted. Pathology can also arise for the following reasons:
- diabetes;
- atherosclerosis;
- intoxication of the body with ethyl alcohol or narcotic substances;
- eclampsia;
- thrombosis;
- eye diseases;
- Raynaud's syndrome.
The following factors can provoke the development of vasospasm of the retinal vessels:
- exposure to negative chemicals;
- work in production with hazardous conditions;
- sleep disturbance;
- prolonged stay at the computer or TV;
- hypothermia of the body;
- inflammatory processes;
- stressful situations.
Symptoms
In most clinical cases, both eyes are affected at once.
With a short-term narrowing of blood vessels of a spasmodic nature, the clarity of vision is significantly reduced, “floaters” appear before the eyes, and blurred vision is also observed. These symptoms disappear within a couple of minutes.
In the case of persistent spasm of the central vein, these signs are observed for a long time and are accompanied by the following clinical manifestations:
- difficulty focusing;
- discomfort in the visual area;
- impaired color vision;
- problems recognizing shapes and sizes of objects;
- light flashes before the eyes.
Often additionally there is pronounced pulsation in the temples, headaches and dizziness.
Modern diagnostic methods
First of all, to make an accurate diagnosis, the doctor listens to the patient’s complaints, collects anamnesis and conducts a visual examination. Then various instrumental studies are prescribed:
- ophthalmoscopy – the fundus of the eye is studied, the external condition of the vessels is determined;
- tonometry - intraocular pressure is determined, which increases slightly during an attack;
- angiography – a fluorescein analysis is performed, allowing a detailed examination of the dynamics in the vessels of the retina;
- optical coherence tomography – the central area of the retina is scanned and the degree of macular thickness is determined.
We can speak about the presence of vasospasm of the retina if the following changes were identified during such diagnostic measures:
- venous arteries are filled with blood;
- the optic disc is swollen and pale pink;
- the foveal pit is leveled;
- the internal blood-retinal barrier is impermeable;
- retinal reactivity is reduced;
- arteriovenous junction.
Drug treatment
Drug therapy for vasospasm is aimed at achieving the following goals:
- decreased blood pressure;
- dilation of blood vessels undergoing spasms;
- restoration of impaired blood flow;
- removal of puffiness;
- normalization of material metabolism.
First of all, when selecting medications, the doctor focuses on the cause of the spasm.
If the pathology occurs against the background of diabetes, atherosclerosis or another disease, therapy should first of all be aimed at eliminating them.
In case of severe intoxication or eclampsia, treatment is carried out in a hospital. With retinal vasospasm, it is important to quickly relieve symptoms. To do this, infusions of antispasmodics and plasma substitutes are immediately carried out.
After this, electrophoresis with vasodilators (Drotaverine) and peripheral vasodilators (Bendazole) is prescribed.
Also prescribed are drugs to improve blood flow (Trental), drugs that increase the supply of oxygen to cells (Nootropil) and sedative, dehydrating medications.
In addition, carbonic anhydrase inhibitors, saluretics, and beta-adrenergic receptor blockers may be prescribed. An irrigation system can be installed in the retrobulbar space.
Treatment with folk remedies
For short-term attacks of retinal vasospasm, the following folk remedies may be recommended to alleviate eye conditions:
- Pour 1 tablespoon of dill seeds into 200 ml of boiling water, let it brew for 1 hour, then divide the infusion into 2 equal parts and drink them in the morning and evening.
- Pour 1 tablespoon of cumin seeds into a glass of water, boil and simmer for 5 minutes. Remove from heat, add 1 teaspoon of blue cornflower flowers, let steep for 1 hour. Strain, add clean boiled water so that there is a total of 200 ml of infusion. Take 100 ml twice a day.
Teas made from black currant leaves and chokeberry fruits also help well.
Possible complications
If attacks of vasospasm are not treated on time, then visual impairment becomes more pronounced, which significantly affects a person’s performance.
Sudden frequent attacks are accompanied by severe discomfort and incapacitate the patient for a long time.
People with this problem cannot anticipate the next spasm and are always in a state of alertness.
Lack of treatment for retinal vasospasm can lead to the development of such severe complications:
- stroke, heart attack;
- retinal dystrophy;
- ocular hypertension;
- ocular migraine.
Such consequences can result in loss of vision. But this is only possible with persistent attacks.
Forecast
The prognosis for vasospasm of the retina depends on the nature of the attacks. If the spasms are short-lived, then they pass without a trace. But in the case of prolonged attacks, the duration of which is more than 15 minutes, the prognosis is unfavorable. With such prolonged vasospastic reactions, irreversible destructive changes occur in the retina, leading to loss of vision.
Prevention
There are no specific measures to prevent vasospasm of the retinal vessels. However, you can reduce the likelihood of developing a pathological process if you follow the following recommendations:
- to live an active lifestyle;
- do not lift heavy objects;
- refuse or minimize alcohol consumption;
- Healthy food;
- do not use drugs;
- quit smoking;
- comply with safety rules in enterprises with hazardous working conditions;
- avoid stressful situations;
- avoid excessive visual strain;
- Do not work in poor lighting.
You can also prevent the development of the problem by regularly monitoring your blood sugar levels and monitoring your blood pressure. If you have atherosclerosis, you must take statins.
Source: https://GlazaLik.ru/bolezni-glaz/bolezni-setchatki/angiospazm/
Symptoms of latent spasmophilia
Spasms of the arteries with simultaneous expansion of the venous vessels are characteristic of the first stage of hypertension. The uneven contraction causes different calibers along the arteries and gives them a tortuous appearance.
Fundus of the eye with retinal vasospasm
These phenomena are aggravated in the second stage of hypertension. Persistent spasm of the arteries gives way to their sclerosis, followed by complete obliteration of the vessel. The changed artery, when crossing with a vein, puts a certain pressure on it, causing the latter to sag a little. This is how another ophthalmological sign of hypertension appears - arteriovenous chiasm.
The last stage of the underlying disease for the retina occurs in the form of angioretino- and neuroretinopathy. Impaired blood circulation in a state of vasospasm leads to hemorrhages, swelling of the retina and optic nerve nipple. A so-called “star” of small foci of damage forms around the macula.
The disease can have a hidden (latent) or obvious form. The latent form of spasmophilia in children is very difficult to determine - they are actually healthy, they have normal physical and psychomotor development, but they often show symptoms of rickets. There are a number of symptoms characteristic of spasmophilia that confirm its latent form. Let's name some of them:
- Chvostek's sign. It is characterized by contraction of the facial muscles when lightly tapping the cheek between the corner of the mouth and the earlobe along the trunk of the facial nerve;
- Weiss's sign. It is characterized by the occurrence of contraction of the muscles of the forehead and eyelids when tapping with a percussion hammer in the area of the edge of the orbit from the outside;
- Trousseau's sign. When the shoulder is intensively pulled with a tourniquet or cuff, a convulsive contraction of the hand muscles occurs in the overtightened arm. This leads to the position of the hand in the form of an “obstetrician’s hand”. Convulsions in spasmophilia are preceded by a feeling of numbness and pain in the fingers;
- Maslov's symptom. In children suffering from spasmophilia, unlike healthy ones, when a needle is pricked in the leg, not only rapid breathing is observed, but also apnea (short-term cessation of breathing) recorded by a pneumograph.
An obvious form of spasmophilia in children can be expressed by laryngospasm, carpopedal spasm, eclampsia, or a combination of them:
- Laryngospasm. One of the most common forms of spasmophilia, also called “birthmark,” is characterized by a sudden acute narrowing of the glottis, with its possible partial or complete closure, which occurs during crying or fright. With moderate manifestations of laryngospasm, the child’s skin turns pale, cold sweat appears, and a change in voice occurs with hoarse or sonorous inhalation. The attack can last up to 2 minutes, then when breathing is restored, the child falls asleep. In the absence of adequate treatment for spasmophilia, attacks can be repeated; during severe laryngospasm, complete cessation of breathing and loss of consciousness are sometimes observed; in the most severe cases, death is possible;
- Carpopedal spasm. Symptoms of spasmophilia in this form of the disease are tonic spasms of the hands, feet and face. In this case, the child has bent arms at the elbows, drooping hands with the characteristic Trousseau symptom, bent legs and feet. Attacks of spasmophilia can last from several minutes to several hours, with reactive swelling of the hand and foot appearing; spasms of the respiratory muscles are also possible, threatening to delay and stop breathing, and spasms of the heart muscle with possible cardiac arrest;
- Eclampsia. The rarest and most dangerous form of spasmophilia, manifested by attacks of clonic-tonic convulsions that spread to the entire musculature. With a mild course, facial muscle spasms, the appearance of cyanosis, intermittent breathing and numbness of the child are characteristic. During a severe attack of spasmophilia, convulsions of the whole body, loss of consciousness, tongue biting, involuntary urination and defecation occur; the attack can last up to 25 minutes. In severe cases, respiratory and cardiac arrest is possible; eclampsia most often affects children in the first year of life.
These forms of spasmophilia pose a threat to the health and life of children and require emergency medical care for immediate resuscitation.
What is retinal vasospasm and how to deal with it
A pathological condition in ophthalmology, a pronounced narrowing of the central artery, its branches supplying blood to the visual analyzer section (the thin inner layer of the eye) is vasospasm of the retina. It occurs 2 times more often in men than in women.
Characteristics of the pathology
Retinal angiospasm refers to functional disorders of the organ of vision. The narrowing often occurs abruptly, the access of oxygen to the retinal tissue is suddenly blocked, and trophism is disrupted. The condition is urgent and requires emergency medical attention.
In more than 91%, the disease develops against the background of malfunctions of the cardiovascular system. In 60% of cases, the pathology is caused by hypertension or atherosclerosis. In every third case, the origin of the disease cannot be determined. Angiospasm is diagnosed at any age, in 70% of patients over 40 years of age.
Symptoms of the disease
In most cases, vascular damage is bilateral, less often ─ unilateral. Fog appears before the eyes, and clarity of vision is lost. Some patients notice the flickering of floaters. If the spasm is short-lived, these symptoms go away on their own.
Failures in visual function are possible in the form of impaired perception of shapes, colors, and volumes of visible objects.
Other symptoms of the disease:
- discomfort from the affected eye;
- headaches, dizziness;
- pronounced pulsation in the temples.
The disease proceeds in paroxysms. After an acute manifestation, clinical signs disappear and vision is restored.
In severe cases, vasospasm provokes ischemia, which leads to irreversible partial loss of vision.
How to identify pathology
In patients with signs of retinal vasospasm, a thorough history is collected and the external condition of the eye is assessed. Symptoms such as redness of the conjunctiva and swelling indicate an acute attack. During the period of subsidence, the eyes return to normal and visually, without diagnostic equipment it is impossible to suspect pathology.
Ophthalmological examinations to detect vasospasm of the eye:
- ophthalmoscopy ─ examination of the anterior chamber, fundus of the eyes using an ophthalmoscope, slit lamp;
- non-contact tonometry ─ measurement of intraocular pressure by exposing the cornea to a directed air pulse;
- OCT of the retina (optical coherence tomography) ─ scanning of eye structures with a directed beam of light;
- angiography is a method of examining the fundus of the eye to assess the vascular and capillary network of the retina.
How to treat
There is no treatment aimed at eliminating the causes of the disease. It is possible to stop the development of pathology and restore normal blood flow in the ischemic zone. The primary task of the ophthalmologist is to relieve symptoms and ensure blood supply to the membrane. A prolonged absence of microcirculation can lead to loss of visual function.
Medicines
After examination and clarification of the diagnosis, patients are prescribed antispasmodic drugs to relax the muscle layer of blood vessels and relieve tension and spasm. At the first stage, infusions with plasma substitutes are also given.
The second stage of drug treatment is electrophoresis using vasodilating solutions (Drotaverine, Bendazole).
For high intraocular pressure, carbonic anhydrase inhibitors are prescribed: Diacarb, Dorzamed, Rosalin, Azopt, Simbrinza and saluretics (diuretics).
Instillation of drops (Timolol, Pilokartina hydrochloride) is indicated.
If there is no therapeutic effect, the patient is given retrobulbar injections, and medicinal solutions are injected through the skin of the lower eyelid along the lower edge of the orbit.
Folk recipes
Traditional medicine methods for retinal vasospasm are aimed not only at alleviating the condition of the eyes, but also at treating the underlying disease.
Avoid foods that contribute to the deposition of cholesterol plaques from the diet:
- pork;
- smoked meats, sausages;
- offal;
- baked goods, confectionery products;
- full-fat milk, butter;
- rich broths.
Folk remedies for retinal vasospasm are taken only orally. It is strictly forbidden to drop decoctions, tinctures into the eyes, make baths, lotions, or compresses.
- Recipe No. 1. Take 1 tbsp. l. dill seeds, pour a glass of boiling water, let it brew for an hour. Strain, divide into two doses, drink in the morning and evening half an hour before meals.
- Recipe No. 2. Take 1 tbsp. l. caraway seeds, add 200 ml of water, bring to a boil, simmer for 5 minutes. Remove from heat, add 1 tsp. blue cornflower flowers and leave for 1 hour. Strain, bring to a volume of 200 ml, adding clean boiled water. Drink 100 ml 2 times a day.
Teas made from chokeberry fruits and black currant leaves are beneficial.
Complications and prognosis
Prolonged spasm and poor circulation lead to irreversible loss of vision. Periodic spasms of capillaries provoke constant eye pain.
Frequent acute attacks cause discomfort and reduce ability to work. The situation is complicated by the fact that a person cannot predict the progression of an attack; symptoms appear suddenly and sharply. Relapses contribute to stable intraocular pressure. This is how ocular hypertension develops above 20 mmHg. Art., while there are no changes in the fundus, as with glaucoma.
Short-term attacks of vasospasm do not cause complications.
The prognosis of the disease directly depends on the severity of the clinical picture. Adverse effects are observed in patients with attacks lasting more than 15 minutes. This time is enough for destructive processes to begin in the retina.
Prevention rules
There is no specific prevention against retinal vasospasm.
Nonspecific methods of preventing the disease:
- regular monitoring of blood pressure in people with a predisposition to hypertension;
- systematic monitoring of blood sugar levels in patients with prediabetes and diabetes mellitus;
- daily use of statins (drugs to lower blood cholesterol) for severe atherosclerosis;
- compliance with labor safety rules in industries with a high risk of poisoning by toxic chemicals, wearing personal protective equipment.
Retinal angiospasm, with timely diagnosis and adequate treatment, does not affect a person’s quality of life. Advanced pathology can lead to partial, and over time, complete loss of vision.
Source: https://oculistic.ru/bolezni/drugie-zabolevaniya/cimptomy-angiospazma-setchatki-glaza-lechenie-i-profilaktika
Features of the course of the disease during pregnancy and childbirth
Help: The manifestation of angiopathy is an important signal about disturbances in the functioning of blood vessels, but often after childbirth the unpleasant symptoms go away on their own.
The patient’s condition during labor and subsequent birth is also important. So, in the presence of this pathology, experiencing strong physical stress immediately at the time of birth, the patient increases the likelihood of vascular rupture, which can lead to complications, namely:
- hemorrhage into the eye cavity;
- thrombosis of the fundus vessels and partial loss of vision;
- retinal detachment with complete loss of vision.
In such cases, if the expectant mother is found to have both high blood pressure and severe symptoms of angiopathy, then doctors refuse natural childbirth in favor of cesarean section.
It is better not to start treatment for a disease unless it is severe. When starting, the doctor should consider all the pros and cons, but it is better not to implement drug therapy, because during pregnancy this can affect the health of the unborn child. Experts try to avoid prescribing drugs that normalize blood flow in the vessels of the eyeball, which are usually prescribed to every sick person.
Smasmophilia is a pathological condition characterized by increased nervous muscle excitability and frequent clonic convulsions. The disease can appear in a child between three months and two years of age. According to statistics, boys are more likely to get sick. After a year, the disease manifests itself in the form of spasms of individual muscle groups.
More often they occur in spring or late winter. The cause is a violation of the metabolism of phosphorus and calcium, as a result of which the level of calcium in the blood decreases. Keeping your baby exposed to sunlight for a long time may also be one of the reasons. Disruption of the parathyroid glands leads to a decrease in calcium and its active excretion in the urine, which also leads to spasmophilia. A negative factor is also a decrease in the content of sodium, magnesium, chlorides, vitamins B6 and B1.
Spasmophilia can occur in latent, overt or hidden form. The latent form becomes overt when the baby develops rickets due to vitamin D deficiency. The latent form is expressed by restless sleep, increased sweating, fearfulness and anxiety.
At the end of the attack, the child takes two to four shallow wheezing breaths, and then breathing returns to normal. It happens that an attack leads to death. Tetany manifests itself as a spasm from three hours to several days. Cramps cause severe pain. The feet may swell. Eclamptic convulsions are manifested by twitching of the facial muscles, as well as the muscles of the neck, leg or arm.
To diagnose the disease, various methods are used - Trousseau, Lyust, Khvostek, Maslov. They are based on identifying the degree of nervous excitability.
If a baby suffers from spasmophilia, then after six months it is necessary to introduce fruit and vegetable dishes into the diet. A bottle-fed baby needs to reduce the amount of milk, replacing it with vegetables and fruits. The baby should be in a calm environment and walk in the fresh air more often.
Angiospasm of the retina, what is it? Retinal angiospasm is not considered to be an independent pathology; the disease develops against the background of other diseases affecting the vascular system. This is a functional damage in which there is a sharp narrowing of the blood vessels in the eyes.
In this case, no pathological changes in the structure of the vessel are observed, however, there is a violation of metabolic processes. This leads to poor vision
When the first signs appear, it is important to make a diagnosis and begin treatment as soon as possible
With vasospasm of the retina, there is a sharp narrowing of the artery of the eye or its branches - smaller vessels that penetrate the retinal tissue, providing its nutrition. In this case, the spasm does not lead to the development of destructive changes and disruption of the structure of the affected vessel.
Depending on the causes of development, a unilateral or bilateral form of the disease is distinguished. The second option is accompanied by damage to both eyes and is considered the most severe form.
ATTENTION! The disease is considered a very dangerous ophthalmological problem. Lack of therapy can lead to serious complications
One of them is retinal dystrophy, accompanied by significant or complete loss of vision.
The very first thing to do is to establish the cause of the development as soon as possible. Doses of drugs must be selected very carefully depending on the age of the child.
Prevention
The main goal of prevention is to prevent complications from the main disease: high blood pressure, diabetes mellitus.
All patients must follow the following rules:
- Visit an ophthalmologist several times a year and undergo preventive examinations;
- Complete cessation of bad habits;
- Pay due attention to sleep and rest;
- Watch your diet;
- Distribute physical activity correctly;
- Diseases that have a negative impact on blood vessels must be treated promptly.
Treatment of fundus vasospasm is lengthy and difficult. There is no need to panic or despair, as timely treatment starts gives a high chance of recovery. When the first signs of pathology appear, you should immediately visit the hospital and undergo a full examination.
Features of treatment
After the diagnosis, the ophthalmologist will prescribe you complex therapy for false myopia, which will include:
- drug treatment using drops that dilate the pupil and relax the fibers of the ciliary muscle;
- physiotherapeutic procedures;
- hardware treatment;
- special therapeutic exercises for the eyes.
Hardware treatment involves the use of different techniques. Your doctor may recommend that you:
- electrical stimulation of the eyes using current pulses;
- eliminating spasms using Sidorenko glasses - they provide an electric vacuum massage and improve blood flow in the eyes;
- acupuncture can improve visual acuity and stop the development of the pathological process;
- magnetotherapy involves stimulation of the ciliary muscles with a special electromagnet with alternating current;
- specially developed computer programs help train the ciliary muscle;
- electrophoresis makes it possible to quickly deliver medications to the optical sphere of the eyes.
In eye clinics, laser therapy is deservedly considered the most effective way to treat false myopia. It helps stimulate the ciliary muscle and speeds up metabolic processes. Laser therapy quite quickly and effectively eliminates spasm of accommodation. In addition, this procedure is considered absolutely safe, since a special neon laser is used in the process.
If, during the examination, a relationship between spasm of accommodation and spinal pathologies was revealed in a child or adult, massage sessions of the collar area and back, as well as therapeutic exercises, are required.
Development mechanism
This condition is caused by tension in the ciliary muscle, which simply loses the ability to change the curvature of the lens. As a result, after natural refraction in the optical sphere, the beam is focused not on the retina, as expected, but in the plane located in front of it.
Gradually the lens becomes convex. It changes its shape depending on the relaxation or tension of the ciliary muscle. When looking into the distance, its fibers become relaxed and the lens becomes almost flat. If the object is close, the muscle, on the contrary, contracts and the lens becomes convex.
When working with a nearby object for too long, muscle tension is fixed, a spasm occurs, and the lens no longer changes its shape. Of course, the clarity of the picture with distant objects is significantly reduced.
According to statistics, this pathology is much more common in children of preschool and school age, but in adults it is diagnosed extremely rarely. False myopia got its name due to the fact that such a vision defect is reversible and can usually be easily treated. But if you do not start therapy on time, blood flow in the fibers of the ciliary muscle will be disrupted, the ligaments that support the lens will become weaker, and it will stop changing its shape. As a result, permanent myopia may appear, and vision will lose its sharpness. So you definitely shouldn’t delay treatment.
The code for spasm of accommodation according to ICD-10 is H52.5.
Symptoms and diagnosis
With retinal vascular spasm, patients complain of the following:
- periodic blurred vision (can last from 1-5 minutes to an hour);
- the appearance of spots before the eyes;
- headache;
- discomfort in the eye area;
- sensation of pulsation in the temples;
- distortion of vision.
Signs of eye changes and well-being depend on the location of the pathological process and the presence of concomitant diseases. Thus, patients with stage II cervical spine osteochondrosis complain of changes in visual perception, darkening, the appearance of flickering, sparks and colored spots before the eyes. During an attack, hyperemia (redness of the mucous membrane of the eyes) and swelling of the conjunctiva are possible. After the end of the attack, visual dysfunction can be leveled, and the general condition of the patient can be completely normalized.
The main method for diagnosing the disease is ophthalmoscopy using a mirror or electric hand-held ophthalmoscope. If you conduct an examination during spasms, you can detect characteristic signs of malnutrition in the fundus:
- a sharp narrowing of the CAS and its branches;
- pallor of the fundus;
- swelling and waxy appearance of the optic disc.
The examination does not require special preparation of the patient, it is painless and does not take much time. Diagnostics includes testing, because in most cases, vascular spasms are associated with diseases of internal organs and systems, and if necessary, additional examinations are prescribed:
- non-contact tonometry;
- retinal antiography;
- Retinal OCT.
Causes
Angiospasm of retinal vessels is not an independent disease. It can appear in various pathologies. Causes of the disease:
- diabetes;
- Raynaud's syndrome;
- endocrine and mental disorders associated with diseases of the central nervous system;
- atherosclerotic vascular lesions.
If cramps last up to 15 minutes, they do not pose any particular health hazard. But if they appear frequently and last a long time, then blood circulation is disrupted, the central retinal artery (CRA) and the membranes of vascular cells do not receive potassium, sodium, and calcium. Swelling forms in the spasm area, the walls of blood vessels weaken, and the muscles do not relax.
The risk group includes:
- weather-sensitive people;
- straining the eyesight (for example, when working at a computer);
- those suffering from chronic intoxication when working with lead or carbon disulfide compounds in industries with hazardous working conditions;
- exposed to hypothermia;
- pregnant women during the period of late toxicosis;
- smokers, alcoholics and drug addicts.
Prognosis and prevention
The prognosis for vasospasm depends on the nature of the attack. Short-term narrowing of the small branches of the central nervous system of the eyeball passes without a trace. Vasospastic reactions lasting more than 15 minutes, when irreversible changes in the retina occur, are considered unfavorable in terms of prognosis. Specific preventive measures have not been developed. Nonspecific prevention comes down to monitoring blood pressure and blood glucose levels, taking statins for atherosclerosis, and using personal protective equipment when working with pesticides in an industrial environment.
Retinal angiospasm is a functional disorder of the retina. The disease appears as a result of intense contraction of the muscles of the walls of blood vessels, when they spasm, narrow and cut off the blood supply to the tissues of the organ to one degree or another.