Atherosclerosis of the vessels of the lower extremities is a disease in which lipid metabolism is disrupted; cholesterol plaques form on the walls of the arteries of the legs, narrowing their lumen. Mild forms of the disease are asymptomatic, moderate and severe forms are manifested by deterioration of the skin, nails, pain, cramps, trophic ulcers, even gangrene.
Stages, degrees of pathology
The formation of cholesterol plaques is a long process, consisting of several stages. Depending on the severity of the disorders, doctors distinguish 4 stages:
- Asymptomatic. While the fatty formation is small in size, the narrowing of the lumen of the vessel is slightly expressed. The body manages to compensate for the limited patency and deliver a sufficient amount of blood to the leg muscles. Due to this there are no symptoms.
- Moderate intermittent claudication. Appears when large plaques become a mechanical barrier to normal blood flow. The muscle fibers of the limb begin to experience a deficiency of oxygen and nutrients, which is clinically manifested by pain during physical activity. There are two degrees of severity of intermittent claudication: 2a – lameness develops when walking at a distance of 200 m to 1 km; 2b – a person begins to limp after walking less than 200 m.
- Pain at rest. The patient experiences persistent pain in the legs, which gets worse when leaning back or raising the legs. Relief comes from sitting or standing.
- Gangrene. Accompanied by necrosis of tissues of the lower extremities with complete/almost complete blockage of the artery.
| Degree | Pain and weakness in legs when walking | Trophic disorders |
| First | Heavy loads, walking more than 1 km | Externally, the legs and feet do not change |
| Second | From 200–300 m to 1 km | Pale skin, impaired hair growth |
| Third | From 50 to 200–300 m | Hypotrophy, trophic ulcers |
| Fourth | Less than 50 m and at rest | Gangrene of a finger or foot |
Diagnostics
To identify vascular stenosis of the lower extremities, the doctor performs:
- interviewing the patient and taking a medical history;
- examination of the patient to determine objective symptoms;
- condition of the skin, veins in the legs, checks tendon and nerve reflexes,
Prescribes examinations to determine the degree of vasoconstriction:
Laboratory diagnostics:
- urine and blood analysis;
- coagulogram;
- lipid profile;
- immunogram;
- D-dimer determination;
- gas and acid composition of blood;
There is no universal diagnostic method. Each method has advantages and disadvantages, as well as contraindications. The required type of examinations and their scope are selected by the attending physician together with a neurologist and cardiologist from the list provided.
Instrumental diagnostics
- tonometry;
- duplex (triplex) scanning;
- Doppler ultrasound;
- contrast angiography;
- ophthalmoscopy;
- CT (computed tomography);
- MSCT (multispiral CT);
- MRI (magnetic resonance imaging);
- infrared thermography;
- ECG (electrocardiography);
- ECG with a certain physical activity;
- EchoCG (echocardiography);
- bicycle ergometry, spiroergometry;
- REG (rheoencephalography);
- radionuclide scintigraphy
- EEG (electroencephalography).
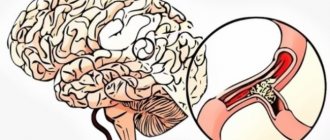
Of the listed diagnostic methods, angiography is considered the most informative. A contrast agent is injected into the femoral artery and the condition of the leg veins is imaged using X-rays. The image shows the places of narrowing of blood vessels and the formed collaterals (branches of blood vessels replacing dead channels). Contraindicated in patients with allergies (to iodine) and renal failure.
The percentage of vasoconstriction is well determined using Doppler ultrasound. During the examination, a special drug test can be performed to determine the functional reserve of the vessel. Nitroglycerin is administered to cause vasospasm.
Contrast-enhanced tomography to establish the ankle-brachial index helps determine the extent of vascular damage.
Main causes of the disease
It takes 30-40 years for a mature cholesterol plaque to form. During this time, the body is exposed to the harmful effects of various factors that contribute to the growth of existing deposits and the formation of the beginnings of new ones. The greatest role in the development of atherosclerosis of the legs is played by:
- smoking – there is a history of 80-90% of patients;
- diabetes mellitus – increases the risk of atherosclerosis by 2-4 times;
- age-related arterial damage - most patients at the time of diagnosis of the disease are over 50 years old (men) / 60 years old (women);
- high levels of bad cholesterol;
- hypertension – increases the chances of developing pathology by 2.5-4 times;
- any chronic diseases accompanied by an increase in the concentration of CRP factor, fibrinogen, high blood viscosity, and a tendency to thrombosis.
People with:
- overweight;
- genetic predisposition;
- sedentary lifestyle;
- men;
- lovers of foods containing excess cholesterol, saturated fats, and a diet poor in fiber.
Causes
Smoking is considered the main cause of narrowing of the blood vessels in the legs. A bad habit leads to spasm of the arteries, which prevents normal blood from circulating in the body. Nicotine increases the likelihood of blood clots forming that block the lumens of blood vessels. Other causes of stenosis include the following factors:
- increased levels of cholesterol in the blood (when eating foods containing animal fats, plaque accumulates on the walls of the arteries);
- arterial hypertension (the disease is characterized by impaired blood circulation in peripheral vessels, which causes thrombosis);
- obesity (excess weight increases stress on the legs and disrupts metabolism, impairing blood circulation);
- genetic predisposition (if close relatives have venous stenosis of the lower extremities, the risk of developing the disease increases several times);
- staying in an uncomfortable position for a long time, wearing tight shoes (these factors contribute to mechanical compression of tissues with subsequent poor circulation);
- diabetes mellitus (advanced forms of the disease lead to the development of inflammatory processes in the walls of arteries and veins);
- pathologies of the excretory system;
- excessive physical and psycho-emotional stress;
- hypothermia of the body;
- varicose veins;
- systemic vasculitis (autoimmune pathology violates the integrity of the vascular walls, leading to blockage of the lumens of veins and arteries);
- long periods of standing.
Characteristic symptoms
The clinical picture depends on the degree of stenosis. There are two main forms that differ in external manifestations.
Stenosing stage
It develops when the plaque reaches a large size sufficient to narrow the lumen of the artery. The pathology is typical for stage 2-3 atherosclerosis of the legs. In the initial stages, it manifests itself as chilliness of the lower extremities, a sensation of goosebumps, and a burning sensation.
As the plaque grows, intermittent claudication appears - a pathological condition that patients describe as fatigue and pain that occurs while walking. A little rest brings relief. Insufficient nutrition of the skin of the feet makes it dry. Any wounds heal poorly, hair falls out. Nails acquire an unhealthy color and become dull.
Obliteration stage
Occurs with complete/almost complete blockage of the arteries (stage 3-4). A nagging, burning pain bothers a person even during rest. The condition of the skin worsens, it becomes thinner. Any injury does not heal for a long time. Complications appear in the form of cracks and ulcers. Distances of more than 25-50 meters are already accompanied by unbearable pain, which is why the patient rarely leaves the apartment.
The terminal stage of obliterating atherosclerosis of the lower extremities is characterized by the appearance of non-healing trophic ulcers - open areas of inflammation filled with dirty gray contents. The feet and legs swell greatly, and tissue necrosis—gangrene—begins to develop.
Treatment: which methods are effective?
Drug therapy
All medications are prescribed by a doctor; self-medication can aggravate the condition. Complex treatment includes taking the following medications shown in the table:
| Pharmgroup | Name |
| To reduce lipid fractions | "Simvastatin" |
| "Gemfibrozil" | |
| "Fluvastatin" | |
| "Bezafibrate" | |
| To normalize blood pressure | "Atenolol" |
| "Captopress" | |
| "Bisoprolol" | |
| "Lisinopril" | |
| Antispasmodics | "Papaverine" |
| "Drotaverine" | |
| "No-shpa" | |
| Anticoagulants | "Heparin" |
| "Acetylsalicylic acid Cardio" | |
| "Parsedyl" | |
| "Angioflux" | |
| To improve blood circulation | "Nootropil" |
| "Vinpocetine" | |
| Thromboid dissolving | "Vizaprostan" |
Surgical intervention
If the narrowing of the blood vessels in the legs is not cured conservatively, surgery is required. To alleviate the patient's condition, the following techniques are used:
The pathology can be eliminated with shunting.
- Cryoplasty, in which nitrogen is introduced into the vessel cavity, destroying atherosclerotic plaques - one of the causes of stenosis.
- Angioplasty. It is characterized by the introduction of a catheter into the vessel with a balloon at the end, which expands the walls. Protects the vascular tubes of stents.
- Shunt installation. An open operation, when a shunt made from the saphenous vein is installed on the damaged area.
Physiotherapy
For vascular stenosis of the lower extremities, it is recommended to undergo a course of physical procedures such as:
- magnetic therapy;
- laser treatment;
- phonophoresis;
- electrophoresis;
- shock wave therapy;
- inductothermy;
- infrared irradiation;
- electromyostimulation;
- exposure to ultrasound.
Physiotherapeutic methods have the following therapeutic effect on narrowed veins:
Such procedures help relieve pain in the limbs.
- normalize blood and lymph flow;
- relieve pain and swelling;
- strengthen blood vessels and muscles;
- saturate the tissues of the lower extremities with oxygen;
- improve cellular metabolism;
- restore nerve conduction;
- eliminate excess adipose tissue.
Treatment with traditional methods
The use of drugs prepared independently is possible in the initial stages of the development of the disease and only after consultation with a doctor.
To dilate blood vessels, healers advise preparing the following remedy:
- Take 2 tbsp. l. hawthorn fruit and add 200 ml of water.
- Put on fire, bring to a boil and simmer for 5-7 minutes.
- Remove from the stove, leave, cool.
- Drink 10 ml per 20 minutes. before every meal.
Healers recommend a medicinal compress, which is prepared as follows:
To prepare a compress, you need to chop the parsley.
- Take a few parsley stems with leaves and chop.
- Pour 100 ml of boiling water and leave for 20 minutes.
- Filter.
- Add milk.
- Soak gauze in the product and apply it to the sore leg.
Critical stenosis can be cured with the following remedy:
- Take 10 g of crushed oak bark and barberry root.
- Add 0.5 liters of hot water.
- Let it brew for 4 hours and filter.
- Take 100 ml before meals.
Modern methods of diagnosis and treatment
After reviewing the patient’s complaints, assessing the appearance of the skin of the legs and nails, and palpating large vessels, the doctor makes a preliminary diagnosis. It can be confirmed using functional tests - simple tests that help the surgeon examine the state of blood flow.
Further instrumental examination is necessary to determine the location and amount of cholesterol deposits.
- Dopplerography is an ultrasound scan, the doctor evaluates the speed of blood flow, size, localization of the atherosclerotic plaque, and the features of its structure.
- Angiography – obtaining a clear image of the vascular network using X-rays, MRI or CT. It involves the preliminary introduction of a medical dye, which makes the contours of arteries, veins, capillaries, and lipid formations clearly visible.
Symptoms and stages of the disease
In the classic version, the symptoms of atherosclerosis of the lower extremities are of an increasing nature: they intensify as the disease passes from one stage to another. If at the beginning of the pathological process the patient feels virtually no changes, then by the final stage he is bothered by a whole set of painful symptoms.
What symptoms does atherosclerosis have with varying degrees of damage to the arteries of the legs by atherosclerotic complications:
- Preclinical stage. There are no alarming signs for atherosclerosis of the lower extremities at this stage of the disease. Pathological changes can be detected only during instrumental examination of the vessels of this part of the body and during laboratory blood tests, which indicate a violation of lipid metabolism.
- The second stage, which in medicine is called non-stenotic atherosclerosis of the arteries of the lower extremities. The lumen of the vessels is narrowed, but not critically. Discomfort in the form of acute or aching pain in the legs occurs after a long walk of about a kilometer. After a short rest the pain goes away. Pallor and numbness of the feet may also be observed with increased load on the legs, and night cramps.
- The ischemic or third stage is characterized by severe symptoms, when pain appears after walking short distances (50-100 m). Often the disease takes on more threatening features if the arteries of the legs become stenotic, that is, severely narrowed in a small area. This form of the disease is accompanied by paleness of the legs during exercise, increased sensitivity to cold, and changes in the skin: it becomes dry, flaky, and pale.
- The fourth stage of atherosclerosis of the arteries of the lower extremities is accompanied by the most pronounced alarming signs. The pain persists constantly and intensifies with the slightest physical activity. The patient's gait becomes shuffling. External changes also take place: the skin and nails become thinner, become brittle and peel, trophic ulcers and areas of necrosis (blackened skin) appear on the ankle and foot. The reason for such deterioration is stenosis of the arteries of the legs with complete blockage of the blood vessels by atherosclerotic plaques.
If you do not treat stenosing atherosclerosis of the arteries of the lower extremities at stages 3 and 4, there is a high probability of developing gangrene with subsequent amputation of the legs.
Since the disease tends to gradually increase symptoms, patients postpone a visit to the doctor until it becomes difficult for them to move even within their own home. This happens because most patients are sure that pain in the legs is a consequence of natural wear and tear of the musculoskeletal system, and not a sign of a serious problem with the blood vessels.
To independently differentiate the disease, it is enough to pay attention to the following feature: with atherosclerosis, pain comes from muscles that lack oxygen and nutrients. Vascular insufficiency can also be determined by weakening of the pulse under the knee. It is either not palpable at all, or is felt too weakly.
Diet, nutritional habits
Diet is an important component of the treatment regimen; to normalize fat metabolism, doctors recommend:
- Drink 1.5-2 liters of water daily. Otherwise, the body begins to escape dehydration by increasing cholesterol synthesis.
- Limit your intake of saturated fat. They increase the level of bad cholesterol and contribute to the formation of atherosclerotic plaques. The body's need for lipids is better met through unsaturated fatty acids.
- Eliminate trans fats. These lipids are considered the most atherogenic component of the diet.
- Make sure your diet contains enough omega-3 fatty acids. They are natural lipid-lowering drugs that effectively reduce the concentration of triglycerides, low-density lipoproteins, and increase the content of healthy cholesterol.
- Eat more fiber-rich foods. Dietary fiber promotes normal digestion and inhibits the development of atherosclerosis.
- Alcohol - only in moderate doses. Small portions of alcoholic drinks have a beneficial effect on vascular health and increase the concentration of good cholesterol, which prevents the formation of lipid deposits. However, higher doses have the opposite effect. The maximum permissible daily alcohol consumption for women should not exceed 14 g of ethyl alcohol, for men - 28 g.
Sources of harmful, beneficial nutrients
| Harmful | |
| Saturated fats |
|
| Trans fats |
|
| Useful | |
| Unsaturated fats |
|
| Omega-3 fatty acids |
|
| Cellulose |
|
Causes
Obliterating atherosclerosis affects predominantly men; the development of pathology is facilitated by:
- Smoking . About 90% of patients with atherosclerosis are long-term smokers.
- Insufficient physical activity . Among people leading a sedentary lifestyle, vascular pathologies are more common.
- Alcohol . Systematic and excessive consumption of alcoholic beverages accelerates the course of the disease.
- Violation of the principles of healthy eating . An abundance of smoked, fried, and fatty foods contributes to the formation of cholesterol plaques.
- Chronic stress and neuro-emotional overload cause vasospasms, which impair blood circulation in the tissues.
- Chronic diseases . Atherosclerosis can develop against the background of diabetes mellitus, obesity, rheumatism, tuberculosis, hypertension and other pathologies of the cardiovascular system.
Risk factors can be divided into two groups: they either lead to constant narrowing of blood vessels, impede blood circulation and accelerate the deposition of cholesterol, or increase the content of cholesterol and related lipoproteins in the blood.
Exposure to one or more risk factors accelerates the aging process in the walls of blood vessels, loss of elasticity and creates ideal conditions for their gradual hardening.
Ointments, tablets and medications
Prescribing medications helps stop the growth of existing plaques, prevent the appearance of new ones, improve the patient’s overall well-being, and restore blood flow. Drug therapy is always accompanied by following a diet and getting rid of bad habits.
Therapy of atherosclerosis involves prescribing a complex of drugs for the legs:
- antispasmodics;
- non-steroidal anti-inflammatory drugs;
- anticoagulants;
- lipid-lowering drugs;
- tissue metabolism activators;
- local drugs.
Of course, one patient rarely receives all categories of tablets and ointments. Usually the doctor selects 3-6 medications that most effectively solve the patient’s problems.
Antispasmodics
Antispasmodics are medications that relieve spasms of smooth muscles. Prescribing antispasmodics helps the arteries increase their lumen, relax, and facilitate blood flow through them.
Papaverine, but-shpa is not recommended for patients with atherosclerosis. These medications dilate large vessels, but provoke the formation of atherosclerotic plaques in smaller ones. Cardiologists prefer drugs containing pentoxifylline (Trental, Vazonit) or alprostadil (Vasaprostan). Both medications are given intravenously.
Prevention of vascular lesions of the lower extremities
The peculiarity of blood flow in the vessels of the legs is increased blood flow through the main arteries and difficult outflow due to counteraction to gravity. The occurrence of atherosclerosis and other vascular pathologies is directly related to the influence of environmental factors.
Primary prevention means:
- adequate physical activity (at a young age - playing sports, at an older age - daily walking);
- correction of body weight (obesity increases the volume of circulating blood, increases blood pressure, and stress on the blood vessels of the legs);
- control of lipid levels in patients with a family history;
- a balanced diet enriched with B vitamins, proteins, polyunsaturated fatty acids (in vegetable oils), phospholipids (sea fish);
- compensation for diseases of other organs and systems;
- giving up bad habits: smoking, drinking alcohol.
Surgical treatment
Stenosing atherosclerosis of the vessels of the lower extremities is accompanied by a noticeable deterioration in the health of patients and is an indication for surgical intervention. There are several surgical techniques used in modern practice:
- Stenting is a procedure in which the doctor widens the lumen with a miniature balloon that is inserted through a large artery. At the first stage, he flattens the cholesterol plaque, then the doctor attaches a tiny frame (stent) to the site of the lesion, which will prevent relapse of stenosis.
- Laser angioplasty is the removal of deposits with a directed laser beam.
- Bypass surgery is a more complex operation, during which the doctor creates a “bypass” path for blood flow by sewing a vascular graft above, below the site of stenosis.
- Sympathectomy – removal of the sympathetic nerves. If the spasm cannot be relieved with medication, resection of the nerve fibers may solve the problem. This operation is indicated for seriously ill people who will not survive more extensive surgery, as well as for patients with multiple lesions.
- Amputation – used for necrosis of the toes, feet, legs.
The operation does not exclude the need for conservative therapy, nutritional correction, and lifestyle. On the contrary, the success of surgery largely depends on the effectiveness of anti-relapse therapy.
Clinic and main symptoms of the disease
The appearance of clinical signs is associated with a narrowing of the vessel lumen by more than 75%. Most often, the pathological process is localized in the lower abdominal aorta (below the origin of the renal arteries): 33% - aortoiliac segment, 66% - femoropopliteal.
The emergence of an atherosclerotic plaque with the formation of fibrosis (dense connective tissue) can be considered as an adaptation mechanism in response to trauma and aseptic inflammation of the inner lining due to the strong blood flow in the main arteries.
Typical signs of lower extremity lesions
The symptoms of the disease are caused by impaired blood delivery through the affected vessels to the muscles and nerve fibers.
The most characteristic symptoms of atherosclerosis of the vessels of the lower extremities:
- decreased tolerance to physical activity (fatigue when walking);
- intermittent claudication is a specific symptom that is characterized by the appearance of intense pain (burning) in the leg during physical activity, the need to stop and rest;
- neuropathies arise due to impaired nutrition of nerve fibers and are felt by goosebumps, numbness, and convulsions;
- change in skin color (pallor) of the legs, local decrease in temperature;
- thinning of the layer of subcutaneous fatty tissue, muscle atrophy (the volume of the limbs differs from each other with unilateral lesions);
- atrophy of hair follicles (hair on the legs becomes thin, brittle, and falls out over time);
- hyperkeratosis of the skin of the feet and nails.
The severity of symptoms is determined by the level, extent and degree of narrowing (stenosis). In addition, the presence of concomitant aggravating factors (diabetes mellitus, smoking, old age) worsens the prognosis for the patient’s life and health.
Manifestations of the disease in older people: what are the features?
The diagnosis is more often made in men, since the fairer sex has a protective effect of estrogen before menopause, which prevents the development of atherosclerosis. In addition, pathology is more often diagnosed in older people due to the depletion of adaptive and compensatory mechanisms. Features of atherosclerosis of the lower extremities in such patients are:
- slow progression of symptoms due to damage to nerve fibers;
- high intensity of pain syndrome (the reason is that the collateral arteries, which provide the minimum necessary blood flow in the tissues, no longer grow);
- systemic disorders: weight loss, exhaustion, mental status disorders;
- progressive muscle atrophy;
- frequent ulcers that cannot be treated conservatively;
- high risk of complications (in 30% of cases): gangrene, septic conditions.
Additional chronic pathologies of the respiratory system, heart, and kidneys complicate diagnosis and selection of effective treatment.
Amputation of the lower limb is prescribed in 45% of cases in elderly patients, which leads to disability and a deterioration in their quality of life.
Lifestyle changes, disease prevention
Taking medications should be supplemented with diet, physical activity, and cessation of smoking and alcohol.
It has been proven that in addition to a balanced diet, you can stop the progression of pathology, achieve improved well-being, and increase the effectiveness of taking medications:
- giving up smoking;
- moving more - at least 30 minutes of walking/day, playing sports 2-3 times/week;
- maintaining a healthy weight (BMI less than 25 kg/m2);
- learning to relax and deal with stress.
Therapeutic exercise is recognized as a more effective method of treating atherosclerosis with damage to the peripheral arteries of the lower extremities than simply uncontrolled physical activity, especially in the early stages of the disease.
Special gymnastics classes allow you to (2):
- increase the distance of pain-free walking;
- improve quality of life;
- accelerate the healing of skin defects.
Atherosclerosis can be prevented by following dietary recommendations and lifestyle changes. It is also necessary not to develop systemic diseases (arterial hypertension, diabetes, migraines, sleep apnea), undergo annual medical examinations, and consult a doctor when the first symptoms appear.
As a background treatment, you can use folk remedies, which are described in more detail in this article.
Disease prognosis
The prognosis for the natural course of obliterating atherosclerosis of the leg arteries is unfavorable. This is largely due to damage not only to the arteries of the legs, but also often to the vessels of the heart and brain.
- The chance of losing a leg due to gangrene is about 10% per year.
- The probability of losing your ability to work due to the inability to walk is 25%.
- The probability of developing a vascular accident in the heart or brain is approximately 40% over 5 years of observation.
- People in the world most often die from vascular atherosclerosis.
Medical prognosis
For most people with atherosclerosis of the lower extremities, the prognosis is good. Mild and moderate patients usually suffice with conservative therapy and correction of risk factors; severe cases require surgical intervention.
In patients with diabetes mellitus, grade 3 hypertension, severe hypercholesterolemia, the disease is more complicated and is often accompanied by serious complications: stroke, myocardial infarction, gangrene (3). Women are more likely than men to need blood transfusions, have concomitant cardiovascular pathologies, and an increased risk of embolism. But gender has no effect on mortality rates or the likelihood of heart or cerebral attacks (1).
Drugs for the treatment of atherosclerosis of the lower extremities
The main symptom indicating the severity of the disease is lameness while walking, occurring alternately in one or the other leg. The severity of this symptom depends on the method of taking medications, namely the choice and dose of the drug.
Thus, treatment of atherosclerosis of the lower extremities involves the use of pharmacological drugs for the treatment of OASNK:
- Medicines that block the formation of an enzyme involved in the synthesis of cholesterol.
- Acetylsalicylic acid, which thins the blood and promotes its fluidity.
- Cilostazol - dilates blood vessels and inhibits the production of the enzyme responsible for platelet aggregation.
- To enhance blood fluidity - purine derivatives (trental)
- Glucurono-amino-deoxyglucoglucan sulfate is an angioprotector that also reduces the amount of fibrinogen and lipid levels.
- Arginine, a substance that restores the structure of the vascular wall.
- Carbiogenplasmid – stimulates the formation of bypass vascular branches.
In addition to drugs that have a direct effect on the affected vessels, additional drugs are used for a complex effect on the disease. Their selection is trusted only to the attending physician.
- Cholestyramine and its analogues, which bind and remove bile acids from the body that take part in the biosynthesis of LDL.
- Medicines that lower cholesterol.
- Hydroxymethylglutaryl reductase inhibitors - affect the production of lipids in liver tissue.
- Fibric acid preparations that correct lipid metabolism and reduce their quantitative composition in the blood.
In addition to the listed types of treatment, auxiliary ones are used:
- Drugs with antithrombotic effects.
- Substances that enhance blood circulation processes, eliminating pain.
- Agents that reduce hemocoagulation.
- Drugs with antispasmodic activity.
- External creams, gels, ointments with antimicrobial action, used for trophic lesions of the extremities.
- Groups of drugs that dilate blood vessels and have a hypotensive effect.
- Agents that enhance tissue metabolism.
- Vitamins.
Some substances used in the treatment of vascular occlusive disease should be considered in more detail.
Bile acid sequestrants
Medicines in this group are intended for the correction of hyperlipidemia.
Sequestration is isolation. In relation to this situation, the term used means that the drug (sequestrant) prevents the absorption of cholesterol-containing acids produced by the liver, as well as bile acids that are formed as a result of digestion.
In terms of their composition, sequestrants are insoluble synthetic compounds involved in metabolic processes. They capture and retain predominantly low-density lipids without being absorbed in the gastrointestinal tract, and remove them from the body. Losing a certain amount of cholesterol speeds up its metabolism. Drugs in this group have a minimum of undesirable effects, but also a number of contraindications.
When to see a doctor?
If a person is over forty years old, any unexpected sensations in the legs should be alarming : stiffness, heaviness, increased sensitivity to cold, chilliness, especially if they are combined with rapid fatigue and muscle pain. Troubles, insignificant at first glance, are in fact a threatening warning from the blood vessels about the presence of a pathological process.
The clinical picture of vascular pathologies in the early stages of development resembles the manifestations of other diseases not directly related to blood flow disorders. Therefore, the first symptoms of suspected vascular atherosclerosis (veins and arteries) of the lower extremities are a reason for a visit to a therapist , who will refer the patient to a specialist of the appropriate profile to receive treatment.
Pain that appears when walking is a direct indication that you cannot put off a visit to a phlebologist any longer . Painful sensations, changes in local temperature and skin color indicate that pathological changes have gone far enough and pose a serious threat, even a threat to life.
Very dangerous phenomena - difficult healing of scratches, small wounds, slower growth of nails, hair loss on the legs . If one or more symptoms are detected, you should immediately contact an endocrinologist (to rule out diabetes mellitus) or immediately contact a vascular surgeon.
Find out also about the symptoms and treatment of cerebral atherosclerosis - this is a similar disease that causes completely different consequences. The diet for cerebral atherosclerosis is also suitable for patients with a form of the disease in the lower extremities. Find out more about her.
What drugs are used for cerebral atherosclerosis? They are all listed here.
Complementary therapy
Along with medications, patients are often prescribed a course of massage, therapeutic exercises, physiotherapy, the use of essential oils, therapeutic mud or clay for manifestations of necrosis.
Massage helps to increase tissue tone, improve the movement of biological fluids, and strengthen the muscle corset. During the sessions, rubbing techniques of varying intensity, stroking and pinching are used. For atherosclerosis, many of the existing types of massage practices are allowed.
Therapeutic exercises are selected depending on the patient’s age, weight, stage of the disease and external chronic processes. The complex consists of exercises aimed at improving blood circulation, eliminating congestion, and strengthening muscles. You need to perform gymnastics daily in the absence of severe pain.
Effective additional therapy is hirudotherapy, wraps, and medicinal baths.
Diagnosis of obliterating atherosclerosis
The examination of a patient with suspected OA begins with recording complaints, taking an anamnesis and identifying bad habits.
The main goals of diagnosing atherosclerosis are:
- Confirmation of vascular pathology;
- Identification of the exact location of the lesion;
- Establishing the degree and prevalence of narrowing of the lumen of the vessel;
- Determination of the degree of ischemia of internal organs;
- Identification of cholesterol plaques with risks of rupture.
During diagnostic measures, it is necessary to identify all risk factors in order to clarify their influence on the development of the disease. During the physical examination, blood pressure and waist circumference must be measured. If it exceeds 88 cm in women and 102 cm in men, then this indicates the presence of metabolic syndrome.
The next stage is palpation and auscultation of the vessels of the legs. In the normal position of the arteries, the absence of a pulse in the popliteal region indicates damage to the femoropopliteal segment, and its disappearance in the femoral artery indicates blockage of the vessels of the iliac arteries.
Stenosing atherosclerosis of the arteries of the lower extremities of the obliterating form is detected by a blood test:
- According to the level of total cholesterol;
- By the amount of LDL at a norm of 3 mmol/l;
- According to the HDL level at a norm of 1 mmol/l;
- By triglyceride level;
- According to the level of c-reactive protein at a norm of 2 g/l;
- By identifying homocysteine in young people;
- In terms of apolipoprotein A1;
- According to apolipoprotein B.
If diabetes mellitus is previously diagnosed, then glycosylated hemoglobin and blood glucose levels are additionally determined.
Tests and samples
The Panchenko knee phenomenon test is performed from a sitting position. The patient places the sore leg on the healthy one, and if after some time there is pain in the calf muscles or numbness of the foot, a feeling of pins and needles, then OA is diagnosed. The Goldflam test is performed on a couch. The patient is asked to raise his legs and bend and straighten the knee several times. If blood circulation is impaired, the legs get tired after 10-20 repetitions. At the same time, the color of the skin changes, and in case of severe pathology of blood flow in the lower extremities, blanching of the foot occurs within a few seconds.
To calculate the brachial-ankle index, the ratio of blood pressure levels at the shoulder and ankle is used. When its value is less than 0.4, a severe form of atherosclerosis is diagnosed. With indicators from 0.41 to 0.7 - moderate severity, with 0.71 to 0.9 - moderate, and from 0.91 to 1.3 - slight deterioration in the elasticity of blood vessels. A normal ABI is above 1.31. When performing the Sitenko-Shamova test, the upper third of the thigh is compressed with an elastic bandage so that the artery is compressed. After a few minutes, the tourniquet is loosened and the time is noted. If there is no pathology, then the limb acquires a normal color after 10-15 seconds. The symptom of plantar ischemia is detected when the foot becomes pale when the legs are raised up at an angle of 45°. The rate of change in skin color depends on the degree of damage to the limb and in the severe stage ranges from 4 to 7 seconds.
Instrumental diagnostics
Instrumental diagnostic methods are prescribed to clarify the diagnosis, clarify the condition of blood vessels and determine the degree of damage to organs and tissues.
The rheography method consists of recording changes in the electrical resistance of muscle tissue with changes in pulse. This is explained by the difference in the filling of blood vessels during contraction and relaxation of the heart muscle. Using the program, you can determine the presence of occlusion, stenosis or thromboembolism. Angiography is also prescribed. It is a combination of radiography with the introduction of a contrast agent into the vessel under local anesthesia. An iodine-based contrast agent is administered through a catheter. The images show areas of narrowing and dilation of the vessel, the presence of blood clots, blood flow speed and the condition of the vascular wall.
Atherosclerosis of the vessels of the legs is also detected using duplex scanning, based on the ability of ultrasonic waves to be reflected from body tissues. When performing it, dopplerography and scanning of blood vessels are used in simultaneous or sequential mode. It depends on the capabilities of the device. The procedure allows you to study the structure of blood vessels, the speed and volume of blood flow. Using a duplex ultrasound diagnostic method, a two-dimensional image of the walls of blood vessels with places of formation of plaques, their components and condition is obtained.
Oscillography is a method of recording changes in pressure using special pneumatic cuffs or electronic sensors. Then the doctor evaluates the amplitude of the oscillations and determines the location of the pathology. This diagnostic method is usually used for mediasclerosis. The method of transcutaneous measurement of partial oxygen pressure involves placing sensors on the patient’s body that record changes in pressure at a depth of up to 100 microns. The method allows you to establish the level of critical ischemia and helps predict the healing of trophic ulcers.
MRI is the most accurate tool for diagnosing the disease and is new. Treatment of atherosclerosis of the lower extremities after examination with a tomograph allows you to adjust the dosage of drugs, select an appropriate course of physiotherapy and prevent circulatory disorders in small vessels. It is safe for all patients because... has no ionizing radiation. New diagnostic methods also include angioscopy, which involves examining the inner surface of the vascular wall using a special endoscope. Thermography allows us to determine the instability of cholesterol plaques and the degree of risk of their rupture.
Endovascular treatment
Endovascular treatment is a minimally invasive alternative to surgery and is used in later stages of atherosclerosis, when conservative methods are no longer effective enough. A device is inserted into the affected area of the artery to prevent further narrowing of the lumen of the vessel.
Endovascular treatment options include balloon dilatation, stenting, and angioplasty. The procedures are carried out in the cath lab, after which the patient is given a pressure bandage and placed on bed rest for 12-18 hours.
Surgery
Surgery is a last resort in treating leg disease. Surgery is prescribed only in cases of severe ischemic heart disease with severe complications, when drug therapy is powerless. The frequency of leg amputation after diagnosis within 1 year is up to 40%. What procedures are we talking about?
- Bypass surgery - organizing an additional opportunity near the problem area of the artery to normalize blood flow.
- Balloon angioplasty with placement of a balloon in the vascular bed to expand the clogged lumen.
- Vessel stenting, when a tubular spacer is inserted into the problem artery to control the size of the lumen at the expected level.
- Endarterectomy with removal of the affected area and clot accumulations.
- Autodermoplasty used in the treatment of trophic ulcers that are not amenable to local therapy.
- Prosthetics, which consists of replacing the affected area with an autovenous or synthetic vessel.
- Amputation of the necrotic part of the leg with further prosthetics.
WHO statistics on mortality after amputation: within a year - 20%, within 5 years - up to 70%, within 10 years - up to 95%. In the UK it is the second most common cause of disability and disability.