Statistics on the natural history of atherosclerotic lesions of the subclavian artery indicate a high incidence of disability and a pronounced decrease in quality of life. It should be noted the low effectiveness of conservative treatment - improvement is observed in only 10-15%.
Occlusive lesions of the proximal branches of the aortic arch are one of the main causes of the development of cerebrovascular insufficiency and ischemia of the upper extremities.
Atherosclerotic changes are found mainly in the initial segments of the extracranial arteries supplying blood to the brain. Intracranial lesions are found 4 times less often. Occlusions and stenoses more often affect the carotid arteries (54-57% of observations), approximately 20-35% more often than the arteries of the vertebrobasilar region. The frequency of atherosclerotic lesions of the 1st segment of the subclavian artery, according to various authors, is 3-20%. In 2/3 of patients, damage to the subclavian artery in the 1st segment is not accompanied by damage to other brachiocephalic arteries. In 17% of cases there is concomitant damage to the vertebral artery and/or the 2nd segment of the subclavian artery. In approximately the same percentage of cases, damage to the carotid system and/or the contralateral vertebral artery is noted. Bilateral damage to the subclavian artery is observed in approximately 2% of cases. The 2nd-3rd segments of the subclavian artery are affected much less frequently (mainly non-atherosclerotic lesions) and do not play a significant role in the pathogenesis of cerebrovascular and brachial ischemia. This led to a significant increase in the role of surgical methods and recognition of their leading role in the treatment of lesions of the subclavian artery.
Clinical picture and diagnosis
Stenosis/occlusion of the subclavian artery in the 1st segment in patients may manifest itself as one of the following symptoms or a combination of them:
- vertebrobasilar insufficiency;
- ischemia of the upper limb;
- symptoms of distal digital embolism;
- coronary-mammary-subclavian steal syndrome.
According to the literature, when the subclavian artery is damaged, vertebrobasilar insufficiency is observed in approximately 66% of cases (transient ischemic attacks in approximately 1/3 of patients, symptoms of ischemia of the upper limb in approximately 55%). About 20% of patients with damage to the subclavian artery do not have clinical symptoms. Distal embolism in the upper limb is observed in no more than 3-5% of cases. The incidence of coronary-mammary-subclavian steal syndrome in patients who underwent mammary-coronary bypass surgery does not exceed 0.5%.
General information
Occlusion of the subclavian artery is a complete closure of the lumen of the subclavian artery, accompanied by insufficient blood supply to the brain and upper extremities.
In vascular surgery and cardiology, stenosis and occlusion of the carotid arteries are more common (54-57%). Occlusion of the first segment of the subclavian artery, according to various authors, is found in 3-20% of cases; Moreover, in 17% of cases there are concomitant lesions of the vertebral artery and/or the second segment of the subclavian artery. Bilateral occlusion of the subclavian artery occurs in 2% of cases; the second and third segments of the subclavian artery are affected much less frequently and do not have independent significance in the pathogenesis of cerebrovascular ischemia. Occlusion of the left subclavian artery occurs 3 times more often than the right one. The subclavian artery is a paired branch of the aortic arch, consisting of the right and left subclavian arteries that supply blood to the upper limbs and neck. The right subclavian artery originates from the brachiocephalic trunk, the left one directly arises from the aortic arch. Topographically, 3 segments are distinguished in the subclavian artery. From the first segment depart the vertebral artery (supplies the spinal cord, muscles and dura mater of the occipital lobes of the brain), the internal thoracic artery (provides blood supply to the pericardium, main bronchi, trachea, diaphragm, sternum, anterior and superior mediastinum, pectoral muscles, rectus abdominis ) and the thyrocervical trunk (supplies blood to the thyroid gland, esophagus, pharynx and larynx, muscles of the scapula and neck).
The only branch of the second segment of the subclavian artery (costocervical trunk) supplies blood to the muscles of the neck, cervical and the beginning of the thoracic spine. The branch of the third segment (transverse cervical artery) mainly supplies blood to the back muscles.
Subclavian artery occlusion
Vertebrobasilar insufficiency
Clinically, vertebrobasilar insufficiency is manifested by one of the following symptoms or a combination of them: dizziness, headaches, instability when walking or standing, cochleovestibular syndrome, drop attacks, visual disturbances, etc. With pathology of the subclavian artery, vertebrobasilar insufficiency occurs, as a rule, with the development of steel syndrome: with proximal occlusion or critical stenosis of the subclavian artery before the vertebral artery departs from it, as a result of a decrease in blood pressure (BP) in the distal bed of the subclavian artery, blood flows from the contralateral vertebral artery artery along the ipsilateral vertebral artery into the subclavian artery distal to the site of stenosis, that is, to the detriment of the brain, blood flows from it to the arm (see figure). Many patients with steel syndrome (about 20%) do not have clinical manifestations of circulatory failure in the posterior cranial fossa or symptoms of ischemia of the upper limb. However, research in recent years has proven the unpredictability of this syndrome, the possibility of developing severe circulatory disorders of cerebral circulation with an increase in theft against the background of various physical and emotional stress, with fluctuations in blood pressure levels. Therefore, many authors consider the presence of steel syndrome to be an indication for surgical treatment even in the absence of clinical manifestations.
For the purpose of a more detailed study of the hemodynamic characteristics of steel syndrome, a compression cuff test (reactive hyperemia test) is used to determine the percentage increase in the average speed of retrograde blood flow through the vertebral artery and the time of stabilization of this blood flow speed to the background (initial) level when the cuff is removed. The critical values for these values are 20% or less for the speed increase and 8 seconds or more for the blood flow stabilization time. The presence of subcompensated or decompensated steel syndrome in a patient significantly increases the statistical risk of developing cerebral complications intraoperatively or in the immediate postoperative period.
Catheterization of the subclavian vein. Puncture
As mentioned above, in the neck the subclavian vein (and artery too) lie on the surface. It is this place that is used to take a puncture and insert a catheter. What is the rationale for choosing this particular part of the vessel? There are several criteria for this choice, these are:
- Anatomical accessibility.
- Position stability and lumen diameter.
- Sufficient or significant size (diameter).
- The speed of blood flow exceeds the speed of blood movement in the veins of the extremities.
Based on the data presented above, a catheter placed in a vein will almost not touch the walls of the artery. Medicines that are administered through it will quickly reach the right atrium and ventricle, they contribute to an active effect on hemodynamics. Medicines injected into the subclavian vein mix very quickly with the blood, without irritating the inside of the artery. In some cases, there are contraindications for punctures and catheter insertion.
Upper limb ischemia
The second most common symptom of damage to the subclavian artery is ischemia of the upper limb, in which four stages are distinguished:
I – stage of compensation. There is increased sensitivity to cold, chilliness, paresthesia, and a feeling of numbness.
II – stage of subcompensation. Symptoms of ischemia in the fingers, hands and forearm muscles during physical activity - pain, weakness, coldness, numbness, fatigue.
III – stage of decompensation. Symptoms of ischemia at rest with pain, constant numbness and coldness, muscle wasting, decreased muscle strength.
IV – stage of ulcerative-necrotic changes. Swelling, cyanosis, severe pain, impaired trophism, ulcers, necrosis and gangrene.
Stages III and IV of ischemia of the upper limb in chronic atherosclerotic occlusion of the subclavian artery occur quite rarely: stage III in no more than 6-8% of cases, stage IV occurs occasionally (usually with aortoarteritis). This is explained by the well-developed collateral circulation of the upper limb.
Symptoms of stenosis
Stenosis of the subclavian artery can manifest itself with the following symptoms:
- Feeling of weakness in the muscles;
- Regular feeling of fatigue;
- The occurrence of pain in the upper extremities;
- The occurrence of bleeding in the area of the nail plates;
- Necrosis of the fingers.
In addition, stenosis can manifest itself as symptoms that are neurological in nature, that is, the body redirects blood from normally functioning vessels to the pathological area, resulting in:
- Deterioration of vision;
- Speech dysfunction;
- Loss of balance;
- Fainting;
- Dizziness;
- Decreased facial sensitivity.
Coronary-mammary-subclavian steal syndrome
The use of the left intrathoracic artery for revascularization of the coronary arteries can aggravate myocardial ischemia in the case of hemodynamically significant stenosis/occlusion of the 1st segment of the subclavian artery. These patients may develop coronary-mammary-subclavian steal syndrome, which can lead to infarction.
Detection of damage to the subclavian artery before CABG surgery will help prevent the development of this pathology by revising surgical tactics (primary revascularization of the subclavian artery, use of other vascular grafts, etc.).
Data from a detailed physical examination of the patient in most cases allows one to suspect a hemodynamically significant lesion of the subclavian artery. The difference in blood pressure in the upper extremities is more than 20 mm Hg. indicates probable critical stenosis of the subclavian artery, and the blood pressure difference is more than 40 mm Hg. – about its occlusion. Palpation determines weakened pulsation (or its absence) of the radial artery on the affected side of the subclavian. When auscultating the subclavian artery, if it is damaged, a systolic murmur is heard in the supraclavicular region, which is observed in 60% of patients (in the absence of heart murmurs). Doppler ultrasound and duplex scanning are the leading screening methods for suspected occlusive-stenotic lesions of the main arteries of the head and neck. The sensitivity of ultrasound scanning for occlusions of the subclavian artery is 95%, and for its stenoses – 75%.
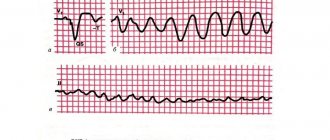
Occlusion of the first segment of the subclavian artery is characterized by:
- complete vertebral-subclavian steal syndrome;
- collateral blood flow in the distal portion of the subclavian artery;
- retrograde blood flow through the vertebral artery;
- positive test of reactive hyperemia.
Stenosis of the first segment of the subclavian artery is characterized by:
- transitional vertebral-subclavian steal syndrome - main-line altered blood flow in the distal section of the subclavian artery, systolic reversal of blood flow through the vertebral artery;
- blood flow through the vertebral artery is shifted below the isoline to approximately 1/3;
- during decompression, the blood flow curve through the vertebral artery “sits” to the isoline.
Depending on the severity of the stenotic process at the mouth of the subclavian artery, three types of subclavian steel syndrome are distinguished in the literature: latent (hidden) - stenosis of 50-60%; transient - stenosis 60-80%; permanent - occlusion or stenosis >90%. Each of them corresponds to a certain change in Dopplerograms, which, in combination with the reaction to the reactive hyperemia test - under the influence of which the transition from one stage of subclavian steal to another can be observed - makes it possible to accurately determine the degree of damage to the subclavian artery at the mouth. Digital subtraction arteriography
remains the “gold standard” for visualizing the lumen of the vascular bed. The vast majority of authors, despite advances in the development of non-invasive methods, consider angiography to be a mandatory and unconditional condition for a high-quality diagnosis and determination of treatment tactics.
Thus, if the subclavian artery is damaged, surgical treatment is indicated in the following cases:
- Subclavian artery stenosis ≥75% in patients with clinical vertebrobasilar insufficiency or symptoms of upper limb ischemia.
- Occlusion of the subclavian artery with clinical signs of vertebrobasilar insufficiency or symptoms of ischemia of the upper limb.
- Heterogeneous atherosclerotic plaques in the first segment of the subclavian artery with proven digital embolism.
- Proven subclavian-vertebral steal syndrome, regardless of clinical manifestations.
- Asymptomatic lesions of 1 segment of the subclavian artery (≥75%) in patients for whom mammary-coronary anastomosis is indicated (or has been applied) (to prevent the development of coronary-mammary-subclavian steal syndrome).
What causes
Stenosis in most cases develops against the background of thrombosis and atherosclerosis, leading to narrowing of the vascular lumen. According to doctors, the following factors can provoke this pathology:
- arteritis;
- exposure to radiation;
- muscle dysplasia;
- a vessel affected by atherosclerotic plaques;
- compression of the subclavian artery;
- diabetes;
- excess body weight;
- elevated blood pressure;
- the age category of the patient is over 60 years old;
- sedentary, sedentary lifestyle;
- hereditary predisposition;
- elevated blood cholesterol levels;
- hormonal imbalances;
- traumatic injuries to the supraclavicular region and the artery itself;
- increased blood clotting rates, tendency to thrombosis.
The disease can develop against the background of congenital pathologies that affect the structure of the vascular walls, infectious, inflammatory processes, and oncological tumors.
The narrowing of the vascular ostium in particularly complex, advanced clinical cases is more than 80%, which threatens artery obstruction, the development of concomitant ischemia, and stroke, so the disease must be treated in a timely manner.
Bilateral stenoses in practice occur in no more than 2% of patients.
Much more often in medicine, lesions of the left subclavian artery, responsible for the blood supply to the arms, neck and head, are recorded.
The right artery emerges from the region of the brachiocephalic trunk, supplying blood to the brachial and thoracic vertebral regions. Stenoses of the right subclavian artery are recorded by doctors much less often than the left.
The main cause of the disease is the development of atherosclerotic processes in the area of the affected artery, disruption of blood flow and circulation, leading to tissue hypoxia and the formation of necrotic foci of cellular structures in the artery.
Types of operations on the subclavian artery
Surgical treatment of subclavian artery pathology has a half-century history. In 1957, De Bakey performed a transaortic endarterectomy from the 1st segment of the left subclavian artery. Previously used methods of direct reconstructive operations for “aortic arch syndrome”, which involved performing sternotomy or thoracotomy, currently have no practical significance. In case of damage to the arteries of the vertebrobasilar region (VBB), “switching operations” were mainly performed using extrathoracic access, which allows avoiding prosthetics in most cases. Previously it was assumed that during “switching operations” “steal syndrome” could develop in the “donor artery” basin. However, flowmetric studies during reimplantation of the subclavian artery into the carotid showed that there was no decrease in blood flow through the donor artery. The only condition for the successful outcome of such operations is the complete intactness of the “donor arteries”, since stenosis of the bifurcation of the carotid artery during the operation of reimplantation of the subclavian artery into it causes a pronounced discharge of blood into the arterial system of the upper limb, 2-3 times higher than normal.
Many years of practice have not only confirmed the effectiveness and priority of angiosurgical care for damage to the subclavian artery, compared to conservative treatment, but also led to the fact that, among the variety of proposed operations, angiosurgeons have now settled on performing several standard operations for this pathology.
Today, for pathology of the 1st segment of the subclavian artery, the following operations are mainly used:
Reimplantation of the subclavian artery into the common carotid artery
This operation restores direct blood flow through the subclavian artery and does not require the use of shunt material. The hemodynamic effectiveness of the operation is not disputed: by eliminating the vertebral-subclavian steal syndrome and restoring direct blood flow through the subclavian artery, it compensates for the upcoming steal of the common carotid artery (no more than 10–15% of the carotid blood flow) and increases the total blood flow through the common carotid artery and vertebral artery approximately 1.5 times the original.
Carotid-subclavian shunt
This operation is performed when stenosis extends to the 2nd segment of the subclavian artery, as well as in patients with a hypersthenic physique, when isolating the 1st segment of the subclavian artery is associated with technical difficulties.
Subclavian-subclavian or carotid-subclavian cross-shunting operations
Subclavian-subclavian or carotid-subclavian cross-bypass operations are extremely rarely performed. These types of reconstruction are performed when the ipsilateral common carotid artery is damaged or when the brain has low tolerance to ischemia when the common carotid artery is clamped. However, with these reconstructive interventions, low long-term patency of the shunt is noted due to non-physiological blood flow through the shunt.
Characteristics of individual types of surgical interventions are presented in the table.
Advantages and disadvantages of replantation and bypass surgery of the subclavian artery
| Reimplantation of the subclavian artery into the common carotid artery | Carotid-subclavian shunt |
| Advantages | |
| Using only autologous tissue when forming a single anastomosis | Elimination of the risk of kinking of the vertebral artery in the variants of its origin from the subclavian when pulling the latter to the common carotid artery during reimplantation |
| Possibility of adequate endarterectomy (EAE) from the vertebral and II segment of the subclavian artery | Possibility of performing with the proximal origin of the vertebral artery |
| Performing only one anastomosis | Low risk of damage to the thoracic lymphatic duct and the dome of the parietal pleura |
| Minimal development of intimal hyperplasia | |
| Restoration of direct antegrade blood flow through the artery | |
| The most physiological blood flow in the reconstruction zone in terms of its characteristics | |
| Flaws | |
| There is a risk of kinking the vertebral artery in the variants of its origin from the subclavian when pulling the latter to the common carotid artery | Use of synthetic grafts |
| Impossibility of surgery for the proximal origin of the vertebral artery | Difficulty in performing adequate endarterectomy from the vertebral and II segment of the subclavian artery |
| Possibility of damage to the thoracic lymphatic duct and the dome of the parietal pleura | The need to form two anastomoses |
| Lengthening the operation time due to the need for careful mobilization of the subclavian artery in segments I and II | Retrograde nature of blood flow through the vertebral artery |
| The stump of the subclavian artery, located proximally, is potentially an area of thrombosis, which can also lead to thrombosis of the vertebral artery arising from it | |
| Theoretically, carotid stealing may occur | |
| There is a discrepancy between the elastic properties (compliance) of the arteries and the prosthesis, which can lead to intimal hyperplasia at the sites of anastomosis | |
| When using a prosthesis, its increased thrombogenicity is noted | |
Basic methods of treating pathology
The main method of treatment and providing adequate therapeutic influence is surgery. It can be implemented by performing one of three operations:
- plastic – consists of resection of a fragment of the subclavian artery with its subsequent implantation into the carotid artery, as well as prosthetics of the area;
- bypass – consists of creating an additional path for blood circulation to bypass the affected area;
- endovascular - consists of dilatation and stenting of the affected fragment by installing a structure inside the artery to restore blood flow.
This treatment is carried out both on the left subclavian artery and on the right lobe, as well as arterial branches. In addition, laser and ultrasound recanalization methods, which are used in the initial stages of pathology, have recently become widespread. These methods allow not only to preserve the patient’s health, but also to avoid surgery and its main complications.
Complications
- Considering the special sensitivity of the brain to ischemia and the complexity of the anatomical structure of the neck and chest, a number of specific complications occur during operations on the subclavian-vertebral segment.
- Stroke intraoperative or in the immediate postoperative period due to embolism, prolonged compression of the artery or acute thrombosis of the anastomosis.
- Damage to peripheral nerves (Horner's syndrome due to damage to the sympathetic trunk, plexitis due to damage to the brachial plexus, paresis of the dome of the diaphragm and impaired swallowing due to trauma to the phrenic and recurrent nerves).
- Reperfusion cerebral edema (the microvasculature, adapted to reduced blood flow, cannot immediately adapt to accept a large volume of blood).
- Other complications (bleeding, lymphorrhea, paresis of the diaphragm dome, pneumothorax, etc.).
Who's at risk
Medical specialists identify a group of people most at risk of developing subclavian artery stenosis. These include heavy smokers who abuse alcoholic beverages, as well as patients with the following health problems:
- arterial hypertension;
- vascular malformations;
- disturbances in the functioning of the cardiovascular system;
- aortic insufficiency;
- scoliosis affecting the cervical and thoracic spine;
- osteochondrosis;
- aortic aneurysm;
- pathological lesions of the pulmonary artery.
If there are risk factors, it is recommended to regularly undergo preventive examinations to monitor the condition of the cardiovascular system and in particular the subclavian aorta. Timely detection of pathology significantly increases the chances of successful treatment.
Angioplasty and stenting of the subclavian artery
The introduction of new medical technologies into clinical practice makes it possible to consider endovascular correction of the subclavian artery as an alternative to surgical treatment in patients with its damage.
Today, the following types of endovascular interventions on the subclavian artery are used:
- angioplasty of the subclavian artery. It is indicated for small stenoses (60-80%), with a plaque of a homogeneous structure, and with a relatively large diameter of the artery. The isolated angioplasty procedure is used in no more than 5% of cases, which is associated with limited indications for its implementation and a fairly high incidence of restenosis.
- stenting of the subclavian artery (isolated or with angioplasty).
- recanalization (ultrasound or laser) followed by angioplasty and stenting. It is used for occlusion of the subclavian artery, when the occlusion zone cannot be passed by a soft conductor.
Compared to surgical operations, they have certain advantages. These interventions are less traumatic for the patient, short-term compared to surgery, performed under local anesthesia (which makes it possible to perform them in patients with severe concomitant pathology), are accompanied by fewer complications, and reduce the number of bed days.
If the result of surgical intervention is unsatisfactory (thrombosis, restenosis), repeated operations are difficult due to the anatomical features of the reconstruction area. Repeated endovascular intervention is associated with fewer difficulties.
The development of endovascular technologies has led to their widespread use and their proposal as starting (primary) methods for treating atherosclerotic lesions of the subclavian artery. At the same time, there are no randomized studies comparing stenting and various surgical techniques, and the long-term results of endovascular treatment have not been sufficiently studied - all published studies are a description of the clinic’s experience.
Causes and risk factors
The reasons for the development of atherosclerosis of the subclavian artery are the same as for other atherosclerotic plaques. Most often these are high cholesterol, diabetes, obesity, and smoking. Lesions most often occur in the initial section (proximally) of the subclavian artery, but can also occur in other segments.
Damage to the subclavian artery may be associated with compression between the first rib and the clavicle (compression syndrome at the thoracic outlet). Proximal lesions of the subclavian artery can be insidious and are detected by measuring blood pressure on different arms or pulsations. However, complications related to blood circulation in the arm or brain often develop.
Surgical tactics for combined lesions
In case of combined lesions of the carotid system and the subclavian artery, the priority of reconstruction of the carotid arteries is beyond doubt. This is due to a higher risk of developing acute cerebrovascular accidents (ACVA) in the carotid area with damage to the carotid arteries than in the vertebrobasilar area with damage to the subclavian artery. In addition, during replantation or bypass operations, the common carotid artery is the donor artery, and the operation is accompanied by its compression, which, if the second carotid artery is damaged, can lead to stroke in the carotid area. The embologenic nature of the plaque in the carotid bifurcation increases the risk of developing stroke in the carotid region during reconstruction of the subclavian artery.
In case of contralateral damage to the carotid arteries and subclavian artery, the first stage is carotid endarterectomy, reconstruction of the subclavian artery is performed no earlier than 2-3 weeks later. In case of ipsilateral damage to the carotid arteries and subclavian artery, it is possible to perform both staged and one-stage operations: carotid endarterectomy and implantation of the subclavian artery into the common carotid artery. In case of hemodynamically significant lesions of both carotid arteries and damage to the subclavian artery, the first stage is to restore blood flow in the carotid artery with a more significant lesion. The second stage involves surgical intervention on the second carotid artery.
In case of bilateral damage to the subclavian artery, the first stage is reconstruction of the artery on the side of the steel syndrome, and in its absence, reconstruction of the artery with more pronounced stenosis.
In case of ipsilateral damage to the vertebral artery and subclavian artery, simultaneous reconstruction of these arteries is indicated.
In case of contralateral damage to the vertebral artery and subclavian artery, the first stage is reconstruction of the subclavian artery (to eliminate style syndrome). Reconstruction of the affected vertebral artery is carried out only in the absence of regression of the clinic of vertebrobasilar insufficiency.
The question remains unresolved about the surgeon's tactics in cases of damage to the left subclavian artery and anterior interventricular branch (LAD) in patients for whom myocardial revascularization is indicated or has been performed. Several approaches have been proposed to solve this problem:
- use of other grafts for LAD revascularization.
- surgical correction of damage to the subclavian artery. The question of surgical tactics remains unresolved: is a staged or one-stage operation indicated for these patients, the timing of staged interventions, the possibility of performing operations in patients who have undergone MCS, etc.
- Angioplasty and stenting of the subclavian artery are a good method for the prevention and treatment of coronary-mammary-subclavian steal syndrome. Unfortunately, there is a relatively high percentage of the development of restenosis (13-16%), and there are no results on studying long-term patency. The question of disaggregant therapy after stenting of the subclavian artery remains open: Plavix, which is indicated for patients after stenting, increases the volume of blood loss and the risk of bleeding after coronary artery bypass surgery.
The algorithm for managing a patient with isolated or combined lesions of the subclavian artery is presented in the figure.
Possible risks of stenting
The subclavian artery stenting procedure lasts approximately 2 hours. This operation is performed in the cardiac catheterization department. After stenting, painkillers are taken if necessary, as pain may occur in the area where the subclavian artery and tissue were cut. Complications after this procedure are very rare, since the patient undergoes careful preparation and observation before it. But still, some unpleasant consequences may arise, these are:
- Allergy to medications taken.
- Reaction to anesthetics.
- Minor bleeding at the incision site.
- Temperature.
- Headache.
- Infection.
- Air embolism.
- Damage to the wall of the artery or aorta.
- Thrombosis of the subclavian artery.
- Stent migration.
- Neurological complications, etc.
How is surgery performed?
Stenting of the heart vessels allows you to expand the coronary arteries, which cannot function normally due to the presence of a blood clot, and normalize the impaired blood flow. The essence of the operation is to insert a stent into the artery, which is a special prosthesis for the wall of the affected vessel.
Essentially, it is a tube with walls in the form of a fine mesh. The stent is placed at the site of narrowing of the artery. Initially it has a folded appearance. At the site of arterial damage, the stent is inflated and fixed, thus maintaining the vessel in normal condition.
Although such an operation is a minimally invasive intervention, the walls of the vessel are still in an inflamed state. To speed up the healing of the vessel, improve the results of the operation and consolidate them, it is necessary to undergo a special rehabilitation program.
Stenting of coronary vessels is not a particularly complex or lengthy operation. But it still requires special preparation and is carried out according to a clear plan.
Stent in an artery
Although coronary stenting does not require complex preparation, some procedures will still have to be done. In this case, preoperative preparation is as follows:
- general blood test and coagulogram, which determines the ability of blood to clot;
- blood chemistry;
- ECG;
- X-rays of light.
If the situation is not critical, but the operation is planned, then the person undergoes a comprehensive examination. Surgery is often performed in emergency cases when every minute counts. For example, in the case of a heart attack, after the onset of which more than 5 hours have passed, the operation begins without test results.
Operation procedure
The operation of stenting heart vessels is performed in operating rooms, under conditions of absolute sterility. Surgeons must also have at their disposal precise, modern equipment that will ensure constant monitoring of the patient’s condition and allow them to monitor the progress of the operation.
- Local anesthesia by administering, for example, Novocaine. Anesthesia is performed on the inguinal-femoral area of one leg.
- A catheter-manipulator is inserted into the femoral artery through a previously made puncture puncture.
- As the catheter moves through the vessel, an iodine-containing drug is administered. It is clearly visible on x-ray. As a result, the vessels are clearly visible, and the surgeon can control the process of catheter movement.
- When the catheter approaches the site of arterial damage, a stent is placed. To do this, the balloon, which is located at the end of the catheter, is inflated by introducing air. This expands both the stent and the artery to the required size.
Diagnostic methods
To make an accurate diagnosis and identify the stage of the pathological process, the degree of narrowing of the vascular lumen, if arterial stenosis is suspected, a comprehensive medical examination is required. Patients with such a preliminary diagnosis are prescribed the following types of studies:
- CT scan;
- Magnetic resonance imaging;
- ultrasonography;
- angiography and extensive arteriography (x-ray examination of blood vessels);
- X-ray examination;
- Dopplerography or Doppler ultrasound (examination using ultrasound);
- infrared thermography (electromagnetic examination);
- rheovasography (safe passage of electric current).
After preliminary diagnosis, based on the results obtained and the characteristics of a particular clinical case, the doctor develops an individual treatment course for the patient.
Preparing for surgery
The operation of stenting the carotid arteries is carried out according to strict indications. The need for surgical intervention is determined by the vascular surgeon in each specific case. The specialist asks the patient about the medications he is taking;
if you are allergic to contrast agents, metals or plastics. The patient is prohibited from eating and drinking the evening before stenting. 5-7 days before the operation he is prescribed to take drugs from the group of antiplatelet agents.
A preoperative comprehensive examination of the patient is aimed at determining the location of the narrowing. Carotid angiography is the most common diagnostic technique used to detect stenosis or blockage of the carotid artery.
A catheter is inserted into the femoral or radial artery under local anesthesia and directed through the aorta to the carotid artery under x-ray guidance. After the contrast agent penetrates the body, a series of photographs are taken at certain intervals.
Angiographic data allow us to make a final conclusion about the degree of stenosis of the carotid arteries. Ultrasound, MRI and CT scans with contrast also provide images of the affected area of the blood vessel.
After local anesthesia, administration of Heparin and sedatives, the patient is connected to equipment that measures heart rate and blood pressure. A Doppler ultrasound study performed during the procedure provides control over the linear velocity of blood flow and the passage of microemboli through the vascular bed.
During the operation, the vascular surgeon communicates with the patient, thus monitoring the functioning of the brain. The patient feels sleepy and relaxed, but is conscious, follows the doctor's instructions and describes his sensations.
Patients deemed suitable for stenting undergo consultation with an interventional neuroradiologist. They explain the procedure and possible risks in detail. The necessary diagnostics are carried out. To prevent blood clots, the patient is prescribed clopidrogel three days before the procedure. A few hours before the procedure, you should not eat or take any medications.
Types of stents
It is impossible to give an exact answer to this question. The prognosis of life expectancy after stenting depends not so much on the operation itself, but on the disease for which it was performed and on the degree of damage to the heart muscle (that is, on the contractile function of the left ventricle).
- conservative therapy – mortality 13%;
- fibrinolytic therapy – mortality 6–7%;
- stenting – mortality 3–5%.
The prognosis for each individual patient depends on his age, the presence of other diseases (diabetes mellitus), and the degree of myocardial damage. There are various scales to determine it, of which the TIMI scale is the most widely used.
Stenting for stable coronary heart disease does not reduce the risk of future myocardial infarction, nor does it increase the life expectancy of these patients, compared with conservative drug therapy.
- Group 3 disability is assigned to patients with angina pectoris or a history of myocardial infarction without the development of severe impairment of left ventricular function.
- Group 2 disability is established for patients with angina pectoris or a history of myocardial infarction, in whom heart failure limits the ability to work and move.
- Group 1 disability is assigned to patients in whom myocardial infarction or angina pectoris has led to severe heart failure, limiting the ability to self-care.
Recovery after cardiac stenting depends on many factors, including the reason for the procedure, the severity of the patient's condition, the degree of deterioration in cardiac function, and the site of vascular access.
- The next day after the procedure, you can remove the bandage from the artery puncture site. The easiest way to do this is in the shower, where you can wet it if necessary.
- After removing the bandage, apply a small patch to the area. For a few days, the catheter site may be black or blue, slightly swollen, and slightly painful.
- Wash the catheter site at least once a day with soap and water. To do this, put soapy water in your palm or soak a washcloth in it and gently rinse the desired area. Do not rub the skin at the puncture site too much.
- When not showering, keep the vascular access area dry and clean.
- Do not apply any creams, lotions or ointments to the skin at the puncture site.
- Wear loose clothing and underwear if vascular access was via the femoral artery.
- For one week, do not take a bath, do not visit the bathhouse, sauna or swimming pool.
Doctors make recommendations for restoring physical activity, taking into account the location of the arterial puncture and other factors related to the patient's health. In the first two days after stenting, it is recommended to get plenty of rest.
Recommendations after femoral artery puncture:
- You should not strain during bowel movements for the first 3–4 days after stenting to prevent bleeding from the puncture site.
- During the first week after stenting, it is prohibited to lift more than 5 kg, as well as move or pull heavy objects.
- For 5-7 days after the procedure, you should not perform strenuous physical exercise, including most sports - running, tennis, bowling.
- You can climb the stairs, but slower than usual.
- During the first week after surgery, gradually increase your physical activity until it reaches normal levels.
- During the first 24 hours, do not lift more than 1 kg with the hand through which the stenting was performed.
- For 2 days after the procedure, you should not perform strenuous physical exercise, including most sports - running, tennis, bowling.
- Do not use a lawnmower, chainsaw, or motorcycle for 48 hours.
- For 2 days after surgery, gradually increase your physical activity until it reaches normal levels.
After planned stenting, you can return to work in about a week, if your general health allows. If the operation was performed for urgent reasons for myocardial infarction, full recovery may take several weeks, so you can return to work no earlier than after 2-3 months.
If before stenting a person’s sexual activity was limited by chest pain caused by insufficient oxygen supply to the myocardium, after stenting the possibility of having sex may increase.
- Clopidogrel.
- Prasugrel.
- Ticagrelor.
It is very important to follow all doctor's recommendations for taking these medications. Stopping them early may significantly increase the risk of myocardial infarction caused by stent thrombosis.
The duration of treatment with clopidogrel, prasugrel or ticagrelor depends on the type of stent implanted, approximately one year. Most patients need to take low-dose aspirin for the rest of their lives.
There are about a hundred types of stents in the world. Only an experienced cardiac surgeon can choose from this assortment a single specimen that will exactly suit a specific case. In any case, it must be of very high quality and reliable, because the stent is installed for a long time and performs an important function. Modern stents have a number of characteristics and distinctive properties:
- The outer coating uses a special substance that prevents blood from clotting. Thus, the formation of blood clots is prevented.
- Stents are available in various designs. This can be a ring element, a tube or mesh option. There are many options, and it will not be difficult for the surgeon to select the necessary stent.
- Stents also vary in diameter. This figure varies between 2 – 6 mm. The length is usually one centimeter.
- Stents may differ in composition. In any case, all manufacturers use special alloys, and production is based on high technology. The most commonly used alloy is cobalt and chromium, but other options are possible.
- New models of stents are coated with drugs, the effect of which is aimed at reducing the likelihood of developing re-stenosis and preventing myocardial infarction. Such designs are primarily necessary for people with kidney problems and diabetes.
Installation of a stent on the arteries of the heart has a number of indications. In each individual case, the doctor assesses the need for such an operation and prescribes it only when other methods of treatment without surgery are unsuccessful. The main indications for stenting are outlined below:
- ischemic disease in a chronic form, which is accompanied by the development of atherosclerotic plaques that block the arterial lumen by more than half;
- angina attacks that occur with light exertion;
- the likelihood of developing myocardial infarction in combination with coronary syndrome;
- myocardial infarction (extensive or small) in the first 6 hours with a stable body condition;
- re-closure of the arterial lumen after balloon angioplasty, bypass surgery and stenting.
After stenting of cardiac vessels, a rehabilitation period is required. It is important to follow all the rules. In this case, you can reduce the likelihood of complications that may occur after stenting of the heart vessels.
It is difficult to say how long they live after stenting surgery. A lot depends on a person’s compliance with the principles of rehabilitation. Does he want to change his life, take care of his heart and blood vessels, eat right, not be nervous and normalize his workload? This is exactly what we will talk about now.
Strict diet
Every person must adhere to a special diet after stenting the heart vessels. This way you can reduce the likelihood of blood clots and other complications. The essence of the diet is as follows:
- exclusion from the diet of fatty animal products;
- refusal of easily digestible carbohydrates and foods that are a source of cholesterol;
- reducing the daily salt intake;
- inclusion of vegetables, cereals, dietary meat and fish in the diet.
Physical activity after cardiac stenting is contraindicated during the first week after surgery. Only walking on level ground is allowed. Then physical activity is added gradually.
It is advisable to engage in physical therapy and perform a set of special exercises. Every person should not only know how to behave after stenting the heart vessels, but also strictly adhere to these rules.
How to treat
For stenosis of the subclavian artery, treatment is carried out exclusively by surgery. There are the following types of operations aimed at combating this vascular pathology:
- Plastic surgery - during a surgical procedure, a specialist removes atherosclerotic plaques from the area of the affected vessel, implants the subclavian artery in the carotid area, removes the damaged area, replacing it with a high-quality implant.
- Bypass surgery involves the creation of additional blood circulation pathways. Depending on the characteristics of a particular case, bypass surgery can be cross-subclavian, carotid-subclavian, or aorto-subclavian in nature. This technique allows you to restore the processes of blood circulation and blood supply, bypassing the affected area.
- Stenting is a minimally invasive and relatively safe surgical method. During the procedure, the narrowed vascular lumen is expanded by introducing a special catheter under high pressure. At the next stage, laser or ultrasound vascular recanalization is performed.
Surgical treatment for stenosis of the subclavian artery is considered the most effective method to prevent possible relapses. In the early stages of pathology, modern surgeons give preference to minimally invasive techniques, which are characterized by minimal trauma, safety and an accelerated recovery period.