Features of the disease
Ventricular fibrillation (VF) is characterized by chaotic contractions of myocardial tissue . Their frequency increases from 250 to 480 per minute. The movements of the ventricles cease to be coordinated. As a result, blood circulation stops and the heart stops.
Fibrillation is the leading cause of sudden death from heart problems.
The ECG produces irregular and chaotic waves that vary in width, height and shape. At the beginning of the attack they are high-amplitude. This is the so-called large-wave fibrillation. Afterwards, the waves become low-amplitude and their duration increases. At this stage, the effectiveness of defibrillation decreases .
Often this condition occurs as a complication of extensive myocardial infarction.
What is ventricular fibrillation
Normal contraction of the heart muscle is ensured by bioelectric impulses. They are generated by the atrioventricular and sinus nodes. The impulses affect the myocardium, cardiomyocytes of the atria and ventricles, provoking the heart to push blood into the vessels. When the conduction of impulses is disrupted, arrhythmia occurs. Ventricular fibrillation is a condition in which chaotic movement of myocardial muscle fibers occurs. They begin to work inefficiently, with a frequency of 300–500 beats per minute. For this reason, urgent resuscitation of the patient is necessary.
The result of fibrillation is a rapid decrease in the number of heart contractions. The volume of ejected blood decreases along with blood pressure, which leads to complete cardiac arrest. If it is not started with the help of special resuscitation measures, the patient will live no more than 3–5 minutes. The arrhythmia cannot stop on its own, so artificial defibrillation is required.
Prevalence, stages of development
About 75-80% of sudden deaths that are caused by cardiac problems occur due to VF. This disease occurs in both young and old people.
The risk group includes those patients who have suffered sudden circulatory arrest . Unexpected death affects 10-30% of such patients.
The chance of experiencing VF in people who suffer from idiopathic dilated cardiomyopathy is 10%. Within 1 year after a major heart attack, the disease affects 5% of patients. For hypertrophic cardiomyopathy – 3%.
Fibrillation is characterized by random contraction of the muscle fibers of the heart. The stages of development of the disease quickly replace each other : the patient feels weak, loses consciousness, and his pupils dilate.
About 2 minutes pass from the onset of the attack to clinical death.
Classification of species
Experts distinguish 3 types of VF after heart attacks: primary, secondary and late . Although discussions regarding the classification of this disease are still ongoing.
Primary fibrillation occurs 1-2 days after a heart attack . It shows that the myocardium is characterized by electrical instability, which resulted from acute ischemia.
About 60% of primary VF occurs within 4 hours, 80% - 12 hours after a heart attack. Such fibrillation often leads to sudden death. With left ventricular failure and cardiogenic shock, secondary VF sometimes develops in people who have suffered a myocardial infarction.
If fibrillation began 48 hours after a heart attack, then it is called late . About 40-60% of people who experience this disease die. In most cases, such fibrillation begins 2-6 weeks after a heart attack. More often it developed in those people whose anterior wall of the heart was damaged.
Doctors distinguish between 2 types of fibrillation. If the rhythm of contractions is correct, and their number does not exceed 200-300 per minute, then we are talking about ventricular flutter. With abnormal rhythm and contraction frequency from 200 to 500 per minute. talking about flickering.
Causes of development and risk factors
In most cases, the cause of primary and other types of gastric fibrillation is a complication of myocardial infarction. Experts identify the following reasons for the development of VF:
- IHD of the heart (acute and post-infarction, coronary circulatory disorders);
- hypertrophic cardiomyopathy: death occurs in young people with excessive physical exertion;
- dilated idiopathic cardiomyopathy: fibrillation begins against the background of hemodynamic disorders in half of these patients;
- problems with the right ventricle (arrhythmogenic cardiomyopathy);
- different types of heart defects (the most common cause is aortic stenosis);
- specific cardiomyopathies;
- violation of the electrophysical characteristics of the myocardium.
The disease sometimes develops even in the absence of problems with the heart muscle . Risk factors that in some cases lead to ventricular fibrillation include:
- a sharp decrease in blood volume (this causes a drop in pressure and an increase in heart rate);
- severe poisoning (hypokalemia develops and cardiac excitability increases);
- hypothermia of the body;
- hormonal imbalance that arose due to pathologies of the thyroid gland;
- chronic stress or excessive nervous tension;
- overdose of drugs: diuretics or cardiac glycosides.
There are cases when the cause of ventricular fibrillation cannot be determined.
Causes of pathology
Fibrillation and ventricular flutter occur due to the pathology of impulse transmission through the myocardium. These rhythm disturbances are successive stages of the development of one process. In ICD-10 (International Classification of Diseases, 10th revision) they are classified under one heading.
Dysfunction of the cardiac pathways can occur as a result of:
- large scar (consequence of myocardial infarction);
- focal post-infarction cardiosclerosis;
- coronary heart disease;
- acute myocardial infarction;
- cardiomyopathy with severe hypertrophy of cardiomyocytes;
- dilatation (stretching of the walls) of the heart chambers;
- arrhythmogenic cardiomyopathy;
- myocarditis (inflammation of the heart muscle);
- valve defects;
- severe intoxication (including alcoholism).
Symptoms and signs
You can suspect VF in a person based on characteristic signs:
- in 5 sec . the person becomes dizzy and weak;
- in 20 sec . the patient loses consciousness;
- after 40 sec . from the onset of the attack, the patient experiences characteristic convulsions: the skeletal muscles begin to contract once tonically, and at the same time defecation and urination occur involuntarily;
- in 45 sec . from the onset of ventricular fibrillation, the pupils dilate and reach their maximum size after 1.5 minutes.
The breathing of patients with ventricular fibrillation is noisy, frequent, and accompanied by wheezing.
By the end of the second minute it becomes less frequent and clinical death occurs. The patient sometimes has time to complain about:
- strong heartbeat;
- dizziness and weakness;
- heartache.
External signs include:
- pallor of the skin and mucous membranes;
- rapid breathing, shortness of breath;
- loss of consciousness;
- absence of pulsation in large arteries.
Doctors have 4 minutes to restore heart rhythm . If this cannot be done, then irreversible changes begin in the body.
Find out more about the disease from the video:
Complications
It is vital that a person with ventricular fibrillation receives immediate care followed by treatment in a cardiac hospital. If this does not happen, an unfavorable outcome may occur within 30 minutes to 1 hour.
Complications of ventricular fibrillation include coma and impairment of neurological functions (intelligence, speech, memory, and others). They arise due to the death of brain cells during oxygen starvation, which occurs from the onset of an arrhythmia attack.
As a result of a serious condition and coma, the following may occur:
- aspiration pneumonia, caused by particles from the stomach entering the lungs;
- “stunning” of the myocardium, accompanied by a constant decrease in cardiac contractility;
- convulsive attacks.
With indirect cardiac massage, fractures of the sternum and ribs often occur. The doctor who assisted the patient should not be blamed for this. It is sometimes believed that such fractures are an indicator of effective resuscitation efforts.
Diagnostics and emergency care
Experts determine ventricular fibrillation by external signs . If the doctor is near the patient during the onset of the attack, he will diagnose:
- increased heart rate;
- lack of rhythm;
- difference between heart rate and pulse;
- no difference between I and II heart sounds;
- wheezing in the lungs.
Competent resuscitation measures can save a person.
If the attack occurred outside the hospital, you must call an ambulance. A person’s complaints, sudden fainting and characteristic convulsions can be used to suspect VF. Before doctors arrive, it is recommended to do the following:
- Make sure that a state of clinical death has occurred.
- It is necessary to “start” the heart : in the absence of a defibrillator, a sharp blow is given to the sternum.
- In cases where the heartbeat is not restored, artificial respiration and cardiac massage . If resuscitation is carried out by 1 person, then for 2 insufflations he makes 15 rhythmic pressures on the sternum.
More details about resuscitation measures are described in the video:
An ECG is done in a hospital setting or in ambulances . This examination allows for differential diagnosis and establishment of an accurate diagnosis.
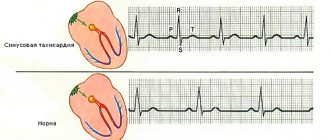
With ventricular fibrillation and flutter, the ECG will show the following signs:
- P waves are in most cases absent before ventricular contractions;
- chaotic frequent waves instead of the necessary QRS complexes;
- with flutter the waves will be rhythmic, with ventricular fibrillation they will not.
Diagnostic methods
Ventricular fibrillation can be diagnosed only during instrumental examination methods. The key method is electrocardiographic examination of the heart. The advantages of recording an electrocardiogram are the speed of the examination and the ability to carry it out anywhere.
Signs of development of ventricular fibrillation on the ECG:
- Absence of QRS complexes and any intervals and waves;
- Registration of fibrillation waves with a frequency of 300-400 per minute, chaotic, variable in length and amplitude;
- Absence of isoelectric line.
An electrocardiogram can record large-wave VF - if the contraction force is more than half a centimeter based on the length of one cell. This type is typical in the first minutes of the disease.
For reference. Gradually, the heart cells are depleted, the acid-base balance shifts to the acidic side, metabolic changes increase - small-wave fibrillation is recorded. This condition poses the greatest danger to the patient and is characterized by the most unfavorable prognosis.
Treatment tactics
In the hospital, all actions are aimed at restoring the heart rhythm . These measures are called cardioversion. Doctors perform chest compressions and artificial ventilation. Insufflation of air allows you to provide the body with oxygen.
Electropulse therapy gives good results . The sooner it is carried out, the higher the patient’s chances of survival.
Some argue that after 3 ineffective defibrillator shocks, the patient should be intubated and put on artificial respiration.
VF is continued to be treated with sodium bicarbonate. Injections are given every 10 minutes until blood circulation is restored.
They increase the effectiveness of electrical pulse therapy by intracardiac administration of the drug "Adrenaline hydrochloride" . But such injections are fraught with complications.
For drug stimulation of the myocardium, “Norepinephrine” and “Mezaton” are used.
If defibrillation is ineffective, then in addition to Adrenaline hydrochloride, Anaprilin, Novocainamide, and Lidocaine . The patient continues to undergo cardiac massage and artificial respiration, defibrillation is repeated after 2 minutes.
In cases where the heart stops after electrical pulse therapy, the drugs “Calcium chloride” and “Sodium lactate” .
Resuscitation measures are carried out until the heart rhythm is restored or signs appear that the brain has begun to die.
Drug treatment of ventricular fibrillation
As stated, there are no other treatments for ventricular fibrillation other than electrical impulse therapy. Also, in such cases, treatment of ventricular fibrillation with folk remedies does not help. Everything is connected with the fact that this is a borderline state between life and death, therefore pharmacotherapy is used only in the form of VF prevention. Also, after the rhythm is restored, medications are prescribed to maintain it.
Thrombolytic therapy is important in the post-resuscitation period. The introduction of heparin and new anticoagulants can reduce the likelihood of developing VF, as well as blockage of blood vessels formed during cardiac dysfunction.
Commonly used medications and drugs to treat ventricular fibrillation:
- Sodium bicarbonate is often used after the tenth minute of resuscitation.
- Magnesium sulfate - indicated for prolonged, stable or recurrent fibrillation.
- Potassium chloride - prescribed in the presence of initial microelement deficiency.
- Ornid - can be administered several times during the treatment of VF.
- Atropine is necessary in case of previous VF asystole or bradycardia.
- Anaprilin is a beta blocker used for pre-existing VF rhythm disturbances in the form of tachycardia.
- Calcium preparations are used according to strict indications (excess potassium, lack of calcium, excessive intake of calcium antagonists).
During the treatment of ventricular fibrillation, early defibrillation is of greatest importance. Other methods of therapy fade into the background. In patients at high risk of developing a critical condition, implantation of a cardioverter-defibrillator is recommended.
Rehabilitation
After ventricular fibrillation, the patient is monitored.
His condition is constantly monitored using a Holter ECG: this is done continuously for 1-7 days .
Treatment is aimed at preventing recurrence of attacks.
If patients experience fibrillation due to heart disease, then surgery . Surgeons can install a device that will correct the myocardial rhythm.
The radiofrequency ablation method is also used - this is the introduction of a special device that destroys the pathological focus of abnormal heart rhythm.
Drug antiarrhythmic therapy is also carried out . To prevent possible complications, anticoagulants are prescribed. They prevent increased blood clotting and reduce the likelihood of developing a heart attack. They also recommend products that improve metabolism and nourish muscles.
Possible consequences and prognosis
In most cases, complications occur after VF. The prognosis will be better in cases where assistance is provided in the first seconds of an attack. But it is difficult to avoid the negative consequences of this condition.
When the heart stops, total myocardial ischemia . After blood circulation is restored, dysfunction of the heart muscle appears.
The following complications may also develop:
- the appearance of arrhythmia;
- lung problems: aspiration pneumonia, tissue damage due to rib fractures;
- neurological problems (arise due to a temporary deterioration in blood circulation in the brain tissue);
- thromboembolism: blockage of blood vessels by blood clots.
When carrying out defibrillation in the first 6 minutes and other resuscitation measures in the first 3 minutes, the probability of survival is 70%. If more than 12 minutes have passed since the onset of the attack, then less than 20% of patients remain alive.
Preventive methods, preventing relapses
Monitoring the work of the heart muscle can reduce the likelihood of developing VF. If the slightest deviation appears, you must consult with doctors and follow their instructions.
Doctors recommend reconsidering your lifestyle. Need to:
- give up cigarettes, alcohol, drugs;
- focus on plant foods and dairy products;
- exclude smoked, fried, fatty foods from the diet;
- reduce salt intake;
- Lead an active lifestyle, but avoid overload.
After VF, it is advised to follow all medical recommendations and take prescribed medications.
It is difficult to provide competent, timely medical care for ventricular fibrillation. After all, an attack does not always begin in the hospital. Because of this, this disease is considered the leading cause of sudden death due to heart problems . You can reduce the likelihood of its development if you monitor the condition and adhere to the basics of a healthy lifestyle.