Extrasystoles
Extrasystole is premature excitation of the entire heart or any part of the heart in relation to the main rhythm.
Depending on the site of origin, ES is divided into supraventricular (occurs above the bifurcation of the His bundle) and ventricular (occurs below the bifurcation of the His bundle).
If there is extrasystole, I definitely evaluate:
1- coupling interval - the distance from the sinus complex preceding the extrasystole to the ecstasitole
2- compensatory pause - the distance between the extrasystole and the sinus complex following it
Supraventricular extrasystoles usually have a narrow QRS and an incomplete compensatory pause (the sum of the pre-extrasytolic and post-extrasystolic intervals is not equal to 2 RR). SVEs can be rare (up to 5 per minute), moderate in frequency (from 6 to 15 per minute) and frequent (more than 15 per minute). In addition, they can be single or paired, as well as sporadic or regular. An obvious regularity in the appearance of SVE is also possible: bigeminy (SVE after each main complex) or trigeminy (SVE after every two main complexes). All this data must be indicated in the diagnosis, since these types of NJES have different clinical significance.
In healthy people, when monitoring ECG, SVE is found in 43-63% of cases. In this case, SVE is most often rare (less than 30 per hour) and occurs during a decrease in sinus rhythm.
In various diseases of the cardiovascular system, SVE is more often of medium frequency and frequent; it can appear against the background of sinus tachycardia; allometry is characteristic. Sporadic SVE is possible, appearing during attacks of angina pectoris and hypertensive crises.
The clinical significance of SVE is that it provokes more severe NRS: atrial fibrillation and flutter, supraventricular reentrant tachycardia, etc. In addition, SVE is often subjectively poorly tolerated by patients.
Examples of diagnoses for SVE:
Stage II hypertension, stage 2 hypertension, risk 3. Frequent regular supraventricular extrasystole. CHF I-1 f.k.
Treatment of patients with SVE:
Patients with VES, which are subjectively difficult to tolerate by patients, or VES, provoking paroxysms of tachycardia, are subject to specific therapy. The most commonly used are beta blockers and calcium antagonists (verapamil and diltiazem group). However, if it is proven that SVE causes paroxysms of one or another tachycardia, then an antiarrhythmic drug (AAP) selected to prevent attacks of tachycardia is used for treatment.
With ventricular extrasystole , the QRS complexes are widened and deformed, and there is a complete compensatory pause (the sum of the pre-extrasystolic and post-extrasystolic intervals is equal to 2 RR).
Right ventricular ES have the form of left bundle branch block, left ventricular ES have the form of right bundle branch block.
For prognostic assessment, the PVC grading system developed by V. Lown and M. Wolf (1971) is used.
Gradations of PVCs according to V. Lown (1971):
0- no PVCs 1- 30 or less PVCs per hour 2- more than 30 PVCs per hour 3- polymorphic PVCs 4(A)- paired PVCs 4(B)- three or more PVCs in a row 5- PVCs of type R on T.
If a PVC is registered in a practically healthy (especially young) person and does not cause serious unpleasant subjective sensations, then there are no absolute indications for antiarrhythmic therapy (AAT) in such a patient. If PVCs are frequent and poorly tolerated, then certain treatment may be possible.
If the patient has a tendency towards sympathicotonia. PVCs occur during the daytime, during stress, and during physical activity, he is recommended to be treated with beta-blockers in combination with mild sedative therapy. It is advisable to limit coffee, tea, alcoholic drinks, and smoking. It is possible to consult a psychotherapist and provide adequate treatment for depressive and anxiety states.
If the patient has a tendency to parasympathicotonia. PVCs occur at night, at rest, against the background of bradycardia, and reflexively in diseases of the gastrointestinal tract. Such patients are recommended to receive adequate treatment for gastrointestinal diseases, possibly using sedatives, tranquilizers (Grandaxin), and drugs that slightly increase heart rate.
In organic diseases of the CVS, the clinical significance of PVCs is determined by their ability to provoke attacks of VT and ventricular fibrillation.
The risk of sudden death (SD) in this group of patients is highly variable and very difficult to estimate. It can be assessed according to 3 main risk factors: MI, EF less than 40%, PV (more than 10 per hour). In the presence of 1 risk factor (MI or EF less than 40%), the risk of VS per year is 5%, when combining each of these risk factors with PVCs the risk of VS is 10%, with a combination of 3 risk factors - 15%.
When treating patients with PVCs, a number of rules must be followed:
The most important direction in the management of such patients is active therapy of the underlying heart disease. Do not prescribe VS to patients with RF for continuous use of class I AAP. In patients with a history of MI, EF less than 40% and PVCs IV in the gradation, endocardial EPS is indicated. If VT is provoked during EPS, implantation of a cardioverter-defibrillator (CV-DF) is indicated in a patient resistant to AAP. If EPS does not provoke AAP-resistant VT, prophylactic therapy with amiodarone is possible.
Causes
Supraventricular extrasystole can be idiopathic, that is, it occurs without any apparent reason. It can be observed in practically healthy people at any age. In addition, there are different reasons for the development of supraventricular extrasystole:
Heart diseases: heart failure; cardiac ischemia; myocardial infarction; heart defects, both congenital and acquired; myocarditis (inflammatory processes in the heart muscle); cardiomyopathy. Endocrine diseases: diabetes mellitus; hyperthyroidism, or thyrotoxicosis; adrenal gland diseases. Toxin exposure: alcohol abuse; smoking. Long-term use of certain heart medications, including: antiarrhythmic drugs; glycosides; diuretics. Autonomic disorders. Electrolyte imbalance (disturbance in the body's metabolism of electrolytes - sodium, potassium, magnesium). Oxygen starvation for bronchitis, sleep apnea, anemia.
Complications of extrasystole
Group extrasystoles can transform into more dangerous rhythm disturbances: atrial - into atrial flutter, ventricular - into paroxysmal tachycardia. In patients with atrial overload or dilatation, extrasystole can develop into atrial fibrillation.
Frequent extrasystoles cause chronic insufficiency of coronary, cerebral, and renal circulation. The most dangerous are ventricular extrasystoles due to the possible development of ventricular fibrillation and sudden death.
Classification and causes of supraventricular extrasystole
The disease is characterized by extraordinary premature excitation of the heart
Supraventricular extrasystole is a special condition directly related to heart rhythm disturbances. The disease is expressed in an extraordinary contraction of either the entire heart or its individual sections.
Supraventricular extrasystole is also called supraventricular extrasystole, and it is characterized by premature impulses that occur in ectopic foci located in the atria.
As a result of this action, defective contraction of the heart occurs. There are cases when heart contractions in the atria can cause atrial fibrillation and supraventricular tachycardia.
Classification of the disease
In medicine, it is customary to classify supraventricular extrasystole according to several characteristic features:
According to the location of the outbreak:
atrioventricular (occur in the septum between the atria and ventricles); atrial (occurs in the upper parts of the heart).
By frequency (per minute):
group (several extrasystoles in a row are observed at once); single (up to five contractions are observed); multiple (from five extraordinary reductions); doubles (two in a row).
According to the number of emerging outbreaks:
monotopic (there is one focus); polytopic (there are several foci).
By order:
ordered extrasystoles (meaning the alternation of normal contractions with extrasystoles); disordered extrasystoles (implies the absence of any pattern in the alternation).
By time of appearance:
early (appear during atrial contraction); medium (appears in the interval between contractions of the atria and ventricles); late (appear during contraction of the ventricles with complete relaxation of the heart).
Causes
There are several reasons that can lead to the development of supraventricular extrasystole:
Cardiac, that is, cardiac causes. These include the presence of diseases such as: Ischemic disease. In this case, this is due to insufficient blood supply and oxygen starvation; Myocardial infarction. The death of an entire section of the heart muscle occurs, which is subsequently replaced by scar tissue; Cardiomyopathy. In such cases, damage to the heart muscle occurs; Myocarditis. This is inflammation of the heart muscle; Congenital/acquired heart defects (implies a violation of the structure of the heart); Heart failure. Here we are talking about conditions when the heart is not able to fully perform its function of pumping blood. Drug treatment. In this case, it is meant that the causes of the disease can be various drugs that were taken by the patient, either uncontrolled or over a long period of time. These medications include the following: drugs against arrhythmia (they can cause irregular heart rhythms); cardiac glycosides, which are aimed at improving heart function while reducing the load on it; diuretics, which increase the production and excretion of urine. Violations of the level of electrolytes, that is, a change in the existing proportions of the ratio of salt elements: potassium, magnesium, sodium. Toxic effects on the body, namely, the effects of cigarettes and alcohol. Disorders of the autonomic nervous system. The presence of the following hormonal diseases: diabetes mellitus (the pancreas is affected, which leads to disturbances in glucose metabolism); adrenal gland diseases; thyrotoxicosis (the thyroid gland secretes an increased amount of hormones that have a destructive effect on the body). Chronic oxygen starvation (hypoxia). This is possible if the patient has diseases such as sleep apnea (short-term stops in breathing during sleep), bronchitis, and anemia (anemia). Idiopathic cause, that is, the case when the disease occurs without any reason.
Symptoms
The disease often has no obvious symptoms
Supraventricular extrasystoles are insidious in that they often do not have any pronounced symptoms.
Patients often do not have any complaints, and the disease proceeds unnoticed, but only for some time.
Supraventricular extrasystole may have the following symptoms:
Shortness of breath, feeling of suffocation. Dizziness (this occurs due to decreased blood flow and oxygen starvation). Weakness, increased sweating, discomfort. Interruptions in the work of the heart (feeling of beats outside the heart). “Hot flashes” that have no reason.
The most important and common sign of the disease is a feeling as if the heart stops for a while. Most often this causes panic, anxiety, paleness, etc. in people.
Generally speaking, supraventricular extrasystole accompanies a large number of heart diseases. Sometimes it is associated with the presence of vegetative or psycho-emotional disorders.
Diagnosis of the disease
Diagnosis of the disease is based on the following points:
Analysis of patient complaints, which refers to a feeling of “interruptions” in the heart, general weakness and shortness of breath. The doctor will definitely ask how long ago all these symptoms appeared, what treatment was carried out previously, if any, and how the signs of the disease changed during this time; Analysis of anamnesis. The cardiologist must find out what operations and diseases the patient has had previously, what kind of lifestyle he leads, what bad habits he has, if any. Heredity is also important, namely, the presence of heart disease in close relatives; General inspection. The doctor feels the pulse, listens and taps the heart in order to identify any changes in the boundaries of the organ; Taking a biochemical analysis of blood, urine, analysis of hormone levels; ECG data. It is this moment that makes it possible to identify changes characteristic of the disease; Holter monitoring indicators. This diagnostic procedure involves the patient wearing a machine that performs an ECG throughout the day. In this case, a special diary is kept where absolutely all the patient’s actions are recorded. The ECG and diary data are subsequently compared, which makes it possible to identify unknown heart rhythm disturbances; Echocardiography data. The procedure allows us to identify the fundamental causes of the disease, if any.
Consultation with a therapist and cardiac surgeon is also important, so if you have the above symptoms, it is better to contact them along with a visit to a cardiologist.
Treatment
Treatment of supraventricular extrasystole has two types:
conservative; surgical.
Conservative treatment involves prescribing several drugs against arrhythmia from different groups of drugs. This allows you to normalize your heart rate and improve heart function.
The choice of medication depends on the type of extrasystole and the presence/absence of contraindications to the drug.
Commonly prescribed medications include the following:
etacizin; anaprilin; obzidan; allapinin; arrhythmil; verapamil; amiodarone.
Treatment can only be prescribed by an experienced doctor
Also, the doctor, at his discretion, can prescribe cardiac glycosides to the patient, which are designed to improve heart function while reducing the load on it. It is also possible to prescribe medications that lower blood pressure.
Surgical intervention is used only in the case of a complete lack of improvement after taking medications from different groups. The operation is most often recommended for young patients.
The following types of intervention are possible:
Radiofrequency catheter ablation. A catheter is inserted through a large blood vessel into the atrium cavity, through which, in turn, an electrode is passed that cauterizes the altered area of the patient’s heart; Open heart surgery, which involves excision of ectopic foci (those areas of the heart where an additional impulse occurs).
Possible complications
How dangerous is the disease? It can cause the following complications:
Ischemic disease. In this case, the heart ceases to perform its function correctly; Change the structure of the atria; Create atrial fibrillation (that is, defective heart contractions).
Preventive measures and forecasts
When preventing the disease, the following is recommended:
Maintain a rest regime, control the duration of sleep; Eat right, exclude spicy foods, fried, salty, canned foods from your diet. Doctors recommend eating more greens, fruits, and vegetables; Any medication intake should be carried out under the supervision of a specialist; Quitting smoking, alcohol; Contact a cardiologist at the first manifestation of symptoms of the disease.
In conclusion, I would like to note that if you consult a doctor in a timely manner and follow all norms and recommendations, patients are given a good prognosis.
Extrasystole is a condition related to heart rhythm disturbances, or arrhythmias, which are expressed by extraordinary contractions of the heart or its parts. Depending on the location of the source of excitation, it can be ventricular, atrial, atrioventricular.
Supraventricular extrasystole, or supraventricular, is characterized by the fact that premature impulses arise in ectopic foci located in the upper parts of the heart (atria) or in the septum between the ventricles and atria, which is called the antiventricular. As a result, incomplete additional contractions of the heart occur.
Therapy tactics
A cardiologist is involved in the treatment of supraventricular extrasystole. Only he can prescribe medications and select the dosage regimen. If there are no structural heart diseases, and supraventricular extrasystole is asymptomatic, treatment is not required. When signs of the disease are felt by the patient, taking medications is mandatory.
Drug treatment
Taking antiarrhythmic drugs is the basis of treatment for EVE. Medicines from this group have approximately the same therapeutic effect, but at the same time have various contraindications and side effects. Therefore, the attending physician takes into account all the nuances and selects a drug based on the course of the pathology and the individual characteristics of the patient’s body. There are 4 classes of antiarrhythmic drugs:
| Class | Name | Short description |
| I | Propaphenone, Ritmonorm, Allapinine, Quinidine | Sodium channel blockers. The main purpose is arrhythmia of the type of extrasystole |
| II | Nebilet, Concor, Anaprilin | Beta blockers. The drugs in this group reduce heart rate, reduce blood pressure, and increase bronchial tone |
| III | Amiodarone, Sotalol, Sematilid, Dofetilide | Potassium channel blockers and/or slow sodium channel activators. Normalize heart rate, prolong the action of cardiomyocytes. Medicines of the group are toxic |
| IV | Verapamil, Adenosine | Calcium channel blockers. They increase myocardial resistance to hypoxia, dilate coronary vessels, and improve blood properties. Often prescribed to prevent the development of heart pathologies. Extrasystole is not affected |
Attention! Treatment with antiarrhythmic drugs may be accompanied by bronchospasm, dyspeptic symptoms, liver dysfunction, dizziness, convulsions, and tremor.
Atropine, Digoxin, Strophanthin, Magnesium Sulfate are medications that are not included in the group of antiarrhythmic drugs, but doctors often prescribe them.
Surgical methods
Surgery is indicated when the symptoms of the disease are not controlled by medications and the patient is at risk of developing heart failure. The heart surgeon may use one of the following surgical methods:
- Radiofrequency ablation of the heart. A method of endoscopic treatment of cardiac arrhythmias, which consists of cauterizing additional conduction pathways in the heart muscle using special equipment. Typically, with supraventricular extrasystole, the success of this procedure reaches 98%.
- Open heart surgery. The general principle boils down to the fact that there is an intervention in the human body in order to carry out the necessary measures on an open heart. It involves excision of pathologically altered areas of the heart muscle in which abnormal impulses occur.
The operation is performed only in extreme cases.
Causes
Supraventricular extrasystole can be idiopathic, that is, it occurs without any apparent reason. It can be observed in practically healthy people at any age. In addition, there are different reasons for the development of supraventricular extrasystole:
Heart diseases: heart failure; cardiac ischemia; myocardial infarction; heart defects, both congenital and acquired; myocarditis (inflammatory processes in the heart muscle); cardiomyopathies. Endocrine diseases: diabetes mellitus; hyperthyroidism, or thyrotoxicosis; diseases of the adrenal glands. Effects of toxins: abuse alcohol; tobacco smoking. Long-term use of certain heart medications, including: antiarrhythmic drugs; glycosides; diuretics. Autonomic disorders. Electrolyte imbalance (impaired metabolism of electrolytes in the body - sodium, potassium, magnesium). Oxygen starvation with bronchitis, sleep apnea, anemia.
Causes of pathology
One of the features of the pathology is that a single extrasystole does not manifest itself in any way. At this moment, a healthy person will not feel any discomfort. The causes of supraventricular extrasystole are varied, among them the most common are heart diseases:
- Acute myocardial infarction is necrosis of a portion of the myocardium as a result of prolonged circulatory disturbance in the heart muscle.
- Coronary heart disease (CHD) is myocardial damage caused by hypoxia.
- Myocarditis is an inflammatory process in the heart.
- Congenital (abnormalities of the heart structure existing from birth) and acquired (stenosis, valve insufficiency, combined and combined defects) heart defects.
- Hypertension is a persistent increase in blood pressure.
- Chronic heart failure.
- Various cardiomyopathies are a group of various myocardial lesions that are not associated with an inflammatory, tumor process or lack of blood supply to the heart muscle.
Classification
Supraventricular extrasystoles are classified according to several criteria:
According to the location of the outbreak
atrial - in the upper parts of the heart, atrioventricular - in the septum between the ventricles and atria.
Frequency per minute
single (up to five extraordinary contractions), multiple (more than five), group (several extrasystoles in a row), paired (two in a row).
By number of outbreaks
monotopic (1 focus) polytopic (several lesions).
By time of appearance
early (with contraction of the atria), middle (between the time of contraction of the atria and the ventricles), late (with contraction of the ventricles or with complete relaxation of the heart).
By order
ordered (alternating normal contractions with extrasystoles), disordered (there is no pattern).
Description of the pathology
However, not everyone understands what it is. Single ventricular extrasystoles are a disturbance in the rhythm of the heart that occurs under the influence of premature nerve impulses emanating from the walls of the right or left ventricle. The extrasystoles that develop in this case, as a rule, affect only the ventricular rhythm, without affecting the upper parts of the heart. But single extraordinary contractions that come from the atrioventricular septum and atria can excite ventricular extrasystoles.
Such a pathology, in the absence of organic damage to the heart, as a rule, does not pose any danger to life. The cardiac cycle is a certain sequence of processes occurring during a single cardiac contraction and its subsequent weakening. Each such cycle consists of ventricular systole, atrium and diastole. This is a relaxation of the muscle in the period of time between systoles, during which the cavities of the heart expand.
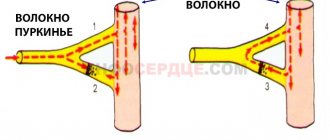
There are electrical (activity that stimulates the myocardium) and mechanical (contraction of the heart muscle, reduction in the volume of its chambers) systole. At rest, the cardiac ventricle of an adult is capable of pumping out approximately 50–70 ml of blood per systole. Normal cardiac impulses are produced in the sinus node, which is located in the upper part of the heart. 1 single ventricular extrasystole is characterized by premature excitation of the ventricles in relation to the leading rhythm of the heart, emanating from the conduction system of this organ, in particular, Purkinje fibers and branches of the His bundle.
Signs
With supraventricular extrasystole there are often no complaints. In some cases, the disease causes the following symptoms:
lack of air, shortness of breath; interruptions in the work of the heart: a feeling of “reversals” of the heart or beats out of rhythm; dizziness; general weakness.
In children, supraventricular extrasystole most often occurs without any symptoms. Complaints usually come from older children. The child may experience weakness, irritability, fatigue, dizziness, and a feeling of heart failure.
How is pathology diagnosed?
Clinical assessment and diagnosis of ventricular extrasystoles should be carried out fully, taking into account the patient’s complaints, as well as the complex state of the patient’s cardiovascular, autonomic and central nervous systems.
Ventricular extrasystoles are counted per 100 QRS complexes. They are considered frequent if they exceed 10%. Using daily monitoring of the rhythm of the heart muscle, a direct connection was noted between the occurrence of ventricular extrasystoles and human physical activity. Thus, many athletes complain of frequent “interruptions” and “fading” in the heart’s function during training or active pastime.
Diagnostics
Diagnosis is based on the patient’s complaints, a general examination with listening and measuring the pulse, as well as on the patient’s story about the lifestyle, bad habits, heredity, past illnesses and operations.
In addition, laboratory tests are required: general and biochemical analysis of blood and urine, determination of hormonal status.
Pulse measurement
Instrumental diagnostic methods include the following: ECG, Holter monitoring, electrophysiological study, echocardiography (ultrasound of the heart), stress tests with recording of an electrocardiogram during and after exercise.
Diagnosis of extrasystole
The main objective method for diagnosing extrasystole is an ECG study, however, it is possible to suspect the presence of this type of arrhythmia during a physical examination and analysis of the patient’s complaints. When talking with the patient, the circumstances of the occurrence of arrhythmia are clarified (emotional or physical stress, in a calm state, during sleep, etc.), the frequency of episodes of extrasystole, and the effect of taking medications. Particular attention is paid to the history of past diseases that can lead to organic heart damage or their possible undiagnosed manifestations.
During the examination, it is necessary to find out the etiology of extrasystoles, since extrasystoles with organic heart damage require different treatment tactics than functional or toxic ones. When palpating the pulse on the radial artery, an extrasystole is defined as a prematurely occurring pulse wave followed by a pause or as an episode of pulse loss, which indicates insufficient diastolic filling of the ventricles.
When auscultating the heart during extrasystole, premature I and II sounds are heard above the apex of the heart, while the I tone is strengthened due to low filling of the ventricles, and the II sound is weakened as a result of a small ejection of blood into the pulmonary artery and aorta. The diagnosis of extrasystole is confirmed after an ECG in standard leads and daily ECG monitoring. Often, using these methods, extrasystole is diagnosed in the absence of patient complaints.
Electrocardiographic manifestations of extrasystole are:
- premature occurrence of the P wave or QRST complex; indicating a shortening of the pre-extrasystolic coupling interval: with atrial extrasystoles, the distance between the P wave of the main rhythm and the P wave of the extrasystoles; with ventricular and atrioventricular extrasystoles - between the QRS complex of the main rhythm and the QRS complex of the extrasystoles;
- significant deformation, expansion and high amplitude of the extrasystolic QRS complex during ventricular extrasystole;
- absence of the P wave before the ventricular extrasystole;
- following a complete compensatory pause after a ventricular extrasystole.
Holter ECG monitoring is a long-term (over 24-48 hours) ECG recording using a portable device attached to the patient’s body. Registration of ECG indicators is accompanied by keeping a diary of the patient’s activity, where he notes all his sensations and actions. Holter ECG monitoring is performed for all patients with cardiac pathology, regardless of the presence of complaints indicating extrasystole and its detection with a standard ECG.
The identification of extrasystole, not recorded on the ECG at rest and during Holter monitoring, can be done by the treadmill test and bicycle ergometry - tests that determine rhythm disturbances that appear only during exercise. Diagnosis of concomitant cardiopathology of an organic nature is carried out using ultrasound of the heart, stress echo-CG, and MRI of the heart.
Treatment
If there are no organic heart diseases, the patient has no complaints, then specific treatment for supraventricular extrasystole, as a rule, is not carried out . Therapy is usually indicated when symptoms are present and poorly tolerated.
First of all, the doctor assesses the number of extraordinary heart contractions per day. A single extrasystole does not pose a health hazard. Then you need to make sure that there are no organic heart diseases. If the patient has subjective complaints and does not tolerate them well, sedatives may be used. The doctor should evaluate the advisability of taking antiarrhythmic drugs. The fact is that they have many side effects, and therefore the treatment can become more dangerous than the disease itself. Rare supraventricular extrasystole (several tens or hundreds of contractions per day) does not require taking such serious medications. Thus, in the absence of complaints and diseases, the patient is recommended:
Eat right, that is, exclude preservatives, fatty, fried, spicy, hot foods. Eat more plant foods rich in fiber. Eliminate bad habits (alcohol, smoking, energy drinks). Avoid stress, maintain moderation during physical activity. Ensure restful and sufficient sleep. Spend more time outside.
In the presence of heart disease and severe symptoms, conservative treatment with glycosides and antiarrhythmic drugs is indicated, which are selected strictly individually.
If medications do not help and the patient does not tolerate extrasystole, surgical treatment is performed.
This may be an open operation in which ectopic lesions are removed. As a rule, it is performed when intervention for heart valve replacement is required.
Another type of surgical treatment is radiofrequency ablation of lesions using a catheter, which is inserted into a large blood vessel, an electrode is passed through it and the area where the pathological impulse occurs is cauterized.
Prediction for therapy of this disease
Supraventricular extrasystole responds well to therapeutic and drug treatment.
This type of extrasystole does not cause sudden death (ventricular extrasystole can cause sudden death in the presence of heart disease).
Complications of supraventricular extrasystole
If supraventricular extrasystole is not treated or not treated in a timely manner, heart failure and pathological changes in the atria and cardiac ventricles may develop.
Atrial fibrillation does not occur suddenly; it is a consequence of frequent additional contractions that have occurred for several calendar years without drug treatment.
There is also a risk of developing supraventricular tachycardia.
Timely consultation with a doctor leads to a complete cure of this disease.
Forecast
Supraventricular extrasystole usually indicates a good prognosis. It does not lead to sudden death, like ventricular death, in which such a risk exists in the presence of organic heart disease.
The term “extrasystole” usually refers to the occurrence of a nerve impulse followed by contraction of the heart, ahead of the normal rhythm. Depending on the location of the impulse, several types of extrasystole are distinguished. One of the types is supraventricular extrasystole.
Possible complications
If the heart rhythm abnormality is advanced, it can provoke the development of coronary heart disease, heart failure, atrial fibrillation, angina pectoris, destructive changes in the structure of the organ, and disruption of its activity. There is a change in cerebral circulation (fainting and cuts occur).
Important! Supraventricular extrasystole is not an independent disease and does not require mandatory medical or surgical treatment. But a person with additional heartbeats must undergo regular medical examinations and be seen by a cardiologist.
Supraventricular extrasystole is a pathology associated with a disturbance in heart rhythm as a result of the appearance of additional heart contractions. Its appearance does not lead to death. But the anomaly is characterized by unpleasant symptoms, reduces a person’s quality of life, and in the absence of proper treatment can lead to more serious problems with the functioning of the organ.
An anomaly occurs in both adults and children. In order to prevent the development of complications, it is necessary to consult a doctor for advice and undergo a full medical examination to identify and eliminate the causes of the development of the disorder.
Features of extrasystole
Premature contraction of the heart is not always noticed by the patient if there are no provoking factors for further development of the disease. But, if another heart disease occurs, the arrhythmia worsens, which becomes life-threatening for the child and adult.
Children cannot express their condition in words and are not aware of the existing pathology, so in childhood it is more difficult to suspect the presence of a disease than in adults. The supraventricular type of extrasystole occurs several times less frequently than the ventricular type.
For more information about what it is, rare and frequent sinus, single, single supraventricular extrasystoles, read on.
Symptoms
Supraventricular extrasystoles are insidious in that they often do not have any pronounced symptoms.
Patients often do not have any complaints, and the disease proceeds unnoticed, but only for some time.
Supraventricular extrasystole may have the following symptoms:
- Shortness of breath, feeling of suffocation.
- Dizziness (this occurs due to decreased blood flow and oxygen starvation).
- Weakness, increased sweating, discomfort.
- Interruptions in the work of the heart (feeling of beats outside the heart).
- “Hot flashes” that have no reason.
The most important and common sign of the disease is a feeling as if the heart stops for a while. Most often this causes panic, anxiety, paleness, etc. in people.
Generally speaking, supraventricular extrasystole accompanies a large number of heart diseases. Sometimes it is associated with the presence of vegetative or psycho-emotional disorders.
Classification
Supraventricular extrasystole has several varieties. The classification may be based on the source of the outbreak, etc.
According to the location of the outbreak
According to the localization of the source of excitation, they are distinguished:
sinus sudden contraction, i.e. the focus of excitation is in the sinoatrial node; atrial pathology, in which excitation is generated in the structures of the atypical muscles of the atria; atrioventricular type of extrasystole, originating in the atrioventricular node, localized in the tissue separating the atria and ventricles.
By the number of arousals
By the number of excitations in 1 minute:
single, if there are 1-5 unscheduled reductions; paired, 2 pulses formed with a minimum time interval between each other; group (several extrasystoles are noted in a short period of time); multiple, the number of which exceeds 5 premature contractions.
By the number of premature contractions
By the number of premature contractions:
OUR READERS RECOMMEND!
For the prevention and treatment of cardiovascular diseases, our readers recommend the drug “ReCardio”. This is a natural remedy that acts on the cause of the disease, completely preventing the risk of heart attack or stroke. ReCardio has no contraindications and begins to act within a few hours after its use. The effectiveness and safety of the drug has been repeatedly proven by clinical studies and many years of therapeutic experience.
Doctors' opinion... >>
monotopic, if the emerging focus of excitation is the only one; polytopic – there are several foci of nerve impulse generation.
According to the organization of extrasystoles
According to the organization of extrasystoles:
organized (there is a pattern of a certain alternation of premature and planned impulses); disorganized (there is no pattern of alternation of premature and timed impulses).
By time of manifestation
By time of manifestation:
early, characterized by contractions during the 1st stage of the cardiac cycle - atrial systole; average, arising in the post-systolic period of the atria, preceding ventricular systole; late, when supraventricular extrasystole appears during ventricular systole.
According to symptoms
Symptomatically, supraventricular extrasystole is divided into:
organic, during which the patient feels worse in a standing position than in a lying state; functional, characterized by better health of the patient when standing.
Division of extrasystole by variety
The division is based on the root of the manifestation of the outbreak. Varieties of extrasystole can be:
- Location of the outbreak;
- Number of cuts;
- Organization of extrasystole;
- Number of additional cuts;
- Severity of symptoms;
- Manifestation over time.
Classification by location of extrasystoles
The locality of this variety is divided into:
- Sinus contraction - the root of localization is located in the sinus node of the atrium;
- Atrial contraction - pathology is located in the muscles of the atrium;
- Atrioventricular extrasystole - the source of the disease is in the wall that separates the ventricle from the atrium.
Causes of supraventricular extrasystole
Supraventricular extrasystole is not a rare disease, sometimes it has no cause and, especially in childhood, no noticeable manifestations. In more than half of the cases, supraventricular extrasystole is recorded when:
Heart pathologies: myocarditis – inflammation of the heart muscles (myocardium); coronary heart disease, in which the circulatory organ suffers from oxygen starvation during a period of impaired blood flow in the heart; damage to the heart muscle of a non-inflammatory and vascular nature (cardiomyopathy); a scar formed from connective tissue after acute myocardial infarction; heart failure, when the main circulatory organ is unable to fully perform its functions; heart defects of any etiology. Taking certain medications under conditions of uncontrolled use or for periods of use exceeding those specified by the doctor or in the instructions for the drug. As medications, a similar effect is achieved by taking: medications that normalize abnormal heart rhythms; diuretics that increase urine secretion and output; cardiac glycosides aimed at increasing the performance of the myocardium while reducing the overall load on the organ. Changes in the acid-base balance when the norm of the content of alkali and alkaline earth metal ions (K+, Ca2+, Na+, etc.) shifts. The toxic effects of certain poisons, including nicotine and alcohol. Deviations in the functioning of the autonomic nervous system. Repeated conditions of hypoxia resulting from apnea (nocturnal cessation of breathing), anemia, inflammation of the bronchi. Diseases of the endocrine system: excessive release of thyroid hormones into the blood by the thyroid gland and their destructive effect on cells (the condition of thyrotoxicosis); dysfunction of the adrenal glands; diabetes mellitus, leading to deviations in blood glucose concentrations. No apparent cause (idiopathic cause).
Forecast for extrasystole
The prognostic assessment of extrasystole depends on the presence of organic heart damage and the degree of ventricular dysfunction. The most serious concerns are caused by extrasystoles that develop against the background of acute myocardial infarction, cardiomyopathy, and myocarditis. With pronounced morphological changes in the myocardium, extrasystoles can turn into atrial or ventricular fibrillation. In the absence of structural damage to the heart, extrasystole does not significantly affect the prognosis.
The malignant course of supraventricular extrasystoles can lead to the development of atrial fibrillation, ventricular extrasystoles - to persistent ventricular tachycardia, ventricular fibrillation and sudden death. The course of functional extrasystoles is usually benign.
Symptoms of pathology
It is not always possible to recognize the disease in time due to its low manifestation of symptoms. When symptoms appear, the disease moves into the next stage, which takes longer and more difficult to treat. Patients typically present with the following symptoms:
the heart works intermittently, sometimes there is a feeling that it is “jumping out of the chest”; malaise, feeling of discomfort; excessive sweating; increased irritability; anxiety, fear of death; dizziness in the head; oxygen starvation (not enough air).
Supraventricular extrasystole is often accompanied by another cardiac or somatic disease. Vegetative-vascular dystonia is characterized by increased innervation of the heart by the parasympathetic division of the autonomic nervous system, independent of the degree of physical activity and is accompanied by the symptoms described above. When examined, an electrocardiogram reveals supraventricular extrasystole.
The disease also accompanies osteochondrosis of the upper spine, with pinching of blood vessels and insufficient blood supply to the heart and other organs.
During pregnancy, women experience extrasystole if blood tests show increased levels of thyroid hormones and low hemoglobin concentration (anemia). Pathology can be observed after suffering inflammation of the bronchi and lungs, physical fatigue, problems in the functioning of the circulatory system.
Extraordinary heart beats are a parameter of compensation for the work of the parasympathetic system, aimed at weakening the work of the heart after eating.
Symptom severity
Supraventricular extrasystoles (hereinafter referred to as SVE) according to symptoms are divided into:
- Organic systole. This is a condition in which the patient feels much worse in an upright position than in a horizontal position;
- Systole is functional. A condition when the patient feels much better in an upright position than in a lying position.
The patient cannot always recognize the pathology at the initial stage of the disease. The symptoms of this disease do not appear clearly and often the person simply does not feel them.
When the symptoms become pronounced, then we can talk about a more complex stage of development of the pathology, which is much more difficult to treat. Therapy for this stage of the disease is quite complex and takes a long period of time.
In order to recognize supraventricular extrasystole, you need to listen to the following symptoms in the body:
- The performance of the heart occurs intermittently. A situation in which the heart simply “jumps out of the chest”;
- Discomfort behind the chest;
- Malaise of the whole body;
- Large amounts of sweat;
- Unreasonable irritability;
- Deep state of overexcitation;
- State of paranoia;
- Sense of anxiety;
- Dizziness that occurs over a long period;
- Shortness of breath or lack of oxygen in the body.
Supraventricular extrasystole quite often is not the main diagnosis of cardiac abnormalities, but is a concomitant disease of heart disease, and can also be a consequence of somatic diseases.
Dystonia (vegetative-vascular) is confirmed by identical symptoms of increased heart rate, which does not depend on the amount of physical activity. When examined using an electrocardiogram, supraventricular (supraventricular) extrasystole is detected.
Also, this disease can provoke osteochondrosis of the thoracic spine. Disorders in the spine impinge on blood vessels that do not normally supply vital internal organs in the body. The heart muscle suffers the most from insufficient blood circulation. The main pathologies due to which she may get sick
Diagnostics
Most often, the disease can be detected using an electrocardiogram. This is a method available to all clinics and the most widely used. In some cases, when it is necessary to find out the dependence of the occurrence of extrasystole on physical activity, they resort to measuring ECG indicators after the patient performs physical activity on an exercise bike, as well as performing a trimedyl test.
The doctor also collects data for anamnesis, measures pulse and systolic pressure, and listens to the heart with a phonendoscope.
Read below about what treatment frequent and rare supraventricular extrasystole requires.
Prevention of extrasystole
In a broad sense, the prevention of extrasystole involves the prevention of pathological conditions and diseases underlying its development: ischemic heart disease, cardiomyopathies, myocarditis, myocardial dystrophy, etc., as well as the prevention of their exacerbations. It is recommended to exclude drug, food, and chemical intoxications that provoke extrasystole.
For patients with asymptomatic ventricular extrasystole and without signs of cardiac pathology, a diet enriched with magnesium and potassium salts, cessation of smoking, drinking alcohol and strong coffee, and moderate physical activity are recommended.
Treatment
If a patient with a supraventricular extrasystole detected on an ECG has no complaints, then a treatment regimen, as a rule, is not drawn up. It is recommended to avoid provoking factors that may further aggravate the situation and lead a healthy lifestyle. When complaints arise, a cardiologist or therapist counts the number of sudden contractions to determine the type of disease according to the specified classification and selects a treatment method for the patient. Only single systoles do not require treatment.
The video below will tell you in an interesting and accessible way about the treatment and prevention of extrasystole:
Therapeutic
If the patient’s condition is not dangerous, the doctor recommends taking relaxers and following some recommendations:
normalize nutrition by eliminating smoked foods, saltiness, sweets, etc. from the diet; get rid of bad habits, if this seems unlikely, then their harmful influence should be reduced; learn to quickly overcome psycho-emotional stress; avoid eating in the late evening hours; observe the recommended number of hours allotted for sleep; take walks in the fresh air more often.
Medication
Medications are prescribed depending on the identified pathologies. Independent extrasystole is treated with Cordarone, Anaprilin and their analogues under the supervision of a doctor.
Symptoms of extrasystole are eliminated by treating the concomitant disease. If the cause lies in osteochondrosis, the doctor prescribes drugs to relax muscles and treat blood vessels (Mexidol, Mildronate). The recommendation to take β-blockers (Egilok et al.) cannot be ruled out.
Surgical treatment
Surgical intervention is resorted to when the therapeutic effect is not achieved with medication. The patient is prescribed catheter ablation or replacement of the pacemaker (sinoatrial or atrioventricular node) with an artificial analogue.
ethnoscience
Extrasystole is treated with an infusion of herbs from a mixture of hawthorn flowers, hop cones and vegetative parts of heather, motherwort and lemon balm. Before using the infusion, consult a doctor.
Symptoms of extrasystole
Subjective sensations during extrasystole are not always expressed. The tolerance of extrasystoles is more severe in people suffering from vegetative-vascular dystonia; patients with organic heart damage, on the contrary, can tolerate estrasystole much easier. More often, patients feel extrasystole as a blow, a push of the heart into the chest from the inside, caused by vigorous contraction of the ventricles after a compensatory pause.
Also about hearts, interruptions and fading in his work. Functional extrasystole is accompanied by hot flashes, discomfort, weakness, anxiety, sweating, and lack of air.
Frequent extrasystoles, which are early and group in nature, cause a decrease in cardiac output, and, consequently, a decrease in coronary, cerebral and renal circulation by 8-25%. Patients with signs of cerebral atherosclerosis experience dizziness, and transient forms of cerebral circulatory disorders (fainting, aphasia, paresis) may develop; in patients with coronary artery disease - angina attacks.
Symptoms of manifestation
Specific symptoms in SES are sometimes practically not observed. However, in some cases, the symptoms of the pathology are extremely pronounced and significantly complicate the person’s condition.
The appearance of extraordinary atrial rhythms manifests itself with the following symptoms:
- the occurrence of shortness of breath;
- attacks of suffocation;
- general malaise;
- dizziness;
- sweating;
- hot flashes;
- interruptions or frequent heartbeats, sudden jolts.
The feeling of fear of sudden death, caused by the feeling of cardiac arrest, is the most common complaint of patients with SES. Developing extrasystole is characterized by the likelihood of more intense symptoms and signs of poor health.
Treatment with folk remedies
Of course, in folk medicine there are recipes designed to treat this disease. A one-time dose of any drug, even a medicinal one, will have absolutely no effect on the manifested arrhythmia, and this also applies to folk remedies.
Arrhythmia is a disturbance in the normal functioning of the heart muscle caused by certain reasons. During treatment, you should exercise maximum attention and caution, and be sure to first consult with a specialist.
Currently, traditional medicine recipes are the most in demand and are quite popular.
- Treatment with valerian
- Cornflower will help avoid acute attacks
- Calendula will eliminate heart rhythm disturbances
- Horsetail will eliminate heart weakness
- Hawthorn tincture with alcohol
A tincture of it is often taken for stress, nervous excitement, and overexertion. By the way, there is an interesting fact: it is believed that arrhythmia in some cases occurs in patients against the background of a disturbed psycho-emotional state or stress. If arrhythmia is caused by stress, then ordinary valerian is the best remedy.
To prepare the infusion, 1 tbsp is enough. Brew a spoonful of plant roots with a glass of hot, just boiled water. Let it brew for 10 hours, strain and take 1 tbsp. l. 3 times a day.
Severe attacks accompanied by unpleasant sensations caused by polytopic pancreatic extrasystole can be stopped by using an infusion of cornflower.
For cooking you need 1 tbsp. l. Pour 1 cup boiling water over the plants and let it brew. Take before meals, 3 times a day. It is advisable to take the decoction when severe attacks occur.
Traditional medicine is very effective against extrasystole, because the disease causes disturbances in the normal functioning of the heart rhythm; medicinal plants help normalize the rhythm.
It will take 2 hours to prepare the infusion. l. dry plant, which are poured with boiling water, in the amount of two glasses. You need to leave for an hour, then strain and drink about 4 times a day, half a glass.
Often, arrhythmia occurs due to weakness of the heart muscle itself (myocardium); at first it manifests itself as a rare pancreatic extrasystole.
To train the muscle and, accordingly, eliminate the symptoms of arrhythmia, use an infusion of ordinary horsetail. To prepare 1 tbsp. l. The plants are poured with boiling water in the amount of three glasses and left for 3 hours in a sealed container. Take the resulting tincture 6 times a day, only 1 tbsp. l.
A very effective product, sold everywhere in pharmacies. If you are intolerant to ethyl alcohol, then you should not take it. It lowers blood pressure well, soothes, improves heart rate, and improves blood circulation.
It is taken in the amount of 10 drops, before meals, no more than three times a day. The tincture should not be overused, since it is made with alcohol. If consumed excessively, it will only cause harm, not benefit.
Doctors advise establishing a healthy lifestyle and diet:
- sleep in a cool room at least 7-8 hours a day;
- reduce salty, fried, hot foods in the diet to a minimum;
- smoke and drink alcohol as little as possible, it is better to eliminate energy drinks completely;
- walk in the fresh air for at least an hour a day, preferably 2 hours;
- moderate physical activity: swimming in the pool, taking the stairs instead of the elevator, skiing or jogging in the park. This is especially true for people with sedentary jobs.
Supraventricular (supraventricular) extrasystole occurs in people of any age. Mild cases do not require treatment. More serious ones may be accompanied by heart and other diseases and require drug therapy, and in extreme cases, surgical treatment. The main thing with this disease is to remain calm and lead a healthy lifestyle.
The best prevention of supraventricular extrasystole is to eliminate the causes that influence its occurrence. Forget about all habits that are harmful to the vascular system and health in general. Stop smoking and alcohol. Reduce your intake of strong coffee or tea.
Try to avoid stress and overwork. Include in your diet foods that have a beneficial effect on the functioning of the heart and the entire circulatory system. Lead a healthy lifestyle, strengthen your heart muscle.
Remember to get plenty of rest. Don't disturb your sleep schedule.
When faced with a stressful situation, buy calming drops at the pharmacy. This could be: tincture of hawthorn, valerian or motherwort. At the first manifestations of the disease, it is important to begin treatment immediately so as not to start the process of its development.
Supraventricular pacemaker is an excitation of the heart caused by an extraordinary impulse emanating from the atria or atrioventricular node. The main mechanism of extrasystole is the mechanism of micro-reentry in areas of the myocardium or conduction system with different conductivity and unidirectional blockade of impulse conduction. Another common mechanism of ECS is pathological focal automatism of a section of the conduction system of the heart, as well as increased oscillatory triggering activity of the membranes of myocardial sections in late systole or early diastole.
The appearance of this type of arrhythmias is facilitated by autonomic disorders, as well as any pathological changes in the myocardium of an inflammatory, ischemic, dystrophic or sclerotic nature. The intoxicating effects of various drugs, including antiarrhythmics, also play a role. In medical practice, the most common cause of supraventricular pacemaker is disturbances of autonomic balance with a predominance of vago- or sympathotonia. These disorders are closely related to emotional, meteorological factors, as well as the influence of smoking, coffee and alcohol. Supraventricular pacemaker can be observed in healthy individuals in amounts up to 20-30 per day.
Clinical picture. The pacemaker is often not felt by patients. In other cases, they are disturbed by freezing, tumbling, a feeling of shortness of breath, a lump in the chest, freezing followed by a blow and a short period of tachycardia. Frequent pacing may feel like chest tightness and shortness of breath.
ECG signs of supraventricular pacemaker:
1. Premature appearance of the P wave with the QRS complex.
2. Deformation and change in the polarity of the P wave of the extrasystole.
3. The presence of an incomplete compensatory pause: the sum of the time interval before and after the extrasystole is less than two normal intervals before the extrasystole.
4. The presence of a slightly changed extrasystolic QRS complex. An aberrant complex during supraventricular pacemaker may resemble a widened and deformed ventricular complex, but there is a deformed P wave before the pacemaker, and the compensatory pause is incomplete (Fig. 14)
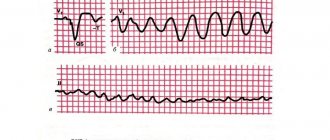
Figure 14. Suproventricular pacemaker, incomplete compensatory pause.
If a supraventricular extrasystole occurs before the end of the refractory period, then it is not carried out to the ventricles and there is no QRS. Such an pacemaker is called blocked (Fig. 15).
Fig. 15. The first ECG from above: before the atrial pacemaker, a slightly changed P wave. On the second ECG after the atrial pacemaker, QRS did not appear: the atrial pacemaker was blocked. On the third ECG, the P wave overlapped the QRS. On the fourth ECG, retrogradely excited atrial P layered onto the ST segment.
If the shape of the P wave changes from complex to complex, such pacemakers are called polymorphic supraventricular.
The management of patients with supraventricular pacemaker depends on the clinical situation:
1. Patients do not have any heart pathology. Their ECS is of a functional vegetative nature. There are no pathological ECG changes in the form of nonspecific ST-T changes or wide QRS.
2. Patients have heart pathology: defects, ischemic heart disease, cardiopathy, myocarditrophy. The ECG usually shows nonspecific ST-T changes of moderate or severe degree, or bundle branch block with QRS widening. However, they do not have dilatation of the left atrium (according to echocardiography, no more than 4 cm).
3. Patients have heart pathology with ECG changes and there is dilatation of the left atrium of more than 4 cm. In this group there is a threat of developing atrial fibrillation.
If patients of the first (functional) group of ECS are of little concern, then we can limit ourselves to general recommendations. It is necessary to provide an explanation of the non-hazardous nature of these violations. If patients in this group have few pacemakers, but they are poorly subjectively tolerated, or there are a large number of them (more than 1000/day) and the age of the patients is over 50 years (threat of atrial fibrillation), then such patients need to be treated with calcium antagonists or? - adrenergic blockers. It is necessary to start with half the daily doses, gradually increasing them if necessary: anaprilin 20 mg 3-4 times (up to 160 mg), metoprolol 25 mg 1-2 times (up to 100 mg), bisoprolol 2.5 mg 1-2 times (up to 10 mg) , betaxolol 5 mg 1-2 times (up to 20 mg), sotalol 40 mg 1-2 times (up to 160 mg), nebilet 2.5 mg 1-2 times. It is necessary to take into account that ECS often depends on the time of day. This can be used for a single dose of the drug at exactly this time of day.
If there is no effect from these AAPs, you can try first class drugs (start with half doses): propafenone 150 mg 2-3 times a day, allapinin 25 mg 2-3 times, quinidine durules 200 mg 2-3 times, etc. If ineffective, prescribe amiodorone 200-300 mg or sotolol 80-160 mg per day.
Treatment of patients in group 2 is also carried out, but it must be carried out more persistently, with larger doses and tried in combination with taking trimetazidine, Magnerot, Riboxin, Panangin.
Treatment of patients of group 3 with signs of left atrium dilatation, with a high risk of developing AF, can begin with amiodarone 200 mg 2-3 times a day, sotalol 80 mg 1-3 times, propafenone 150 mg 3-4 times, and also use ACE inhibitors and trimetazidine.
It is necessary to explain to the patient of the first and second group that disturbances in his myocardium leading to ECS can appear and disappear. Therefore, after 2-3 weeks of taking the drug, you can reduce the dosage until complete withdrawal. If the ECS appears again, then you need to resume taking the medications. Patients in the third group have to take medications constantly.
Normally, the human heart contracts rhythmically, after systole (contraction) comes diastole (relaxation).
Any disturbance of the heart rhythm (its rhythm, the duration of pauses between systole and diastole, additional contractions, etc.) is called arrhythmia.
The appearance of additional defective heart contractions - extrasystoles - is a pathology of the heart rhythm and can disrupt the functioning of the heart.
Supraventricular extrasystole - what is it, is it dangerous and why, what consequences can rare single or frequent attacks lead to?
Extrasystole occurs due to the appearance of an ectopic (abnormal) focus of trigger activity in the myocardium (heart lining) or its parts. Depending on the site of excitation, supraventricular (supraventricular - atrial and from the atrioventricular septum) and ventricular extrasystoles are distinguished.
The term “supraventricular” means that additional contraction occurs in the upper - supraventricular - part of the heart, that is, in the atrium or the septum between the atria and ventricles (antiventricular septum).
General information about pathology
In medical practice, several types of heart rhythm disturbances are considered, one of which is the option under consideration. Among medical terminology, synonymous names for supraventricular extrasystole (SES) are used. This:
- supraventricular extrasystole;
- premature atrial contractions;
- extraordinary atrial rhythms;
- atrial extrasystole;
- atrial extrasystole;
- atrial contractions;
- atrial premature complexes.
The reason for this diversity is the appearance of premature heartbeats emanating from the atria. Depending on the location of the source of excitation that provokes the occurrence of extraordinary contractions of the heart muscle or other parts of the heart, arrhythmia can be of the atrial, atrioventricular or ventricular type.
Consideration of the question of what supraventricular extrasystole is focuses attention on the characteristic signs of the pathological condition, that is, the occurrence of premature impulses in the zone of ectopic foci located in the atria. Also, an impulse can occur in the interventricular septum, located between the ventricles and atria
This septum is called the antiventricular septum. Heart contractions of this type are in the nature of defective additional contractions of the heart.
Based on the frequency of occurrence, supraventricular extrasystoles are divided into:
- rare frequency of manifestations, amounting to about 5 manifestations per minute;
- average frequency (6 – 15 beats per minute);
- frequent - more than 15 manifestations in 60 seconds.
Manifestations of extrasystole can be paired or single, regular and episodic.
According to statistics, heart rhythm disturbances are accidentally detected in more than half of healthy people during a routine preventive examination. In most cases, rare supraventricular extrasystole is detected, which occurs against the background of various diseases of the cardiovascular system.
The pathology in question is dangerous because it can provoke serious problems with cardiac activity - heart flutters, atrial fibrillation, tachycardia. It should be noted that even minor heart rhythm disturbances and accompanying symptoms are difficult for most patients to tolerate.
Relapse prevention and prevention measures
Specific prevention for supraventricular extrasystole is not required. Doctors advise establishing a healthy lifestyle and diet:
- sleep in a cool room at least 7-8 hours a day;
- reduce salty, fried, hot foods in the diet to a minimum;
- smoke and drink alcohol as little as possible, it is better to eliminate energy drinks completely;
- walk in the fresh air for at least an hour a day, preferably 2 hours;
- moderate physical activity: swimming in the pool, taking the stairs instead of the elevator, skiing or jogging in the park. This is especially true for people with sedentary jobs.
Supraventricular (supraventricular) extrasystole occurs in people of any age. Mild cases do not require treatment.
More serious ones may be accompanied by heart and other diseases and require drug therapy, and in extreme cases, surgical treatment. The main thing with this disease is to remain calm and lead a healthy lifestyle.
Who has it?
Supraventricular extrasystole (SE) occurs in 60-70% of people
. Normally, it can also occur in clinically healthy patients.
The presence of supraventricular extrasystole (SVES) does not mean that a person is sick.
SE is more often recorded in adults and older children
, since young children are not yet able to describe their sensations and do not really understand what is happening to them.
In newborns and small children, supraventricular extrasystole is detected during an ECG
during medical examination, general examination or in connection with an alleged disturbance in the functioning of the heart (congenital defects, a sharp deterioration in the child’s condition in the absence of external factors).
What to do if you are diagnosed with supraventricular extrasystole?
Supraventricular extrasystole or otherwise supraventricular extrasystole is a pathology in which cardiac contraction in ectopic foci can be observed ahead of schedule.
These lesions are localized either in the walls between the atria and ventricles of the heart, or in the atria. In this regard, additional defective heart contractions occur.
What does it represent?
According to the International Classification of Diseases (ICD-10), supraventricular extrasystole has code 149.4. It is included in the registry of cardiac arrhythmias in the heart diseases section.