Most diseases have the most difficult course and threaten the most severe consequences when they appear in children.
Their body has not yet acquired the necessary resistance to disease, and identifying symptoms can be difficult.
Therefore, it is so important to monitor the child’s condition and pay attention to any warning signs. Further in the article there is very necessary and important information about what are the symptoms and treatment of heart failure in children.
Causes of development and risk factors
The causes of the disease are almost the same in children of different ages:
- congenital heart defects;
- previous trauma, heart surgery or serious infectious disease;
- myocarditis;
- diseases of the lungs, kidneys, rheumatism;
- other heart and vascular diseases.
The likelihood of illness is especially high in the following cases:
- the child has poor heredity (one or both parents had heart problems);
- the baby has ischemic disease;
- the child suffers from chronic arrhythmia or hypertension.
Classification: degree of disease
In children and adults, there are two stages of heart failure - chronic and acute . The second is a complication and is associated with a sharp increase in symptoms, in which the pathology can no longer be ignored.
The disease is diastolic and systolic.
In the first case, problems arise with filling the heart with blood, in the second - with a decrease in its contractility and insufficient blood ejection.
Heart failure is also divided into left ventricular, or cardiopulmonary, in which the lungs, which are part of the pulmonary circulation, are affected, and right ventricular, which affects the liver and kidneys. Cough and difficulty breathing are characteristic of the first type, swelling and problems with the spleen are characteristic of the second .
There are four stages of the disease:
- In the first stage, the symptoms remain almost unnoticeable, physical activity causes significant fatigue and shortness of breath, and the child tries to avoid active games.
- At the second stage, the heartbeat accelerates, the rate of breathing increases in the left ventricular type, or the liver begins to protrude several centimeters from under the lower rib.
- The third stage is characterized by a heart rate accelerated up to one and a half times, shortness of breath, coughing and wheezing in the lungs or bulging of the liver along with a noticeable enlargement of the neck veins.
- The worst symptoms of stage four are pulmonary edema or general swelling of the body, depending on the type of disease.
Possible reasons
Serious diseases of the cardiovascular and respiratory systems can lead to the development of heart failure.
The development of this disease can be influenced by many factors, which may differ depending on the age of the child.
- In newborns and babies in the first months of life, the disease usually manifests itself as a result of the presence of congenital heart disease or myocarditis, accompanied by cardiac failure, pneumonia or sepsis.
- Children from one to three years of age may develop deficiency after suffering from subacute myocarditis.
- Common causes of this disease include:
- genetic predisposition;
- inflammation of the myocardium of an infectious nature, carditis;
- suffering from severe pulmonary pathology;
- serious attacks of bronchial asthma;
- acute hypoxia;
- pathologies of the respiratory system;
- severe arrhythmia;
- anemia;
- acute neuritis;
- the presence of neuromuscular pathologies;
- pathological process in connective tissue;
- tumor of the valve apparatus or located in the heart area;
- presence of vasculitis;
- heart defect (congenital or acquired);
- electrolyte deficiency;
- serious overload of the heart muscle as a result of excessive physical activity;
- previous trauma to the thoracic region;
- surgery on the heart muscle;
- the presence of kidney or vascular diseases;
- persistent hypertension;
- cardiac ischemia;
- consequence of excessive infusion therapy.
Signs
Signs to identify the disease depend on age. It is characteristic that in the early stages it is almost impossible to identify them, much less associate them with heart failure. They are not noticeable from the outside and do not distract the child’s attention. However, gradually the symptoms manifest themselves more and more and become a constant factor that greatly reduces the quality of life. In infants the disease is said to be:
- anxiety;
- tearfulness;
- uneven breathing;
- sweating;
- rapid loss of interest in the breast during feeding;
- regurgitation;
- restless sleep.
Detection of the disease becomes easier with age. Attracts parents' attention:
- unusually low mobility, spending a lot of time sitting or lying down;
- shortness of breath, which not only appears during physical activity, but also becomes a constant companion over time;
- cough and wheezing;
- dizziness;
- painful sensations behind the sternum;
- pale skin;
- fainting;
- bluishness of lips or fingers;
- easy fatigue;
- darkening in the eyes, black spots in front of them;
- disturbances in the functioning of the stomach and intestines, nausea and vomiting;
- swelling of the neck veins and swelling of the lower half of the body are possible - signs of late stage heart failure.
A number of these symptoms individually can be attributed to a common cold or other illness.
However, several signs at the same time can indicate the seriousness of the situation, and if heart failure is suspected, one should not hesitate. In children, the disease is treated exclusively in a hospital setting , and the faster the doctor examines the child, the higher the chances of successful treatment without complications.
The appearance of alarming signals: which doctor to contact
Often, parents turn to a pediatrician or ENT specialist because of cough and shortness of breath, and the real cause of the problem is revealed in the doctor’s office.
Another option is to self-identify symptoms and contact your pediatrician.
In any case, the child must ultimately see a cardiologist, who will confirm or rule out the disease.
Heart failure can also be noticed during examination by other specialists using the following diagnostic methods:
- Manual examination, or auscultation, when the doctor feels the patient's abdominal cavity. This method allows you to identify an increase in internal organs suffering from disease.
- Measuring blood pressure and heart rate.
- Chest X-ray, which may reveal that the heart is too large or fluid has accumulated in the lungs.
- ECG, echocardiography or tomography.
- Taking a blood test.
Diagnostics: how to recognize by deviations in examination results
A cardiologist is responsible for clarifying the diagnosis, stage of heart failure and prescribing treatment. Required examination methods include:
- ECG;
- EchoCG;
- tomography;
- chest x-ray;
- blood analysis;
- daily wearing of a Doppler monitor that takes a cardiogram and shows the full picture of heart contractions.
As a result, the doctor determines the degree of damage to the heart, its increase in size, and the condition of the lungs, kidneys and liver.
Watch the video in which a pediatric cardiologist will talk about heart diseases:
Classification of pathology
The disease is classified as follows:
| Classification | Form | |
| By localization | left ventricular | right ventricular |
| According to the form of flow | acute | chronic |
| By degree of compensation | compensated | decompensated |
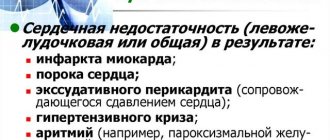
Left ventricular heart failure occurs against the background of a heart attack, ischemia of the heart muscle, stenosis of the aortic and mitral valve. It implies stagnation of blood in the pulmonary circulation.
Right ventricular failure - stagnation of blood in the large circulating circle. The prerequisite for its occurrence is left ventricular failure, diseases of the heart, lungs and their blood vessels.
The chronic form is characterized by a slow development of the disease, while the acute form has pronounced symptoms and a rapid course.
In the compensated form, the patient feels the symptoms of the disease during physical activity and immediately after it, and in the decompensated form, they bother him even at rest.
Treatment
The effectiveness and timing of getting rid of the disease depend on the timely detection of the problem. A mandatory companion to drug therapy is bed rest , which eliminates stress on the heart.
If it is necessary to call an ambulance, peace must be ensured by bringing the child into a semi-lying state, creating a comfortable place with the help of several pillows and blankets. Infants may require tube feeding and sedation.
Therapy is carried out in the following areas:
- Stimulating the ability of the heart muscle to contract: for this, the patient is given cardiac glycosides (for example, digoxin).
The medicine begins to be administered in the form of intravenous injections, eventually switching to tablets. - Reducing cardiac stress: taking diuretics (for example, uregitis) allows you to get rid of swelling of the body and internal organs.
- ACE inhibitors act with the first two groups of drugs, allowing them to gradually reduce their dosages while maintaining a high effect.
- Beta blockers perform similar functions.
- At the same time, concomitant diseases are treated and other affected organs are treated.
The entire course of treatment takes place in an inpatient setting. It is unnecessary to remind that taking medications must strictly comply with the instructions of the attending physician and be supervised by him.
A good additional treatment ( precisely additional! ) is traditional medicine.
The use of jaundice, medicinal asparagus, vitamin infusions (from rose hips or rowan, for example) will supply the body with the nutrients necessary to fight the disease.
Emergency care for acute cardiovascular failure
Acute cardiovascular failure as an independent syndrome is rare. In most cases, it develops as a concomitant syndrome against the background of toxic or toxic-septic pneumonia, toxic dyspepsia and other infectious diseases.
In recent years, a new concept has been introduced - low output syndrome, which denotes a decrease in cardiac output regardless of the cause that caused it.
Cardiovascular failure resulting from small output syndrome may be caused by a sudden deterioration in myocardial contractility; decrease in blood volume; decreased vascular tone.
The most common cause of acute deterioration in myocardial contractility in childhood is parenchymal myocarditis (sepsis, diphtheria, viral infection), congenital heart defects in the adaptation phase, the result of large doses of anesthetic (fluorotane, barbiturates), poisoning with certain poisons, uremia. With these diseases and conditions, damage to the myocardial parenchyma occurs (necrobiosis, necrosis of muscle fibers, dystrophic changes). In addition, plethora and stromal edema develop. In cases of acutely developed decline in myocardial contractility, the vascular reaction can be compensatory (vasoconstriction), which can ultimately lead to centralization of the blood circulation.
With a sudden decrease in blood volume (acute blood loss, toxicosis with exicosis), small output syndrome develops due to venous return.
A sudden decrease in vascular tone (anaphylactic reaction, anaphylactic shock, fainting) leads to redistribution of blood in the vascular bed and a sharp decrease in venous return.
Circulatory failure can also develop against the background of an increased stroke volume of blood, with the transfusion of an inadequate amount of aqueous-salt solutions, blood substitutes and blood,
Clinic. Acute left ventricular failure is characterized by shortness of breath, tachycardia, cyanosis and circulatory hypoxia. Stagnation in the pulmonary circulation and increased hydrostatic pressure in the pulmonary veins lead to hypoxia, the development of cardiac asthma and pulmonary edema, that is, acute left ventricular failure is accompanied by acute respiratory failure (sweating of the liquid part of the blood into the alveoli, impaired ventilation of the lungs).
Treatment. To improve myocardial contractility, fast-acting cardiac glycosides (corglicon, strophanthin) are prescribed. Administered in 2-3 doses over 24-36 hours, in addition, cocarboxylase is prescribed.
For pulmonary edema accompanied by increased blood pressure, cardiac glycosides are not indicated. In this case, it is necessary to administer 5% pentamine intravenously (from 0.5 to 1.5 mg/kg, which corresponds to 0.1-0.3 ml of solution, slowly in a 40% glucose solution under blood pressure control) to increase the volume of the vascular bed .
Free passage of the airways (suction of mucus) can be ensured with the help of anti-foam therapy (inhalation of oxygen passed through alcohol, inhalation of 10% antifomsilane for 10-15 minutes). The use of a defoamer is necessary due to the fact that the protein that has penetrated into the alveoli foams all the liquid there. Oxygen therapy with alcohol vapor or an antifoam agent should be used for a long time. It is carried out through nasal catheters with the patient in a semi-sitting position. It is necessary to reduce the blood supply to the vessels of the lungs by applying loose tourniquets to the legs to retain venous blood. Bleeding up to 50-75 ml is rarely performed in older children, since this removes a large number of red blood cells.
To reduce the volume of circulating blood, a 1% solution of Lasix 10-40 mg should be prescribed intramuscularly or intravenously. The use of aminophylline to improve blood circulation in the lungs is justified.
In order to maintain adrenal function, intramuscular or intravenous administration of prednisolone (15-30 mg) is indicated.
Reducing vascular permeability can be achieved by administering calcium, ascorbic acid and rutin, as well as antihistamines: diprazine intravenously or intramuscularly, diphenhydramine, suprastin. The use of these drugs is justified in case of hypoxic excitation, since they have a sedative effect. Prescribing promedol is dangerous because it can cause blockage of the respiratory center.
The acid-base state must be corrected. A 10-20% glucose solution with a 3% potassium chloride solution and insulin is prescribed intravenously. A 10% solution of albumin or concentrated plasma is also administered intravenously.
In the terminal stage of pulmonary edema, the patient is transferred to controlled breathing and the subclavian vein is punctured, through which infusion therapy is administered and central venous pressure is measured.
Acute left ventricular failure is accompanied by a syndrome of centralization of blood circulation (vasoconstriction of peripheral vessels of compensatory origin). As a result, peripheral resistance increases, which increases the load on the left ventricle. In the presence of circulatory centralization syndrome, catecholamines should not be administered. To relieve spasm of peripheral vessels, a number of drugs are used (see, “Neurotoxicosis”),
In case of acute right ventricular failure, to improve the contractile function of the myocardium and relieve the systemic circulation, cardiac glycosides, diuretics, aminophylline, cocarboxylase, and potassium preparations should be prescribed.
In case of total failure, it is necessary to apply the entire above set of measures.
Acute vascular insufficiency can be clinically manifested by fainting and collapse.
Fainting is a short-term loss of consciousness caused by acute anemia of the brain, resulting from a psychogenic or reflex effect on the regulation of blood circulation. In case of fainting, it is necessary to place the child without a pillow with his legs elevated, give access to fresh air, and free the neck and chest from clothing. Moisten your face and chest with cold water, bring a swab moistened with an ammonia solution to your nose. If these measures are not effective, one of the drugs should be administered subcutaneously: caffeine, ephedrine or cordiamine in an age-specific dosage.
Collapse is an acutely developing circulatory disorder, primarily manifested by a disorder of extracardiac circulation as a result of damage to the vasomotor center and heart failure secondary to this. The latter is due to the fact that small output syndrome during collapse develops due to insufficient venous return.
The basis of the collapse is the discrepancy (excess) between the volume of the vascular bed and the volume of circulating blood due to deposition and exclusion from circulation.
The most reliable differential diagnostic criterion for acute cardiac and acute vascular failure is the study of central venous pressure. A decrease in it indicates a decrease in the volume of blood flowing to the heart, that is, vascular insufficiency, and an increase indicates blood stagnation, that is, heart failure (Table 22).
The capacities of the vascular bed and the bcc are in strict accordance. Hypovolemia can be absolute (blood loss, exicosis) or relative due to expansion of the vascular bed (shock). Compensation for hypovolemia occurs as a result of the release of previously deposited blood, spasm of peripheral vessels and the development of circulatory centralization syndrome. Thanks to spasm of peripheral vessels, liver and kidney vessels, sufficient blood supply to the brain and heart muscle is ensured. However, with prolonged spasm of the blood vessels of the liver and kidneys, renal and liver failure may subsequently develop. In addition, it is known that blood from arterioles to venules can flow, bypassing the capillary, through the so-called arteriovenous shunt. The wall of the latter is impermeable to oxygen, as a result of which under-oxidized products accumulate (oxygen-free breakdown of carbohydrates) and metabolic acidosis develops.
Normalization of impaired blood circulation is impossible without restoration of peripheral circulation.
To treat acute vascular insufficiency, the following is necessary:
- restore the volume of circulating blood through intravenous infusion of a 5-10% solution of albumin (5-7 ml/kg), polyglucin (5-10 ml/kg), gelatinol {5-10 ml/kg), plasma (5-10 ml/kg );
- normalize cell metabolism and acid-base status.
In case of severe intoxication, to improve microcirculation and detoxification, it is necessary to prescribe low molecular weight hemodez, neocompensan (5-10 ml/kg), low molecular weight polyvinol (10 ml/kg), 10% albumin (3-5 ml/kg).
All these colloidal solutions should be administered slowly, dropwise, no more than 50-100 ml at a time. Only after this, glucose-saline solutions are introduced;
- restore the regulation of vascular tone, taking into account various types of collapse.
In case of sympathotonic collapse, the use of pressor amines (adrenaline, norepinephrine, mesatone), as well as cordiamine and corazol, is contraindicated, since they intensify the vascular spasm already present in this type of collapse. To relieve spasm of peripheral vessels, a number of drugs are used (see “Neurotoxicosis”); for paralytic and vagotonic collapse, pressor amines are indicated: 1% solution of mezaton (0.1 ml per 1 year of life), 0.2% solution of norepinephrine (0.1 -0.3 ml depending on age per 100-200 ml of 5% glucose, intravenous drip), adrenaline, cordiamine, ephedrine, caffeine in age-specific dosages.
In addition, strychnine is used subcutaneously (0.1% solution 0.1-0.15 ml 1-2 times a day). It increases the tone of the vasomotor center and narrows the vessels of the abdominal cavity. Contraindications to the use of pressor amines are left ventricular failure and hypertension in the pulmonary circulation.
Due to secondary developing heart failure in a collaptoid state, the use of fast-acting cardiac glycosides is indicated: corglycone or strophanthin, cocarboxylase and potassium preparations.
In the complex treatment of all types of vascular insufficiency, glucocorticoids are used (prednisolone 1-2 mg/kg body weight intravenously in a 20% glucose solution), oxygen therapy and sodium bicarbonate solution to combat acidosis.
Severe forms of cardiac arrhythmia, resulting from a sharp decrease in blood flow through the coronary vessels, can cause acute heart failure, the treatment of which, in addition to the above, should include additional measures.
The most severe forms of cardiac arrhythmia: an attack of paroxysmal tachycardia, atrial fibrillation and Morgagni-Edams-Stokes attacks.
Atrial fibrillation . Persons suffering from the tachyarrhythmic form of atrial fibrillation need emergency care. The latter contributes to the development of hypodiastolic heart failure. The main medications for stopping atrial fibrillation are digitalis preparations. The higher the ventricular rate, the more severe the degree of heart failure and the shorter the duration of atrial fibrillation, the faster digitalization is necessary. In these cases, a rapid rate of saturation with drugs such as isolanide and digoxin is usually used. For chronic atrial fibrillation, digitalization is usually administered orally at a moderately fast saturation rate. In this case, digitoxin may be the drug of choice. Regardless of the saturation method, immediately after receiving a positive therapeutic effect from glycosides, they switch to long-term treatment with these drugs in maintenance doses.
To eliminate tachyarrhythmia, antiarrhythmic drugs are used simultaneously with cardiac glycosides. They are prescribed against the background of preliminary digitalization, which neutralizes the negative inotropic effect of most antiarrhythmic drugs. Among antiarrhythmic drugs for this rhythm disorder, β-blockers are the most effective. In emergency cases, p-blockers (Inderal, Trazicor) are administered intravenously, then orally.
To relieve paroxysmal fibrillation, isoptin is used (see “Paroxysmal tachycardia”). Often the therapeutic effect is achieved by the simultaneous administration of cardiac glycosides, β-blockers and isoptin.
The use of other antiarrhythmic drugs depends on individual sensitivity to certain drugs.
Emergency care for Morgagni-Edams-Stokes syndrome should be aimed at improving atrioventricular conduction and increasing the electrical activity of the second-order pacemaker. In emergency cases, an intravenous drip infusion of sympathomimetic drugs is first performed: isoprenaline (norepinephrine 1-2 mg) or alupent (10-20 mg in an isotonic glucose solution). The rate of administration is 10-12 drops per minute under ECG control. Drugs with similar effects (novodrine, isadrine, ephedrine, etc.) can also be used. At the same time, it is advisable to carry out treatment with a 0.1% solution of atropine sulfate.
The administration of large doses of corticosteroids, such as hydrocortisone (up to 200 mg, then 100 mg 3-4 times a day for 1 week) or prednisolone (2-3 mg/kg), is indicated. They have an anti-inflammatory effect and eliminate electrolyte disturbances in the myocardium.
In addition to medications, indirect cardiac massage, mouth-to-mouth breathing, and cardiac stimulation are performed.
Paroxysmal tachycardia . An attack of paroxysmal tachycardia may be one of the causes of acute hemodynamic failure. It usually occurs suddenly and is characterized by a significant increase in heart rate. Along with this, energy deficiency of the myocardium is observed, and the efficiency of individual cardiac systoles decreases. First, the stroke and then the cardiac output decreases. The blood supply to organs and tissues is disrupted, the speed of blood flow slows down, and the phenomena of hypoxemia and hypoxia increase. The blood supply to the heart itself deteriorates, which aggravates changes in metabolic processes in the myocardium. Protracted and frequent attacks reduce the contractility of the heart, which entails the development of total circulatory failure.
The occurrence of paroxysmal tachycardia in children can be due to a number of reasons, both congenital and acquired. The first include heart defects, endocardial fibroelastosis, congenital pathology of the cardiac conduction system, etc.
The second group of reasons includes:
- violation of the regulatory effect on the heart of the autonomic nervous system;
- the occurrence of a focus of increased excitation in the conduction system of the heart or in the own myocardial tissue during inflammatory lesions of various etiologies, sclerosis, some endocrine diseases, drug intoxications (cardiac glycosides, sympathomimetic drugs, etc.);
- cardiotrophic changes due to viral or infectious diseases;
- reflex effect in inflammatory lesions of other organs (gallbladder, urinary tract, carious teeth).
To a large extent, the prognosis of paroxysmal tachycardia depends on the duration of the attack. In this regard, it is necessary to carry out a set of measures to facilitate the fastest possible relief of paroxysm. To relieve an attack, you should use drugs that act on the pathological focus in the myocardium, normalize the ratio of vegetative influences on the heart, or reduce myocardial excitability.
Treatment tactics depend primarily on the level of pathological impulses. Depending on the location of the focus of heterotopic impulses, supraventricular and ventricular forms of paroxysmal tachycardia are distinguished. Thus, in some cases, an attack can be interrupted using methods of reflexively increasing the tone of the vagus nerve. However, it should be remembered that in children under 3 years of age, as well as in cases of ventricular tachycardia, they are not effective.
In children over 3 years of age, as well as in the supraventricular form of paroxysmal tachycardia, when the attack is associated with neurovegetative disorders, the method of reflex increase in the tone of the vagus nerve can be used at the beginning of treatment:
- Aschner reflex, which occurs when pressure is applied to the inner corner of the eyeballs;
- carotid sinus reflex, which occurs when massaging the area at the site of the branching of the carotid artery or when cooling the sinus area, which is achieved by applying cotton wool soaked in ether to the site of its projection;
- the gag reflex is caused by irritation of the root of the tongue;
- Valsalva maneuver (straining).
Impaired cardiac excitability and paroxysmal tachycardia are usually accompanied by a shift in ionic ratios in the myocardium towards intracellular hypokalemia. Prescribing sufficient doses of potassium preparations reduces myocardial excitability. Improving the permeability of the cell membrane for potassium ions during an attack is facilitated by a polarizing mixture (5-10 ml of 10% glucose solution, the required amount of insulin and one of the potassium preparations - 3% or 7.5% potassium chloride solution, panangin). It is administered intravenously under mandatory ECG monitoring. The action of the mixture is based on the ability of insulin to accelerate the processes of repolarization of the cell membrane and promote the penetration of potassium ions into the cell.
It is advisable to combine intravenous administration of potassium chloride with oral administration of drugs. So a 10% solution of potassium chloride or acetate can be used, 1 teaspoon, dessert or tablespoon (depending on age) with an interval of 2 hours.
The drug has an irritating effect on the gastric mucosa, so it must be washed down with fruit juices.
From tableted potassium preparations, use panangin (potassium and magnesium aspartate) at 10 mg/kg or potassium orotate at the same dosage 3 times a day.
The main means of treating the supraventricular form of paroxysmal tachycardia include cardiac glycosides. Drugs in this group have a positive inotropic effect, that is, the ability to increase myocardial contractile function. At the same time, the stroke and minute volumes of the heart increase, coronary blood flow improves, and metabolic processes in the myocardium are normalized. After calculating the full saturation dose, a rapid type of digitalization is usually used for intravenous drip administration of the drug. In emergency cases, preference is given to fast-acting glycosides with a high elimination coefficient (0.05% strophanthin solution, 0.06% corglicon solution or 0.02% isolanide solution). After the attack has stopped, it is necessary to continue taking glycosides in a maintenance dose. In this case, drugs with a pronounced chronotropic effect and a moderate elimination coefficient (celanide, isolanide, acedoxin, digoxin or lantoside) can be used. It should be remembered that the sensitivity of the myocardium to cardiac glycosides varies significantly. For example, in acute myocarditis it is increased, so treatment with glycosides must be carried out with careful clinical and ECG monitoring, and the initial doses of drugs should be minimal.
Due to the increase by glycosides of the electrical activity of the ventricular myocardium and the likelihood of ventricular fibrillation in the ventricular form of paroxysmal tachycardia, their prescription should be determined only by the symptoms of rapidly increasing circulatory failure, as well as the lack of effect from the use of other anti-arrhythmic drugs.
In recent years, drugs belonging to the group of β-blockers have been successfully used to eliminate paroxysmal attacks. They have a negative chronotropic effect, suppress ectopic foci of excitation in the atria and ventricles, and have a coronary dilatator and hypotensive effect. The drugs can be prescribed parenterally and orally. Treatment should be carried out with mandatory ECG monitoring and blood pressure monitoring. Of the drugs in this group, Inderal (propranolol) can be used - in a dose of 0.5 to 2 mg/kg body weight per day. In some cases, its use may be accompanied by the development of undesirable phenomena, such as the occurrence of atrioventricular blockade up to complete hypotension, bronchospasm, and worsening circulatory failure. A “softer” β-blocker is Trazicor. It has basic (5-adrenergic blocking properties, but is well tolerated, low toxicity, minimal side effects. The dose of the drug for adults is 60-80 mg per day orally or intravenously. For children it is selected strictly individually: for younger children it is 10 mg per day day, after 3 years - up to 20 mg per day. For recurrent forms of paroxysmal tachycardia, in order to prevent an attack, the drug in the optimal dose can be used for a long time - 3 or more months.
Isoptin can be used to relieve attacks. The drug has β-adrenergic blocking and Ca-antagonistic effects. Prescribed intravenously in doses: newborns 0.3-0.4 ml; children under 1 year - 0.8 ml; 3-5 years -0.8-1.2 ml; 5-10 years—1.2-1.6 ml; 10-14 years - 1.6-2.0 ml of 0.25% solution. For recurrent forms of paroxysmal tachycardia, the drug is used orally for 1.5-2 months.
The use of ajmaline, one of the rauwolfia alkaloids, is based on its ability to have an adrenolytic effect. The drug is prescribed intravenously at a dose of 50 mg (2 ml of 2.5% solution) in isotonic sodium chloride solution or 5% glucose solution. The dose of the drug is selected individually under ECG monitoring. Inject slowly over 3-5 minutes. If necessary and in the absence of side effects, the initial dose of the drug can be repeated during the day. Aymalin is also administered intramuscularly at intervals of 8 hours. The maximum dose for adults is 150 mg. After achieving a therapeutic effect, you should continue taking the drug orally at a dose of 50-150 mg/day.
The antiarrhythmic effect of novocainamide lies in its ability to reduce myocardial excitability, increase the time of impulse conduction through the conductive tissue of the heart, and suppress ectopic foci of excitation in the myocardium. The drug is prescribed in an approximate dose of 0.2 ml/kg body weight (10% solution). Dissolve in isotonic sodium chloride solution or 5% glucose solution. Introduce slowly by drip. At the same time, blood pressure and conduction function are constantly monitored (using ECG). If there is no effect, you can re-administer the drug after 1-2 hours, slightly increasing the dose. Subsequently, to consolidate the therapeutic effect and to prevent repeated paroxysms, the drug can be administered intramuscularly or orally.
For the ventricular form of paroxysmal tachycardia, lidocaine in the form of a 1% or 2% solution can be used intravenously in a stream (slowly!) or drip. The average daily dose of the drug is 50-100 mg. If necessary, under ECG monitoring, it is increased to 200 mg.
To relieve ventricular paroxysm, cordarone can be used, which has antianginal and antiarrhythmic effects. The latter is due to the ability of the drug to cause partial blockade of α- and β-receptors. A distinctive feature of the drug is its slight cardiodepressive effect. The drug is administered intravenously during an attack at a dose of 5 mg/kg body weight. The rate of administration is from 30 s to 3 min. If necessary, it can be administered intravenously in an isotonic glucose solution. Subsequently, to prevent secondary attacks of arrhythmia, cordarone is used parenterally for 4-5 days, then in tablet form for 2-3 weeks.
Along with the above antiarrhythmic drugs, intravenous administration of cocarboxylase (50-100 mg) is indicated during an attack. The latter is involved in the decarboxylation of pyruvic and alpha-ketoglutaric acids, the accumulation of which in excess can cause the appearance of a focus of increased excitation in the myocardium and provoke a paroxysmal attack.
The complex of therapy must include ascorbic acid, sedatives, hypnotics, and, if necessary, anti-inflammatory drugs and diuretics.
All antiarrhythmic drugs are the method of choice and can be used in children from a very early age. In the absence of a therapeutic effect, electric pulse therapy is used (Table 23).
Diet and lifestyle
What diet should a child have for heart failure? Diet is one of the most important factors in rehabilitation and must comply with the doctor’s recommendations after discharge.
You need to eat a lot of fresh fruits and dairy products. Food should contain a significant amount of potassium and a small amount of salt in order to avoid swelling. It is recommended to salt food not at the cooking stage, but during serving.
Physical activity should be appropriate to the child’s condition.
For those with first-degree heart failure, aerobic exercise and walking (hiking in summer and skiing in winter) are recommended.
Usually they are exempted from physical education classes or transferred to a special group.
After a second degree illness, fast walking and running should be treated very carefully, and after the third degree, walking in a sitting position is preferable.
In any case, it is worth emphasizing the need for fresh air and staying outside for at least 2 hours a day.
Causes of heart failure in older children
Dilated cardiomyopathy
If symptoms indicate cardiac failure in an older child, the cause of its development may be:
- suffered a rheumatic attack,
- cardiomyopathy,
- hypertension in the pulmonary circulation, developing against the background of decompensation of pulmonary pathology (bronchial asthma, chronic obstruction) or pneumonia, tuberculosis,
- infective endocarditis,
- myocarditis,
- heart rhythm disturbances.
Prevention measures
Prevention measures will help you never encounter heart failure in your children (or insure against the return of the disease). It’s not difficult to follow them, but it will help make your child’s life healthy and his well-being consistently wonderful:
- Physical activity . Even moderate exercise (walking to school or taking the stairs instead of the elevator) significantly reduces the risk of heart failure.
- Proper nutrition . Eliminating excess salt, spices and fatty foods, coupled with sufficient minerals, vitamins and amino acids, is the key to health for many years.
- Body weight control .
Parents often do their offspring a disservice by making sure they are always well-fed. It is worth listening to your child when he declares he is full, and not accustoming him to excessive amounts of fatty foods, baked goods and sweets. - Rest . The number of educational tasks and additional clubs must be commensurate with the capabilities of the children. Also, don’t let them get into the habit of sacrificing sleep in favor of computer games.
- Stress is a strong risk factor , so eliminating nervous situations will have a positive effect on the health of the offspring.
What are the prognosis for the treatment of heart failure in children? In most cases, timely medical intervention and strict adherence to doctors’ recommendations can effectively relieve the symptoms of the disease.
Children who have suffered it are able to fully return to life without regard to heart problems and look forward to a happy future.
And in conclusion, there is a lot of useful information about cardiovascular failure (acute and chronic) and other heart diseases in children:
Causes of heart failure in early childhood
Chronic alcoholism of a woman
Heart failure is a condition of the cardiac muscle in which it is not properly able to contract and emit the amount of blood required by the body, resulting in stagnation of blood in the circulatory system, depletion of tissues and cells in oxygen, and hemodynamic disorders.
Heart failure in children can occur in newborns and young children, as well as in older children. In infants and children of the first years of life, symptoms of heart failure mainly develop due to congenital heart defects. Risk factors for the occurrence of defects in utero in babies are the following: genetic predisposition, medication taken by the mother during pregnancy, chronic alcoholism of the woman, diseases of the mother (endocrine disorders, systemic diseases, diabetes), as well as an early viral infection.
Severe cardiac congenital defects (transposition of the great vessels, valvular atresia, stenosis of the great vessels) can immediately after birth cause the clinical picture of acute heart failure in children: cyanosis of the skin increases, shortness of breath, increased anxiety, agitation, convulsions and loss of consciousness are possible. Without emergency surgical intervention in such cases, developing acute heart failure can lead to death.
Heart failure
With congenital defects that are less hemodynamically significant, the clinical course of heart failure in a child can proceed according to the following scenario:
- Adaptation stage. The baby’s body adapts to circulatory disorders due to pathological features in the development of the heart and blood vessels.
- Compensatory stage. If the adaptation stage is successfully completed, a stage of imaginary well-being may begin: by the age of 2-3 years the baby’s condition supposedly improves. In fact, a decrease in the clinical manifestations of heart failure occurs due to an increase in the volume of the heart, because he was under too much pressure. And the myocardium, like any muscle, hypertrophied.
- Terminal stage. It comes after the stage of compensation, since any compensatory possibilities are not unlimited. Hypertrophic changes in the child’s myocardium are replaced by dystrophic ones, cardiosclerosis develops, and blood flow through the coronary arteries decreases. The little patient's condition deteriorates sharply, cardiac decompensation occurs, and chronic heart failure becomes acute. Without specialized medical care, decompensation of heart failure is dangerous due to its complications: pulmonary edema, cardiogenic shock, severe arrhythmias, which can become a threat to the baby’s life.