Cardiovascular diseases can be complicated by heart failure and require a very rapid response. Therefore, it is important, if there are risks of complications, to know what emergency care for acute heart failure is and what steps should be taken to prevent the death of the patient.
Acute left ventricular failure (ALF) is an emergency condition in which the left ventricle undergoes disproportionate strain due to hypertension, coronary artery disease, or valve disease. In such cases, ALV is considered a complication.
The development of acute left ventricular failure is associated with a high risk of death, in particular, some authors indicate that out of 250 patients, 59 died within the first six months, and another 69 within the next two years (Palmer, RS, and White, PD; Clinical significance of cardiac asthma. JAMA 92:431 (Feb. 9) 1929).
There is often very little time left to assess the patient’s condition, so it is important not only to provide emergency care for acute left ventricular failure step by step, but also to determine the symptoms of the disease.
Video: Left ventricular failure. How to treat left ventricular failure
Emergency care for acute cardiovascular failure
Content
Nursing process in acute cardiovascular failure plays an important role in treatment. It is the nurse who ensures that medical instructions are followed accurately.
Acute cardiovascular failure is manifested by a decrease in the contractility of the heart muscle (myocardium). This leads to circulatory problems in the heart and lungs, most often resulting in the death of the patient.
The main causes of the development of pathology are myocardial infarction and coronary heart disease. Arterial hypertension can also cause heart failure. The disease can affect not only older people, but also newborns. A common consequence of the disease is death, so the first signs should be the reason to consult a doctor.
Hypokinetic variant of acute left ventricular failure
In order to increase myocardial contractility, fast-acting drugs with a short half-life (sympathomimetics) are used. Of these, the most commonly used are dobutamine [2-5 mcg/kgmin) and dopamine [3-10 mcg/kgmin)].
For decompensated heart failure, cardiac glycosides are prescribed (strophantine at a dose of 0.01 mg/kg or digoxin at a dose of 0.025 mg/kg intravenously slowly or drip). The use of cardiac glycosides is most justified in children with tachysystolic form of atrial fibrillation or flutter.
Against the background of normal or elevated blood pressure, ganglion blockers should be administered (azamethonium bromide at a dose of 2-3 mg/kg, hexamethonium benzosulfonate - 1-2 mg/kg, arfonade - 2-3 mg/kg). They promote the redistribution of blood from the small circle to the large circle (“bloodless bloodletting”).
They are administered intravenously by drip under the control of blood pressure, which should decrease by no more than 20-25%. In addition, with this option, the administration of a 0.25% solution of droperidol (0.1-0.25 mg/kg) intravenously, as well as nitroglycerin and sodium nitroprusside, is indicated.
Urgent Care
HF is one of the leading causes of death in older people. After 60 years, common causes of pathology are diabetes mellitus combined with hypertension. Some causes of the disease are irreversible. Signs of the disease are the same in children and adults.
First aid for acute heart failure consists of the following actions:
- Call medical professionals.
- Provide access to fresh air.
- Place the patient in a sitting position.
- To reduce blood flow to the heart, tourniquets must be applied to the arms and legs without interfering with arterial blood flow.
- Immerse your feet in hot water.
- If these measures do not bring relief, emergency care should consist of chest compressions and artificial respiration.
If emergency care is provided incorrectly or not quite on time, the consequence will be the death of the patient.
Emergency care for acute heart failure in children is aimed at eliminating the cause of deterioration in well-being.
For children, the following action plan is followed:
- Reduces strain on the heart.
- Reduces pressure in blood vessels.
- Reduce the permeability of alveolar-capillary membranes.
- Strengthens myocardial contractility. For this purpose, glucosides are prescribed.
- Improves metabolic metabolism in the myocardium.
After stabilization of the condition, diuretics are used to treat children; in the presence of edema, cardiotrophic drugs are used. The first aid process must be carried out very quickly to avoid death. Smaller doses of drugs are used to treat children than for adults.
Description of the pathology
Cardiac asthma is formed according to the following pathogenetic mechanism:
- Increased hydrostatic pressure in the pulmonary capillaries. It occurs when these small vessels overflow with blood. This process is accompanied by exudation of plasma through small endothelial pores into the interstitium.
Hypervolemia. In the medical literature it is also called overhydration. The term refers to fluid retention in the intercellular space.- An increase in the volume of blood that enters the pulmonary circulation. The latter passes through arteries, arterioles, capillaries, veins and venules throughout the lungs. Redistribution of blood volume occurs when the patient moves to a horizontal position.
- Violation of central regulation. In this case, the medulla oblongata, in which the vasomotor and respiratory centers are located, is affected.
- Increased workload on the heart due to excessive work of the main and auxiliary respiratory muscles. Trying to capture more air, the patient performs a forced inhalation, which increases the blood supply to the lungs.
- Acidosis. Due to hypoxia, under-oxidized metabolic products accumulate and the body becomes intoxicated.
Nursing care for heart failure
The nursing process involves the nurse providing care to the patient. The nurse receives information about the doctor's orders and ensures that the patient strictly adheres to them.
Today the nursing process consists of the following steps:
- Nursing examination and diagnosis.
- Setting goals and planning the scope of actions.
The nursing process begins with an examination of the patient.
The nurse should do the following:
- Assess the patient's condition and identify the causes of the disease.
- Measure body temperature and analyze breathing status.
- Determine heart rate and measure blood pressure.
- Check the patient's ability to satisfy his natural needs.
- Find out if the patient uses any medical equipment.
- It is also necessary to measure the patient's height, weight and chest volume.
The nursing process at the diagnostic stage consists of observation and conversation with the person. Nursing care consists of facilitating the patient’s external reaction to the disease.
The nurse must be concerned not only about the patient's current problems, but also to identify signs of possible worsening of the disease.
The nursing process after examination and diagnosis consists of drawing up a schedule of proper care that will protect the patient from conditions that complicate the course of the disease.
The nurse's help can be:
Short-term assistance is provided over several weeks, and long-term assistance includes training in prevention, adaptation of the patient to society, and prevention of exacerbations of the disease.
After drawing up a plan for the process, the nurse must coordinate her actions with the patient, and when treating children, with the parents. She must obtain the support and consent of the patient.
The nursing process consists of independent, dependent and interdependent actions:
- In the first case, help consists of measuring pulse, temperature and pressure. The nurse carries out these procedures for her own reasons to monitor the patient's condition.
- The nurse provides dependent care under the supervision of a physician, for example, administering injections, conducting laboratory or instrumental tests.
- Interdependent care is when a nurse works together with a doctor. For example, assisting during operations.
If the nursing process does not produce the desired result, then the action plan is reviewed and adjustments are made. The nurse's assistance should satisfy the basic requirements of the patient's body, maintain and restore the patient's independence in self-care.
The nurse must teach the patient or parents (when treating children) the principles of proper nutrition. It is also necessary to monitor medication intake and create a physical activity regimen.
It is necessary to teach the patient to observe the rules of personal hygiene independently.
To relieve some symptoms and improve the patient's condition, the nurse performs the following actions:
- Helps the patient get into a comfortable position that will reduce symptoms such as shortness of breath and heart palpitations.
- Ensures that the patient adheres to the doctor's instructions.
- Monitors the patient's breathing and pulse. If symptoms such as a slow pulse or an overdose of glycosides occur in a patient, this should be reported to the doctor.
- Provides oxygen therapy.
- Monitors whether symptoms such as swelling and blueness of the skin occur.
- To alleviate the unpleasant symptoms of the disease, the nurse recommends that the patient wear loose clothing, without tight elastic bands.
- If necessary, controls the amount of fluid drunk and urine excreted per day.
- There are psychological signs of the disease. The patient begins to feel that he will soon die, and depression may develop. Therefore, the nurse tries to reassure the person and increase his confidence in improving his health.
- The nurse tells the patient about the side effects of prescribed medications and how to take them. Controls their reception.
- If necessary, gives a cleansing enema.
- Ventilate the room before going to bed.
- Make sure that your last meal is no later than 3-4 hours before bedtime.
- Teaches the patient's relatives to measure blood pressure and pulse, give an enema and prevent bedsores, constipation and pneumonia.
Taking into account the responsibilities of a nurse, we can conclude that the nursing process significantly alleviates the patient’s condition, eliminates the manifestations of pathologies and helps the patient adapt to society after recovery. Proper care can avoid consequences such as sudden death.
In the treatment of children and adults from acute cardiovascular failure, the nursing process plays an important role. The care and support of nurses can significantly improve the patient’s well-being and delay death.
LECTURE 9 (2 HOURS) NURSING PROCESS IN HEART FAILURE
THE STUDENT SHOULD KNOW:
! definition of the concept of “heart failure” (HF), “left ventricular failure”, “right ventricular failure”;
! medical and social significance and etiology of HF;
! main clinical symptoms of heart failure; classification of heart failure by stages and functional classes; principles of diagnosis and treatment of heart failure; medications for the treatment of heart failure; typical problems of patients with heart failure; general approaches to the prevention of heart failure, prognosis
BASIC CONCEPTS AND TERMS
Secondary pulmonary hypertension
- increased pressure in the pulmonary artery, observed with mitral valve defects and left ventricular failure.
Hepatomegaly
- pathological increase in liver size.
Cardiopathy
- a myocardial disease of unknown origin, characterized by an increase in heart size and progression of heart failure. With dilated cardiomyopathy, significant expansion of all cavities of the heart, a decrease in its contractility and heart failure are observed.
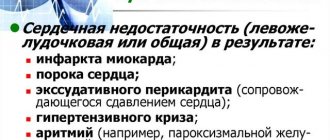
Causes of heart failure
1. In order to eliminate dehydration, administer a hypotonic 0.45% sodium chloride solution intravenously.
2. Start insulin therapy against the background of rehydration. Administration of sodium bicarbonate is not indicated.
3. Symptomatic therapy.
1. Prescribe insulin therapy.
2. To eliminate acidosis, introduce a 4% solution of sodium bicarbonate (2.5 ml/kg intravenously).
3. Symptomatic therapy (antibiotics, cardiac glycosides, vitamins B and C)
Emergency care for acute cardiovascular failure
Content
Nursing process in acute cardiovascular failure plays an important role in treatment. It is the nurse who ensures that medical instructions are followed accurately.
Acute cardiovascular failure is manifested by a decrease in the contractility of the heart muscle (myocardium). This leads to circulatory problems in the heart and lungs, most often resulting in the death of the patient.
The main causes of the development of pathology are myocardial infarction and coronary heart disease. Arterial hypertension can also cause heart failure. The disease can affect not only older people, but also newborns. A common consequence of the disease is death, so the first signs should be the reason to consult a doctor.