Even with proper medical treatment, mortality from heart failure remains high. Most clinical trials did not include patients with severe or end-stage heart failure (stage D). These patients are often indicated for heart transplantation.
However, in 2001 in the United States, 40,000 patients were on the waiting list for heart transplantation, while only 2,102 were performed. Alternatives to heart transplantation are needed to close this gap. Many surgical interventions are being developed to at least improve the condition of patients and allow them to survive until heart transplantation. Improvements in cardiac surgery and a better understanding of the changes that occur in heart failure have led to the proliferation of several new surgical treatment methods. However, there is still insufficient data on the safety and effectiveness of many methods. This article discusses elective operations for heart failure (myocardial revascularization, mitral valve surgery, cardiomyoplasty, geometric reconstruction of the left ventricle - Dora operation) and emergency circulatory support measures (up to a total artificial heart). Surgical interventions must be accompanied by active drug treatment. Coronary artery bypass grafting for ischemic cardiomyopathy. Mitral valve surgeries Reconstructive surgeries on the left ventricle Assisted circulation
Indications for heart transplantation.
Recipients are patients with end-stage heart failure who are not eligible for drug therapy or alternative surgical treatments for heart failure. Prognosis of one-year survival without transplantation <50%. Objective criteria for such a prognosis are: LVEF < 20%, serum Na < 135 mEq/L, pulmonary artery wedge pressure > 25 mm Hg, plasma norepinephrine level > 600 pkg/ml, cardiothoracic index > 0.6, decrease in VO2 max < 10 ml/kg/min. against the background of maximum medical support. The initial examination of the recipient includes a thorough analysis of the medical history and objective examination: chest x-ray, stress test for maximum oxygen consumption (VO2), routine hematological and biochemical tests, serological testing for the presence of infectious diseases, determination of human lymphocyte antigen (HLA). Carrying out cardiac catheterization with tonometry of the right heart to exclude irreversible pulmonary hypertension before placing patients on the waiting list for heart transplantation is mandatory.
Assisted circulation
Assisted circulatory support is necessary in cases of severe hemodynamic impairment, when the prognosis without heart transplantation is extremely unfavorable. Assisted circulation helps keep a patient alive while waiting for a heart transplant. Assisted circulation includes intra-aortic balloon counterpulsation, extracorporeal membrane oxygenation, ventricular and biventricular permanent or pulsatile pumps (artificial ventricles), artificial heart. The choice of one or another method is determined by the expected duration of use, the reversibility of the cause of cardiogenic shock, the need to maintain the function of one left or both ventricles, as well as the patient’s physique. Circulatory support is usually used when, despite intensive drug treatment, hemodynamics remain unstable. Most often these are patients who need a heart transplant.
Systolic blood pressure is less than 75-80 mm Hg. Art. Cardiac index less than 1.5-1.8 l/min/m2. Blood oxygen saturation in mixed venous blood (SvO2) is less than 50%.
Circulatory support may be used short-term for cardiogenic shock in the following situations.
- After heart surgery
- For myocardial infarction
- For fulminant myocarditis
- When circulatory arrest occurs during cardiac surgery (survival rate in this case is low)
If it is expected that the pumping function of the heart will soon be restored, it is best to choose the least complex and traumatic method of assisted circulation. For small patients (with a body surface of less than 1.3 m2), only external devices with centrifugal pumps are suitable. If restoration of the pumping function of the heart is not expected, long-term implantable devices must be used.
Devices for short-term circulatory support
Extracorporeal membrane oxygenation
Extracorporeal membrane oxygenation is a method of extracorporeal circulation in which blood is sucked out by a centrifugal pump and enters a membrane oxygenator, where carbon dioxide is exchanged for oxygen. Blood is taken from the femoral vein and returned to the femoral artery. Extracorporeal membrane oxygenation requires systemic anticoagulant therapy and may cause significant damage to blood components. This method allows you to saturate the blood with oxygen in case of severe respiratory failure. In addition, the right ventricle is unloaded.
Category pump Hemopump
The Hemopump category pump can only be used for a few days. It, like the intra-aortic balloon pump, is inserted through a catheter in the femoral artery. However, unlike intra-aortic balloon counterpulsation, which only partially facilitates the work of the left ventricle, the catheter pump completely takes over it. The catheter is passed through the aortic valve into the left ventricle. The catheter with a diameter of 14, 21 or 24 F contains a permanent pump, the productivity of which reaches 3.5-5.7 l/min. Anticoagulant therapy, constant monitoring and bed rest are necessary. In addition, the catheter pump does not unload the right ventricle and cannot be used in cases of damage to the aorta and aortic valve. The most common complications are hemolysis and ventricular arrhythmias caused by contact of the catheter with the myocardium.
Centrifugal pumps
Centrifugal pumps are used extracorporeally. They are usually used to support both ventricles in patients with a body surface area of less than 1.3 m2. Typically, centrifugal pumps are combined with extracorporeal membrane oxygenation. The flow in these pumps is non-pulsating; it is formed by the rotation of impellers or funnel-shaped impellers. Blood is taken from the right atrium and returned to the aorta. Catheters are inserted through a sternotomy access; usually only the skin is sutured. The operation of the device requires constant monitoring; long-term use is not possible. Heparin therapy is required.
Pharmacological bridge to transplantation.
Patients with critical stage end-stage disease require treatment in the intensive care unit with infusional inotropic agents. In patients with insufficient effect of drug treatment, intra-aortic balloon counterpulsation is used. Mechanical bridge to transplantation. In potential recipients who remain hemodynamically unstable for 24-48 hours, a monoventricular bypass device, a biventricular bypass device, or a total artificial heart is used with maximum pharmacological support. The donor is screened in three stages. The first step is to collect accurate information regarding the patient's age, height, weight, gender, blood type and Rh factor, cause of death, laboratory data, including biochemical tests, and serological tests for infectious diseases (cytomegalovirus, hepatitis B and C). The second stage of screening includes further investigation in search of potential contraindications: ECG, chest radiography, arterial O2 saturation and echocardiography are assessed. The final stage of donor screening occurs during the organ retrieval operation: ventricular function, valvular or coronary pathology is assessed.
Diet
Treatment and preventive measures for heart failure begin with a diet, which should consist of high-calorie, easily digestible foods and contain virtually no salt (this food additive contributes to the spread of edema).
Drinking for such heart problems is also limited.
The most favorable regimen of food intake is fractional, but 5-7 times a day. The first food for heart failure is Brussels sprouts.
Eliminate strong tea, chocolate, coffee, and alcohol completely from your diet. It is also not recommended to eat spicy foods and smoked foods.
It is recommended to consume foods that contain large amounts of potassium:
- dried apricots, raisins, nuts,
- oat and buckwheat groats,
- baked jacket potatoes,
- peaches, bananas,
- veal meat.
The substance potassium is extremely necessary for patients who take diuretics.
Read on - first aid for heart failure. Algorithm of actions.
In this article you will learn what myocardial infarction is.
To explore treatments for cardiac arrhythmia, go here
Compatibility of donor and recipient.
Compatibility criteria are based on matching the ABO blood group and the patient’s body size. The donor's weight should be within 30% of his body weight. The recipient is screened for human lymphocyte antigen (HLA) titer. A positive cross-reaction is an absolute contraindication to transplantation. An increase in the number of reactive antibodies (PRA) of more than 10-15% indicates increased sensitivity of the recipient to alloantigens.
The Russian Scientific and Practical Center uses the classic N. Shumway technique for heart transplantation.
The successful and long-term results of orthotopic heart transplantation have made it the treatment of choice for patients who have failed medical treatment. However, the obvious limitations of transplantation, including the need for immunosuppression and the shortage of donor organs, do not allow this treatment method to be used in all patients. To solve this problem, the Republican Scientific and Practical Center widely uses alternative surgical methods for the treatment of heart failure.
3. How to prevent worsening of the condition in heart failure?
To prevent congestive heart failure from progressing, it is important to monitor your health very closely. Do not violate the recommended medication regimen. And you need to regularly visit your doctor to make sure that the disease is not developing. Fluid retention in the body is one of the symptoms of heart failure and is a reason to immediately consult a doctor. Dizziness, weakness, shortness of breath can also be signs of heart failure, and if these symptoms reappear during treatment, do not delay a visit to a specialist.
About our clinic Chistye Prudy metro station Medintercom page!
Myocardial revascularization.
Successful myocardial revascularization in patients with EF <30% can be performed with low in-hospital mortality. Ideal patients for myocardial revascularization are those with a good distal coronary bed, the presence of a sufficiently large volume of hibernating myocardium, and the absence of right ventricular failure. Diagnosis of viable myocardium using scintigraphy, which makes it possible to distinguish hibernating myocardium from a connective tissue scar, as well as stress echocardiography with dobutamine are mandatory tests for predicting the restoration of ventricular function in the postoperative period. In addition, in order to predict the outcome of the operation, a study of the level of brain natriuretic peptide (BNP) is carried out. A BNP level <400 pkg/ml is a favorable prognostic sign of surgical outcome.
Correction of artrioventricular valve insufficiency.
Functional insufficiency of atrioventricular valves is observed in almost all patients with ischemic or dilated cardiomyopathy. Ischemia leads to the development of direct dysfunction or rupture of the papillary muscles and the formation of mitral regurgitation. A decrease in the contractility of the LV myocardium causes dilatation of its cavity, distortion of the posterior papillary muscle and increases mitral regurgitation. Backward shunting of blood into the left atrium increases LV volume overload and further increases myocardial ischemia. A vicious circle arises, which can only be interrupted by restoring the obturator function of the mitral valve.
For this correction of mitral regurgitation, support rings with modified spatial geometry are used, which reduce the recurrence of mitral regurgitation in the long-term postoperative period.
Surgical remodeling of the left ventricle.
Pathological LV remodeling in patients with cardiomyopathy leads to an increase in ventricular volume and stress on the ventricular wall. After the LV becomes spherical, the orientation of the cardiomyocytes changes. At the same shortening fraction, the ejection fraction in the spherical ventricle decreases significantly. In the natural course of the disease, the 5-year survival rate for SILV < 100 ml/m2 is 85%, and for SILV > 100 ml/m2 - 53%. Thus, any intervention aimed at optimizing these relationships is justified, and a favorable prognosis for the patient is possible when the LVSI decreases < 90 ml/m2.
Folk remedies
In the treatment of the disease in question, folk remedies provide significant assistance, which, by the way, are prescribed to their patients by the most eminent cardiologists. We present several of the most effective recipes.
- Elecampane plant . The roots of the plant are dug up in late autumn or early spring. They need to be washed, dried and dried in the oven. Separately, prepare a decoction of oats - pour half a glass of grains in the husk with 600 grams of water and boil a little (2-3 minutes). After this, take a third of a glass of elecampane roots and pour in a pre-prepared decoction of oats. Boil the mixture and leave, strain, add 1-2 tbsp. natural honey. For two weeks, drink 100 grams three times a day.
- Ordinary bean pods will help with heart failure , for which you need fresh pods (2 tbsp) and 750 ml of water. Boil the pods brought to a boil for five minutes. You can also add hawthorn flowers, motherwort leaves, mint, and lemon balm to the water. Leave for 4 hours, strain. Use 4 tbsp. before bedtime.
- The following mixture of dried fruits in equal quantities is recommended: raisins, dried apricots, walnuts, prunes. Grind these dried fruits in a meat grinder, add a little honey and the juice of one lemon. Stir and eat 1 tbsp. in a day.
Operative technology.
Circular sutures running through the tissue at a depth of at least 5 millimeters are applied from the endocardium side with a step calculated based on echocardiographic data. An LV cone is formed with a pre-calculated end-diastolic volume.
After cardiac recovery, surgical LV remodeling is assessed using transesophageal echocardiography.
| before surgery | after operation |
Heart resynchronization.
Intra- and interventricular dyssynchrony, associated with intra- and interventricular conduction delay, is an essential component of the pathogenesis of severe chronic heart failure. In heart failure, intra- and interchamber interactions change. Normal physiological asynchrony between the interventricular septum (IVS) and the posterior wall of the LV (about 60 ms) increases and leads to LV dysfunction. Cardiac resynchronization allows you to change the degree of electromechanical asynchrony of the atria and ventricles. The criterion for predicting the success of cardiac synchronization is the initial prolongation of the QRS interval >130 ms. The most informative criterion is the assessment of the intraventricular mechanical delay of contraction - an increase in the initial intra- or interventricular mechanical asynchrony > 50 ms.
Treatment methods for CHF (chronic heart failure)
A syndrome with the manifestation of shortness of breath, moist rales in the lungs, fatigue, swelling, signs of tachycardia - CHF (chronic heart failure) - a consequence of a violation of the pumping function of the heart. The condition leads to a decrease in cardiac output, failure of the metabolism and hematopoietic system, and an imbalance between the neurohumoral and vasoconstrictor systems.
Symptoms begin to appear when the heart is stressed during heavy lifting or exercise, fluid retention in the body, and tissue perfusion while at rest.
Risk factors
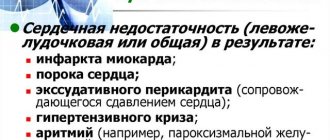
CHF is a consequence of complications of a number of vascular and heart diseases. It begins to manifest itself as the inability of the pumping system to function fully, disturbances in heart rhythm and normal blood circulation. Provoking factors:
- high blood pressure;
- hypertension;
- cardiac ischemia;
- myocarditis (congenital, acquired);
- heart disease;
- restrictive (hypertrophic) cardiomyopathy;
- pericarditis;
- ventricular tachycardia;
- atrial fibrillation;
- diseases not related to the heart: diabetes mellitus, thyrotoxicosis, alcoholism lead to damage to the myocardial muscle and massive cell death.
8
24/7
In chronic heart failure, the functional capacity of the heart decreases, leading to increased production of aldosterone, adrenaline, and angiotensin. The result is vascular spasms, a decrease in the volume of the vascular bed, and an increase in the body’s need for oxygen. Low levels of components provoke an increase in blood pressure, water and sodium retention in the body, excessive stress on the myocardium, damage and weakening of the heart. Compensatory mechanisms are sharply depleted.
Classification
According to WHO, chronic heart failure under the influence of hidden provoking factors has a staged course:
- The initial stage with the absence of obvious signs of impaired circulation. It is possible to detect hidden dysfunction in the left ventricle during echocardiography.
- The second stage is a disturbance of blood flow in one of the circulatory circles or hemodynamics in both circles. At the same time, the structure of the heart and blood channels are affected.
- The third stage is hemodynamics, accompanied by the occurrence of irreversible processes in the structures of the heart.
If we take into account functional modifications in the organ, then CHF is divided into 4 types.
- Type 1 - there are no obvious signs of pathology. There is the appearance of slight shortness of breath and heaviness in the heart area during intense sports activities.
- Type 2 - no signs at rest. At times, shortness of breath, fatigue, and increased rhythm appear.
- Type 3 - decreased heart activity. Symptoms appear at rest.
- Type 4 - symptoms become obvious and intensify even with minor physical activity. As it increases, cardiac discomfort, angina pectoris and heart failure become apparent.
To determine the degree of development of CHF, it is enough to walk at a brisk pace for up to 6 minutes. A mild degree will be observed when covering a distance of 420-560 m, a medium degree - 150-425 m, a severe degree of decompensation - less than 150 m.
Causes
In chronic heart failure, the heart's ability to pump the optimal amount of blood through the vessels is impaired. Causes:
- heart disease;
- arterial hypertension;
- ischemic disease;
- myocardial disease;
- cardiosclerosis against the background of proliferation of connective tissue.
The provoking factor of CHF in women is often arterial hypertension, in men - ischemic disease.
Symptoms
Heart failure can be recognized by the following clinical signs:
- increased heart rate;
- rapid fatigue when walking, at rest;
- increased heart rate per minute;
- shortness of breath with a feeling of lack of air;
- The cough is dry at the initial stage, then with sputum discharge.
8
24/7
CHF develops slowly and is more often diagnosed in old age. During the diagnosis, the following is revealed:
- tissue hypoxia;
- insufficiency of peripheral blood flow;
- insignificance of cardiac output;
- development of muscle weakness;
- swelling of the lungs;
- paroxysmal shortness of breath at night;
- signs of cardiac asthma against the background of emotional overexcitation, excessive physical effort during the daytime.
Symptoms appear in episodes. Patients develop a phobia or fear of falling asleep. In severe cases, attacks of cardiac asthma become prolonged and breathing becomes deep. Lung ventilation and respiratory ability are impaired.
Diagnostics
Before treatment of CHF, a diagnosis is carried out. It begins with the study of complaints and analysis of existing symptoms. It is based on instrumental examination methods to establish an accurate diagnosis and obtain objective results of the development of CHF:
- blood test for creatinine, urea, protein;
- X-ray shows the condition of the lungs if congestion is suspected;
- ECG to detect ischemia, myocardium, hypertrophy, concomitant arrhythmia, cardiac conduction disturbances;
- Holter 24-hour monitoring to clarify the condition of the heart muscle;
- ventriculography to assess ventricular contractility;
- electrocardiography to detect rhythmic changes, cardiac ischemia, myocardial hypertrophy.
It is important to identify the degree of heart failure, determine the etiology, assess the possible progression and risk of developing complications in CHF, and direct diagnosis and treatment to minimize unpleasant symptoms. Next, predict the degree of development of unpleasant consequences, confirm or refute pathological changes in the myocardium.
Treatment at different stages
For the treatment of CHF, clinical recommendations include a whole range of measures aimed at:
- reducing the load on the heart,
- helping myocardial functions,
- restoration of water-salt metabolism.
The volume of procedures in the treatment of CHF is directly related to the degree and stage of development of the disease. Patients are recommended:
- limit heavy lifting and physical activity;
- review your diet, eliminate animal products (hydrogenated fats);
- reduce salt intake;
- stop drinking alcoholic beverages.
Treatment of CHF in older people is long-term and complex: medications, diet therapy, cardiotonic methods. At an early stage, the main therapy is medication. Its goal is to improve the quality of life of patients, increase the function of cardiac contractility, and minimize unpleasant symptoms of the disease.
The high effectiveness of beta-blockers, ACE inhibitors of angiotensin-converting enzyme, and mineralocorticoid receptor antagonists has been proven.
The standard treatment for CHF is a combination of 4 drugs: a beta-blocker, a glycoside, a diuretic, and an ACE inhibitor. Main purposes:
- angiotensin beta receptors (ARB);
- anticoagulants to eliminate possible thrombus formation in blood vessels (Warfarin, Aspirin);
- B vitamins;
- nitrates to improve blood filling of the ventricles, dilation of the coronary arteries (Nitroglycerin, Sustak, Nitrong);
- ACE inhibitors to dilate veins, reduce vascular resistance, increase arterial tone (Captopril, Perindopril, Ramipril, Enalapril, Lisinopril);
- beta blockers to increase cardiac output, minimize heart rate (Carvedilol);
- active loop diuretics (Furosemide) for congestion while taking certain antagonists;
- beta blockers (Chlorthalidone, Hydrochlorothiazide, Indapamide).
Many drugs for decompensation and treatment of CHF have contraindications and side effects. Some relieve extremely unpleasant symptoms, but cannot have a positive effect on the life expectancy of patients. Others are less effective or their effectiveness has not been established at all. Still others can only worsen the course of the disease.
Among ARB drugs, the effectiveness of Candesartan has been proven; among beta-blockers with antiarrhythmic, antianginal, antihypertensive effects to reduce the intensity of heart contractions and minimize the frequency of repeated myocardial infarctions - highly selective drugs (Nebivolol, Bisoprolol, Carvedilol, Metoprolol succinate).
If there are contraindications to the use of beta-blockers, experts recommend taking Ivabradine. The product is recommended for heart rates above 70 beats/min. to reduce the load on the heart muscle, slow down myocardial hypertrophy.
The effectiveness of antiplatelet agents and statins in the treatment of CHF has not been proven. These drugs are applicable for cardiac ischemia and atherosclerosis of the carotid arteries (aorta).
It is unacceptable to carry out correction using traditional methods. Only modern treatment of CHF with new generation drugs is applicable. Diuretic herbs and cranberry juice to remove excess fluid from the body can only be taken with the permission of the attending physician
Methods of correction after treatment of CHF:
- implantation for implantation of an artificial left ventricle;
- heart transplantation;
- installation of a defibrillator-cardioverter for severe tachyarrhythmia;
- resynchronizing technique.
Surgery for CHF is rarely prescribed.
Treatment of CHF in children is carried out with medications, as in adults. Dosages and treatment regimen are selected by the doctor based on the clinical signs, weight and age of the child.
Forecast
CCM is a serious pathology that is fraught with various complications:
- thromboembolism;
- liver failure;
- prolonged pneumonia;
- myocardial hypertrophy;
- severe exhaustion of the body;
- cardiac conduction disturbance;
- failure of kidney (liver) function;
- fatal cardiac arrest;
- stroke, myocardial infarction.
Prevention
Chronic heart failure is a pathological condition in which prevention can be divided into:
- primary with the ability to prevent the development of pathology in the heart;
- secondary to stop the progression of already identified deficiency.
Patients should give up alcohol abuse and smoking, moderate physical activity, and adjust their diet. If a diagnosis is made, then follow the recommendations for the treatment of CHF and preventive measures prescribed by the doctor during your stay at home.
If treatment for CHF is not started at the initial stage, the prognosis is unfavorable. The heart wears out quickly as the disease progresses. Severe irreversible processes develop.
If you undergo a timely course of medication or cardiac surgery, you can hope for a favorable outcome and slow down the development of heart failure. If, when treating CHF in the elderly, the recommendations of doctors are followed strictly, then sometimes it is possible to radically minimize the progression of the disease and even achieve stable long-term remission.
8
24/7
Operative technology.
Correction of these disorders is carried out by implantation of a multi-chamber pacemaker with separate stimulation of the right atrium and ventricles. To do this, three electrodes are passed through the subclavian vein and fixed to the wall of the right atrium, at the apex of the RV and through the coronary sinus in the left lateral vein of the LV at the base of the heart.
During open myocardial revascularization, LV remodeling or mitral valve repair, electrodes are fixed epicardially - in the right atrium and at the base of the heart to both ventricles. A prerequisite for the effectiveness of resynchronization is optimization of the pacemaker.