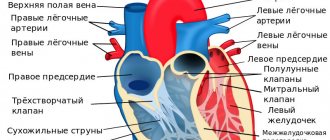
Heart - anatomical data
Structure of the heart
So, the heart (Greek kardia, hence the name of the science of the heart - cardiology) is a hollow muscular organ that receives blood from the flowing venous vessels and pumps already enriched blood into the arterial system. The human heart consists of 4 chambers: the left atrium, the left ventricle, the right atrium and the right ventricle. The left and right hearts are separated from each other by the interatrial and interventricular septa. Venous (non-oxygenated blood) flows in the right sections, and arterial (oxygenated blood) flows in the left sections.
Causes of systolic arrhythmia
The disease is most often associated with other cardiac pathologies. The highest percentage of occurrence is with coronary heart disease . With this disorder, organic damage to the myocardium is observed due to insufficient coronary circulation, which affects the functioning of individual parts or the heart as a whole.
Other cardiac causes include:
- heart failure;
- acquired and congenital heart defects;
- cardiomyopathy;
- infectious lesions of the myocardium.
External influences on the heart also play an important role in the development of arrhythmias. These may be incorrectly selected dosages of medications that increase the ejection fraction - adrenergic agonists, or, on the contrary, weaken it - cardiac glycosides, antiarrhythmic drugs, diuretics.
Electrolyte imbalance often causes arrhythmia, since the activity of the heart depends a lot on the concentration of microelements such as magnesium and potassium in the blood. Both a lack of potassium and magnesium, as well as an excess of the former and an excess of calcium in the blood, negatively affect the functioning of the heart.
In some diseases, the heart rate increases with the possible development of systolic arrhythmias. This primarily concerns thyrotoxicosis, when the thyroid gland begins to intensively produce thyroxine and triiodothyronine. Diabetes mellitus can also cause systolic arrhythmia, since impaired carbohydrate metabolism affects the functioning of many systems and organs, including the heart.
General functions of the heart
In this section we will describe the general functions of the heart muscle as an organ as a whole.
Automatism
Automaticity of the heart
Heart cells (cardiomyocytes) also include so-called atypical cardiomyocytes, which, like an electric ramp, spontaneously produce electrical excitation impulses, which in turn contribute to the contraction of the heart muscle. Violation of this property most often leads to cessation of blood circulation and, without timely assistance, is fatal.
Conductivity
In the human heart there are certain conducting paths that ensure the conduction of electrical charge through the heart muscle not chaotically, but directionally, in a certain sequence, from the atria to the ventricles. If there is a disturbance in the conduction system of the heart, various types of arrhythmias, blockades and other rhythm disturbances are detected, which require medical therapeutic and sometimes surgical intervention.
Contractility
Contraction of the heart
The bulk of the cells of the cardiac system consists of typical (working) cells that ensure the contraction of the heart. The mechanism is comparable to the work of other muscles (biceps, triceps, iris muscle), since a signal from atypical cardiomyocytes enters the muscle, after which they contract. When the contractility of the heart muscle is impaired, various types of edema (lungs, lower extremities, arms, entire surface of the body) are most often observed, which are formed due to heart failure.
Tonicity
This is the ability, thanks to a special histological (cellular) structure, to maintain its shape in all phases of the cardiac cycle. (Contraction of the heart is systole, relaxation is diastole). All the properties described above make possible the most complex, and perhaps the most important function - pumping. The pumping function ensures the correct, timely and complete movement of blood through the vessels of the body; without this property, the life of the body (without the help of medical equipment) is impossible.
Endocrine function
Atrial natriuretic hormone
The endocrine function of the cardiac and vascular system is provided by secretory cardiomyocytes, which are found mainly in the ears of the heart and the right atrium. Secretory cells produce atrial natriuretic hormone (ANH). The production of this hormone occurs when the right atrium muscle is overloaded and overstretched. Why is this being done? The answer lies in the properties of this hormone. PNH mainly acts on the kidneys, stimulating diuresis; also, under the influence of PNH, vasodilation and a decrease in blood pressure occur, which, coupled with an increase in diuresis, causes a decrease in excess fluid in the body and reduces the load on the right atrium, as a result, the production of PNH decreases.
Isolated systolic hypertension in the elderly
Isolated systolic hypertension is defined as increased systolic blood pressure with normal or decreased diastolic pressure. With this disease, there is an increase in pulse pressure, defined as the difference between systolic and diastolic blood pressure. Isolated systolic hypertension can be a variant of primary hypertension, usually observed in the elderly, or secondary in nature (secondary isolated systolic hypertension), being a manifestation of various pathological conditions, including moderate and severe aortic insufficiency, arteriovenous fistulas, severe anemia and kidney damage . In the case of secondary hypertension, if the root cause is eliminated, normalization of blood pressure is possible.
Diastolic blood pressure has been considered for many years as a marker for the diagnosis and prognosis of hypertension, and most studies have been devoted to assessing the effect of diastolic pressure on cardiovascular complications and mortality. However, this approach turned out to be irrational and has undergone changes due to the results of a number of recent large studies. They showed the leading role of systolic blood pressure in the development of cardiovascular damage. Thus, it has been shown that systolic pressure, to a greater extent than diastolic pressure, determines the incidence of strokes and coronary heart disease in people over 45 years of age. According to the study, individuals with isolated systolic hypertension have a 2- to 3-fold increased risk of cardiovascular complications and mortality. Moreover, a significant increase in the risk of cardiac and cerebral complications occurred even with a slight increase in systolic blood pressure (not higher than 160 mmHg). The prognostic role of systolic blood pressure increased with age.
How severe is your isolated systolic hypertension?
The diagnosis of “isolated systolic hypertension” is established when systolic pressure levels are greater than or equal to 140 mmHg. Art., with diastolic pressure levels below 90 mm Hg. Art. There are 4 degrees of isolated systolic hypertension depending on the levels of systolic blood pressure:
ISG degree
Systolic blood pressure, mm Hg. Art.
| I | 140-159 |
| II | 160-179 |
| III | 180-209 |
| IV | 210 and above |
Note. For any degree of isolated systolic hypertension, diastolic (“lower”) blood pressure does not exceed 90 mmHg. Art.
The prevalence of isolated systolic hypertension in different communities varies quite widely (from 1 to 43%), due to the heterogeneity of the population groups studied. There is clearly an increase in the prevalence of isolated systolic hypertension with age. An analysis of the 30-year Framingham study showed the presence of this problem in 14% of men and 23% of women, while in people over 60 years of age it was noted in 2/3 of cases.
- The best way to cure hypertension (quickly, easily, healthy, without “chemical” drugs and dietary supplements)
- Hypertension is a popular way to cure it at stages 1 and 2
- Causes of hypertension and how to eliminate them. Tests for hypertension
- Effective treatment of hypertension without drugs
With age, a person experiences an increase in systolic blood pressure, but there is no significant increase in average pressure, since after 70 years there is a decrease in diastolic pressure due to the development of stiffness of the arterial system.
Hypertension will go away, and the pressure will be 120 over 80 if you include it in the diet...
Hypertension will disappear forever! Here's the secret...
The mechanisms of development of isolated systolic hypertension in the elderly seem complex and not fully understood. The development of hypertension is classically associated with a decrease in the caliber and/or number of small arteries and arterioles, which causes an increase in total peripheral vascular resistance. An isolated increase in systolic blood pressure may be due to a decrease in vascular compliance and/or an increase in stroke volume. In addition, factors such as age-related changes in the renin-angiotensin system, renal function and electrolyte balance, as well as an increase in adipose tissue mass, play a role in the development of isolated systolic hypertension.
As a result of atherosclerotic arterial damage, an increase in systolic blood pressure and pulse pressure, in turn, leads to an increase in mechanical “fatigue” of the arterial wall. This contributes to further sclerotic damage to the arteries, causing the development of a “vicious circle”. Stiffness of the aorta and arteries leads to the development of hypertrophy of the left ventricle of the heart, arterial sclerosis, vascular dilatation and weakening of the blood supply to the heart.
Diagnosis of isolated systolic hypertension
As with other types of hypertension, the diagnosis of isolated systolic hypertension should not be made on the basis of a single blood pressure measurement. It is recommended to establish the presence of persistent pathology only after the second visit of the subject, which should be carried out within several weeks after the first visit. This approach is recommended for all subjects, with the exception of those with high blood pressure levels (systolic pressure above 200 mm Hg) or with clinical manifestations of coronary heart disease and/or cerebral atherosclerosis.
For elderly people with severe sclerotic lesions of the brachial artery, which prevent compression by the tonometer cuff and inflate blood pressure readings, the term “pseudohypertension” is used.
A temporary situational increase in blood pressure during a patient's visit to the doctor, called “white coat hypertension,” should not be considered true arterial hypertension. To clarify the diagnosis in such cases, outpatient (at home) blood pressure monitoring is indicated.
In some cases, isolated systolic hypertension is not diagnosed in a timely manner. The reason for this may be the presence of severe atherosclerosis of the subclavian artery, which is manifested by significant differences in systolic pressure in the left and right arms. In such situations, the true pressure should be considered the blood pressure in the arm, where its levels are higher. Some older people experience an afternoon drop in blood pressure lasting up to 2 hours, which can also cause “pseudohypotension.” In this regard, when measuring blood pressure, the timing of meals should be taken into account.
Finally, orthostatic hypotension often occurs in older people. It is diagnosed when systolic blood pressure decreases by 20 mmHg. Art. or more after moving from a horizontal or sitting position to a vertical one. Orthostatic hypotension (hypotension) is often associated with carotid artery stenosis and can lead to falls and injury. To establish its presence, it is necessary to measure pressure 1-3 minutes after moving to a vertical position.
Considering that isolated systolic hypertension can be primary or secondary, measuring blood pressure alone is not enough to clarify its diagnosis in a particular patient. According to indications, it is necessary to conduct additional laboratory tests.
Treatment of isolated systolic hypertension
In the past, negative attitudes towards the treatment of isolated systolic hypertension were quite widespread. This position was justified by the following points. First, an isolated increase in systolic pressure was not considered a significant risk factor for the development of cardiovascular diseases and their complications. Second, achieving optimal systolic blood pressure levels was considered a difficult and often impossible task. Third, the use of hypertension medications was associated with a high risk of serious side effects. For example, it was considered that a decrease in diastolic blood pressure of less than 85 mmHg. Art. is associated with an increase in morbidity and mortality.
However, the large SHEP trial found no evidence of an increased risk of increased mortality with either lowering diastolic blood pressure or lowering systolic blood pressure in elderly patients undergoing treatment for hypertension.
The results of large studies conducted over the past 10-15 years have demonstrated a significant reduction in cardiovascular and cerebral complications with adequate control of systolic pressure in patients with isolated systolic hypertension. In particular, a significant reduction in the development of myocardial infarction (by 27%), heart failure (by 55%) and strokes (by 37%), as well as a decrease in depression and the severity of dementia were found when adequate treatment of hypertension was carried out in patients with isolated systolic hypertension.
The above data on the high effectiveness of competent treatment for isolated systolic hypertension convincingly argue for the need for strict control of blood pressure in patients with this problem.
Prescribing medications for hypertension for older people should be carried out with extreme caution and only after repeated measurements of blood pressure (if necessary, 24-hour monitoring) confirming the real presence of the disease. In order to reduce the risk of developing orthostatic hypotension both before and during therapy, it is necessary to control pressure in the supine, sitting, and upright positions. Elderly patients often take various medications for concomitant diseases, and therefore the possibility of interaction with prescribed medications for hypertension should be taken into account, which may affect the effect of the drugs and cause additional complications of therapy.
In modern recommendations for the treatment of isolated systolic hypertension, the target value of “upper” pressure is considered to be less than 140 mmHg. Art. However, it is appropriate to note here that in large studies a beneficial effect was achieved already with systolic pressure values below 150 mm Hg, and an additional effect was achieved when systolic pressure values reached less than 140 mm Hg.
A mandatory requirement is a slow gradual decrease in blood pressure. If lifestyle interventions fail to achieve optimal blood pressure levels, the use of hypertension medications is required. In this case (if there are no critical lesions of internal organs yet), it is recommended to initially prescribe small dosages of drugs, with their gradual increase until target levels of systolic pressure are achieved (i.e. less than 140 mm Hg).
What pills to take for isolated systolic hypertension?
In patients with isolated systolic hypertension, an important issue is also the choice of one or more medications that can successfully achieve target blood pressure values with a low level of side effects. Thiazide diuretics and beta blockers are traditionally widely used in the treatment of this disease. This is supported by the results of several large-scale studies assessing the effectiveness of various treatment regimens in elderly people with isolated systolic hypertension. Thus, in a Swedish study, which included 1,627 hypertensive patients aged 70-84 years (61% of them had isolated systolic hypertension), a favorable clinical effect was established with the use of these groups of drugs (a significant reduction in the incidence of strokes and heart attacks myocardium, overall mortality and mortality in strokes).
Another study also assessed the effectiveness of treatment for isolated systolic hypertension in the elderly. It included 4,736 people aged 60 years or older with systolic blood pressure >160 mmHg. and diastolic pressure <90 mm Hg. The average follow-up period was 4.5 years. The initial treatment regimen included chlorthalidone (12.5–25 mg/day). In the absence of adequate blood pressure control, atenolol (25-50 mg/day) or reserpine (0.05-0.1 mg/day) was additionally prescribed.
Mean blood pressure levels during the follow-up period were 155/72 and 143/68 mmHg. respectively for the placebo group and the drug group. The 5-year stroke rate in the group of patients taking hypertension medications was 36% lower than in the placebo group. In the group of patients treated with hypertension, there was a reduction in the incidence of non-fatal myocardial infarction and cardiovascular mortality by 27%. The study noted that medications for hypertension were well tolerated and did not have any adverse effects on the psychoemotional sphere.
In the 80-90s of the twentieth century, data were published on the high ability of ACE inhibitors and calcium antagonists (diltiazem, amlodipine, felodipine) to effectively control blood pressure in patients with isolated systolic hypertension. The large Swedish study STOP-2 (Swedish Trial in Old People) included 6614 hypertensive patients aged 70 to 84 years, with background blood pressure levels of approximately 190/100 mmHg. and target pressure values of about 160/80 mmHg. The study authors noted similar beneficial effects with low-dose ACE inhibitors and calcium antagonists as with thiazide diuretics and beta blockers. However, among these 4 classes of hypertension medications compared, there were no differences in the ability to control blood pressure, as well as in the prevention of cardiovascular mortality.
In recent years, data have been presented on the good blood pressure-lowering effect of angiotensin II receptor blockers for patients with primary hypertension, including the elderly with isolated systolic hypertension. Drugs in this class (in particular, eprosartan) are effective medications for normalizing systolic blood pressure. Recently published reports also provide data on the relatively high effectiveness and safety of the use of small doses of spironolactone in isolated systolic hypertension.
- Hypertension in the elderly - general information)
- What medications for hypertension are prescribed to elderly patients?
- Medicines for the treatment of hypertensive crisis
Right ventricular (RV) function
Mechanical function of the right ventricle
The pancreas primarily performs a mechanical function. So, when it contracts, blood enters through the pulmonary valve into the pulmonary trunk, and then directly into the lungs, where the blood is saturated with oxygen. With a decrease in this property of the pancreas, stagnation of venous blood occurs, first in the RA, and then in all veins of the body, which leads to edema of the lower extremities, the formation of blood clots, both in the RA and mainly in the veins of the lower extremities, which, if left untreated, can lead to a life-threatening, and in 40% of cases even fatal condition - pulmonary embolism (PE).
Afterload
Afterload is the resistance to the expulsion of blood from the ventricles into the aorta and pulmonary artery. The main factor of afterload is an increase in total peripheral vascular resistance (TPVR). The reasons for the increase in afterload, which prevents the expulsion of blood from the heart, may be arterial hypertension, aortic stenosis, coarsening of the aorta and narrowing of the lumen of the pulmonary artery, hydropericarditis.
The magnitude of stroke volume directly depends on the degree of shortening of the fibers of the ventricular myocardium. The speed and degree of shortening of the muscle fibers of the ventricular wall at a given value of the length of the myocardial fiber in diastole and myocardial contractility are inversely proportional to the afterload experienced by the myocardium.
The amount of afterload in a healthy heart depends on the level of pressure in the aorta, but afterload can also be defined as the tension or force developed by the ventricular wall during ejection of blood. Consequently, the afterload experienced by the cardiac muscle fibers also depends on the size of the heart, which is consistent with Laplace's law, according to which the tension of the muscle fibers is equal to the product of the pressure in the ventricular cavity and the radius of the ventricle, divided by the thickness of the ventricular wall.
Thus, at the same aortic pressure, the afterload experienced by a dilated ventricle is higher than by a normally sized ventricle. Moreover, at any aortic pressure and left ventricular volume, the afterload on the myocardium is inversely proportional to its wall thickness.
In turn, the pressure in the aorta largely depends on peripheral vascular resistance, the physical characteristics of the arterial bed and the volume of blood present in it at the time of blood ejection from the ventricle. At any value of the end-diastolic volume of the ventricle and the level of myocardial contractility, the value of the stroke volume of the left ventricle is directly dependent on the afterload.
As noted above, an increase in preload and myocardial contractility stimulates the shortening of myocardial fibers, and afterload slows down this process. The main determinants of stroke volume are the degree of shortening of myocardial fibers and the size of the left ventricle.
Blood pressure is a function of cardiac output and systemic peripheral vascular resistance. The amount of afterload depends on the size of the left ventricle and the level of blood pressure. An increase in blood pressure caused by vasoconstriction, for example, leads to an increase in afterload, which, through a feedback mechanism, has a depressive effect on the process of shortening myocardial fibers, reducing stroke volume and cardiac output. This in turn helps restore blood pressure to its original level.
Thus, myogenic mechanisms regulating the activity of the heart can provide significant changes in the strength of its contractions.
The pressure-volume loop is a graphic image of the pumping function of the heart
For convenience and objectification of the analysis of cardiac activity, the relationship between preload, inotropic state and afterload, i.e. factors that determine the pumping function of the heart, often the relationship between pressure and blood volume in the cavities of the heart, are integrated graphically in the form of corresponding diagrams (syn: loops) “pressure-volume” [in the context of the material presented, “loop” is a scientific concept (syn: loops) Carnot cycle), which is used to denote a reversible circular process (historically it entered the scientific lexicon in the study of thermodynamics)].
The dynamics of the “construction” of such a loop (using the example of the pumping function of the left ventricle) are presented below.
When the mitral valve opens, the left ventricle begins to fill with blood. The volume of the ventricle gradually increases, and at the end of its diastole, left atrium systole occurs, which actively increases the filling of the ventricle and, accordingly, the pressure in its cavity - this is preload. The slope of the diastolic pressure curve is an indicator of the diastolic “stiffness” (resistance, compliance) of the left ventricle.
Then systole begins (the period of isovolumic contraction): the pressure in the ventricle increases sharply (the curve goes up) and when it exceeds the pressure in the aorta, the aortic valves open and blood begins to flow into the aorta. The resistance to blood flow when the aortic valves open is afterload (resistance to emptying of the heart). Next, the blood enters the vessels, the volume of the ventricle decreases slowly at first, and then the pressure in its cavity quickly drops. The end of systole depends on the contractility of the myocardium (the better the contractility, the more to the left this angle will be located and the wider the volume-pressure loop).
The loop area is numerically equal to the work, i.e. pumping function of the left ventricle in one cardiac cycle, and the shape of the loop reflects the mechanisms for performing this work. Of course, the area and shape of the loop depend on the specific operating conditions of the cardiac pump.
Thus, the volume-pressure loop allows you to visualize, i.e., form a visual image of the pumping function of the heart, and conduct an objective analysis of the state of intracardiac hemodynamics and its changes under the influence of various factors, including. drugs acting on the inotropic state of the myocardium, preload and afterload. In an integrated form, this statement is illustrated in Fig. 1.16.
As afterload increases, the volume-pressure loop moves upward. This shift is due to the fact that the aortic valves (upper right corner of the loop) open only when the systolic isovolumic pressure of the ventricle exceeds the pressure in the aorta. The resistance to blood flow when the aortic valves open is an afterload, which is determined by two factors: the resistance to emptying of the heart and the tension of the myocardial fibers. During the isovolumic phase of systole, fiber tension must increase to overcome resistance to blood flow. It is obvious that the lower the contractility of the myocardium, the smaller the width of the loop and the more to the right its upper left corner (end of systole) is located.
As preload increases, the volume-pressure loop shifts to the right. The lower left corner of the loop is the time of opening of the mitral valve (the beginning of diastolic filling of the left ventricle). The volume of the left ventricle gradually increases, and at the end of diastole the pressure in its cavity also increases (the lower right corner of the loop corresponds to the end of diastole) - this is preload. This angle shifts to the right due to increased end-diastolic pressure in the left ventricle.
Thus, using the above example, one can be convinced that the “volume-pressure” loop, or more precisely, its area graphically (quantitatively) reflects the pumping function of the left ventricle to overcome aortic blood pressure, and the shape of the loop, i.e. its structure, is the mechanism performing this work.
(No Ratings Yet)
Left ventricular function
LV wall 10-12 mm
Between the LA and LV there is the mitral valve, it is through it that blood enters the LV, and then through the aortic valve into the aorta and the entire body. The LV has the highest pressure of all the cavities of the heart, which is why the LV wall is the thickest, so normally it reaches 10-12 mm. If the left ventricle ceases to perform its properties 100%, there is an increased load on the left atrium, which can also subsequently lead to pulmonary edema.
Preload
Preload is a measure of the volume of blood entering the chambers of the heart, which creates the filling pressure of the cavities of the heart (primarily the ventricles) necessary to stretch the cardiomyocytes relative to their original length. An increase in preload is observed with hypervolemia and heart valve insufficiency. In this case, regardless of the inotropic state of the heart muscle, its work is regulated mainly by the length of the muscle fibers of the ventricle at the end of diastole, i.e., the end-diastolic volume of the ventricle.
Frank-Starling Law
Back in the 18th century. it was found that an increase in ventricular filling, i.e. An increase in end-diastolic volume or preload leads to an increase in the strength of heart contractions and stroke volume. This property of the heart is a manifestation of the Frank-Starling law. In experiments on isolated muscle cells with their stretching (increasing length) with suspended weights, it was proven that with a consistent increase in preload [in the figure - this is the traction force (weight) of suspended weights - A, B, C, D] in the activated myocyte, its tension increases no real reduction.
Frank-Starling Law: The force of contraction of the ventricles of the heart, measured by any method, is a function of the length of the muscle fibers before contraction
The dependence of the force of cardiac contraction on the value of the end-diastolic volume is shown in graphical form. When the intact left ventricle is filled with blood in a moderate amount (volumes A, B, C), intracavitary pressure slowly increases, which then ensures an increase in the force of heart contractions. The pressure created during the isovolumic (initial) phase of systole reflects an increase in ventricular contractility. As the inotropic state of the ventricle increases, the isovolumic systolic pressure curve shifts upward (dashed line)].
This is the so-called isometric contraction (fragment I). The muscle tension created in response to each of the four preloads is shown in fragment I. Exposure to increasing preloads A, B and C causes an increase in myocyte tension. However, with a further increase in preload (weight D), the overlap of thick and thin filaments begins to decrease, which is expressed in a drop in the voltage of the activated myocyte during its isometric contraction (fragments I and II, fragment III).
If the left ventricle fills with blood in increasing quantities, but at the same time maintains its volume unchanged, the course of the isovolumic systolic pressure curve will reflect the tension, i.e. contractility, syn: inotropic state) of the ventricles. This curve is similar to the tension (isometric contraction) curve established for isolated muscle cells.
Under physiological conditions, filling the ventricle to an increasing volume leads to an increase in intracavitary pressure, which determines an increase in the force of ventricular contraction.
If sympathomimetics act on the heart, which, mediating their effects through (1-adrenergic receptors, increase the concentration of intracellular Ca2+, then this leads to an increase in myocardial contractility. The more intracavitary blood pressure increases with a given constant volume of ventricular filling, the more the isovolumic pressure curve shifts upward reflecting increased contractility of the ventricular wall.
When the pressure in the left ventricular cavity rises above the blood pressure in the aorta, the aortic valve opens and blood is expelled from the left ventricle. As aortic pressure increases, the force of ventricular contraction should also increase in response to increased afterload. In a certain limited range, filling the ventricle in increasing quantities leads to an increase in the force of its contraction due to an increase in intrastriatal pressure.
Function of the interventricular septum
The main function of the interventricular septum is to prevent the mixing of flows from the left and right ventricles. With the pathology of the IVS, mixing of venous blood with arterial blood occurs, which subsequently leads to lung diseases, failure of the right and left parts of the heart, such conditions without surgical intervention most often end in death. Also, in the thickness of the interventricular septum there is a path that conducts an electrical charge from the atria to the ventricles, which causes synchronous operation of all parts of the cardiac and vascular system.
Heart pacemaker
What makes the heart beat? How does our far from perpetual motion machine work? The pacemaker of the heart is responsible for the operation of the heart “pump”. Due to various external and internal reasons, its function may be impaired. What are the consequences of pacemaker migration and is it possible to restore its normal operation?
Natural pacemaker
Anatomically, the pacemaker of the heart is located in the right atrium where the superior vena cava flows into it. This piece of muscle tissue is called the sinus node. It is responsible for the generation of impulses that form a wave of excitation, which travels further through all parts of the heart and regulates its normal functioning. This excitation and transmission system ensures the rhythm and synchronization of the work of all chambers - both the atria and the ventricles.
Nature has provided several pacemakers in the heart. The main one is the sinus node (first order driver). It provides a normal heart rate - 60 - 90 per minute. In a pathological condition, when the sinus node fails, the second-order pacemaker, the atrioventricular (atrioventricular) node, is activated. It generates a smaller number of contractions - from 40 to 50. If this node also refuses to produce impulses, the conductive bundle of His takes over this function. Normally, it is the conductor of impulses sent by the sinus node. The number of heart contractions produced by the His bundle as a pacemaker does not exceed 30–40 per minute.
Driver migration and heart block
Sometimes the heart begins to beat unevenly - the rhythm slows down or speeds up, it “misses” a beat or, conversely, gives out an “extra” beat. Such a malfunction in its work is called arrhythmia. This means that the sequence of impulse transmission has been disrupted. The transition of the sinus driver function to the atrioventricular driver is called migration. Arising first in the second-order pacemaker, it suppresses the wave from the sinus node. In this case, the synchronicity of contraction of all chambers of the heart and the passage of the impulse from the main generating beam to the conductive (Gis) beam are disrupted. Doctors call this condition heart block.
Uneven contraction of the atria and ventricles disrupts the normal flow of oxygenated blood and its flow to all tissues and organs. First of all, the brain “starves”. With a partial blockade, a person may not experience specific symptoms. Arrhythmia is accompanied by symptoms that can be attributed to other diseases:
- general malaise and decreased performance;
- dizziness;
- increased blood pressure;
- feeling of interruptions and pain in the heart.
One of the causes of heartbeat disturbances is AV block. It has three degrees:
Degree
Violations
| 1st degree | The conduction of impulses from the sinus node through the atrioventricular node is disrupted. The interval of its passage increases |
| 2nd degree | Type 1 – the interval of impulse passage through the atrioventricular node increases with periodic loss of ventricular contractions; |
| Type 2 – the interval does not shorten, but ventricular contractions are lost; | |
| Impulse pathology increases | |
| 3rd degree | The transmission of impulses through the atrioventricular node stops, spontaneous contraction of the ventricles begins |
Bradysystole is especially dangerous. This is a condition when the atria contract in a normal rhythm, and the ventricles contract in a slow rhythm. The person feels shortness of breath, severe dizziness, and darkening of the eyes. Objectively, this occurs due to a sharp deterioration in blood circulation and cerebral ischemia, especially when the heart rate drops to 15 beats per minute. Possible loss of consciousness, a feeling of intense heat in the head and sudden paleness of the skin. Among all heart diseases that lead to death, a tenth are arrhythmias.
Indications for installation of a pacemaker
An artificial heart pacemaker (APM) can return a patient to normal life with heart block and other rhythm disturbances. Pacemakers work by being able to electronically detect changes in the heart and adjust its rhythm if necessary. Indications for installation:
- pathological bradycardia (slow heartbeat);
- inconsistency of heart rate with physiological needs during physical activity;
- ventricular tachycardia (ventricular extrasystole);
- permanent or transient (transient) AB heart block of 2 and 3 degrees after myocardial infarction;
- atrial fibrillation (fibrillation and flutter).
Contraindications for surgery are acute infectious diseases and mental disorders of the patient, with whom productive contact to set up the device is impossible.
Types of artificial pacemaker
The type of artificial pacemaker (pacemaker) depends on the problem that needs to be solved:
- cardioverter - a defibrillator designed to correct the rhythm during ventricular paroxysmal tachycardia (rapid heart rate);
- An electrical pacemaker (pacemaker) normalizes a slow heartbeat by stimulating the sinus node.
Electrical pulse therapy, which includes the use of cardioverters - defibrillators, has proven itself as an effective means of correcting cardiac arrhythmias. The essence of the technique is to electrically “reboot” the heart. A short-term current is applied to the myocardium, which depolarizes active muscle cells and forces them to work in the correct mode.
Operating principle of IVR
The main part of the ECS is the microcircuit. In fact, it continuously takes an electrocardiogram, monitoring the heart rhythm. The device is equipped with a battery, which is used to influence the myocardium. The proper functioning of the heart is stimulated by electrodes that are implanted into the heart muscle. Setting up and monitoring the operation of the pacemaker is carried out through a programmer - a computer located in the clinic where the pacemaker was implanted.
How is the operation performed?
Implantation is performed under local anesthesia and under X-ray control. The doctor makes an incision and inserts an electrode through the subclavian vein into the right atrium. Using an electrocardiogram, he empirically selects the best position of the electrode and secures it in the heart muscle. The ECS body is sewn into the thickness of the left pectoral muscle.
The pacemaker is programmed using the following parameters:
- ECG recording mode;
- stimulation mode;
- recognition of the degree of physical activity;
- operation in emergency mode (for example, when the battery is prematurely discharged).
After the operation, the patient is under medical supervision for several more days. The device’s battery is designed for uninterrupted operation for 8 to 10 years.
Possible complications
Complications are rare and may include the following:
- wound infection with suppuration and fistula formation;
- displacement of the electrode in the heart cavity;
- fluid accumulation in the pericardium and bleeding;
- exposure to current (stimulation) on the pectoral muscles and diaphragm;
- depletion of the stimulant and loss of its sensitivity;
- electrode damage.
Complications can be prevented by observing all requirements for device installation, providing adequate drug therapy after surgery and promptly reprogramming the pacemaker.
conclusions
Pumping activity of the ventricles
All of the above properties are very important for the normal functioning of the heart and the functioning of the human body as a whole, since the violation of at least one of them entails varying degrees of threat to human life.
- The pumping function is the most important property of the heart muscle, ensuring the movement of blood throughout the human body and its enrichment with oxygen. The pumping function is carried out due to certain properties of the heart, namely:
- automatism - the ability to spontaneously generate an electrical charge
- conductivity - the ability to conduct an electrical impulse through all parts of the heart, in a certain sequence, from the atria to the ventricles
- contractility - the ability of all parts of the heart muscle to contract in response to an impulse
- tonicity is the ability of the heart to maintain its shape in all phases of the cardiac cycle.
- Neuroendocrine function - the production of natriuretic hormone occurs precisely in the heart muscle, it (the hormone) ensures an increase in diuresis, a decrease in blood pressure and dilation of blood vessels, and due to this, the load on the heart is reduced.
Healthy heart
All these properties ensure stable and continuous cardiac activity, and in the absence of at least one of the above properties, life activity (without external medical equipment) is impossible.
Each of the departments of the cardiac and vascular system has its own very important function. The right parts of the heart pump blood to the lungs, where venous blood is saturated with oxygen, and the left parts help move arterial blood from the heart throughout the body. Therefore, it is important to understand that the synchronous work of each department contributes to the normal functioning of the body, and disruption of the structure or functioning of at least one of them will eventually lead to pathological processes in other departments.
Cardiovascular function
The main purpose of the cardiovascular system is to ensure blood circulation, that is, constant blood circulation in a closed system of the heart.
Functions of the cardiovascular system:
- transport of substances necessary to ensure the functions of body cells;
- delivery to the cells of the body of chemicals that regulate their metabolism;
- removal of their metabolites from cells;
- humoral connection of organs and tissues with each other;
- delivery of protective agents to tissues;
- removal of harmful substances from the body;
- heat exchange in the body.
The pumping function of the heart is based on the alternation of relaxation ( diastole ) and contraction ( systole ) of the ventricles.
Blood leaves the heart through arterial vessels and arrives through venous vessels .
Activity of the heart: contraction of the heart is observed due to periodically occurring processes of excitation in the heart muscle.
Calculating the pulse is the amount of PD.
For effective pumping activity, synchronous work of myocardial muscle fibers is necessary.
Global systolic function
Global systolic function
Accurate examination of LV function requires obtaining multiple views from parasternal and apical approaches. First, an image of the LV is usually obtained from a parasternal approach along its long (Fig. 2.1) and short (Fig. 2.9, 2.10) axes. Two-dimensional images of the LV allow precise targeting of the ultrasound beam for M-modal examination (Fig. 2.3, 2.4). It is necessary to select the gain parameters so that the LV endocardium is clearly visible on the image. Difficulties in determining the true contours of the LV are the most common source of error in determining its function.
From the apical approach, visualization of the LV is performed in two-dimensional mode in four and two-chamber positions (Fig. 2.11, 2.12, 2.14). It is also possible to study the LV from a subcostal approach (Fig. 2.16, 2.18).
Among the parameters of LV function obtained using M-modal echocardiography, the most informative are the following: anteroposterior shortening of the short axis of the LV, the distance from the E-peak of movement of the anterior mitral valve leaflet to the interventricular septum [20], amplitude of movement of the aortic root.
Anteroposterior shortening
characterizes the ratio of diastolic (coinciding with the apex of the R wave of the electrocardiogram) and systolic (end of the T wave) sizes of the LV. Normally, the anteroposterior size of the short axis of the LV is reduced by 30% or more. In Fig. 2.4 shows a record of an M-modal study of the LV with its normal anteroposterior shortening, in Fig. 5.15C - with dilated cardiomyopathy.
Relying only on M-modal measurements can lead to serious errors in assessing LV function, since these measurements only take into account a small part of the LV at its base. In case of coronary heart disease, segments with impaired contractility can be removed from the base of the LV; however, anteroposterior shortening of the LV will create a false impression of global LV systolic function. M-modal measurements of LV dimensions do not take into account its length; when calculating LV volumes according to Teichholz [37], the length of the short axis of the LV is raised to the third power; this formula is extremely inaccurate. Unfortunately, it is still used in some laboratories.
Distance from the E-peak of movement of the anterior mitral valve leaflet to the interventricular septum
- this is the distance between the point of greatest opening of the mitral valve (during early diastole) and the nearest section of the interventricular septum (during systole). Normally, this distance does not exceed 5 mm. With a decrease in global contractility of the LV, the amount of blood remaining in its cavity at the end of systole increases, which leads to LV dilatation. At the same time, a decrease in stroke volume leads to a decrease in transmitral blood flow. In this case, the mitral valve does not open as wide as normal. The amplitude of movement of the interventricular septum is also reduced. As global LV contractility worsens, the distance between the E-peak movement of the anterior mitral valve leaflet and the interventricular septum increases increasingly. The UCSF Echocardiography Laboratory does not use M-modal data to quantify LV function, preferring two-dimensional and Doppler echocardiography parameters.
The amplitude of movement of the aorta at the base of the heart
should also be assessed only qualitatively. It is proportional to stroke volume. The behavior of the aorta depends on the filling of the left atrium and on the kinetic energy of the blood ejected by the left ventricle during systole. Normally, the aortic root moves anteriorly during systole by more than 7 mm. This indicator should be treated with caution, since a low stroke volume does not necessarily mean a decrease in LV contractility. If the aortic valve leaflets are clearly visualized along with the aorta, systolic time intervals can be easily calculated. The degree of opening of the aortic valve leaflets and the pattern of their movement are also indicators of LV systolic function.
In past years, many publications have appeared devoted to methods of computer processing of M-modal images of the LV. But we will not dwell on them, since in most clinical echocardiography laboratories computers are not used for these purposes, and in addition, with the development of echocardiographic technology, more reliable methods for assessing global LV contractility have appeared.
A two-dimensional echocardiographic study provides both qualitative and quantitative assessment of global LV contractility. In everyday practice, echocardiographic images are evaluated in the same way as ventriculograms: the approximate ratio of the systolic and diastolic dimensions of the heart is determined. A number of researchers believe that it is possible to very accurately estimate the ejection fraction without resorting to measurements [25]. We, however, when comparing the results of such an assessment with the quantitative calculation of the ejection fraction during ventriculography, found an unacceptably large number of errors.
The most accurate way to assess global LV contractility is quantitative two-dimensional echocardiography. This method, of course, is not without errors, but it is still better than visual assessment of images. In all likelihood, Doppler studies of global LV systolic function are even more accurate, but for now they play an auxiliary role.
To quantify the global contractility of the LV, the choice of a stereometric model of the LV is fundamental [29, 31, 32, 33, 34, 39, 42, 43]. After selecting a model, the LV volumes are calculated based on its planimetric measurements using an algorithm corresponding to the selected model. There are many algorithms for calculating LV volumes, which we will not dwell on in detail. The UCSF Echocardiography Laboratory uses a modified Simpson algorithm, more correctly called the disk method (Fig. 5.1). When using it, the accuracy of measurements is practically independent of the shape of the LV: the method is based on the reconstruction of the LV from 20 disks - sections of the LV at different levels. The method involves obtaining mutually perpendicular images of the LV in two- and four-chamber positions. Several centers have compared the disc method with radiocontrast and radioisotope ventriculography. The main disadvantages of the disc method are that it underestimates (by approximately 25%) LV volumes and requires the use of computer systems. Over time, the cost of computer systems will decrease and image quality will improve; therefore, quantitative methods for assessing LV contractility will be more accessible.
Figure 5.1. Calculation of left ventricular volumes using two algorithms. Top: Calculation of left ventricular volume using the disc method in two planes (modified Simpson algorithm). To calculate the left ventricular volume (V) using the disc method, it is necessary to obtain images in two mutually perpendicular planes: in the apical position of a four-chamber heart and in the apical position of a two-chamber heart. In both projections, the left ventricle is divided into 20 disks (ai and bi) of equal height; the areas of the discs (ai ? bi ??/4) are summed up, the sum is then multiplied by the length of the left ventricle (L). The disc method is the most accurate method for calculating left ventricular volumes, since its results are least affected by left ventricular deformations. Bottom: calculation of left ventricular volume using the area-length formula in one plane. This method, originally intended for calculating left ventricular volumes with radiopaque ventriculography, is best if a good image of the left ventricle can be obtained in only one apical position. A is the area of the left ventricle in the image, L is the length of the left ventricle. Schiller NB Two-dimensional echocardiographic determination of left ventricular volume, systolic function, and mass. Summary and discussion of the 1989 recommendations of the American Society of Echocardiography. Circulation 84(Suppl 3):280, 1991.
Upper pressure is high, lower pressure is normal - what does this mean?
Arterial hypertension is gradually becoming a disease that is increasingly common among relatively young people. The popular belief that it is a disease of the elderly is not so true.
Increasingly, doctors are diagnosing hypertension in men under 40 and in women who have not yet entered menopause. But still, it is isolated systolic arterial hypertension (ISAH), a disease in which high upper blood pressure is observed, to a greater extent in people in the 60+ category.
Characteristics of isolated hypertension
Why is this disease classified as a separate class and not simply called arterial hypertension? The point is the difference in development mechanisms, i.e. ISAH and so-called classical hypertension develop differently, the diseases also affect the target organs in their own way, and the prognosis will vary.
ISAH is not such a common disease; it is diagnosed in no more than 14% of cases, and this is the maximum threshold for the frequency of occurrence. At risk are people over 60. The percentage of cases increases in proportion to age; in people 70-80 years old, isolated hypertension is detected in 80% of cases.
High upper pressure with normal lower pressure is due to reduced distensibility of the main arteries, and mainly the aorta. The physiological norm of the main artery is to receive and suppress the force of cardiac output precisely due to its own elasticity. Blood is passed further throughout the body.
But if the wall of the main vessel becomes excessively rigid, then in order to push blood out of the heart muscle, a different pressure is required, its indicators have to increase. The functions of smaller vessels do not change at this time, therefore the diastolic blood pressure remains the same.
What does high pressure in the arteries lead to?
High upper pressure leads to:
- Overgrown muscle tissue of the left ventricle, due to which its function gradually decreases, which leads to
- Heart failure;
- Because the speed of blood flow through large vessels is disrupted;
- Because the inner vascular layer, called the endothelium, is damaged, and the deformed area is replaced by connective, stiffer tissue;
- Production of active enzymes such as renin, nitric oxide, angiotensin, and they have a negative effect on the vascular wall.
High systolic pressure is dangerous because a person not only feels unwell, but the functioning of the main vessels deteriorates. Target organs are at particular risk.
Target organs: how ISAH affects them
Isolated systolic hypertension is a pathology, the risk of severe complications of which is several times higher compared to the usual form of hypertension. However, if both ISAH and hypertension with two elevated values are left untreated, the likelihood of developing severe brain and heart damage is more than 80%.
How are target organs affected?
- Brain. There is a loss of some intellectual abilities. A stroke is either seriously disabling or fatal.
- Retina. The chronic form of the disease leads to loss of visual acuity. The acute form is complete loss of vision over a short period.
- Kidneys. With chronic failure, connective tissue grows and the functionality of the organ gradually decreases. The acute form has an inconspicuous course if both kidneys are functional.
- Heart. Chronic insufficiency deprives a person of the strength to withstand normal physical activity. A treated heart attack leads to heart muscle failure, and extensive damage is fatal.
What does the primary form of ISAH mean?
Isolated systolic hypertension is also called primary or essential. The mechanisms of its progression are determined by a combination of risk factors. And these factors are identical to each form of hypertension.
Risk factors for hypertension (including ISAH):
- Genetic disorders;
- Atherosclerosis;
- Diabetes;
- Age-related deformations of vascular tissues;
- Smoking;
- Overweight;
- Alcoholism;
- Female gender (here the incidence is twice as high).
It must be said that in 50% of all cases ISAH has no symptoms. They are not present until signs of disturbances in cardiac blood flow and blood flow in the brain appear. And these signs are the same - these are headaches of different types and durations, this is heaviness in the chest area, visual defects.
More than half of the patients cannot complain about anything - there are really no pronounced symptoms. High blood pressure can be discovered accidentally, usually during an appointment at the clinic. In this case, your general well-being may not suffer at all.
The diagnosis of ISAH is valid if the upper pressure is persistently above 140 mm Hg. Art., and the lower readings are less than 90 mm Hg. Art. To give a more accurate assessment, 24-hour blood pressure monitoring is required (not in a medical facility).
How to treat ISAH
Of course, taking medications on your own, without special prescriptions, is extremely dangerous.
And a hypertensive patient will not be able to reduce his upper pressure without affecting his lower pressure. Each drug has its own contraindications and has its own strength of action. What drugs lower blood pressure?
- Diuretics (or a group of diuretics). Normalization of the condition occurs due to the removal of excess water from the body.
- β-blockers. Medicines in this group are usually prescribed to people with liver pathologies, as well as to those who have suffered a myocardial infarction.
- Calcium antagonists. A larger percentage of funds in this group allow you to lower your blood pressure in the short term. There are longer-acting drugs, they are prescribed often, as their effectiveness is high.
- ACE inhibitors. Medicines in this group have a beneficial effect on the kidneys and central nervous system.
In the primary form of ISAH, treatment will be long-term, in most cases lifelong.
Lifestyle correction for hypertensive patients
It is impossible to reduce high systolic blood pressure without lifestyle adjustments. How to lower high blood pressure? You need to reconsider your menu, your physical activity, exposure to stress and reaction to them.
Everyone can lead an active lifestyle according to their capabilities and strengths. At least proper morning exercises, swimming, walking - the minimum that is most accessible and within the power of almost everyone.
It is a good idea for a hypertensive patient to attend physical therapy classes, where, under the guidance of a specialist, he will work on his body, increasing its physical capabilities.
Nutrition should be correct: avoid fatty and fried foods, rarely allow yourself sweets and starchy foods. But the daily menu must include fruits and vegetables, the fiber of which is very necessary for the body and blood vessels. It removes harmful cholesterol from blood vessels and prevents it from entering the system.
Safe ways to reduce blood pressure at home
Again, you can start with diet. Literally every day it is recommended to drink juices from fresh vegetables. The menu should also have enough beets, carrots, cabbage, legumes, tomatoes, bananas and herbs. Low-fat dairy products, low-fat fish and meat will be beneficial. You should seriously reduce your salt intake. Buckwheat, oatmeal and rice porridge will be useful.
There are some specific home remedies for lowering blood pressure. They are universal, but may not suit you specifically. Therefore, each of the methods should be discussed with your doctor, having received his approval for a particular action.
Ways to lower pressure:
- Vinegar compress. Apple cider vinegar should be diluted with water 1:1, and then stand on a towel soaked in this mixture.
- Temperature difference. Hot water is poured into one basin, cold water into the other. Three to five times you need to alternate immersing your legs in both pelvises. Place your feet in hot water of a permissible temperature for two minutes, and in cold water for half a minute.
- Head massage. Involves a light massage of the forehead, temporal part and parietal part with a transition to a more intense massage.
- Cold compress. It should not be done more often than once every three days. This is ice in a towel applied to the cervical vertebra on both sides. The ice must be held until it melts. Then this place should be lubricated with any oil and rubbed.
- Tincture of calendula. Take 30 drops three times a day.
Once again, it’s worth remembering: these recipes are relatively safe, but they won’t suit everyone. Concomitant diseases, specific numbers on the tonometer, and the patient’s preparedness are also important. Be sure to discuss the proposed methods with your doctor.
Only a doctor can tell you how to lower high blood pressure without lowering low blood pressure. He will take into account the dynamics and progression of the disease and prescribe the combination of drugs that will be effective specifically for you.
Prevention of ISAH
It’s unlikely that anyone doesn’t know that you need to take care of your health. But many do not consider it important that preventing a disease must be done no less responsibly than treating it. It is possible to live a full life, without overcoming daily physical difficulties and pain, only if a number of conditions are met.
Prevention of blood pressure includes:
- Losing excess weight. Obesity entails a huge layer of problems. It almost always affects blood pressure, and as long as there are extra pounds, there is no need to talk about treating hypertension. A smart move would be to see a nutritionist who can help your desire to lose weight become a clear, achievable plan.
- Reducing salt in the diet. You shouldn’t give up salt completely, but you shouldn’t wait for doctors to beg you to forget about salty foods. Just don't accustom yourself to it. Start reducing your consumption gradually. Season the vegetable salad with lemon juice and herbs, avoiding generous salting.
- Foods containing magnesium, potassium and calcium are also beneficial for cardiovascular health.
- Quitting alcohol. And this should also be done as early as possible. Moreover, health is affected not only by the frequency of abuse, dosage, and quality of alcohol. If a person drinks extremely rarely, but once he drinks seriously, the numbers on the tonometer can become dramatically different - the pressure jumps significantly, and this is dangerous.
- Anti-stress therapy. This is the prevention of stress, emotional burnout, and depression. You need to learn to cope with shocks and negative events, so that the force of stress does not affect your physiological state.
- Control of diabetes mellitus, if such a disease exists. This disease is also closely associated with increased blood pressure, but conscious patients can prevent many complications.
- Be attentive to other medications used. Some drugs have increased blood pressure among their side effects. For example, hormonal contraceptives have this quality. But not only these pills can increase blood pressure, therefore any prescription of a drug should also be considered in terms of possible side effects.
The condition of blood vessels and the heart, the influence of physical education on metabolic processes cannot be denied, therefore, even before the first alarm bells arise, you should introduce physical activity into your life. And we are not talking about sports, about serious training, it can be long walks, home exercises, swimming, etc.
Why may upper blood pressure increase in pregnant women?
It makes sense to consider this issue separately. In the bloodstream of the expectant mother, the volume of blood increases significantly, which can lead to systolic hypertension. And this, of course, requires observation and adequate therapy. This symptom is really dangerous - it can be a marker of incipient gestosis and placental insufficiency.
Classic gestosis is a triad of such serious disorders as kidney failure, edema syndrome and hypertension. The signs may not be expressed equally, but almost always they are observed simultaneously. The condition threatens severe complications, which is why a pregnant woman must often visit a doctor, and at each appointment, among other procedures, her blood pressure is measured.
An increase in upper pressure while the lower one is normal is a reason to consult a doctor. Take a coupon for an appointment with a therapist, and then the doctor will prescribe diagnostic measures and refer you to specialized specialists if necessary. A quick response is the key to successful treatment and the ability to avoid negative consequences.
Video - High upper pressure
Classification
All of the above options lead to disruption of myocardial contractility, that is, they affect blood circulation. The cause of the development of dysfunction may be fibrosis of the heart muscle, its total or focal hypertrophy, ischemia, including the development of post-infarction cardiosclerosis.
One of the means of diagnosing this deviation from the norm is ultrasound of the heart with assessment of TMDP (transmitral diastolic flow). This flow is a measure of the blood entering the left ventricle through the mitral valve, which connects the left atrium to the left ventricle.
In the mid-eighties of the last century, it turned out that the assessment of the TMDP spectrum quite accurately coincides with the severity of chronic heart failure, which makes it possible to set various options for prognosis of the course of the disease.
In general, diastolic dysfunction and its indicators are much better associated with assessing the degree of chronic heart failure than disturbances in systolic blood flow. It is diastolic disorders that determine the severity of cardiac congestion, such as edema.
Treatment of such a disorder is necessarily complex. Prevention of arrhythmia is absolutely necessary - restoration of rhythm during atrial fibrillation. In addition, drugs are recommended that slow down the conduction of impulses from the atria to the ventricles.
This allows the atria to relax better. The use of nitrates, diuretics (to eliminate edema and congestion in the lungs), as well as ACE inhibitors, which relax the myocardium, is also indicated. If systolic function is preserved, taking cardiac glycosides is not allowed.
The definition of diastolic dysfunction (or type of diastolic filling) is based on several features. In most (if not all) heart diseases, the process of myocardial relaxation is first disrupted.
As the disease progresses and LA pressure increases from mild to moderate, the rate of TMP resembles normal (pseudo-normalization). With a further decrease in LV myocardial compliance and an increase in LA pressure, diastolic filling becomes restrictive.
Grade 1 (mild dysfunction) impaired relaxation with normal filling pressure; grade 2 (moderate dysfunction) - pseudonormal picture of TMP; grade 3 (severe reversible dysfunction) - reversible restriction (high filling pressure);
Grade 1 diastolic dysfunction is characterized by normal filling pressure, despite the existing impairment of myocardial relaxation. However, in patients with a pronounced impairment of relaxation, for example with HCM, the pressure may be elevated (E/A 2-10 months).
In young patients, the plastic attraction of the LV is normally very pronounced, which is associated with normal relaxation, so the main filling of the LV occurs in early diastole. As a result, usually E/A {amp}gt;
1.5, DT = 160-240 ms (in the septal area), Ea {amp}gt; 10 cm/sec, E/Ea 50 cm/sec. Such strong relaxation in healthy individuals is manifested by active movement of the mitral annulus from the apex into early diastole with a parasternal long-axis position and an apical four-chamber position.
With normal myocardial relaxation, the pattern of velocity of longitudinal movement of the mitral annulus during diastole is a mirror image of normal transmitral blood flow: the velocity of blood flow in early diastole (Ea) is higher than the velocity of blood flow in late diastole (Aa).
The speed of the lateral part of the MV ring is always higher (normally {amp}gt; 15 cm/sec) than the septal part. Ea in healthy individuals increases with exercise, but the E/Ea ratio remains the same as at rest (usually {amp}lt; 8).
DETAILS: The appearance of systolic murmur during myocardial infarction
With age, there is a gradual decrease in the rate of myocardial relaxation, as well as elastic attraction, which leads to a slower decrease in LV pressure. Its filling becomes slower, which contributes to the development of a picture similar to grade 1 diastolic dysfunction.
Reversion of the Ea/Aa ratio occurs 10-15 years earlier than E/A. The velocity of blood flow in the pulmonary veins also changes with age: the velocity of orthograde diastolic blood flow decreases as the LV fills during atrial contraction, and the velocity of orthograde systolic blood flow becomes more significant.
A study of diastolic function in 1012 individuals without a history of CVD using two-dimensional echocardiography showed that all parameters of diastolic function are associated with age.