Minute blood volume
To determine the IOC, the amount of blood passing through one of the atria in 1 minute is calculated. The characteristic is measured in liters or milliliters. Taking into account the individuality of the human body, as well as the difference in physical data, experts introduced the concept of cardiac index (CI). This value is calculated by the ratio of the IOC to the total surface area of the body, which is measured in square meters. The SI unit is l/min. m².
When transporting oxygen through a closed system, blood circulation plays the role of a kind of limiter. The highest indicator of minute volume of blood circulation obtained during maximum muscle tension, when compared with the indicator recorded under normal conditions, allows us to determine the functional reserve of the cardiovascular system and specifically the heart in terms of hemodynamics.
If a person is healthy, the hemodynamic reserve varies from 300 to 400%. The figures inform that without any danger to the body’s condition, a three- to four-fold increase in IOC, which is observed at rest, is possible. In people who regularly engage in sports and are physically well developed, this figure can exceed 700%.
When the body is in a horizontal position and any physical activity is excluded, the IOC is in the range from 4 to 5.5 (6) l/min. Normal SI under the same conditions does not leave the range of 2–4 l/min. m².
Relationship between the IOC and organs at rest
The amount of blood filling the circulatory system of a normal person is 5–6 liters. One minute is enough to complete a full circuit. With heavy physical work and increased sports loads, the IOC of an ordinary person increases to 30 l/min, and for professional athletes even more - up to 40.
In addition to physical condition, IOC indicators largely depend on:
- systolic blood volume;
- heart rate;
- the functionality and condition of the venous system, through which blood returns to the heart.
Systolic blood volume
Systolic blood volume refers to the amount of blood pushed by the ventricles into the great vessels during one heartbeat. Based on this indicator, a conclusion is made about the strength and efficiency of the heart muscle. In addition to systolic, this characteristic is often called stroke volume or VT.
Systolic volume of blood circulation is calculated by the amount of blood pushed by the heart into the vessels during one contraction
At rest and in the absence of physical activity, during one contraction of the heart, 0.3–0.5 volumes of blood are pushed out to diastole, filling its chamber. The remaining blood is a reserve, which can be used in case of a sharp increase in physical, emotional or other activity.
The blood remaining in the chamber becomes the main determinant that determines the functional reserve of the heart. The larger the reserve volume, the more blood can be supplied to the circulatory system as needed.
When the circulatory system begins to adapt to certain conditions, the systolic volume undergoes a change. Extracardiac nervous mechanisms take an active part in the process of self-regulation. In this case, the main effect is on the myocardium, or more precisely, on the force of its contraction. A decrease in the power of myocardial contractions leads to a decrease in systolic volume.
For the average person, whose body is in a horizontal position and does not experience physical stress, it is normal if the OC varies between 70–100 ml.
Factors influencing IOC
Read more: Cardiac index and its norm
Cardiac output is a variable value, and there are quite a few factors that change it. One of them is pulse, expressed as heart rate. At rest and in a horizontal position of the body, its average is 60–80 beats per minute. Changes in pulse occur under the influence of chronotropic influences, and inotropic influences affect strength.
An increase in heart rate leads to an increase in minute blood volume. These changes play an important role in the process of accelerating the adaptation of the IOC to the relevant situation. When the body is exposed to extreme stress, there is an increase in heart rate by 3 or more times compared to normal. Heart rhythm changes under the chronotropic influence exerted by the sympathetic and vagus nerves on the sinoatrial node of the heart. In parallel with chronotropic changes in cardiac activity, inotropic effects may be exerted on the myocardium.
Systemic hemodynamics is also determined by the work of the heart. To calculate this indicator, it is necessary to multiply the data on the average pressure and the mass of blood that is pumped into the aorta over a certain time interval. The result informs how the left ventricle is functioning. To establish the work of the right ventricle, it is enough to reduce the resulting value by 4 times.
If cardiac output indicators do not correspond to the norm and there are no external influences observed, then this fact indicates abnormal functioning of the heart, therefore, the presence of pathology.
Diagnostic tests
You will need to see a doctor to confirm the problem. In this case, low cardiac output syndrome often requires emergency care, as it can lead to the death of the patient. To identify the disease, a comprehensive cardiological examination is performed. Diagnosis begins with examination and auscultation of the heart area and medical history. To determine the etiology of the problem, an ECHO as well as an ECG will be required. During the research, doctors identify pathologies of the valves, coronary vessels and conduction system. X-rays, blood tests, and abdominal ultrasound are used to evaluate the function of other organs.
The key criterion for diagnosis is the calculation of cardiac output. To do this, you will first need to determine the rhythm of the organ, the area of the left ventricle and its outflow tract. From the obtained values, the stroke volume is determined. This indicator is multiplied by the heart rate and the amount of blood pumped by the cardiac structures per minute is obtained.
Decreased cardiac output
The most common causes of low cardiac output are disturbances in basic cardiac functions. These include:
- damaged myocardium;
- blocked coronary vessels;
- abnormally functioning heart valves;
- cardiac tamponade;
- disrupted metabolic processes occurring in the heart muscle.
When cardiac output decreases and tissues are no longer supplied with nutrients, cardiogenic shock can occur.
The main reason leading to a decrease in cardiac output lies in the insufficient supply of venous blood to the heart. This factor has a negative impact on the IOC. The process is determined by:
- a decrease in the amount of blood involved in circulation;
- decrease in tissue mass;
- blockage of large veins and expansion of ordinary ones.
A decrease in the amount of circulating blood helps to reduce the IOC to a critical threshold. A shortage of blood begins to be felt in the vascular system, which affects the amount of blood returned to the heart.
When fainting occurs due to disorders in the nervous system, small arteries become dilated and veins become enlarged. The result is a decrease in blood pressure and, as a consequence, insufficient blood volume entering the heart.
If the vessels supplying blood to the heart undergo changes, they may partially block. This immediately affects peripheral vessels that are not involved in the supply of blood to the heart. The resulting reduced amount of blood sent to the heart causes low cardiac output syndrome. Its main symptoms are expressed:
- drop in blood pressure;
- low heart rate;
- tachycardia.
This process is accompanied by external factors: cold sweat, low volume of urination and changes in skin color (pallor, blueness).
The final diagnosis is made by an experienced cardiologist after carefully studying the test results.
Reasons for the development of pathology
Low cardiac output syndrome occurs due to various factors. They are usually divided into several groups:
- Myocardial dysfunction. This problem occurs due to ischemic changes in the muscle, and can also be the result of inflammatory processes.
- Incompetent heart valves. This cause of the disease is often diagnosed in children, since in many cases it is a congenital problem.
- Tamponade resulting from the accumulation of fluid in the pericardium. A similar condition occurs both during acute processes, for example, after traumatic damage to the heart sac, and during chronic inflammation affecting the serous layers.
- Impaired function of the coronary vessels. A common cause of the development of ischemic processes in the myocardium is thromboembolism of the arteries feeding the muscle.
- Not only heart disease can lead to the formation of low cardiac output. A number of problems affecting the respiratory system also provoke the development of the disease. For example, pulmonary hypertension, which occurs against the background of chronic inflammation or emphysema, can cause hemodynamic disturbances.
The pathophysiology of the disease is multifaceted. Changes in heart function occur for various reasons. Doctors identify several options for hemodynamic disorders. In some cases, a decrease in the volume of pumped blood occurs due to dysfunction of the right ventricle, but more often the normal functioning of the left chambers changes. The clinical picture is largely determined by the phase of cardiac contraction in which the problem occurs - systolic or diastolic.
Complex disorders accompanied by more intense clinical signs are common. Ventricular dysfunction worsens with increasing preload, that is, the force acting on the myocardium before it contracts. A similar cascade of reactions is formed both with an increase in pressure and volume of blood flowing to the cardiac structures.
Pathological changes can also occur in the vessels of the body, which also leads to aggravation of the problem. In such cases, they speak of an increase in afterload associated with an increase in the resistance of the arteries and veins. Such changes often form against the background of chronic lung lesions, as well as in later stages of heart failure, accompanied by the formation of peripheral edema.
Increased cardiac output
The level of cardiac output depends not only on physical activity, but also on the psycho-emotional state of a person. The functioning of the nervous system can reduce and increase the IOC index.
Sports activities are accompanied by an increase in blood pressure. Accelerating metabolism contracts skeletal muscles and dilates arterioles. This factor allows oxygen to be supplied to the muscles to the required extent. Loads lead to a narrowing of large veins, an increase in heart rate and an increase in the strength of contractions of the heart muscle. High blood pressure causes increased blood flow to the skeletal muscles.
Increased cardiac output is most often observed in the following cases:
- arteriovenous fistula;
- thyrotoxicosis;
- anemia;
- vitamin B deficiency.
In an arteriovenous fistula, the artery is directly connected to the vein. This phenomenon is called a fistula and comes in two types. A congenital arteriovenous fistula is accompanied by benign formations on the skin and can be located on any organ. In this variant, it is expressed by embryonic fistulas that have not reached the stages of veins or arteries.
Arteriovenous fistula
An acquired arteriovenous fistula is formed under the influence of external influence. It is created if there is a need for hemodialysis. Often a fistula becomes the result of catheterization, as well as a consequence of surgical intervention. Such a fistula sometimes accompanies penetrating wounds.
A large fistula provokes increased cardiac output. When it takes a chronic form, heart failure is possible, in which the IOC reaches critically high levels.
Thyrotoxicosis is characterized by a rapid pulse and high blood pressure. In parallel with this, not only quantitative changes in the blood occur, but also qualitative ones. An increase in the level of thyraxine is promoted by an abnormal level of erythropatine and, as a consequence, a decreased erythrocyte mass. The result is increased cardiac output.
With anemia, blood viscosity decreases and the heart is able to pump more of it. This leads to increased blood flow and increased heart rate. Tissues receive more oxygen, and accordingly, cardiac output and IOC increase.
Vitamin B1 deficiency is the cause of many pathologies
Vitamin B1 is involved in blood formation and has a beneficial effect on blood microcirculation. Its action significantly affects the functioning of the heart muscles. A lack of this vitamin contributes to the development of beriberi disease, one of the symptoms of which is impaired blood flow. With active metabolism, tissues stop absorbing the nutrients they need. The body compensates for this process by dilating peripheral vessels. Under such conditions, cardiac output and venous return can exceed the norm by two or more times.
Blood pressure during physical work
Changes
Blood pressure
during various types of muscle activity.
An increase in systolic blood pressure during contraction of human skeletal muscles is one of the most important and necessary components in a complex chain of adaptive reactions of the circulatory system to the conditions of muscle activity. An increase in blood pressure helps to increase the blood supply to contracting muscles, and therefore their performance. Changes in blood pressure during work depend on the nature of the work (rhythmic or static), its intensity, the volume of active muscles, ambient temperature and other factors.
Blood pressure during global cyclic operation.
During dynamic work to the point of severe fatigue (running, cycling, etc.), systolic blood pressure increases exponentially until the end of work (Fig. 7.22). Diastolic blood pressure during such work either remains almost unchanged or increases slightly. With some strenuous exercise, diastolic blood pressure may decrease.
During global cyclic work, systolic blood pressure increases linearly depending on its power and oxygen consumption and can reach 200-240 mm Hg. Art. The reserves for the increase in blood pressure, that is, the difference between blood pressure at rest and during maximum aerobic work, increase as training increases. The reserves for the increase in systolic blood pressure decrease in individuals with low resting blood pressure. The increase in the reserves for the increase in systolic blood pressure as training progresses is due to the development of greater opportunities for increasing the IOC due to an increase in systolic volume and more active vasoconstriction in inactive organs and tissues.
| Peace |
| Job |
| Recovery |
| l 140 > n 3* 120 e! |
| Diastolic blood pressure |
| 14 16 Time, min |
Rice.7:22.
Changes in systolic and diastolic blood pressure during exercise on a bicycle ergometer until extreme fatigue
Blood pressure during static work.
During static work, there is a significant increase in both systolic and diastolic blood pressure.
The degree of increase in blood pressure when maintaining static forces depends on the magnitude of the force and the duration of its retention. At loads of 30% of MVC and above, blood pressure at the moment of severe fatigue (refusal to work) can reach 200/130 mm Hg. Art. The increase in blood pressure when maintaining static loads of equal relative magnitude practically does not depend on the size of the contracting muscles. Thus, with isometric contractions with a force of 40% of the MVC of the muscles adducting the thumb, forearm and shin, despite multiple differences in the size and strength of contraction of these muscles, blood pressure by the end of the work increased in all three cases to 170 180/100-110 mm
Hg. Art. A significant increase in blood pressure during static work is of great importance in increasing the blood supply to working muscles, as it promotes better blood flow through the vessels compressed by the contracting muscle.
Blood pressure during local rhythmic work.
During local rhythmic work (for example, contraction of the forearm or calf muscles alone), as well as during static work, both systolic and diastolic blood pressure increase, reaching 170-190/110-125 mm Hg during tiring loads . Art. The specific values of the increase in blood pressure depend on the intensity of the
load, that is, the strength of each contraction, the number of contractions per unit of time, the ratio of the durations of periods of contraction and relaxation.
Magnification Mechanisms
Blood pressure
during physical work.
Three mechanisms play a leading role in changes in blood pressure during muscular work: 1.
An increase in VO2
due to an increase in CO and heart rate.
An increase in IOC leads to an increase in the flow of blood through the arteries and, therefore, causes an increase in pressure in the vessels. 2. Changes in the general peripheral vascular resistance,
depending on the intensity and nature of the work, the ratio of the volumes of active and inactive muscles.
Vasoconstriction in inactive areas increases resistance to blood flow and leads to increased blood pressure. And, on the contrary, dilation of blood vessels in contracting muscles contributes to a drop in vascular resistance and a decrease in blood pressure. 3. An increase in the volume
of circulating blood due to the narrowing of venous vessels contributes to an increase in blood pressure. A decrease in blood volume due to the release of fluid from the vessels, on the contrary, leads to a slight drop in blood pressure.
The increase in blood pressure during work is due to an increase in the activity of the sympathetic-adrenal system. Activation of the sympathetic centers for circulatory regulation located in the medulla oblongata causes two effects: 1) increases the strength and frequency of contraction of the heart muscle, thus increasing the IOC; 2) causes a narrowing of arterial and venous vessels in inactive areas, contributing to a less significant drop in overall vascular resistance.
The main factors causing activation of the cardiac and vasomotor centers of the medulla oblongata are the following: 1. Irradiation of excitation from the motor zone of the cortex to the centers regulating the activity of the cardiovascular system. 2. Receipt of activating impulses to these centers from receptors located in the working muscles themselves. In other words, reflex mechanisms contribute to the increase in blood pressure during work. A very controversial role in the increase in blood pressure during muscle contraction is played by irritation of their mechanoreceptors (muscle spindles, joint and tendon receptors). It is believed that a significant contribution to the activation of the vasomotor center is made by afferent nerve fibers, the free endings of which are located in the muscle and can be excited by mechanical influences (contraction) and various chemicals released during metabolism in active muscle cells (especially potassium ions) .
So, in the regulation of systemic circulation during muscular work, the leading role is played by the increased activity of the centers of the sympathetic nervous system as a result of the influence of impulses coming from both the central nervous system and the periphery.
Cardiac output fraction and diagnosis
The concept of ejection fraction was introduced into medicine to determine the performance of the heart muscles at the time of contraction. It allows you to determine how much blood was pushed from the heart into the vessels. The unit of measurement is set to percentage.
The left ventricle is selected as the object of observation. Its direct connection with the systemic circulation makes it possible to accurately determine heart failure and identify pathology.
Ejection fraction is prescribed in the following cases:
- with constant complaints about heart function;
- chest pain;
- shortness of breath;
- frequent dizziness and fainting;
- low performance, rapid fatigue;
- swelling of the legs.
The initial analysis is carried out using ECG and ultrasound equipment.
Fraction norm
During each systolic state, the heart of a person who is not experiencing increased physical and psycho-emotional stress throws up to 50% of the blood into the vessels. If this indicator begins to noticeably decrease, insufficiency is observed, which indicates the development of ischemia, heart disease, myocardial pathologies, etc.
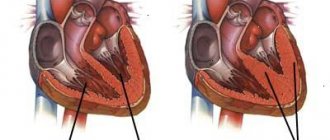
A – normal fraction, B – 45% fraction
The ejection fraction norm is 55–70%. Its drop to 45% and below becomes critical. To prevent the negative consequences of such a decline, especially after 40 years, an annual visit to a cardiologist is necessary.
If the patient already has pathologies of the cardiovascular system, then in this case there is a need to determine an individual minimum threshold.
After conducting the study and comparing the data obtained with the norm, the doctor makes a diagnosis and prescribes appropriate therapy.
Ultrasound does not reveal the full picture of the pathology and, since the doctor is more interested in identifying the cause of this disease, most often it is necessary to resort to additional studies.
Cardiac ejection fraction on ultrasound
Treatment of low fraction level
Low cardiac output is usually accompanied by general malaise. To normalize health, the patient is prescribed outpatient treatment. During this period, constant monitoring of the functioning of the cardiovascular system is carried out, and the therapy itself involves taking medications.
In particularly critical cases, surgery may be performed. This procedure is preceded by the identification of a severe defect or serious disorders of the valve apparatus in the patient.
Surgery becomes inevitable when low cardiac output becomes life-threatening for the patient. In general, conventional therapy is sufficient.
Self-treatment and prevention of low ejection fraction
To normalize the ejection fraction, you must:
- Introduce control over the liquids taken, reduce their volume to 1.5–2 liters per day.
- Avoid salty and spicy foods.
- Switch to dietary foods.
- Reduce physical activity.
Preventive measures to avoid deviations from the normal cardiac ejection fraction include:
- rejection of bad habits;
- maintaining a daily routine;
- eating iron-containing foods;
- exercises and light gymnastics.
If there is the slightest malfunction of the heart or even suspicion of these manifestations, you must immediately see a cardiologist. Timely detection of pathology greatly simplifies and speeds up its elimination.
Effective treatments
Most patients with the disease require intensive care in a hospital setting. This is associated with a high risk of life-threatening complications. Treatment of low cardiac output syndrome involves both influencing the cause of its formation and using supportive measures aimed at preventing the development of threatening consequences. In some cases, patients require surgical intervention, which is especially important for children, who are often diagnosed with congenital malformations of the valve apparatus. With a mild course of the disease, treatment at home using folk remedies is possible. However, it is recommended to use unconventional methods only after consulting a doctor.
Review of drugs
Drug support is aimed at enhancing myocardial function, normalizing vascular tone and restoring the rheological properties of blood. The following tools are used for this:
- To increase cardiac output, drugs such as Dopamine and Dobutamine are used. They have a positive inotropic effect, which helps restore normal blood circulation. The medications also have a moderate diuretic effect due to the fact that they increase perfusion in the kidneys.
- If central venous pressure decreases, infusion therapy will be required. The choice of solution is made after receiving the results of blood tests. Both crystalloids, such as Sodium Chloride and Glucose, and colloids, such as Reopoliglucin, are used.
- Cardiac glycosides, which include Digoxin and Strophanthin, help increase myocardial contractility.
- If the formation of the disease is caused by thromboembolism of the coronary vessels, fibrinolytic therapy will be required. It involves the use of medications such as Streptokinase and Heparin.