Classification
Why does heart rhythm disturbance occur and what is it? The term “arrhythmia” refers to changes accompanied by a disorder in the sequence and regularity of myocardial contractions. The beats per minute will not be constant.
The heart rhythm becomes different from sinus. It is observed normally in a healthy person. Any cause that provokes arrhythmia can lead to disruption of vital functions for which the heart is responsible.
The most widespread classification of rhythm disturbances according to Zhuravleva and Kushavsky from 1981. It includes the following variants of pathology of the cardiovascular system:
- Changes in automaticity in the sinus node (nomotopic arrhythmia): sinus bradycardia;
- sinus tachycardia;
- weak conduction of the sinus node;
- sinus arrhythmia.
- atrial heart rate;
- paroxysmal variant of tachycardia;
- fibrillation (fibrillation, flutter) of the ventricles;
- interatrial block;
- premature excitation of the ventricles;
Each disease from the listed classification has its own causes and treatment. Symptoms of heart rhythm disturbances are expressed depending on the severity of the condition and the therapy performed.
Symptoms
The types of heart rhythm disturbances were discussed in detail above. Now we should discuss the symptoms.
In fact, subjective complaints with this pathology may be completely absent for a long time. This is a problem, because when a person goes to a cardiologist, it turns out that the disease is in an advanced stage.
If any signs appear, it is usually a feeling of “fading” of the heart, as well as “shocks” and “interruptions” that occur due to increased post-extrasystolic contraction.
Often the pathology occurs against the background of vegetative-vascular dystonia. In this case, the following symptoms are observed:
- Periodic headache.
- Irritability.
- Dizziness.
- Increased fatigue.
If extrasystoles occur against the background of organic diseases, then the person is faced with a feeling of lack of air, anginal pain and weakness. Fainting may even occur.
Many symptoms are often combined with fear, anxiety, and anxiety. Due to changing hemodynamics, shortness of breath may occur (even at rest). Angina-type pain and pulse arrhythmia are common. Sometimes pulsation of the veins is noticed.
Causes of heart rhythm disturbances
When heart rhythm disturbances occur, the main focus is on finding the cause. Many types of arrhythmia are similar. You can figure out exactly what type of disorder the patient has through a comprehensive examination.
Endogenous factors
Certain diseases pose a danger to the cardiovascular system. These include the following causes of heart rhythm disturbances:
- Chronic diseases of the cardiovascular system. When symptoms of arrhythmia appear, the main importance is given to ischemic processes in the myocardium, myocarditis, previous infarction, congenital and acquired defects. In people over 40 years of age, atherosclerosis plays an important role. The deposition of cholesterol in the form of plaques on the walls of blood vessels does not allow them to maintain their elastic properties.
- Pathology of the nervous system.
- Metabolic disorders in the form of hypokalemia or hyperkalemia.
- Hormonal changes associated with thyroid diseases (hypothyroidism and thyrotoxicosis).
- Heart rhythm disturbances as one of the manifestations of cancer pathology.
In some cases, patients with glomerulonephritis or pyelonephritis also complain of interruptions in the functioning of the heart. For this reason, it is important to remember that pathology from other organ systems can disrupt the normal rhythm.
Exogenous factors
Some environmental factors (or active human activities) negatively affect the body. They cause heart rhythm disturbances, the symptoms of which may not bother a person for a long time. Factors acting from outside include:
- Age over 40 years. Most often, people in this category begin to feel unpleasant symptoms in the heart area, which are characteristic of arrhythmia.
- Intense physical activity, severe stress.
- Smoking tobacco, drinking alcoholic beverages. Toxic substances negatively affect blood vessels and myocardium.
- Traumatic brain injuries result in damage to the central or autonomic nervous system. Any symptom can have a negative effect on the heart.
- It is not recommended to drink more than 3 cups of coffee. Due to the large amount of caffeine contained, contractions accelerate and blood pressure increases. Changes in the state of the cardiovascular system can lead to arrhythmia.
- Under the influence of anesthetics, the load on the myocardium increases. This becomes one of the reasons for the disruption of its work.
In some cases, the cause cannot be determined. If the factor is not fully understood, then it is idiopathic. Predisposing phenomena are considered to be violation of the work and rest schedule, obesity, and a sedentary lifestyle.
Both adults and teenagers can get sick. The main causes of arrhythmia in a child at an early age are defects, diseases and poor heredity. In pediatrics, they give individual recommendations, depending on age.
Causes of arrhythmias
Based on the causes and mechanism of occurrence, arrhythmias are conventionally divided into two categories: those associated with cardiac pathology (organic) and those not associated with it (inorganic or functional).
Various forms of organic arrhythmias and blockades are frequent companions of cardiac pathologies: coronary artery disease, myocarditis, cardiomyopathies, malformations and heart injuries, heart failure, as well as complications of cardiac surgery.
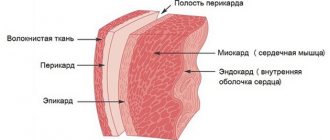
The development of organic arrhythmias is based on damage (ischemic, inflammatory, morphological) to the heart muscle. They impede the normal propagation of an electrical impulse through the conduction system of the heart to its various parts. Sometimes damage also affects the sinus node, the main pacemaker. When cardiosclerosis develops, scar tissue interferes with the conductive function of the myocardium, which contributes to the emergence of arrhythmogenic foci and the development of conduction and rhythm disorders.
The group of functional arrhythmias includes neurogenic, diselectrolyte, iatrogenic, mechanical and idiopathic rhythm disturbances.
The development of sympathetic-dependent arrhythmias of neurogenic origin is facilitated by excessive activation of the tone of the sympathetic nervous system under the influence of stress, strong emotions, intense mental or physical work, smoking, drinking alcohol, strong tea and coffee, spicy food, neurosis, etc. Activation of the sympathetic tone is also caused by diseases thyroid gland (thyrotoxicosis), intoxication, feverish conditions, blood diseases, viral and bacterial toxins, industrial and other intoxications, hypoxia. Women suffering from premenstrual syndrome may experience sympathodependent arrhythmias, heart pain, and sensations of suffocation.
Vague-dependent neurogenic arrhythmias are caused by activation of the parasympathetic system, in particular the vagus nerve. Vague-dependent rhythm disturbances usually develop at night and can be caused by diseases of the gallbladder, intestines, peptic ulcer of the duodenum and stomach, diseases of the bladder, in which the activity of the vagus nerve increases.
Diselectrolyte arrhythmias develop when there are disturbances in electrolyte balance, especially magnesium, potassium, sodium and calcium in the blood and myocardium.
Iatrogenic rhythm disturbances arise as a result of the arrhythmogenic effect of certain drugs (cardiac glycosides, β-blockers, sympathomimetics, diuretics, etc.).
The development of mechanical arrhythmias is facilitated by chest injuries, falls, blows, electric shocks, etc.
Idiopathic arrhythmias are rhythm disturbances without an established cause.
Hereditary predisposition plays a role in the development of arrhythmias.
Diseases that cause rhythm disturbances
Not only pathology of the cardiovascular system leads to dysfunction of the heart. The appearance of signs of the disease is possible if the patient has:
- atherosclerosis;
- myocarditis;
- congenital structural anomalies;
- dystrophic processes in the myocardium;
- heart attack;
- heart failure;
- pheochromocytomas;
- arterial hypertension;
- hernia in the esophageal opening of the diaphragm;
- cardiomyopathy.
Among patients, arrhythmia is more common, the main cause of which is a dysfunction of the cardiovascular system.
Myocarditis
With myocarditis, inflammation of the muscle occurs. This occurs after cardiomyocytes are damaged by infection. Heart rhythm disturbances occur under the influence of toxic substances released by microorganisms.
The clinical picture depends on the degree of change in the walls of the organ and the severity of the process. The onset may be asymptomatic. Based on pathophysiological data, even slightly damaged heart cells become the cause of arrhythmia.
Myocardial infarction
Poor circulation of the coronary vessels leads to myocardial necrosis. Foci form in a local area and cease to be active. In some cases, with arterial spasm, the same outcome occurs. A properly selected emergency care algorithm reduces the risk of complications.
One of the consequences of the post-infarction state is heart rhythm disturbance. Necrotic areas in the myocardium can be large or small.
Pheochromocytoma
The formation is a tumor localized in the adrenal medulla. It is detected in early adolescence and adulthood. The cells begin to produce catecholamines in large quantities. These include adrenaline and norepinephrine. In rare cases, the tumor turns malignant. This type of cell spreads through the bloodstream to other organs.
Pheochromocytoma always occurs with increased blood pressure. During a crisis provoked by catecholamines, it increases sharply. During the interictal period, it remains stably at high levels, or may decrease. When even a small tumor forms, the heart rhythm changes. At the prehospital stage, assistance is provided to normalize blood pressure. The patient is taken to the hospital and after examination is operated on.
Description of idiopathic tachycardia
The most basic difference between idiopathic tachycardia and other forms of arrhythmia is the appearance of the disease against the background of a person’s complete clinical health. During the studies, no changes in the myocardium, metabolic or electrolyte disturbances are detected, so it is quite difficult to prescribe treatment for an unspecified etiology of the pathological process.
In normal condition, the heart rate is 60-90 beats. Some studies have found an association between arrhythmia and the following factors:
- women have a higher heart rate than men;
- heartbeat was directly proportional to height, coffee consumption, and bad habits (smoking);
- Heart rate was inversely dependent on age, increased blood pressure, and physical activity.
The lack of clear mechanisms of disease development often makes it impossible to accurately and quickly establish the correct diagnosis. Nevertheless, with the help of modern diagnostic methods, it is possible to prescribe effective treatment to patients with idiopathic tachycardia.
Manifestations of heart rhythm disturbances
Manifestations and signs of arrhythmia depend on the variant of the disease according to the classification. Some patients feel well and in rare cases unpleasant signs appear in the heart area. Prolonged asymptomatic course negatively affects the myocardium, and this condition is difficult to detect at an early stage.
Atrioventricular block
When the normal function of the atrioventricular node is disrupted, an imbalance occurs between the atria and ventricles. The conduction of the impulse becomes more difficult, and the heartbeat slows down. The frequency of myocardial contractions is about 25-45 per minute. The following symptoms are characteristic:
- severe weakness due to bradycardia;
- dyspnea;
- dizziness;
- darkening of the eyes;
- fainting;
Atrioventricular block is characterized by episodes of loss of consciousness. Fainting lasts about a few seconds.
Atrial fibrillation (flicker)
This type of arrhythmia is more common than others. She was assigned an ICD code - I 48. The heart rate can be up to 600 beats per minute. The process is not accompanied by coordinated work of the atria and ventricles. Patients describe a sharp deterioration in their health. Some of them indicate the minutes of such changes.
It all starts with feelings of strong heartbeat, irregularities and weakness. Gradually, shortness of breath, a feeling of fear and pain in the chest area develop. When atrial fibrillation occurs, the condition worsens sharply. Everything takes just a few minutes. During this time, the feeling that “my heart will soon jump out of my chest” does not leave me.
Sick sinus syndrome
This type of arrhythmia is associated with a disorder of impulse formation in the sinus node and subsequent conduction in the atria. Bradycardia appears normally in healthy people who are trained in sports.
People feel pauses during the work of the heart, and the pulse increases. When the syndrome is severe, there is a tendency to faint, which is preceded by darkening of the eyes or a feeling of heat.
Extrasystole
Under the influence of various factors, the conduction system of the heart generates extraordinary contractions of the myocardium (extrasystoles). Single manifestations are not life-threatening and are rarely felt by people. When there are many of them or they become grouped, patients begin to complain. They experience a rapid heartbeat, and there is a pause between individual beats, which people describe as freezing.
Diagnosis of pathology
Before starting to treat the patient, a complete examination is carried out. It includes the implementation of laboratory and instrumental methods. After receiving the conclusion, the doctor determines further tactics for managing the patient, depending on individual characteristics.
Blood analysis
This examination option is one of the most accessible methods. It includes parameters by which the likelihood of an inflammatory process is determined. This can be done by assessing the level of white blood cells in the blood and the erythrocyte sedimentation rate (ESR). It is also important to study biochemical analysis. The electrolyte composition plays an important role for the normal functioning of the myocardium. An imbalance of potassium and magnesium in the bloodstream leads to arrhythmia.
Lipid profile
This type of examination is necessary for all patients. If there is a rhythm disturbance, the condition of the vascular wall must be assessed. Based on the results obtained, the doctor begins treatment. If there are very few high-density lipids, and the limits of bad cholesterol exceed the permissible values, therapy is necessary.
ECG (electrocardiography)
The instrumental method is considered one of the main ones for determining heart rhythm disturbances. Any disorders occurring in the myocardium will be reflected on the film. Electrocardiography (ECG) reveals the following:
- The source of rhythm, whose task is to form impulses.
- Heart rate.
- Impaired conduction from the atria to the ventricles.
- Possible extraordinary contractions of the myocardium.
- Fibrillation or flutter of the ventricles and atria.
In a number of patients, using this examination, it was possible to detect changes that did not manifest themselves in any way.
Holter ECG
Using a modern research method, it is possible to detect changes that were detected by an electrocardiogram. The advantage is to carry it out within 24 hours. All this time, a sensor is attached to the patient, which takes all indicators of cardiac activity.
The patient is advised to lead a normal lifestyle. So that he does not miss any little detail regarding the activity, a diary is kept. On its pages, the subject records his workload, stress and other parameters that the doctor recommends. The next day he returns to his cardiologist to evaluate the results.
Event monitoring
This type of study is carried out using a portable device for recording an electrocardiogram. The convenience of the method lies in its use only when necessary. The indications are:
- pain in the heart area;
- strong heartbeat;
- feeling of interruptions;
- feeling of freezing;
- the appearance of dizziness and severe headache;
- pre-fainting state.
After recording data at the required moment, the patient can transmit information to his doctor by telephone using a sound sensor.
Treadmill test
During normal physical activity or with severe stress, patients experience pain. Sometimes it is difficult to assess the indicator, and for this reason stress tests are prescribed. The patient gets on the treadmill, and the doctor sets the required pace.
If there are no changes, then the angle of its inclination is changed and the speed is increased. If pain, interruptions and other unpleasant sensations occur, the procedure is completed and the data obtained are evaluated. When a heart rhythm disorder is confirmed, treatment is prescribed.
Tilt test
This procedure is a variation of the one described above. Its essence is to carry out orthostatic load. Before the study begins, the patient is placed on a special table. It is fixed with belts and transferred from a horizontal to a vertical position. During the implementation process, the following indicators are assessed:
- blood pressure level;
- ECG changes;
- cerebral hemodynamics.
If fainting occurs, the cause is determined using a tilt test.
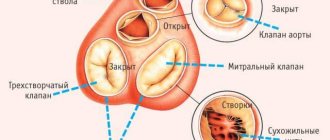
EchoCG (echocardiography)
The study makes it possible to assess the condition of the structural elements of the heart, the level of blood flow, and pressure in the vessels. If there are changes due to age or infectious disease, even minor deviations can be considered.
Electrophysiological research method
To assess the condition of the heart, an electrode is inserted through the nasal passage into the esophagus (transesophageal echocardiography). If it is impossible to perform it in the indicated way, the procedure is done intravenously. The sensor enters the cavity, and the doctor gives a slight impulse. It provokes an attack of arrhythmia.
Ultrasound of the thyroid gland
The presented method is prescribed to each patient with arrhythmia. The cause of this condition may be due to altered thyroid function. If the patient has a reduced rate, then bradycardia and blockade occurs, which is easy to detect using an ECG. With hyperthyroidism, tachycardia and extrasystoles are noted.
Treatment of heart rhythm disorders
The choice of treatment method is based on the causes of arrhythmia, clinical manifestations, and concomitant diseases. It includes several options:
- medicinal;
- non-medicinal.
If there is no effect, treatment of cardiac arrhythmias is carried out by cardiac surgeons.
Medication method
To choose the right product, a comprehensive examination is carried out. The results of treatment with antiarrhythmic drugs are assessed under the control of electrocardiography. The following classes of drugs are prescribed (depending on indications):
- Drugs that stabilize cell membranes (class 1) - Lidocaine, Quinidine, Propafenone.
- Beta-blockers (class 2) - Metoprolol, Atenolol.
- Potassium channel blockers (class 3) - Amiodarone, Sotalol.
- Calcium channel blockers (class 4) - Verapamil, Diltiazem.
The patient is under the supervision of a doctor, and if necessary, he must undergo tests. Depending on the psychosomatics and the patient’s attitude towards his health, a consultation with other specialists is prescribed. According to indications, additional funds may be needed. They should go well with anti-arrhythmia tablets.
Non-drug treatment
If therapy is successful and the condition returns to normal, then folk remedies can be prescribed. For this purpose, medicinal herbs are used, which are mixed in a certain ratio. Valerian root, lemon balm, motherwort and anise are widely used. The ingredients are combined, poured with boiling water and left for about half an hour. Then the resulting infusion is taken in a dose of ½ glass three times a day.
One of the treatment methods is proper lifestyle and nutrition. It is necessary to give up tobacco, alcoholic beverages and junk food. To keep your heart healthy, it is recommended to drink water (1.5-2 liters per day). If there is swelling, then this issue is resolved with the attending physician.
The diet should contain a lot of fresh vegetables and fruits. Bananas, dried fruits and baked potatoes are considered especially beneficial for the myocardium. They are richer in potassium than other foods, which is necessary for heart function.
If there is no improvement in treatment at home, the patient is referred for surgery. The most common and effective are:
- cardioversion;
- placement of an artificial pacemaker;
- ablation;
Cardioversion is indicated for patients with ventricular arrhythmia. The method is based on the use of an electrical discharge. It is important to carry out a correct differential diagnosis. If the form of conduction disturbance turns out to be atrial, then the procedure will be contraindicated. This is due to the high likelihood of blood clots.
If the heart cannot cope with the problem on its own, then an artificial pacemaker is installed under the skin. If a source of arrhythmia is detected, a catheter is inserted, the task of which is to destroy it - ablation. This treatment method will return the patient to a full life.
Complications of heart rhythm disturbances
The danger of arrhythmia lies not only in the disruption of blood flow in vital organs. If left untreated, consequences may include:
- Myocardial infarction. During an attack of arrhythmia, the heart contracts at an accelerated rate and sometimes the coronary vessels cannot cope with the load.
- Stroke. The formation of blood clots is associated with disruption of the myocardium. Over time, clots form that can enter the vessels of the brain and lead to circulatory disorders in it.
- Ventricular fibrillation. A complication develops with tachycardia, which turns into atrial fibrillation. The myocardium loses its ability to contract, and blood does not flow through the vessels to the organs. After a couple of minutes, cardiac activity stops and clinical death occurs. If assistance is not provided in a timely manner, it becomes biological.
In some cases, there are patients with rhythm disturbances that have a lightning-fast course. These consequences of the disease develop quickly, and it is impossible to provide assistance at the prehospital stage in time. This type of development refers to sudden cardiac death.
Forecast
The prognosis for life and health is favorable with early diagnosis and treatment. If complications and concomitant pathology are present, then it is assessed based on the degree of severity, the form of arrhythmia, and the dynamics of the condition after therapy.
Patients at risk of heart rhythm disturbances should remember this and avoid factors that provoke this condition. If the unpleasant symptoms mentioned above appear, it is necessary to undergo a comprehensive examination. Early treatment will help maintain health and avoid complications.
Etiology
According to this criterion, heart rhythm disturbances such as ventricular extrasystole are of the following types:
- Organic. The most complex type. It is caused by trophic changes in the myocardium, heart defects, coronary disease, cardiosclerosis and coronary insufficiency.
- Toxic. The prerequisites in this case are pathological changes occurring in tissues, as well as metabolic disorders directly in the heart muscle. This is caused by the abuse of certain groups of medications, coffee, alcohol, as well as narcotic and toxic drugs.
- Vegetative (functional). They are formed due to vegetative-vascular dysfunction, neurogenic disorders, neuroses and psycho-emotional disorders. Also, the prerequisites are often gastrointestinal pathologies, hormonal imbalances and osteochondrosis.
- Ideopathic. The most controversial type of heart rhythm disorder. Because extrasystole of this form occurs in an absolutely healthy person, when there are no objective reasons for this.
It is important to note that not all types of disorders are manifested by specific symptoms, but it is quite possible to diagnose each of them using echocardiography.