0
Author of the article: Marina Dmitrievna
2017.06.12
258
Arrhythmia
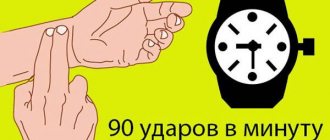
The human heart is a kind of pump that pumps blood through the body’s vascular system. This organ performs about 100 thousand contractions in 24 hours. Contractile function is supported by the conduction system. For a healthy body, the resting contraction frequency ranges from 60 to 90 beats per minute. If deviations from this indicator are noted, then we can safely talk about a violation of the human heart rhythm.
General information about heart rate acceleration and deceleration
What is a heart rhythm disorder, and is emergency help needed? This condition is a deviation from the normal frequency of contraction of a healthy organ (slow or rapid heartbeat). Another manifestation may be an incorrect sequence of heart contractions.
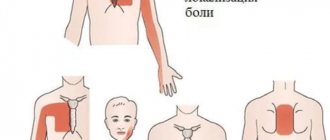
Chest pain is one of the signs of a heart rhythm disorder
The fact that the heart rhythm is disturbed is indicated by:
- Bad feeling. It is expressed by dizziness and frequent shortness of breath (the same symptom is also characteristic of primary cardiomyopathy).
- Pain in the chest area. They are oppressive in nature.
- Interruptions in the functioning of the heart muscle, fluttering, strong heartbeats.
- Excessively fast or rare pulse.
Sometimes you may feel a strange feeling as if the ground is falling away under your feet. Cases of loss of consciousness are common. Vomiting or nausea occurs. They are observed when the position of the body in space changes.
The pathogenesis of different heart diseases is different. However, manifestations of this kind during arrhythmia do not always indicate disturbances in the functioning of the heart. They are also treated in their own way, depending on the complexity and course of the disease.
Note! It often happens that patients suffering from tachycardia do not feel any discomfort, but the disease can be fatal. But some patients with minor illnesses may even lose consciousness and take pills, drops and other medications.
What determines the development of heart disease?
Risk factors for the disease are as follows:
- Age category. The older a person gets, the more worn out their blood pump becomes. The heart ages and weakens. Atrioventricular nodal rhythm, bradycardia. Extrasystoles or other disturbances in the functioning of the heart can occur at any time. Moreover, all the diseases that have accumulated over life will only worsen the situation. Older women are characterized by “broken heart syndrome” (a variant of cardiomyopathy), which is often accompanied by rhythm disturbances.
Weak heartbeat
- Genetics. A predisposition to developing a heart block or other ailment is one of the main risk factors. If a person has congenital anomalies, then secondary cardiovascular pathologies occur many times more often. This disrupts the frequency and rhythm of the heartbeat.
- Diseases of the heart muscle. The condition can be affected by myocardial infarction, scar formation, and sclerosis.
What to do if the rhythm is disrupted - read on.
Does rhythm turbulence in HF have the same importance as in ischemic heart disease for arrhythmic risk stratification? How is turbulence slope measured? Thanks in advance,
Luis Manuel Gomez Saenz
Dear Dr. Luis Manuel Gómez Saenz! Heart rate turbulence (HRT) is a new method (1999) for assessing the functioning of the autonomic nervous system (ANS), which is used to predict sudden cardiac death (SCD). TSR is a physiological biphasic response of the sinus node to PVCs. This response consists of a short initial acceleration followed by a deceleration of the heart rate. Quantitative assessment of TSR is carried out using 2 parameters: 1) The Turbulence Onset; 2) The Turbulence Slope. TCP is a statistically significant predictor of the likelihood of death from cardiac disease after AMI. TCP can predict the risk of SCD and death not only in patients after AMI, but also in patients with other heart diseases. The mechanism of TSR is not yet fully understood. Apparently, TSR is an autonomic baroreflex. PVC leads to a short-term change in blood pressure (low amplitude during extrasystole, high amplitude during subsequent normal contraction). During normal functioning of the ANS, such changes are immediately recorded with an immediate response in the form of TSR. When activity is disrupted, this reaction is weakened or even completely absent. TSR can be used for risk stratification after AMI. In an analysis of 3000 patients who suffered an AMI, TSR was found to be an independent risk predictor (the most powerful ECG risk predictor). The predictive value of TSR is comparable to that of LVEF! In moderate-severe HF, turbulence is observed after running non-sustained VT and this is associated with prognostically important indices of TSR and EF. TSR (VT) is similar to TSR, but the onset of turbulence (VT) is shifted to more positive values than the onset of turbulence (non-VT). TSR (VT) may have prognostic significance. 1)The Turbulence Onset (TO): This is the percentage difference between the heart rate following the PVC and the heart rate before the PVC. TO is calculated as follows: TO = ((RR1 + RR2) - (RR-2 + RR-1)) / (RR-2 + RR-1) * 100 while RR-2 and RR-1 are the first 2 normal interval before the PVC, and RR1 and RR2 are the first 2 normal intervals subsequent to the PVC. First, the TO is determined for each PVC, and then the resulting values are averaged. Positive Turbulence Onset values indicate a slower, and negative values indicate an accelerated sinus rhythm. 2) The Turbulence Slope (TS: To determine TS (ms/RR), the slope of changes in RR intervals is calculated using straight regression lines for every 5 RR intervals out of 20 following a compensatory pause. The algorithm for calculating TSR can give useful results if the trigger event was true PVC (not a T wave artifact).In addition, one must ensure that the sinus rhythm before and after the PVC is free of arrhythmias, artifacts, or other spurious phenomena.To meet these requirements, filters are used that exclude RR intervals with the following characteristics:• intervals < 300 ms • > 2000 ms • > 200 ms difference from the previous sinus interval • > 20% difference from the normal interval (from the average of 5 consecutive sinus intervals) In addition, those ECG recordings in which there are PVCs are allowed for TSR assessment with a prematurity index >20% and a post-extrasystolic interval that is longer than the average RR by 20% or more.To calculate the average TSR tachogram value, the TSR algorithm requires at least 15 normal intervals after each PVC. The concept of TSR was first formally proposed by Georg Schmidt and colleagues from the Munich University of Technology in 1999 in the Lancet journal. In a study of the characteristics of PVCs, Schmidt et al found that heart rate increased after PVCs. To get a clearer picture, they determined the fluctuations in the intervals between contractions (RR intervals) and synchronized these intervals with the PVCs and the average values of the intervals. A graph of these averaged RR intervals (called a PVC tachogram) not only confirmed the fact that the heart rate increases after a PVC, but also highlighted another, less obvious characteristic - the heart rate slows down, regardless of the heart rate before the PVC. If Schmidt et al had left it at that, they would have been able to use these findings only as interesting notes in an educational text on ECG. However, this group of researchers thought that patients at higher risk of death after AMI had decreased HRV. They drew an analogy with TSR. The researchers tested this hypothesis using 24-hour CM in 100 MI survivors with frequent PVCs. Apparently, more severe turbulence was associated with a better diagnosis. The researchers used these data to determine the optimal threshold values for differentiating normal and pathological TSR values and came up with the following data: TS=2.5, TO=0%. Can TSR and these thresholds function in the real world? These threshold values were used in the HM of 1191 patients who suffered a MI. During the 2-year follow-up period, there were 162 deaths (13.6%). It turned out that the risk of death in patients with impaired TSR was 3 times higher than the risk in patients with normal TSR. This is how TSR was born.
All the best,
Andrés Ricardo Pérez Riera MD and Master in Cardiology Area In Charge of Electro-Vectocardiology Sector of the Discipline of Cardiology, ABC Faculty of Medicine (FMABC), Foundation of ABC (FUABC) – Santo André – São Paulo – Brazil.
To determine TSR, sinus rhythm with PVCs is required. However, as HF progresses, the incidence of AF increases, reaching 50% in patients with class IV. So, what is the use of a method that cannot be used in the majority of these patients? In addition, the prognosis of patients with a combination of HF and AF is worse than that of patients without AF. Please comment on this fact. Best regards, Maciej Sosnowski MD, PhD Katowice Poland
Dear Luis Manuel Gomez Saenz and Andres Ricardo Perez Riera,
An analysis of 2 large studies of TCP in patients with HF showed that this method does not stratify the risk of sudden cardiac death, although it is associated with non-sudden death. UK-HEART trial (Moore RK, Groves DG, Barlow PE, Fox KA, Shah A, Nolan J, et al. Heart rate turbulence and death due to cardiac decompensation in patients with chronic heart failure. Eur J Heart Fail. 2006 Oct; 8(6):585-90) included patients with HF (74% with CAD and 26% with non-ischemic cardiomyopathy), and the MACAS trial (Grimm W, Schmidt G, Maisch B, Sharkova J, Muller HH, Christ M. Prognostic significance of heart rate turbulence following ventricular premature beats in patients with idiopathic dilated cardiomyopathy. Journal of cardiovascular electrophysiology. 2003 Aug;14(8):819-24) – patients with idiopathic dilated cardiomyopathy. In multivariate analysis of these trials, no statistical significance was achieved between turbulence onset and slope indices and sudden cardiac death. These 2 indices assess rhythm variability after PVCs. Mean values of these indices were assessed in longitudinal registers. It would be interesting to study them in short-term registers as well. For those interested in the topic of HRV, I recommend reading the review by Sandercock and Brodie (PACE 2006; 29:892–904). They conducted a systematic review of HRV in patients with HF. Sincerely,
Marcos Sousa Programa de Pós Graduação e Serviço de Cardiologia do Hospital das Clínicas da Universidade Federal de Minas Gerais.
Dear Dr. Marcos Sousa from Minas Gerais Brasil, In a recent trial including patients with HF (82% class II), TSR reflected the severity of HF and the degree of LV dysfunction (based on clinical, echocardiographic and biochemical parameters). Patients with FC III had a lower rise in turbulence and a more pronounced onset than patients with FC II. Significant correlations were found between TSR and LVEF as well as with LV diameters. Turbulence slope was also associated with N-terminal-pro-BNP levels. Multivariable analysis showed that impaired TSR parameters are independent predictors of HF severity in patients with class III and LVEF <40%.(1). TSR is a predictor of prognosis in patients with DCM and also in patients with HF of mixed etiology. TSR has also shown predictive value for revascularization therapy in MI (2). The multicenter REFINE (Risk Estimation Following Infarction - Noninvasive Evaluation Study) trial (n = 322 patients) enrolled patients with LVEF <0.50 during the first week after acute MI and followed them for 47 months. The identifiers of high-risk patients in this trial were: TMR, T-wave alternans, and LVEF < 0.50, 8 weeks after AMI (3). All of these patients received optimal medical therapy. In addition, in Chagas disease, UNFORTUNATELY for our disease, TSR correlates well with LVEF and SDNN. The high incidence of PVCs in this group of patients also indicates the utility of TSR (4).
Bibliography
1) Cygankiewicz I, Zareba W, Vazquez R, et al. Relation of heart rate turbulence to severity of heart failure. Am J Cardiol. 2006; 98:1635-1440. 2) Watanabe M.A., Schmidt G.Heart rate turbulence: a 5-year review. Heart Rhythm. 2004; 1:732-738. 3) Exner DV, Kavanagh KM, Slawnych MP, et al. Noninvasive risk assessment early after a myocardial infarction the REFINE study. J Am Coll Cardiol. 2007; 50: 2275-2284. The Canadian study was led by Derek Exner, MD, University of Calgary Associate professor of Medicine, Libin Cardiovascular Institute of Alberta. 4) Tundo F, Lombardi F, Rocha MC, et al. Heart rate turbulence and left ventricular ejection fraction in Chagas disease. Europace. 2005;7:197-203. I think more time and more research is needed. This method is still very young, it is only 8 years old!!!
Best wishes to you,
Andrés Ricardo Pérez Riera MD and Master in Cardiology Area In Charge of Electro-Vectocardiology Sector of the Discipline of Cardiology, ABC Faculty
Dr. Sosnowski asked an interesting question. It is true that the full benefit of biventricular pacing cannot be obtained in patients with AF. Effective CRT is possible with an adequate ventricular response rate, which is why difficulties arise in patients with chronic AF. Effective CRT is possible if rhythm control (from the LV or RV) is at least 90%. If adequate heart rate control cannot be achieved with medication, AV node ablation can be considered. This approach produces good results in a group of patients with AF who may potentially benefit from CRT. (See: Gasparini M. J Am Coll Cardiol. 2006;48:734-43). Brian
Brian Olshansky, MD Professor of Medicine University of Iowa Hospitals 200 Hawkins Drive 4426a JCP Iowa City, IA 52242 Office: 319-356-2344 Cell 319-331-0342
Dear Dr. Olshansky, I agree with you regarding AV node ablation before CRT implantation in patients with AF. However, I would like to know if TSR is of any value in patients with HF, since AF is predominant in these patients. In other words, is there another non-invasive method to help with prognosis and decision making in patients with HF, both in sinus rhythm and in AF? Moreover, such a method would facilitate better selection of potential candidates for CRT-D. Best regards, Maciej Sosnowski MD,PhD
Types of rhythm disturbances
First, it’s worth understanding what your heart rate is. It should be sinus and uniform. In this case, every beat, contraction of the myocardium comes from the sinus node. This impulse is transmitted further downward. A normal heartbeat is characterized by the same periodicity.
The classification of rhythm disturbances is as follows:
- Incorrect impulse formation. If it comes from the sinus node, but at the same time has an increased frequency, sinus tachycardia develops. In this case, the heart rate reaches 91 (rapid heart rate) beats or more. In situations where the pulse is less than 60 (slow heart rate), we speak of bradycardia. Doctors also include a condition such as respiratory arrhythmia as rhythm disturbances, but it is not considered a deviation.
The source of excitation may be in the wrong place. Then it is called ectopic. In this case, impulses arise in those parts of the circulatory system that are located lower, for example, in the atria, in the atrioventricular node, or even in the ventricles of the heart. The impulses from this focus diverge downwards or upwards.
Do not rely on pills and other drugs
The frequency of the ectopic pulse is usually slower than the sinus pulse. Paroxysmal tachycardia also occurs. This type of heart rhythm disturbance is atrial, ventricular or atrioventricular in nature.
- Blockades are bradysystolic heart rhythm disturbances. To understand what they are, it’s worth giving them a brief description. All of them are associated with incorrect conduction of the heart. The impulse is blocked as it passes through any part of the circulatory system. There are several types of the disease: bundle branch block, SVC syndrome (Wolf-Parkinson-White), ventricular asystole, etc.
Important! The latest diagnosis means cardiac arrest, so you should immediately call an ambulance and begin resuscitation measures!
- A combination of several varieties. There are situations in which ectopic and atrioventricular rhythm are noted. In this case, one of the types of heart block occurs.
What is heart rate?
Heart rhythm is the main characteristic of the heart, one of the important indicators of the organ’s functioning, by which the presence of pathology can be determined. It indicates how often the heart muscle contracts and at what intervals this occurs. Heart rhythm is characterized by the frequency of heart contractions per unit time, as well as the duration of the break between contractions.
If the heart muscle contracts evenly, each cardiac cycle (sequential contraction and relaxation) takes the same amount of time - the rhythm is normal. If the duration of several cycles is not the same, there are rhythm disturbances.
The heart rhythm is set by cells in the sinus node (this part of the heart is called the Keith-Fluck node) - pacemakers that generate impulses.
The impulses are then transmitted to muscle cells, causing them to contract and subsequently relax. Since the heart is formed by muscle cells that have a high ability to contract, impulses affect the entire organ, causing it to contract rhythmically and pump blood.
What causes arrhythmia
There are many diseases that lead to heartbeat disturbances. Doctors divide all possible causes into several groups, which they consider when diagnosing or immediately before treating the disease:
- Diseases of blood vessels and the heart itself. This includes congenital and acquired defects, heart attacks, arterial hypertension, rheumatic carditis, pericarditis, myocarditis and heart failure.
- Disturbances in the functioning of the nervous system. Provocateurs of altered heart rhythm can be VSD, neuroses of varying complexity, strokes, tumors and even brain injuries.
Avoid drinking alcohol if you have cardiac arrhythmias
- Endocrinology. Diabetes mellitus, thyroid dysfunction, PMS and menopause in women contribute to the development of heart rhythm disturbances.
- Problems with the gastrointestinal tract also affect the rhythm of the heart. First of all, cholecystitis and pancreatitis are considered provocateurs. Next on the list is a hiatal hernia.
It is worth noting that in the case of severe organic damage to the heart, the most dangerous phenomena associated with arrhythmia occur.
Causes of alpha rhythm disturbance
Disturbances of the α-rhythm are observed primarily in people who have crossed the sixty-year mark.
This is explained by a deterioration in blood circulation in the brain and is accompanied by a decrease in the amplitude of the waves. In addition, changes in brain activity indicators may be accompanied by the following pathologies:
- essential hypertension, epilepsy, including that developed due to drug use (in such situations, direct asymmetry of frequency and amplitude in the left and right hemispheres of the brain is diagnosed);
- hypertension (manifested by a decrease in rhythm frequency);
- oligophrenia (accompanied by increased activity of α-waves);
- tumors of various origins, cysts, pathologies of the corpus callosum (characterized by asymmetry between the cerebral hemispheres, reaching 30%);
- deterioration of blood circulation.
For information: in order to assess alpha activity in vegetative-vascular dystonia, depression, head injuries, dementia of various origins, disorders of the emotional-volitional sphere, hypertension, headaches, vomiting, an electroencephalogram is used.
Who to contact, what to take with you for examination
We figured out what a heart rhythm disorder is. Now it’s time to talk about who should be worried in this situation. Two doctors will help solve the problem:
- arrhythmologist;
- cardiologist.
For any heart rhythm disturbances, they are the ones to turn to. If you have previously performed any examinations, be sure to take the results with you to the consultation; you will need a complete medical history. If the necessary studies are not performed for one reason or another, they will be prescribed by an arrhythmologist or cardiologist.
Rapid heartbeat can be a concern for pregnant women
A qualified doctor will carry out the necessary procedures, prescribe treatment, and answer the question of why the normal functioning of the heart is disrupted and how the syndrome arose. It is important not to consult self-taught and non-doctors on medical portals. They do not always accurately determine the disease and can only harm the patient’s condition.
It is worth understanding that each illness is provoked by certain factors and differs in its characteristic manifestations. Determining the symptoms and factors why a junctional rhythm, tachycardia or arrhythmia occurred is the prerogative of a certified physician. You should not self-medicate. This is the first stage on the path to recovery.
If you have a feeling of anxiety for yourself or a loved one, then you should insist on regularly visiting a cardiologist. Heart rate turbulence can only be diagnosed with constant monitoring. To do this, you only need to see a doctor a few times a year. This way, it will be possible to notice in time what factors cause rhythm disturbances, their nature, and whether the patient has heart pathologies. other organs, or it is an idiopathic rhythm disorder.
Symptoms that accompany arrhythmia
The presence of heart disease leads to a gradual weakening of the heart muscle and the sinus node itself, which produces impulses.
This is accompanied by characteristic symptoms:
- Fatigue;
- Dizziness;
- Loss of consciousness;
- Signs of heart failure;
- Impairment, confusion;
- Chest pain;
- Feeling of shortness of breath, difficulty breathing;
- Feeling of panic during an attack.
How to diagnose and treat the disease
The most common method of cardiac diagnosis is electrocardiography. The ECG shows all changes in the functioning of the myocardium. In addition to stationary instruments, mobile equipment is also used to monitor cardiac processes. A Holter device allows you to view and record everything that happens to the heart for several days.
An ECG will help diagnose the disease
Sometimes this technique does not bring the desired results. In this case, the junctional rhythm is tachycardia. Bradycardia or extrasystole will help detect EPI - electrophysiological study. Now this method is considered the most accurate and reliable in assessing the normal functioning of the heart. Such a diagnostic tool allows the attending physician to correctly select the required therapy.
Treatment Options
Most medical institutions use high cardiac technologies to combat the disease. Today, patients are offered gentle, low-traumatic interventions. The most appropriate model is selected based on the examination results and the syndrome itself. The doctor will provide all the necessary information about the disease, conduct a consultation, and prescribe treatment:
- taking medications;
- pacemaker implantation;
- catheter ablation (discussed below);
- surgical intervention;
- implantation of a cardioverter (special defibrillator).
Note! A complete list of methods for eliminating acute life-threatening disorders is not always used. The technique may include one described option or several.
Catheter ablation of the posteromedial ganglion plexus
It is extremely important to follow all the requirements and recommendations of the doctor. It is worth informing him about the course of the disease, his well-being and even the most minor changes.
Application of catheter ablation
It happens that it is difficult to limit yourself to medications used to treat an illness due to their ineffectiveness. In such cases, the radiofrequency ablation method is used in world practice. What is this procedure? This is a low-traumatic operation with which you can forget about arrhythmia forever. With its help, the cause of the disease is eliminated, and not individual symptoms.
Most often, this is resorted to immediately after the electrophysical examination procedure. Surgical treatment is as follows. After identifying the source of the disease, the doctor locally releases a high-frequency electrical discharge. An impulse of such strength is enough to eliminate the tissue that leads to heart rhythm disturbances. This operation is considered one of the safest in modern medicine.
For the first time, such a surgical intervention was tried in the Russian Federation in 1997 within the walls of the Tyumen Cardiocenter. Now, the effectiveness of all procedures aimed at treating heart rhythm disorders has increased significantly, reaching a new level of accuracy. Advanced equipment and software allow you to see a three-dimensional three-dimensional image on the screen. This provides doctors with the opportunity to observe all spatial features of the patient’s body. Therefore, such tools are indispensable in correction.
Pulmonary vein isolation
One of the procedures aimed at eliminating the disorder is pulmonary vein isolation. This is an advanced technique for combating arrhythmia in surgery. It helps to cure even such serious diseases as paroxysmal atrial fibrillation. This operation minimizes the risk of relapse. Therefore, after its introduction, the number of medications on the market decreased.
It is worth understanding that heart rhythm disturbances are life-threatening changes in the human body. Under no circumstances should you delay diagnosis and treatment! If you have any suspicion, you should immediately consult a doctor. If endovascular surgery is required, it is better to trust your cardiologist and agree to the operation.
Posts
Creative cardiology. 2013; 2:5-14
Cardiac surgeon, scientist, teacher and organizer of science, Doctor of Medical Sciences (1973), Professor (1982), Academician of the Russian Academy of Medical Sciences (1994), Academician of the Russian Academy of Sciences (2011), Honored Scientist of the Russian Federation (1994) , laureate of the Lenin Prize (1976), State Prize of the USSR (1986), State Prize of the Russian Federation (2002), Prize of the Government of the Russian Federation (2003).
In 1994, L.A. Bokeria was elected by competition to the position of director. A.N. Bakuleva. In 1998, he simultaneously became director of the Center for Surgical and Interventional Arrhythmology of the Ministry of Health of the Russian Federation.
Since 1994, he has been the head of the Department of Cardiovascular Surgery at the Russian Medical Academy of Postgraduate Education (RMAPO) of the Ministry of Health of the Russian Federation. Since 1995, he has been the head of the Department of Cardiovascular Surgery No. 2 of the Moscow Medical Academy (now the First Moscow State Medical University), which he created. THEM. Sechenov Ministry of Health of the Russian Federation.
Since 2003, he has headed the Department of Cardiovascular Surgery and Interventional Cardiology at the Moscow State Medical and Dental University. A.I. Evdokimov Ministry of Health of the Russian Federation.
On the initiative of L.A. Bokeria has a successfully functioning educational and research center, which annually conducts 4–6 courses of postgraduate advanced training for senior specialists.
L.A. Bokeria performs the entire known arsenal of heart surgeries for a wide variety of pathologies: from 3 to 6 operations per day, that is, from 700 to 900 operations using artificial circulation per year.
Since 1996, he has been the chief cardiac surgeon of the Ministry of Health of the Russian Federation.
L.A. Bockeria is the author and co-author of over 3,700 scientific publications, including more than 250 books, more than 100 inventions and utility models, more than 300 computer programs and databases, a number of which are registered abroad, on various problems of cardiovascular surgery, cardiology, medicine education and organization of medical science.
L.A. Bockeria owns unique works on the theoretical substantiation and clinical use of the hyperbaric oxygenation method in heart and vascular surgery. He is a leading specialist in the field of diagnosis and surgical treatment of cardiac rhythm and conduction disorders (especially tachyarrhythmias), including various combinations of cardiac arrhythmias with congenital and acquired heart defects and anomalies, coronary disease.
L.A. Bokeria is the initiator of the development of another new section of cardiac surgery in our country - minimally invasive heart surgery. L.A. made a great contribution. Bockeria in solving the problem of surgical treatment of coronary artery disease.
The role of L.A. is great. Bockeria in the development of new approaches to surgical treatment of terminal heart failure. His merit is the development of new operations in a severe category of cardiac surgical patients with various forms of cardiomyopathies. He was the first to develop the concept of dynamic cardiomyoplasty, including in children. L.A. Bockeria performed the first implantation of an artificial heart ventricle in our country and, after a long break, initiated the resumption of heart transplant operations at the Center.
On the initiative of L.A. Boqueria introduced advanced technologies for diagnosis and reconstructive surgery of diseases of the ascending aorta and arch into clinical practice.
He generated the development of another direction of modern medical science - creative cardiology, which determines the need for creative cooperation between doctors of different specialties: cardiologists, cardiac surgeons, specialists in functional diagnostics, fundamental and applied disciplines.
Under the leadership of L.A. At the Boqueria Center, new high-tech principles for the prevention and treatment of patients with cardiovascular pathology are being developed and introduced into clinical practice - the use of gene and cell therapy methods.
Academician L.A. Boqueria is conducting priority research on the creation of bioprosthetic heart valves for the correction of valve defects - a low-profile, curved bioprosthesis of the mitral and tricuspid valves, reproducing the natural shape of the fibrous ring, on an elastic frame. The study of the effectiveness of myocardial protection in children of the first year of life with the use of a new intracellular cardioplegic solution “Bokeria-Boldyreva”, created under the leadership of L.A., continued. Boqueria.
L.A. Boqueria is actively involved in the methodology of medical science and teaching activities. He is the founder of the country's largest cardiac surgery school, having trained more than one generation of doctors - cardiac surgeons, cardiologists, resuscitators and specialists in other related specialties.
L.A. Bockeria is the scientific supervisor of 350 candidate dissertations and a consultant of more than 100 doctoral dissertations. He is the creator of the publishing house. A.N. Bakuleva with the printing house, founder and editor-in-chief of the journals “Annals of Surgery”, “Bulletin im. A.N. Bakulev “Cardiovascular diseases”, “Childhood diseases of the heart and blood vessels”, “Clinical physiology of blood circulation”, “Annals of Ari, information collection “Cardiovascular surgery”; Editor-in-chief of the journal "Thoracic and Cardiovascular Surgery".
Active work of L.A. Boqueria and his contribution to domestic healthcare have been awarded titles and awards of the highest value. He is a laureate of the Lenin Prize (1976), two State Prizes (1986 - USSR, 2002 - Russian Federation), and the Prize of the Government of the Russian Federation (2003). For outstanding achievements of L.A. Bockeria was awarded the Order of Merit for the Fatherland, III (1999), II (2004) and IV (2010) degrees, the Order of Dignity and Honor (Republic of Georgia, 1999), the Order of St. Sergius of Radonezh, II degree (2001). The Russian Biographical Institute has repeatedly recognized L.A. Bokeria “Person of the Year”, and in 2000 - “Person of the Decade” in the “Medicine” category. In 2002, he was awarded the title “Legend Man”, the all-Russian “Russian National Olympus” award, established by the Government, the Union of Industrialists and the Third Millennium Foundation. As one of the leading cardiac surgeons in the world in 2003, L.A. Bokeria was awarded the international Golden Hippocrates award. In 2004, he was awarded the RAS Triumph Prize in the Life Science – Medicine category. In 2004, he was awarded the Order of Patron, which is awarded by the Patrons of the Century Charitable Foundation for his outstanding contribution to the revival and prosperity of the world, for the greatness of the soul, for selfless generosity; in 2004 and 2005 – the Golden Badge of Honor “Public Recognition”, which is awarded by the National Foundation for “Public Recognition”, the National Civil Committee for Interaction with Law Enforcement, Legislative and Judicial Bodies and the independent organization “Civil Society” for great personal contribution to the development of the domestic medicine, conducting unique cardiac surgery using the latest medical technologies that saved the lives of hundreds of children and newborns, many years of fruitful scientific, practical, pedagogical and educational activities, active citizenship.
In 2006, L.A. Boqueria was awarded the Honorary Diamond Order “Public Recognition”, awarded a diploma from the Presidium of the Parliament of the Peoples of Russia “for saving numerous lives, outstanding knowledge, ability to lead, for unique personal qualities - nobility, courage, sense of duty, ability to preserve honor and dignity, keep one’s word and do business, also for faith in the great future of the Fatherland,” a Gold Medal for outstanding contribution to the education of Russia and a Gold Star “Honor, Pride and Glory of Russia.”
In 2008, L.A. Bockeria was awarded the medal “For practical contribution to strengthening the health of the nation”, the Order of Honor with the title “Support of Honest Business” and the honorary title “Outstanding Cardiac Surgeon of Our Time”. In 2009, the huge contribution of L.A. Bockeria's contribution to science and domestic healthcare was awarded the A.N. Prize. Kosygin “For great achievements in solving problems of the development of the Russian economy” and the Moscow City Prize in the field of medicine “for the development and introduction into clinical practice of a new biological valve “Bioglis”.
L.A. Bokeria is a full member of the American Association of Thoracic Surgeons (1991), member of the board (1992) and member of the Presidium (since 2003, consul) of the European Society of Thoracic and Cardiovascular Surgeons, member of the board of the European Society of Cardiovascular Surgeons, member of the scientific board of the International Cardiothoracic Center of Monaco (1992), member of the Serbian Academy of Sciences (1997), honorary member of the American College of Surgeons (1998), academician of the Academy of Medical Sciences of Ukraine, honorary professor of Moscow State University. M.V. Lomonosov (2011), foreign member of the National Academy of Sciences of Georgia (2012).
He is the president of the Association of Cardiovascular Surgeons of Russia (1995), president of the All-Russian public organization “League of National Health” (2003), member of the Public Chamber of the Russian Federation of all convocations.