Heart rhythm disturbances are common. The causes of heart rhythm disturbances can be not only diseases of the heart, gastrointestinal tract, nervous and endocrine systems, but also some physiological conditions of the body.
The heart is the central organ in the human body, its engine. The heart muscle pumps blood constantly, both day and night during sleep, like a pump. The person does not pay attention to this at all. It is what directs blood throughout the body. Sometimes there are problems with the heart. The rhythm by which it works smoothly is disrupted. If this failure occurs within physiological limits, there is no cause for concern. But sometimes attacks of arrhythmia are an indicator of serious disorders in the body and accompany many other cardiovascular disorders.
Origin of heart rate
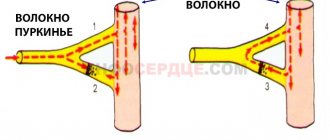
The heart consists of four chambers, represented by two ventricles and two atria, and has the unique ability within itself to generate a spontaneous electrical impulse. This feature is called automatism of the heart muscle. How is this impulse born? Between the right ventricle and the atrium there is a cluster of special muscle cells that can spontaneously contract, causing tissue excitation. Then this impulse spreads to other parts of the heart, thanks to certain intermediaries. This trigger point for muscle cells is called the sinus node. From it, an electrical impulse follows through the atrioventricular node, spreading to the His bundle and Purkinje fibers. This is how the entire heart contracts. From 60 to 90 conductions occur per minute. It should be noted that in children the number of heartbeats per minute is about 120, for them this is the norm. With the correct rhythm, the heart contracts evenly and periodically. If disturbances occur in any of these areas, an attack of arrhythmia occurs. Such disorders may manifest themselves as an increase or decrease in the number of contractions.
Characteristics of different types of cardiac arrhythmias
There are several types of heart rhythm disturbances:
Pathology of impulse formation
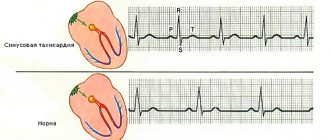
- Excitation impulses arising in the sinus node are called sinus rhythm. In this case, the increased production of the number of such rhythms is called sinus tachycardia. A decrease in the number of impulses – sinus bradycardia. With tachycardia, the heart rate is more than 90 per minute. With bradycardia, the heart rate is below 60 beats per minute. These are disturbances in the number of impulses produced by the heart.
- In some pathologies, nervous excitation does not occur in the sinus node, as it should normally occur, but in any other element of the conduction of nervous excitation in the heart. Such an atypical place of origin of the electrical impulse is called an ectopic focus of excitation. Spontaneous contraction of muscle cells can occur in the atrioventricular node, bundle of His, atria or ventricles. The impulse from them can spread not only through the underlying parts of the heart, but also go upward. Such disorders include extrasystole and paroxysmal arrhythmia. Atypical foci of excitation can also trigger the occurrence of ventricular or atrial fibrillation. These are violations of the site of origin of the nerve impulse.
Heart blocks
In this condition, disturbances in the conduction of nerve excitation occur inside the heart, in any of its areas:
- bundle branch block;
- sinoatrial block;
- atrioventricular block.
Mixed arrhythmic pathologies
Along with sinus rhythm, an ectopic focus of excitation appears in the heart. Both nerve impulses propagate separately due to a blockage between them. The atria contract according to one rhythm, and the ventricles - according to the second.
How to diagnose pathology?
Establishing a diagnosis of rhythm disturbance is not difficult if the patient presents typical complaints. Before the initial examination by a doctor, the patient can independently count his pulse and evaluate certain symptoms.
However, the type of rhythm disturbance can only be determined by a doctor after an ECG , since each type has its own signs on the electrocardiogram. For example, extrasystoles are manifested by altered ventricular complexes, paroxysm of tachycardia - by short intervals between complexes, atrial fibrillation - by an irregular rhythm and heart rate of more than 100 per minute, sinoatrial block - by lengthening of the P wave, reflecting the conduction of the impulse through the atria, atrioventricular block - by lengthening the interval between the atria and ventricular complexes, etc.
In any case, only a cardiologist or therapist can correctly interpret changes in the ECG. Therefore, when the first symptoms of rhythm disturbance appear, the patient should seek medical help as soon as possible.
In addition to an ECG, which can be performed upon the arrival of an ambulance team at the patient’s home, additional examination methods may be needed. They are prescribed in the clinic, if the patient was not hospitalized, or in the cardiology (arrhythmology) department of the hospital, if the patient had indications for hospitalization. In most cases, patients are hospitalized because even a mild heart rhythm disorder can be a precursor to a more serious, life-threatening rhythm disorder. The exception is sinus tachycardia, since it is often treated with tablets at the prehospital stage, and generally does not pose a threat to life.
Additional diagnostic methods usually include the following:
- Monitoring blood pressure and ECG throughout the day (Holter),
- Tests with physical activity (walking on stairs, walking on a treadmill - treadmill test, cycling - bicycle ergometry),
- Transesophageal ECG to clarify the location of the rhythm disturbance,
- Transesophageal electrophysiological study (TEPE) in the case when the rhythm disturbance cannot be detected using a standard cardiogram, and it is necessary to stimulate the heart contractions and provoke the rhythm disturbance to find out its exact type.
In some cases, an MRI of the heart may be required, for example, if the patient is suspected of having a heart tumor, myocarditis, or a scar after a myocardial infarction that is not reflected in the cardiogram. A method such as ultrasound of the heart, or echocardioscopy, is a mandatory standard of research for patients with rhythm disturbances of any origin.
Causes of arrhythmias
The causes of heart rhythm disturbances are divided into two groups:
- Physiological disturbances in heart rhythm can occur several times per day. This should not be a cause for concern.
- Pathological rhythm disturbances go beyond physiological boundaries, which can be caused by several reasons.
The age-related characteristics of the body are such that over time, the heart muscle loses elasticity and firmness, pumping blood in the required volume becomes difficult, which leads to disruption of the organ.
Genetic predisposition is not the least risk factor for the occurrence of pathological rhythmic contractions. A history of this disease increases the chances of heart rhythm disturbances in the offspring.
Abnormalities in the development and structure of the heart can also cause repeated attacks of arrhythmia.
Diagnostics
The attending physician, neurologist or cardiologist can evaluate a single change in pulse or a prolonged failure of heartbeat. Typically, rhythmicity is measured with the patient at rest by counting the beats delivered to the arterial area over 12 or 30 seconds.
If there is a deviation from the norm, the specialist is obliged to prescribe an additional examination.
Not everyone knows what modern diagnostics using the “Tilt-test” is and what it is intended for. It is carried out in specialized cardiology clinics using a special table. During the procedure, the patient, fixed in a horizontal position, is moved to a vertical position.
At the same time, the person experiences the necessary load, which allows one to draw a conclusion about how much the blood pressure changes and whether the heart rhythm is disturbed.
A traditional screening test is performed by placing electrodes on the chest during an electrocardiography procedure. Possible heart rhythm disturbances are recorded graphically.
Modern rhythmocardiography is also widely used, followed by computer processing of the results obtained and their analysis. Determines the affected area in the heart, projects a possible breakdown or complications of the disease.
This method allows you to identify the type and nature of arrhythmia, select appropriate treatment and make a prognosis.
Natural causes of rhythm disturbances
The occurrence of heart rhythm disturbances does not always signal the presence of a disease. There are a number of normal physiological conditions when rhythm changes are observed. Among them are the following reasons:
- During sleep, the heart rate decreases slightly, causing bradycardia.
- Bradycardia is natural in people who play sports professionally. To better adapt to constant strong physical activity, the heart begins to work differently.
- In stressful situations or during unusual excessive physical exertion, increased production of adrenaline occurs, which leads to tachycardia.
- Drinking alcohol and smoking cause physiological tachycardia. Long-term consumption of alcohol in large quantities can lead to heart rhythm pathology, manifested by paroxysmal atrial fibrillation.
Temporary changes in the functioning of the heart lead to:
- food poisoning,
- overheating in the sun and at high temperatures,
- inflammatory processes,
- feverish conditions,
- states of shock,
- hypothermia.
Diseases that cause arrhythmia
1. Diseases of the endocrine system: lack of the hormone insulin (diabetes mellitus), pathologies of the thyroid gland, menopause in women, some tumor processes in the adrenal glands (pheochromocytoma).
2. Diseases of the nervous system:
- brain tumors and injuries,
- neuroses,
- neurasthenia,
- cerebrovascular accidents, strokes,
- vegetative-vascular dystonia.
- Diseases of the heart and blood vessels:
- myocardial infarction,
- hypertension of any severity,
- endocarditis,
- myocarditis,
- heart defects, acquired defects,
- all types of heart failure.
3. Diseases of the stomach and intestines:
- cholecystitis,
- some types of hernias,
- pancreatitis.
Prognosis of the disease.
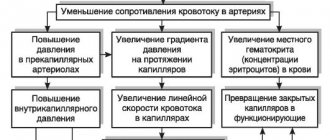
Irregular contractions lead to decreased efficiency of the heart. This can lead to restricted blood flow to the heart muscle (ischemia), impaired heart function, and decreased blood pressure. The mortality rate for atrial fibrillation is twice as high as in the general population.
Risk of stroke.
Violation of the contractile function of the heart leads to the fact that part of the blood remains in the atria, this creates conditions for the formation of blood clots. These blood clots can then travel through blood vessels to distant organs, such as the brain, causing a stroke.
The average risk of stroke is 5% per year and increases with age, as well as in the presence of hypertension, heart failure, diabetes and coronary heart disease. Patients under the age of 60 who do not have the above risk factors have a low risk of developing stroke.
How to relieve an attack of arrhythmia?
Symptoms of arrhythmias are quite diverse, sometimes they can be confused with manifestations of other pathologies. If symptoms such as spontaneous causeless shortness of breath, fainting and pre-fainting states, discomfort in the chest, dizziness, sudden fatigue, the appearance of unconscious fear, darkening in the eyes occur, you should immediately call an ambulance and take urgent measures to improve the patient’s condition. If a person says that he began to feel his heart beating and changes in its work, an arrhythmia can be suspected, which requires some help for the patient. When such a condition occurs, many people become confused and panic because they do not know what to do in the event of an attack of heart rhythm failure.
How to relieve an attack of arrhythmia? Before the arrival of medical personnel, it is necessary to lay the person on a flat surface, loosen all constricting elements of clothing (tie, belt), provide fresh air by opening the windows in the room, and give sedatives to drink (a few drops of Corvalol or valerian tincture). When fainting, the patient should be laid on the floor, head thrown to the side and back to clear the airway. If a person has difficulty breathing despite all this and there is a suspicion of the development of pulmonary edema and atrial fibrillation, the patient must be helped to take a semi-sitting position.
The arriving medical assistance will perform an ECG, carry out therapeutic manipulations to relieve an acute attack of arrhythmia, and take the patient to the hospital for further monitoring of his condition.