Physiology and anatomy of the human cardiovascular system
Anatomically, the human cardiovascular system consists of the heart, arteries, capillaries, veins and performs three main functions:
- transport of nutrients, gases, hormones, and metabolic products to and from cells;
- regulation of body temperature;
- protection from invading microorganisms and foreign cells.
These functions of the human cardiovascular system are directly performed by the fluids circulating in the system - blood and lymph. (Lymph is a clear, watery fluid containing white blood cells and found in the lymphatic vessels.)
The physiology of the human cardiovascular system is formed by two related structures:
- The first structure of the human cardiovascular system includes : the heart, arteries, capillaries and veins, which provide a closed blood circulation.
- The second structure of the cardiovascular system consists of: a network of capillaries and ducts flowing into the venous system.
Prevention of cardiovascular diseases briefly
According to the World Health Organization, every year in our country more than a million people die from pathologies of the heart muscle. And these sad numbers are constantly increasing. But the most amazing thing is that many people could have been saved by starting to adhere to doctors’ recommendations in time.
Specialists advise giving up bad habits (alcohol, smoking, drugs), changing your lifestyle (increase mobility, balance your menu) and learn how to react correctly to stressful situations. These simple rules are a guarantee of normal well-being and protection from negative changes in the functioning of the circulatory system. Periodic examinations in medical institutions will also be useful.
Take care of yourself, because being healthy is always great!
Structure, work and functions of the human heart
The heart is a muscular organ that pumps blood through a system of cavities (chambers) and valves into a distribution network called the circulatory system.
The story about the structure and work of the heart should begin by determining its location. In humans, the heart is located near the center of the chest cavity. It consists mainly of strong elastic tissue - the heart muscle (myocardium), which contracts rhythmically throughout life, sending blood through arteries and capillaries to the body's tissues. Speaking about the structure and functions of the human cardiovascular system, it is worth noting that the main indicator of the work of the heart is the amount of blood that it must pump in 1 minute. With each contraction, the heart throws out about 60-75 ml of blood, and per minute (with an average contraction frequency of 70 per minute) - 4-5 liters, i.e. 300 liters per hour, 7200 liters per day.
In addition to the fact that the work of the heart and blood circulation maintains a stable, normal blood flow, this organ quickly adapts and adapts to the constantly changing needs of the body. For example, the heart pumps more blood when it is active and less when it is at rest. When an adult is at rest, the heart beats 60 to 80 times per minute.
During physical activity, at a time of stress or excitement, the rhythm and heart rate can increase to 200 beats per minute. Without the human circulatory system, the functioning of the body is impossible, and the heart, as its “motor,” is a vital organ.
If the heart rate stops or suddenly weakens, death occurs within a few minutes.
Cardiovascular system of the human circulatory system: what does the heart consist of?
Metabolism.
To meet the metabolic demands of the muscular system during exercise, the heart needs to change 2 major variables. First, cardiac output must be increased. Secondly, blood flow from inactive organs and tissues must be redistributed to active muscles. At rest, muscles receive approximately 20% of total blood flow, but during exercise, blood flow to the muscles increases to 80-85%. As a rule, the longer the duration of physical activity, the greater the role the cardiovascular system plays in metabolism and performance. An example would be a 100-meter sprint, where an athlete’s heart rate increases only at the end of the distance, or generally after finishing, and a marathon, where an increased heart rate is observed throughout the entire distance.
So, what is the human heart made of and what is a heartbeat?
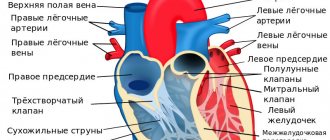
The structure of the human heart includes several structures: walls, septa, valves, conduction system and blood supply system. It is divided by partitions into four chambers, which are not filled with blood at the same time. The two lower thick-walled chambers in the structure of the human cardiovascular system - the ventricles - play the role of a pressure pump. They receive blood from the upper chambers and, contracting, direct it to the arteries. Contractions of the atria and ventricles create what are called heartbeats.
Contraction of the left and right atria
The two upper chambers are the atria. These are thin-walled reservoirs that easily stretch to accommodate blood coming from the veins in the intervals between contractions. The walls and septa form the muscular basis of the four chambers of the heart. The muscles of the chambers are located in such a way that when they contract, blood is literally thrown out of the heart. The inflowing venous blood enters the right atrium of the heart, passes through the tricuspid valve into the right ventricle, from where it enters the pulmonary artery, passing through its semilunar valves, and then into the lungs. Thus, the right side of the heart receives blood from the body and pumps it to the lungs.
Blood in the human cardiovascular system, returning from the lungs, enters the left atrium of the heart, passes through the bicuspid, or mitral, valve and enters the left ventricle, from which it is pushed into the aorta, pressing the aortic semilunar valves against its wall. Thus, the left side of the heart receives blood from the lungs and pumps it to the body.
The human cardiovascular system includes the heart valves and pulmonary trunk
Valves are folds of connective tissue that allow blood to flow in only one direction. The four heart valves (tricuspid, pulmonary, bicuspid or mitral, and aortic) act as a “door” between the chambers, opening in one direction. The work of the heart valves helps blood move forward and prevents it from moving in the opposite direction. The tricuspid valve is located between the right atrium and the right ventricle. The very name of this valve in the anatomy of the human cardiovascular system speaks about its structure. When this valve of the human heart opens, blood flows from the right atrium to the right ventricle. It prevents blood from flowing back into the atrium by closing during ventricular contraction. When the tricuspid valve is closed, the blood in the right ventricle finds outlet only into the pulmonary trunk.
The pulmonary trunk is divided into the left and right pulmonary arteries, which go to the left and right lungs, respectively. The entrance to the pulmonary trunk is closed by the pulmonary valve. This organ of the human cardiovascular system consists of three valves, which are open when the right ventricle of the heart contracts and closed when it relaxes. The anatomical and physiological features of the human cardiovascular system are such that the pulmonary valve allows blood to flow from the right ventricle into the pulmonary arteries, but prevents the reverse flow of blood from the pulmonary arteries into the right ventricle.
Conducting system
In the physiology of the human cardiovascular system, the entire conduction system of the heart is distinguished. It consists of working muscles, which are represented by striated muscle, as well as special, or atypical, tissue. This is where the excitement arises.
Atypical tissue of the human body consists of the sinoatrial node, which is located on the posterior wall of the atrium, the atrioventricular node, located in the wall of the right atrium, and the atrioventricular bundle, or bundle of His. This bundle can pass through the septa and is divided at the end into two legs, which go to the left and right ventricles, respectively.
Function of the bicuspid heart valve during contraction of the atrium and ventricles
The bicuspid, or mitral, valve regulates the flow of blood from the left atrium to the left ventricle. Like the tricuspid valve, it closes when the left ventricle contracts. The aortic valve consists of three leaflets and closes the entrance to the aorta. This valve allows blood to flow out of the left ventricle when it contracts and prevents blood from flowing back from the aorta into the left ventricle when the latter relaxes. The petals of a healthy valve are thin, flexible tissue of perfect shape. They open and close when the heart contracts or relaxes.
In the case of a defect (defect) of the valves, leading to their incomplete closure, a reverse flow of a certain amount of blood occurs through the damaged valve with each muscle contraction. These defects can be either congenital or acquired. The mitral valves are most susceptible to changes.
The left and right chambers of the heart (consisting of an atrium and a ventricle each) are isolated from each other. The right section receives oxygen-poor blood flowing from the body tissues and sends it to the lungs. The left section receives oxygenated blood from the lungs and sends it to tissues throughout the body.
The left ventricle is much thicker and more massive than the other chambers of the heart, since it performs the hardest work - pumping blood into the systemic circulation: usually the thickness of its walls is slightly less than 1.5 cm.
The heart is surrounded by a sac called the pericardium, which contains pericardial fluid. This sac allows the heart to contract and expand freely. The pericardium is strong, it consists of connective tissue and has a two-layer structure. Pericardial fluid is contained between the layers of the pericardium and, acting as a lubricant, allows them to slide freely over each other as the heart expands and contracts.
Heartbeat cycle: phases, rhythm and frequency
The heart has a strictly defined sequence of contraction (systole) and relaxation (diastole), called the cardiac cycle. Since the duration of systole and diastole is the same, the heart is in a relaxed state for half of the cycle.
Cardiac activity is regulated by three factors:
- the heart has the ability for spontaneous rhythmic contractions (so-called automatism);
- heart rate is determined mainly by the autonomic nervous system innervating the heart;
- the harmonious contraction of the atria and ventricles is coordinated by a conduction system consisting of numerous nerve and muscle fibers and located in the walls of the heart.
The heart's function of collecting and pumping blood depends on the rhythm of tiny impulses flowing from the upper chamber of the heart to the lower chamber. These impulses propagate through the conduction system of the heart, which sets the necessary frequency, uniformity and synchronization of contractions of the atria and ventricles in accordance with the needs of the body.
The sequence of contractions of the chambers of the heart is called the cardiac cycle. During the cycle, each of the four chambers goes through a phase of the cardiac cycle such as a contraction (systole) and a relaxation phase (diastole).
The first to occur is the contraction of the atria: first the right one, almost immediately followed by the left one. These contractions ensure that the relaxed ventricles are quickly filled with blood. Then the ventricles contract, forcefully pushing out the blood they contain. At this time, the atria relax and fill with blood from the veins.
One of the most characteristic features of the human cardiovascular system is the ability of the heart to undergo regular spontaneous contractions that do not require an external trigger such as nervous stimulation.
The heart muscle is driven by electrical impulses originating in the heart itself. Their source is a small group of specific muscle cells in the wall of the right atrium. They form a superficial structure approximately 15 mm long, which is called the sinoatrial, or sinus, node. It not only initiates the heartbeat, but also determines its initial frequency, which remains constant in the absence of chemical or nervous influences. This anatomical formation controls and regulates the heart rhythm in accordance with the activity of the body, time of day and many other factors affecting a person. In the natural state of the heart's rhythm, electrical impulses occur that pass through the atria, causing them to contract, to the atrioventricular node, located at the border of the atria and ventricles.
Then the excitation spreads through the conducting tissues into the ventricles, causing them to contract. After this, the heart rests until the next impulse, which begins a new cycle. The impulses arising in the pacemaker propagate in waves along the muscular walls of both atria, causing them to contract almost simultaneously. These impulses can only travel through the muscles. Therefore, in the central part of the heart between the atria and ventricles there is a muscle bundle, the so-called atrioventricular conduction system. Its initial part, which receives the impulse, is called the AV node. The impulse travels along it very slowly, so that about 0.2 seconds elapse between the occurrence of the impulse in the sinus node and its propagation through the ventricles. It is this delay that allows blood to flow from the atria into the ventricles while the latter remain relaxed. From the AV node, the impulse quickly spreads downward along the conducting fibers, forming the so-called His bundle.
The correct functioning of the heart and its rhythm can be checked by placing your hand on your heart or measuring your pulse.
Anatomical and physiological features of the cardiovascular system
Anatomical and physiological features of the cardiovascular system
The cardiovascular system delivers nutrients and oxygen to all organs and tissues of the body, and also removes decay products and carbon dioxide from them.
The heart is a hollow muscular organ located in the chest, at the level of the IV – VIII thoracic vertebrae and is shifted to the left from the midline of the body. Its mass in an adult is 250–300 g. It consists of four cavities: two atria and two ventricles. The bulk of the heart wall is a powerful muscle - the myocardium, consisting of striated muscle fibers. From the inside, the cavity of the heart is lined with an inner membrane - the endocardium, which also forms the valve apparatus of the heart. The presence of valves ensures that blood moves during contraction of the heart muscles always in the same direction. Outside, the myocardium is covered with a thin membrane - the pericardium. The connective tissue around the heart forms the pericardial sac, from the inside of which fluid is released that moisturizes the heart and reduces friction during its contraction.
The walls of the atria are much thinner than the walls of the ventricles, since the work performed by them is relatively small (when they contract, blood enters the ventricles). The muscular wall of the left ventricle is thicker than the wall of the right one, since it is the one that does the most work.
The heart is the main engine of blood; as a result of complex biochemical processes occurring in the heart muscle, the latter periodically contracts (60–90 times per minute).
The rhythm and frequency of heart contractions are influenced by the conditions of the external and internal environment of the body:
- conduction system of the heart (sinus node, atrioventricular node, conducting fibers of the His and Purkinje bundles);
— metabolic processes (bioelectric, physicochemical and biochemical) occurring in the cells of the conduction system and the muscles of the heart;
- special nerve centers located in the brain, medulla oblongata, at various levels of the spinal cord, in the nodes of the sympathetic nervous system, in the walls of the heart itself and blood vessels.
- substances of the hormonal system (endocrine system).
Impulses coming to the heart through the parasympathetic nerves slow down and weaken its contractions, and through the sympathetic nerves they strengthen and speed up. Humoral regulation is associated with the adrenal hormone - adrenaline, pituitary gland, thyroid and pancreas.
The activity of the heart is a rhythmic change of three phases of the cardiac cycle: contraction of the atria, contraction of the ventricles and general relaxation of the heart. Contraction of various sections does not occur simultaneously and consists of systole (simultaneous contraction of the right and left atria, and then the ventricles) and diastole (relaxation of the atria and ventricles). The ability of the heart to contract rhythmically under the influence of impulses arising in the heart muscle itself is called cardiac automaticity. It ensures the functioning of the heart relatively independent of the nervous system.
The movement of blood in the body is called circulation. It occurs through closed systems of blood vessels connected to the heart.
Circulation diagram
During the period of diastole (relaxation of the muscles) of the atria, blood from the vena cava enters the right atrium, and blood enters the left atrium (enriched with oxygen from the pulmonary veins). During atrial systole, blood flows from the atria into the ventricles. As a result of contractions of the ventricles of the heart, blood is released into the vascular system. From the left ventricle it enters the aorta. On average, with one contraction of the left ventricle of the heart, about 60 ml of blood is ejected into the aorta. From there it quickly enters the arteries, then into the arterioles, which in turn branch into capillaries that approach every cell of the body.
From the capillaries, blood collects into venules, then into veins, through which it is delivered to the heart and enters the right atrium. The veins along their entire length have different diameters, increasing from the periphery to the center. This part of the vascular system is called the systemic circulation . Thus, the path of blood from the left ventricle through the arteries, capillaries and veins of all organs of the body to the right atrium is called the systemic circulation.
Metabolism occurs between the blood and body cells through the capillary wall:
- blood gives its oxygen to tissues, and receives carbon dioxide from them;
- nutrients - glucose, amino acids and fatty acids - enter the tissues from the blood, and substances unnecessary for the body, such as uric acid, urea, ammonia and other waste products of cells, enter from the tissues into the blood.
The pulmonary circulation ensures gas exchange in the lungs. The pulmonary artery, upon exiting the right ventricle, is divided into the right and left pulmonary arteries, which in the lungs run next to the bronchi and bronchioles, give off branches to the lobes and segments, break up into arterioles and a capillary network, branch through the alveolar system and carry out gas exchange. The capillaries merge into postcapillaries, which turn into venules, then into the pulmonary veins (right and left), after which they merge into the upper and lower pulmonary veins, heading to the left atrium, into which oxygenated blood enters.
Thus, the path of blood from the right ventricle through the arteries, capillaries and veins of the lungs to the left atrium is called the pulmonary or pulmonary circulation.
The intracardiac circulation serves to enable the heart to work, so that it itself receives nutrition through the coronary arteries of the heart. These arteries originate from the mouth of the aorta. There is a distinction between the left coronary artery (supplies most of the left and anterior walls of the organ) and the right coronary artery (supplies most of the right and posterior walls). With each systole, about 10% of all blood ejected into the aorta enters the coronary vessels.
Through the coronary veins, blood from the heart muscle returns to the vena cava. Thus, the intracardiac circulation consists of the left and right coronary arteries and veins.
The placental circulation is a blood circulation in which the exchange of substances and gases occurs in the placenta between the blood of the fetus and the maternal body. Established by the end of the third month of pregnancy. From the placental villi, blood flows to the fetus through the umbilical vein. Approximately this 40% of the blood enters the right atrium of the fetus through the portal vein through the liver and vena cava and then into the fetal pulmonary circulation. About 60% of the blood enters the left atrium through a special atrial septal defect and flows through the systemic circulation of the fetus providing nutrition and oxygen to the developing organism. From the fetal aortic system, mixed blood reaches the placenta through the umbilical arteries.
The heart of a person at rest, especially during sleep, contracts relatively slowly. During physical activity, contractions become more frequent and increase the volume of blood ejected by the heart. This occurs both due to a more complete contraction of the heart muscle, and due to an increase in its contractions. The work of the heart clearly changes in connection with emotional reactions or mental arousal.
Blood vessels
Blood vessels form a closed system through which blood is transported from the heart to the periphery to all organs and tissues and back to the heart. Arteries carry blood away from the heart, and veins return blood to the heart. Between the arterial and venous sections of the circulatory system there is a microvasculature connecting them, including arterioles, venules, and capillaries.
Arteries are vessels through which blood moves from the heart; they consist of three dense, elastic, elastic membranes - internal, middle (which includes smooth muscles) and external. As the heart contracts, it pumps blood into the arteries under high pressure. Thanks to the plasticity and elasticity of the artery walls, they can withstand this pressure, they stretch and gradually return to their original state, which not only promotes the movement of blood but also smoothes out blood surges. The smallest arteries break up into the thinnest capillaries , their walls are formed by a single layer of flat cells. There are approximately 150 billion capillaries in the human body; if they are stretched in one line, then per kilogram of body weight there will be about 250 km of length. Arterioles and precapillaries regulate the filling of capillaries with blood, and therefore they are called “taps of regional circulation.” Capillaries are the thinnest-walled vessels; after passing through them, the blood loses oxygen and takes carbon dioxide from the tissues. Through venules, blood collects into veins - vessels through which blood moves to the heart. The middle lining of the vein is poor in muscle cells. Only the portal vein has a massive muscular layer, which is why it is called the “arterial vein”. In general, the vein wall is thinner, softer, less elastic and easily stretched. The speed of blood flow through the veins and the pressure in them are much lower than in the arteries. In the lumen of many veins there are valves - folds of the inner lining, resembling a swallow's nest in shape, which do not allow blood to move through the veins in the opposite direction. Typically, the valve flaps are located opposite each other. Valves are especially numerous in the veins of the lower extremities. The division of the blood stream into intervalvular segments, as well as the contraction of the skeletal muscles surrounding the veins, contributes to its movement towards the heart.
Pulse and its parameters
Pulse is a jerky vibration of the walls of blood vessels that occurs as a result of the ejection of blood from the heart into the vascular system. There are arterial, venous and capillary pulses. Of greatest practical importance is the arterial pulse, usually palpable in the wrist or neck.
Pulse measurement. The radial artery in the lower third of the forearm immediately before its articulation with the wrist joint lies superficially and can be easily pressed against the radius. The muscles of the hand that determines the pulse should not be tense. Place two fingers on the artery and squeeze it with force until the blood flow completely stops; then the pressure on the artery is gradually reduced, assessing the frequency, rhythm and other properties of the pulse.
In healthy people, the pulse rate corresponds to the heart rate and is 60-90 beats per minute at rest. An increase in heart rate (more than 80 per minute in a lying position and 100 per minute in a standing position) is called tachycardia, a decrease (less than 60 per minute) is called bradycardia. The pulse rate at the correct heart rhythm is determined by counting the number of pulse beats in half a minute and multiplying the result by two; in case of cardiac arrhythmias, the number of pulse beats is counted for a whole minute. With some heart diseases, the pulse rate may be lower than the heart rate - pulse deficiency. In children, the pulse is more frequent than in adults, in girls it is slightly more frequent than in boys. At night the pulse is lower than during the day. A rare pulse occurs with a number of heart diseases, poisoning, and also under the influence of medications.
Normally, the pulse quickens during physical stress and neuro-emotional reactions. Tachycardia is an adaptive response of the circulatory system to the body’s increased need for oxygen, promoting increased blood supply to organs and tissues. However, the compensatory reaction of a trained heart (for example, in athletes) is expressed in an increase not so much in the pulse rate as in the strength of heart contractions, which is preferable for the body.
Pulse characteristics. Many diseases of the heart, endocrine glands, nervous and mental illnesses, increased body temperature, and poisoning are accompanied by increased heart rate. During palpation examination of the arterial pulse, its characteristics are based on determining the frequency of pulse beats and assessing such qualities of the pulse as rhythm, filling, tension, height, speed
.
Pulse rate
determined by counting pulse beats for at least half a minute, and if the rhythm is incorrect, within a minute.
Pulse rhythm
assessed by the regularity of pulse waves following one after another. In healthy adults, pulse waves, like heart contractions, are observed at regular intervals, i.e.
The pulse is rhythmic, but with deep breathing, as a rule, the pulse increases during inhalation and decreases during exhalation (respiratory arrhythmia). An irregular pulse is also observed with various cardiac arrhythmias
: pulse waves follow at irregular intervals.
Pulse filling
determined by the sensation of pulse changes in the volume of the palpated artery. The degree of filling of the artery depends primarily on the stroke volume of the heart, although the distensibility of the arterial wall is also important (it is greater, the lower the tone of the artery
Pulse voltage
determined by the amount of force that must be applied to completely compress the pulsating artery. To do this, the radial artery is compressed with one of the fingers of the palpating hand and, at the same time, the pulse is determined with another finger distally, recording its decrease or disappearance. There are tense or hard pulses and soft pulses. The degree of pulse tension depends on the level of blood pressure.
Pulse height
characterizes the amplitude of the pulse oscillation of the arterial wall: it is directly proportional to the magnitude of the pulse pressure and inversely proportional to the degree of tonic tension of the artery walls. With shock of various etiologies, the pulse value decreases sharply, the pulse wave is barely palpable. This pulse is called threadlike.
Blood pressure.
Blood pressure is the pressure of blood on the walls of blood vessels - veins, arteries and capillaries. Blood pressure is necessary to ensure that blood can move through the blood vessels. The value of blood pressure (BP) is determined by: the strength of heart contractions; the amount of blood that is released into the vessels with each contraction of the heart and its viscosity; the resistance that the walls of blood vessels provide to the flow of blood;
number of heartbeats per unit of time.
The pressure in the vessels has two extreme values: the maximum - systolic, and the minimum - diastolic, and the difference between them is called pulse pressure.
The first bloodless measurement of blood pressure was made at the end of the 19th century by Riva Rocci. This method consisted of compressing the brachial artery using a special rubber cuff enclosed in a case made of silk fabric. The cuff was connected to a mercury manometer of the original design and air was pumped into it using a rubber balloon. The value of blood pressure was judged by the moment of disappearance and appearance of the pulse on the radial artery, respectively, with an increase and decrease in pressure in the cuff, taking into account the average of these readings. Using the Riva-Rocci method, only systolic pressure was determined.
In 1905, the Russian surgeon Korotkov discovered that noises appeared in the artery when the cuff was loosened. Based on this discovery, he developed an auscultatory method for measuring blood pressure, which was named after him. In a healthy person, blood pressure can vary significantly throughout the day. It is usually reduced during sleep, but when excited or nervous, as well as during physical work, it increases. An increase in blood pressure can also be caused by stress, smoking a cigarette or drinking a cup of coffee.
There are blood pressure standards:
| Age | 16-20 years old | 20 – 40 years | 40 – 60 years | Over 60 years |
| Upper blood pressure (systolic) | 100-120 | 120-130 | 130 — 140 | up to 150 |
| Lower blood pressure (diastolic) | 60-80 | 70-80 | 80 — 90 | up to 90 |
In order to quickly monitor blood pressure, it is useful to have a tonometer on hand - a special device for measuring blood pressure. There are manual (mechanical), semi-automatic and automatic blood pressure monitors.
| mechanical blood pressure monitors | semi-automatic blood pressure monitors | automatic blood pressure monitors |
Rules for measuring blood pressure:
1. Blood pressure measurement should be carried out in a quiet, calm and comfortable environment at a comfortable temperature. Sit on a straight-backed chair next to a table or lying on a couch. The height of the table should be such that when measuring blood pressure, the middle of the cuff placed on the shoulder is at the level of the heart, approximately at the level of the 4th intercostal space in a sitting position or at the level of the midaxillary line in a lying position.
2. The width of the cuff must cover at least 40% of the shoulder circumference and at least 80% of its length. Blood pressure is measured on the right arm or on the arm with a higher blood pressure level (in diseases in which there is a significant difference between the right and left arms, as a rule, the lower one is recorded on the left arm). The use of a narrow or short cuff leads to a significant false increase in blood pressure.
3. At least an hour before measuring blood pressure, you should not smoke, take alcoholic beverages, or take medications that lower or increase blood pressure (such drugs include not only some tablets, but also many eye drops, as well as nasal drops).
4. Blood pressure should be measured 1 - 2 hours after eating. You should not measure your blood pressure immediately after exercise. Even if you had to walk quickly, you need to sit or lie down for a while before measuring your blood pressure.
For greater measurement reliability, you can perform the following points:
- measure blood pressure in both arms;
— on the arm where the pressure was higher, take two more measurements. And the average of the three measurements obtained will give the most accurate information about your blood pressure;
— if you are not a medical specialist, then it is best for you to purchase an automatic tonometer for your home first aid kit. In such devices, the cuff is inflated automatically and the blood pressure numbers are displayed on a special screen.
Instructions for using a mechanical tonometer:
- the lower edge of the cuff should be 2.5 cm above the cubital fossa. The tightness of the cuff: a finger should fit between it and the surface of the shoulder;
— the membrane of the stethoscope should fit completely tightly to the surface of the antecubital fossa. Excessive pressure with the stethoscope should be avoided as it may cause additional compression of the brachial artery. The head of the stethoscope should not touch the cuff or tubes, since the sound from contact with them may interfere with the perception of Korotkoff sounds;
- inflate the cuff using a special bulb until noise is no longer heard in the stethoscope, then slowly deflate the air from the cuff and carefully look at the readings on the tonometer scale. When you hear the first tone in the stethoscope, the number that the arrow points to at that moment will mean the upper (systolic) pressure;
— continuing to slowly release air from the cuff, listen carefully to the tones. When the last tone is heard in the stethoscope, the number that the tonometer arrow shows at that moment will indicate the lower (diastolic) pressure.
In semi-automatic devices, the cuff is inflated by pumping air with a rubber bulb, and the speed of air release from the cuff is adjusted automatically. Automatic devices are characterized by the presence of a built-in compressor that ensures automatic inflation of the cuff; electronic air release valve, which allows you to maintain the rate of air deflation from the cuff during measurement and release air from the cuff after the end of the measurement. They are distinguished by high reliability and accuracy of readings. The disadvantages of automatic devices include the relatively high cost of the device and the need to replace batteries.
Methods for studying the heart.
A modern clinic has a large number of special methods for studying the heart, which are used to diagnose its diseases along with a general clinical examination of the patient, including, in addition to hardware, instrumental and laboratory methods, anamnesis, examination, and physical examination of the heart. Clinical examination of the heart is aimed at identifying structural (anatomical and morphological) changes (by visualizing the structure, geometry of the heart and adjacent vessels, which is not directly observable), as well as at detecting functional changes in the activity of the heart with their quantitative characteristics.
Anamnesis and analysis of the patient’s complaints make it possible to establish the duration, features of the course of heart disease and its manifestations specific to a certain form of heart pathology: for example, the nature of chest pain with angina pectoris, myocardial infarction, the connection between manifestations of heart disease and physical activity, infectious diseases, which is possible with myocarditis and endocarditis.
Examination of the patient reveals changes in body structure and skin color characteristic of certain heart defects: “mitral blush” with mitral stenosis; “heart hump” is a bulging of the chest in the area of the heart with a significant increase in its size due to a congenital or acquired defect in childhood.
Palpation (palpation) of the heart area allows you to assess the position and strength of the apical impulse. With the help of palpation, the cardiac impulse detected during examination is clarified - shaking of the anterior chest wall during systole. Important information about the activity of the heart and its disorders is provided by palpation examination of the pulse, carotid and peripheral arteries, which is of particular importance for assessing stroke volume and diagnosing aortic defects.
Percussion (tapping) of the chest is used to establish the topography and size of the heart by determining the boundaries of the so-called relative cardiac dullness (corresponding to the true boundaries of the heart) and the boundaries of the so-called absolute dullness, corresponding only to that part of the heart, the edges are not covered by the lungs. The diameter of the heart and vascular bundle is also determined. Using percussion, the presence of ascites and hydrothorax, observed in heart failure, is clarified.
Auscultation
(listening) of the heart and blood vessels provides valuable information about the function of the myocardium and valvular apparatus. The heart rate, the number of heart sounds heard during the cardiac cycle and their sonority are assessed, cardiac murmurs and vascular murmurs characteristic of some valvular heart defects, as well as pericardial friction noise are identified. Typically, in healthy individuals, two main heart sounds are heard - the so-called two-part rhythm. Splitting, bifurcation of the main tones and the appearance of additional tones are observed, as a rule, in pathological processes, although in adolescents and young people of asthenic physique the so-called physiological third tone is sometimes heard. The presence of an additional third or fourth tone causes the appearance of a so-called three-member rhythm, and listening to all four heart sounds is defined as a four-member rhythm. Listening to additional tones is sometimes possible only with the help of special auscultation techniques. Thus, to listen to the dull pathological tone that forms the gallop rhythm, the method of direct auscultation of the heart is used with the doctor’s ear tightly pressed directly to the patient’s chest, which creates conditions for better perception of low-frequency sounds.
Instrumental research methods include X-ray, radionuclide, ultrasound, and electrophysiological. The choice of methods in each specific case is made taking into account the information content, the patient’s condition, the nature of the suspected pathology and the amount of data necessary to establish or clarify the diagnosis. Some instrumental studies of the heart require the introduction of sensors (cardiac probing) or indicators into its cavities, i.e. are invasive. They are carried out by puncture of the cavities of the heart or catheterization of the heart by inserting catheters into its cavity through large peripheral vessels. To catheterize the right cavities of the heart, the catheter is passed through the ulnar, jugular or subclavian veins, and for the left cavities - through the femoral artery. From the cavity to the heart cavity, the catheter is passed through the natural bloodstream. Cardiac catheterization is performed by qualified personnel in a specially clinic setting.
MME: Front view of heart
Rice. 4. Front view of the heart: 1 - right ventricle; 2 - right ear; 3 - ascending aorta; 4 - superior vena cava; 5 - pulmonary trunk; 6 - left ear; 7 - great vein of the heart; 8 - anterior interventricular branch of the left coronary artery; 9 - anterior interventricular groove; 10 - left ventricle; 11 - apex of the heart.
MME: Sectional view of the heart
Rice. 5. Sectional view of the heart (transverse section at the level of the coronary sinus, top view): 1 - pulmonary trunk; 2 - aorta; 3 - right coronary artery; 4 - middle leaf of the tricuspid valve; 5 - posterior leaf of the tricuspid valve; 6 - septal leaflet of the tricuspid valve; 7 - coronary sinus; 8 - posterior leaflet of the mitral valve; 9 - anterior leaflet of the mitral valve; 10 - left coronary artery.
MME: Sectional view of the heart
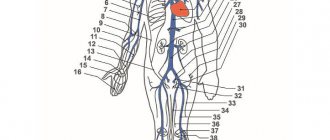
Rice. 6. Sectional view of the heart (frontal section, front view): 11 - left atrium; 12 - left pulmonary vein; 13 - mitral valve; 14 - chordae tendineae; 15 - left ventricle; 16 - fleshy trabeculae; 17 - apex of the heart; 18 - ventricular septum (muscular part); 19 - papillary muscles; 20 - right ventricle; 21 - tricuspid valve; 22 - interventricular septum (membranous part); 23 - valve of the coronary sinus; 24 - pectineus muscles; 25 - inferior vena cava; 36 - right atrium; 27 - fossa oval; 28 - interatrial septum; 29 - right pulmonary veins.
Anatomical and physiological features of the cardiovascular system
The cardiovascular system delivers nutrients and oxygen to all organs and tissues of the body, and also removes decay products and carbon dioxide from them.
The heart is a hollow muscular organ located in the chest, at the level of the IV – VIII thoracic vertebrae and is shifted to the left from the midline of the body. Its mass in an adult is 250–300 g. It consists of four cavities: two atria and two ventricles. The bulk of the heart wall is a powerful muscle - the myocardium, consisting of striated muscle fibers. From the inside, the cavity of the heart is lined with an inner membrane - the endocardium, which also forms the valve apparatus of the heart. The presence of valves ensures that blood moves during contraction of the heart muscles always in the same direction. Outside, the myocardium is covered with a thin membrane - the pericardium. The connective tissue around the heart forms the pericardial sac, from the inside of which fluid is released that moisturizes the heart and reduces friction during its contraction.
The walls of the atria are much thinner than the walls of the ventricles, since the work performed by them is relatively small (when they contract, blood enters the ventricles). The muscular wall of the left ventricle is thicker than the wall of the right one, since it is the one that does the most work.
The heart is the main engine of blood; as a result of complex biochemical processes occurring in the heart muscle, the latter periodically contracts (60–90 times per minute).
The rhythm and frequency of heart contractions are influenced by the conditions of the external and internal environment of the body:
- conduction system of the heart (sinus node, atrioventricular node, conducting fibers of the His and Purkinje bundles);
— metabolic processes (bioelectric, physicochemical and biochemical) occurring in the cells of the conduction system and the muscles of the heart;
- special nerve centers located in the brain, medulla oblongata, at various levels of the spinal cord, in the nodes of the sympathetic nervous system, in the walls of the heart itself and blood vessels.
- substances of the hormonal system (endocrine system).
Impulses coming to the heart through the parasympathetic nerves slow down and weaken its contractions, and through the sympathetic nerves they strengthen and speed up. Humoral regulation is associated with the adrenal hormone - adrenaline, pituitary gland, thyroid and pancreas.
The activity of the heart is a rhythmic change of three phases of the cardiac cycle: contraction of the atria, contraction of the ventricles and general relaxation of the heart. Contraction of various sections does not occur simultaneously and consists of systole (simultaneous contraction of the right and left atria, and then the ventricles) and diastole (relaxation of the atria and ventricles). The ability of the heart to contract rhythmically under the influence of impulses arising in the heart muscle itself is called cardiac automaticity. It ensures the functioning of the heart relatively independent of the nervous system.
The movement of blood in the body is called circulation. It occurs through closed systems of blood vessels connected to the heart.
Circulation diagram
During the period of diastole (relaxation of the muscles) of the atria, blood from the vena cava enters the right atrium, and blood enters the left atrium (enriched with oxygen from the pulmonary veins). During atrial systole, blood flows from the atria into the ventricles. As a result of contractions of the ventricles of the heart, blood is released into the vascular system. From the left ventricle it enters the aorta. On average, with one contraction of the left ventricle of the heart, about 60 ml of blood is ejected into the aorta. From there it quickly enters the arteries, then into the arterioles, which in turn branch into capillaries that approach every cell of the body.
From the capillaries, blood collects into venules, then into veins, through which it is delivered to the heart and enters the right atrium. The veins along their entire length have different diameters, increasing from the periphery to the center. This part of the vascular system is called the systemic circulation . Thus, the path of blood from the left ventricle through the arteries, capillaries and veins of all organs of the body to the right atrium is called the systemic circulation.
Metabolism occurs between the blood and body cells through the capillary wall:
- blood gives its oxygen to tissues, and receives carbon dioxide from them;
- nutrients - glucose, amino acids and fatty acids - enter the tissues from the blood, and substances unnecessary for the body, such as uric acid, urea, ammonia and other waste products of cells, enter from the tissues into the blood.
The pulmonary circulation ensures gas exchange in the lungs. The pulmonary artery, upon exiting the right ventricle, is divided into the right and left pulmonary arteries, which in the lungs run next to the bronchi and bronchioles, give off branches to the lobes and segments, break up into arterioles and a capillary network, branch through the alveolar system and carry out gas exchange. The capillaries merge into postcapillaries, which turn into venules, then into the pulmonary veins (right and left), after which they merge into the upper and lower pulmonary veins, heading to the left atrium, into which oxygenated blood enters.
Thus, the path of blood from the right ventricle through the arteries, capillaries and veins of the lungs to the left atrium is called the pulmonary or pulmonary circulation.
The intracardiac circulation serves to enable the heart to work, so that it itself receives nutrition through the coronary arteries of the heart. These arteries originate from the mouth of the aorta. There is a distinction between the left coronary artery (supplies most of the left and anterior walls of the organ) and the right coronary artery (supplies most of the right and posterior walls). With each systole, about 10% of all blood ejected into the aorta enters the coronary vessels.
Through the coronary veins, blood from the heart muscle returns to the vena cava. Thus, the intracardiac circulation consists of the left and right coronary arteries and veins.
The placental circulation is a blood circulation in which the exchange of substances and gases occurs in the placenta between the blood of the fetus and the maternal body. Established by the end of the third month of pregnancy. From the placental villi, blood flows to the fetus through the umbilical vein. Approximately this 40% of the blood enters the right atrium of the fetus through the portal vein through the liver and vena cava and then into the fetal pulmonary circulation. About 60% of the blood enters the left atrium through a special atrial septal defect and flows through the systemic circulation of the fetus providing nutrition and oxygen to the developing organism. From the fetal aortic system, mixed blood reaches the placenta through the umbilical arteries.
The heart of a person at rest, especially during sleep, contracts relatively slowly. During physical activity, contractions become more frequent and increase the volume of blood ejected by the heart. This occurs both due to a more complete contraction of the heart muscle, and due to an increase in its contractions. The work of the heart clearly changes in connection with emotional reactions or mental arousal.
Blood vessels
Blood vessels form a closed system through which blood is transported from the heart to the periphery to all organs and tissues and back to the heart. Arteries carry blood away from the heart, and veins return blood to the heart. Between the arterial and venous sections of the circulatory system there is a microvasculature connecting them, including arterioles, venules, and capillaries.
Heart function indicators: heart rate and strength
Regulation of heart contractions . An adult's heart usually beats at a rate of 60-90 times per minute. In children, the frequency and strength of heart contractions is higher : in infants - approximately 120, and in children under 12 years old - 100 beats per minute. These are only average indicators of heart function, and depending on conditions (for example, physical or psycho-emotional stress, etc.), the heart rate cycle can change very quickly.
The heart is abundantly supplied with nerves that regulate the frequency of its contractions. The regulation of heart contractions during strong emotions, such as excitement or fear, increases as the flow of impulses from the brain into the heart increases.
Physiological changes also play an important role in the functioning of the heart.
Thus, an increase in the concentration of carbon dioxide in the blood, along with a decrease in oxygen content, causes powerful stimulation of the heart.
Overflow of blood (strong stretching) of certain areas of the vascular bed has the opposite effect, which leads to a slowdown in heartbeat. Physical activity also increases the heart rate up to 200 per minute or more. A number of factors affect the functioning of the heart directly, without the participation of the nervous system. For example, an increase in body temperature speeds up the heart rate, and a decrease slows it down.
Some hormones, such as adrenaline and thyroxine, also have a direct effect and, entering the heart through the blood, increase the heart rate. Regulating the strength and frequency of heart contractions is a very complex process in which numerous factors interact. Some affect the heart directly, others act indirectly - through various levels of the central nervous system. The brain ensures coordination of these influences on the work of the heart with the functional state of other parts of the system.
Heart function and blood circulation
The human circulatory system, in addition to the heart, includes a variety of blood vessels:
- Vessels are a system of hollow elastic tubes of various structures, diameters and mechanical properties filled with blood. Depending on the direction of blood flow, the vessels are divided into arteries, through which blood is drained from the heart and supplied to the organs, and veins, vessels in which blood flows towards the heart.
- Between the arteries and veins there is a microvasculature that forms the peripheral part of the cardiovascular system. The microvasculature is a system of small vessels, including arterioles, capillaries, and venules.
- Arterioles and venules are small branches of arteries and veins, respectively. As they approach the heart, the veins merge again to form larger vessels. Arteries have a large diameter and thick, elastic walls that can withstand very high blood pressure. Unlike arteries, veins have thinner walls that contain less muscle and elastic tissue.
- Capillaries are the smallest blood vessels that connect arterioles to venules. Due to the very thin wall of the capillaries, they allow the exchange of nutrients and other substances (such as oxygen and carbon dioxide) between the blood and the cells of various tissues. Depending on the need for oxygen and other nutrients, different tissues have different numbers of capillaries.
Tissues such as muscles consume large amounts of oxygen and therefore have a dense network of capillaries. On the other hand, tissues with a slow metabolism (such as the epidermis and cornea) do not contain capillaries at all. Humans and all vertebrate animals have a closed circulatory system.
The human cardiovascular system forms two circulatory circles connected in series: large and small.
The systemic circulation supplies blood to all organs and tissues. It begins in the left ventricle, where the aorta emerges, and ends in the right atrium, where the vena cava enters.
The pulmonary circulation is limited by blood circulation in the lungs; here the blood is enriched with oxygen and carbon dioxide is removed. It begins with the right ventricle, from which the pulmonary trunk emerges, and ends with the left atrium, into which the pulmonary veins flow.
A little anatomy: what is included in the cardiovascular system
The cardiovascular system (CVS), or circulatory system, is a complex multifunctional element of the human body, consisting of the heart and blood vessels (arteries, veins, capillaries).
The cardiovascular system has a complex anatomical and physiological structure
This is interesting. A widespread vascular network permeates every square millimeter of the human body, providing nutrition and oxygenation to all cells. The total length of arteries, arterioles, veins and capillaries in the body is more than one hundred thousand kilometers.
The structure of all elements of the cardiovascular system is different and depends on the functions performed. The anatomy of the cardiovascular system is discussed in more detail in the sections below.
Heart
The heart (Greek cardia, Lat. cor.) is a hollow muscular organ that pumps blood through the vessels through a certain sequence of rhythmic contractions and relaxations. Its activity is determined by constant nerve impulses coming from the medulla oblongata.
In addition, the organ has automatism - the ability to contract under the influence of impulses generated in itself. The excitation generated in the sinoatrial node spreads to the myocardial tissue, causing spontaneous muscle contractions.
The human heart is the result of many years of evolution
Note! The volume of organ cavities in an adult is on average 0.5-0.7 liters, and the mass does not exceed 0.4% of the total body weight.
The walls of the heart consist of three layers:
- endocardium , lining the heart from the inside and forming the valve apparatus of the cardiovascular system;
- myocardium – a muscular layer that ensures contraction of the chambers of the heart;
- epicardium - the outer membrane connecting to the pericardium - the pericardial sac.
In the anatomical structure of the organ, there are 4 isolated chambers - 2 ventricles and two atria, connected to each other through a valve system.
Schematic representation of the chambers of the heart
Blood saturated with oxygen molecules from the pulmonary circulation enters the left atrium through four pulmonary veins of equal diameter. In diastole (the relaxation phase), it enters the left ventricle through the open mitral valve. Then, during systole, blood is forcefully ejected into the aorta, the largest arterial trunk in the human body.
The right atrium collects “processed” blood containing a minimum amount of oxygen and a maximum amount of carbon dioxide. It comes from the upper and lower parts of the body through the vena cavae of the same name - v. cava superior and v. cava interior.
The blood then passes through the tricuspid valve and enters the cavity of the right ventricle, from where it is transported through the pulmonary trunk to the pulmonary arterial network to enrich O2 and get rid of excess CO2. Thus, the left parts of the heart are filled with oxygenated arterial blood, and the right parts are filled with venous blood.
Note! The rudiments of the heart muscle are determined even in the simplest chordates in the form of expansion of the great vessels. In the process of evolution, the organ developed and acquired an increasingly more perfect structure. So, for example, the heart of fish is two-chambered, in amphibians and reptiles it is three-chambered, and in birds and all mammals, like in humans, it is four-chambered.
The contraction of the heart muscle is rhythmic and normally amounts to 60-80 beats per minute. In this case, a certain time dependence is observed:
- the duration of contraction of the atrial muscles is 0.1 s;
- the ventricles tense for 0.3 s;
- pause duration – 0.4 s.
Systole and diastole of the heart muscle
Auscultation reveals two tones in the work of the heart. Their main characteristics are presented in the table below.
Table: Heart sounds:
| Name | What caused | Characteristic |
| Systolic | Formed by the oscillation of the leaflets when the mitral and tricuspid valves close | Low, long |
| Diastolic | Formed by closure of semilunar aortic valves and pulmonary valves | Tall short |
Arteries
Arteries are hollow elastic tubes through which blood moves from the heart to the periphery. They have thick walls, formed in layers of muscle, elastic and collagen fibers and can change their diameter depending on the volume of fluid circulating in them. Arteries are saturated with oxygen-rich blood and distribute it to all organs and tissues.
Note! The only exception to the rule is the pulmonary trunk (truncus pneumonalis). It is filled with venous blood, but is called an artery because it carries it from the heart to the lungs (into the pulmonary circulation), and not vice versa. Similarly, the pulmonary veins draining into the left atrium carry arterial blood.
The largest arterial vessel in the human body is the aorta, which emerges from the left ventricle.
According to their anatomical structure they are divided into:
- the ascending aorta, which gives rise to the coronary arteries that supply the heart;
- the aortic arch, from which large arterial vessels emerge that supply the organs of the head, neck and upper extremities (brachiocephalic trunk, subclavian artery, left common carotid artery);
- the descending aorta, which is divided into the thoracic and abdominal sections.
The aorta is the main arterial vessel in the human body
Vienna
Veins are commonly called vessels that carry blood from the periphery to the heart. Their walls are less thick than arterial ones, and they contain almost no smooth muscle fibers.
As the diameter increases, the number of venous vessels becomes fewer and fewer, and eventually only the superior and inferior vena cava remain, collecting blood from the upper and lower parts of the human body, respectively.
The photo shows the difference in the structure of arteries and veins
Microvasculature vessels
In addition to large arteries and veins, the cardiovascular system includes elements of the microvasculature:
- arterioles – arteries of small diameter (up to 300 µm), preceding capillaries;
- venules - vessels directly adjacent to the capillaries and transport oxygen-poor blood to larger veins;
- capillaries - the smallest blood vessels (diameter is 8-11 microns), in which oxygen and nutrients are exchanged with the interstitial fluid of all organs and tissues;
- arteriole-venous anastomoses are connections that ensure the passage of blood from arterioles to venules without the participation of capillaries.
In addition to regulating blood circulation, the cardiovascular system is also responsible for the functioning of the body’s lymphatic system, which consists of lymph itself, lymphatic vessels and lymph nodes.
With the help of tiny capillaries, tissues are saturated with oxygen and nutrients