Interpretation of ECG indicators for arrhythmia
Arrhythmia is the general name for all those conditions when heart rate, strength, rhythm and consistency are disturbed. That is, these are all deviations from the normal heart rhythm, which is called sinus.
During normal heart function, the heart rate is 50-100 beats/min, this depends on the physical activity of the person at the moment. The development of arrhythmia is preceded by a variety of reasons. Arrhythmia will be considered such conditions in which the heart rate becomes less than 60 beats per minute or increases over 100. Arrhythmia on the ECG is visible in different ways, depending on the type of syndrome.
Important information!
Below are descriptions of the main indicators on the ECG in case an electrocardiogram has been performed, but has not yet been deciphered by a cardiologist.
Table-decoding of indicators on the ECG
| Index | What does it mean | What should it be |
| P | bioelectricity in the atria | Positive |
| Q | bioelectricity in the interventricular septum | Negative |
| R | biopotential in the ventricular myocardium | Positive, duration - up to 0.1 second, amplitude - no more than 2.5 cells, normal - PII>PI>PIII |
| S | process of distribution of bioelectricity in the ventricles | Negative |
| T | processes of renewal of biopotential in the heart | Positive |
An ECG requires mandatory interpretation by a cardiologist.
Heart rhythm disturbances: causes
Atrial fibrillation is an asymmetry of heart rhythm, which manifests itself in chaotic excitation and contraction of heart fibers throughout the entire cardiac cycle. The contraction frequency is 300-700 beats/min. The disorder is most often observed in people over 50 years of age who have heart disease. Its root causes are manifold:
- hypertension;
- heart failure;
- ischemia;
- defects, inflammations and tumors of the heart;
- diabetes;
- thyroid diseases;
- chronic renal failure.
Symptoms and the degree of their manifestation depend on the form of the disease, but there are general signs of atrial fibrillation:
- cardiopalmus;
- dyspnea;
- weakness;
- sweating,
- dizziness;
- chest pain.
Arrhythmia is a pathology due to which the frequency, rhythm and sequence of heart contractions are disrupted. That is, with arrhythmia, an impulse cannot be formed and conducted normally.
It should be noted that arrhythmia is a group of diseases of the cardiovascular system, and not one pathology.
I recently read an article that talks about Monastic tea for treating heart disease. With this tea you can FOREVER cure arrhythmia, heart failure, atherosclerosis, coronary heart disease, myocardial infarction and many other diseases of the heart and blood vessels at home.
I’m not used to trusting any information, but I decided to check and ordered a bag. I noticed changes within a week: the constant pain and tingling in my heart that had tormented me before receded, and after 2 weeks disappeared completely. Try it too, and if anyone is interested, below is the link to the article.
There are two types of causes of heart failure. These include:
- Cardiac causes: myocardial infarction;
- heart failure;
- various types of heart defects.
- anemia;
- unhealthy lifestyle (drinking excess alcohol, smoking, stress, systematic overwork);
Symptoms of heart rhythm disturbances include the following conditions:
- Painful sensations or discomfort when inhaling in the left part of the chest.
- Changes in the nature of contractions of the heart muscle.
- Malaise, increased frequency and difficulty breathing, dizziness and fainting.
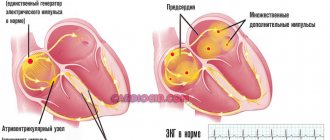
The influence of extrasystoles
These are contractions made prematurely. Electrical impulses do not come from the sinus node. This type most often occurs due to various factors not related to heart disease. The main causes of this type of arrhythmia include:
- unstable psycho-emotional state;
- treatment with specific groups of drugs;
- smoking abuse;
- vegetative disorders.
This is what extrasystole looks like on an ECG
Extrasystoles are exactly the case when the patient may not feel anything for a long time. Sometimes there may be a kind of shock in the heart, or its short-term fading. If such signs are isolated, this may occur even during normal heart function. But if they occur more often, this may indicate an exacerbation of diseases - ischemia, myocarditis. The most dangerous are ventricular extrasystoles. This is when the impulse comes from one of the ventricles. This may be the initial symptom of ventricular fibrillation.
How to determine on an ECG. On an ECG, an extraordinary contraction of the heart looks like a wave different from the others.
Prevention
The main preventive measure for all types of arrhythmic disorders, and even all diseases of the cardiovascular system, is maintaining a healthy lifestyle. Namely:
- Rest and sleep mode. Sleep should be complete and long;
- Healthy eating. You need to eat foods that contain vitamins and microelements, especially foods containing fiber. In turn, it is necessary to avoid fried, fatty, spicy foods;
- Give up bad habits: alcohol abuse, smoking, drugs.
Important! It is also prohibited to self-medicate and take medications without medical supervision.
Preventive measures include regular electrocardiography and other studies in order to prevent the development of diseases of the cardiovascular system. You need to regularly check your pulse and blood pressure.
As you can see, arrhythmia is a complex disorder of the heart. Sometimes even surgical treatment of arrhythmia is performed. Since the impulse comes from the sinus node, if it is damaged, an implant is needed.
Arrhythmic disorders are observed in 15% of patients with diseases of the cardiovascular system. According to medical practice, arrhythmia quite often leads to heart failure and even sudden cardiac death.
Source: serdse.top
Atrial fibrillation
This type is atrial fibrillation. This in itself is a complication that occurs during ischemia. This type is the most common heart rhythm disorder. Often the cause of this type is diseases of the thyroid gland, when its activity is disrupted.
Atrial fibrillation is characterized by disruptions in cardiac activity of varying severity, fainting and darkening of the eyes. Often these symptoms are accompanied by severe weakness, shortness of breath, chest pain and a feeling of increasing fear. Sometimes attacks begin suddenly and end spontaneously without any intervention. But it is most likely that the attack will last a long time, lasting several hours, and maybe even days, and will require mandatory medical care.
How to determine on an ECG. The ECG may indicate large or small atrial waves, deformed, disordered complexes. One patient has both flutter and atrial fibrillation. In a cardiogram of a healthy person, there are no chaotic waves, the rhythm is smooth.
Existing heart rhythm disturbances and their display on the ECG
In medical terms, heart rhythm disturbances are called arrhythmia. Most people understand this term as random abbreviations, but this is not entirely correct. In fact, arrhythmia is an abnormal rhythm, frequency and sequence of heart contractions.
This disease is diagnosed using an ECG, on the graph of which the doctor sees changes in the length of the segments or the size of the teeth. Unfortunately, the problem of cardiac arrhythmia is one of the main ones in cardiological practice, since it is often difficult to identify the etiological causes of heart failure, and deep skills in deciphering the ECG are also required.
Sinus arrhythmia
Despite the sinus rhythm, it is distinguished by its irregularity. Heartbeats either slow down or speed up. It is especially noticeable when breathing: when exhaling, the heart rate is almost twice as large, and when inhaling, it decreases significantly. The patient feels very tired, dizzy, and may faint. Increased symptoms require close attention and treatment.
The causes of sinus arrhythmia are heart diseases, infectious processes involving the myocardium, and heart defects. Of the external factors, arrhythmia of this type is most often provoked by hormonal disorders in the body and diseases of the nervous system.
How to determine on an ECG. On an ECG, abnormal cardiac activity is indicated by a difference in PR intervals of at least 10%.
Atrial flutter
With this diagnosis, the heart rate increases to 200-400 contractions, for example, against the background of the correct atrial rhythm.
The reasons here, as a rule, are organic heart disease, heart surgery (especially the first week after the intervention). Often, hypertension and myocardial dystrophy can provoke atrial flutter.
Risk groups include men over 60 years of age, smokers, people with a lack of potassium or excessive production of thyroid hormones. An attack of such arrhythmia can be caused by extreme heat, physical strain, stress, or the use of alcohol or drugs.
Symptoms are a strong increase in heart rate, weakness, a sharp decrease in pressure with the development of a semi-fainting state, dizziness. Along with this, pulsation of the veins in the neck is often observed.
How to determine on an ECG. On the ECG, flutter is indicated by F-waves appearing instead of the P wave. Heart rate is 240-350 beats per minute. There is also atypical flutter, in which the same waves occur at a heart rate of 340-430 beats.
Features of sinus arrhythmia in children
A child's heart rate is significantly different from an adult's. In newborns, the normal heart rate is between 120 and 170 beats per minute. With age, the heart rate decreases and reaches adult values by adolescence.
Doctors distinguish three types of arrhythmia - mild, moderate and severe. In moderate form, it occurs in children under 5 years of age and in adolescents. Severe bradyarrhythmia occurs after rheumatism or in children involved in sports.
The main causes of arrhythmias are congenital heart defects, endocrine pathologies, metabolic disorders (lack of microelements and impaired water-electrolyte metabolism). In some children, arrhythmia appears during periods of rapid growth - at 5–7 and at 9 years. In adolescence, it is caused by vegetative-vascular dystonia.
Each type of arrhythmia is characterized by certain threshold values of heart rate. Severe bradycardia in children under one year of age is a pulse less than 100 beats. In children from 2 to 7 years old, it is diagnosed with a heart rate of less than 75, from 8 to 18 years old - with a heart rate of less than 62 beats per minute. Severe tachycardia occurs when normal pulse values are exceeded by 40–60 beats.
Common symptoms for all types of sinus arrhythmias in children:
- fast fatiguability;
- intolerance to stuffiness;
- restless behavior (typical of children under one year old);
- poor appetite;
- pale skin;
- When counting the pulse, interruptions are heard (uneven rhythm).
Older children complain of headaches and morning dizziness. If these symptoms are observed continuously, the child should be examined by a cardiologist.
How to treat arrhythmia in a child
First of all, it is necessary to organize the child’s life in such a way as to minimize the risk of further development of the disease and complications. It is necessary to protect him from any conflicts in the family and reduce his time in front of the TV or computer. Daily long walks, balanced nutrition and physical activity will benefit your health.
Sinus arrhythmia in children is not treated with special medications. Usually it is symptomatic, and the efforts of doctors are aimed at correcting the underlying disease.
Supraventricular tachycardia
This type of arrhythmia occurs in a fairly small area of atrium tissue. Because of this, inflammation of the heart soon begins. This inflammation is characterized by its periodicity. The frequency can last for days or even months. Most often, it happens that not one area of the heart becomes inflamed, but several.
This arrhythmia implies an increase in heart rate for no apparent reason. The symptoms are quite varied, but the very first sign is a strong pulsation in the chest. In addition to symptoms typical of other types, sweating, tight throat, increased urination, nausea and vomiting may occur.
How to determine on an ECG. This is noticeable by an increase in the frequency of P waves and QRC complexes, as well as small intervals between them.
Paroxysmal tachycardia
- this is a sudden onset and suddenly ending attack of rapid heartbeat with a frequency above 160 beats/min. while maintaining the correct rhythm. Occurs with ischemic heart disease, myocarditis, congenital anomalies of the conduction system of the heart - WPW syndrome, CLC, etc. The mechanisms of occurrence of paroxysmal tachycardia are similar to those with extrasystole (mechanism of re-entry of the excitation wave re-entry, increased automaticity of ectopic centers of the II and III orders), therefore an attack of paroxysmal tachycardia can be considered as a long series of extrasystoles following one after another with a high frequency. Depending on the location of the ectopic focus, supraventricular (atrial, atrioventricular and ventricular forms of paroxysmal tachycardia are distinguished. Supraventricular forms are characterized by the presence of a P wave (but at high frequency the P wave may overlap the T wave and not be differentiated), the presence of unchanged QRS complexes, the final part of the ventricular complex is positive.Ventricular paroxysmal tachycardia is characterized by aberration of the QRST complex (widened, deformed, discordant) and complete separation of the rapid ventricular rhythm (QRS complexes) and the normal atrial rhythm (P wave), but due to the high frequency, P waves cannot always be detected. Therefore, the main symptom of ventricular paroxysmal tachycardia remains aberration of the ventricular complexes.
Ventricular tachycardia
The pathology is expressed in the acceleration of the rhythm coming from the ventricles. Heart rate is approximately 100 beats, but ventricular impulses can follow each other. The main characteristic of this species is suddenness. The heart rate begins to increase to 200, the heart can no longer fill with blood normally and, accordingly, much less of it is released into the body. This pathology is difficult for patients to tolerate, especially with concomitant heart disease.
Persistent gastric tachycardia is manifested by a strong change in systolic pressure. At this moment, the patient's venous pulsation is reduced.
Unstable gastric tachycardia goes unnoticed if it is not caught on the ECG at this moment.
If the heart rate is 220 beats per minute, everything indicates ventricular flutter. Here you may experience a decrease in blood pressure, sweating, severe agitation or, conversely, stupor and fainting. Sometimes there is swelling, difficulty breathing, shortness of breath - all indicating acute heart failure.
How to determine. The ECG shows expansion or deformation of the QRC complexes, changes in their amplitude and directions. There is a noticeable deviation of the electrical axis to the left.
Classifications of atrial dysfunction
Modern clinical cardiology prefers to distinguish two main forms of pathology. ECG diagnosis of atrial fibrillation is based on the principles of this division.
It is believed that the main course of cardiac arrhythmia in the atria is a permanent form of the disease, which occurs in more than 70% of patients and often occurs without pronounced symptoms. Persistent atrial fibrillation is classified by the number of heartbeats and the interaction of the atria and ventricles. There are three main types of disease:
- Bradysystolic atrial fibrillation is characterized by a reduced number of heart contractions - less than 60 beats per minute. This pathology most often develops in patients with chronic processes in the heart muscle or coronary vessels.
- The normosystolic form of atrial fibrillation is interesting because since the number of heartbeats is close to normal and there is no discrepancy in the functioning of the atria and ventricles, the patient may not notice a disruption in the activity of the heart for a long time. The body adapts to minimal hemodynamic disturbances and corrects it itself.
- If the number of heart contractions exceeds 100 beats per minute, experts talk about the development of the tachysystolic form of the disease. Such symptoms are most often caused by various acute processes in the human body. Such a heart rhythm disturbance can occur even in a healthy person under the influence of acute poisoning, large amounts of alcohol, or a chronic lack of calcium in the blood.
In clinical practice, a picture is often observed when disruption of the atria occurs without any apparent reason or under the influence of physical activity. In this case, experts talk about the development of a paroxysmal form of atrial fibrillation.
Unlike a constant change in heart rhythm, such attacks are short: they can last from a few seconds to 10 - 12 hours. In terms of symptoms, this disease is similar to the tachysystolic form of rhythm disturbance, but there are certain differences.
If a patient has developed paroxysmal atrial fibrillation, an ECG can clearly diagnose the process. Cardiologists consider the main sign of this pathology to be the presence of specific F waves on the electrocardiogram; an excessive frequency of ventricular complexes on the film is also possible.
Atrial fibrillation. Correct ventricular rhythm. Sawtooth fibrillation waves (F waves)
The occurrence of ventricular fibrillation
Here the impulses coming from the ventricles are chaotic and irregular. Because of this, there is flutter of the ventricles and possible absence of their contractions. For this reason, blood cannot be pumped normally throughout the body. This condition is extremely dangerous and requires urgent hospitalization and resuscitation with defibrillation. If all this is not done within 10 minutes after the onset of the attack, then everything can end in death.
If we talk about symptoms, they all correspond to cessation of blood circulation, and, accordingly, clinical death. The patient loses consciousness, he begins to have convulsions, spontaneous urination and defecation, the pupils do not react to light, there is no pulse or breathing, and they cannot be felt in the arteries, blue discoloration of the skin may be noted.
Decoding. On an ECG it may be:
- large-wave fibrillation (stages 1 and 2) with fairly large waves and a frequency of 300-600. This is the best prognosis and means that medical intervention will be effective;
- small-wave fibrillation (late stage, 3 and 4) - the waves are wider and acquire an uneven amplitude. The heart rate is also uneven - first it increases to 600, and then drops to 400 per minute.
This condition is dangerous due to the occurrence of vascular thromboembolism and abnormal expansion of all parts of the heart.
Features of sinus node dysfunction syndrome
SDSU – rhythm disturbances due to weakening of the automaticity function or its complete cessation. There is a decrease in heart rate and cardiac arrest may occur.
Symptoms may be completely absent or present in full, as with other arrhythmias. With SDSU, fainting most often occurs, and they can go away on their own - the skin becomes pale and cold, sweating. There may be disturbances in the gastrointestinal tract and muscle weakness.
Most often, SDSU occurs in people aged 60-70 years, with equal probability in men and women. This is a very rare species - 0.03-0.05% of them all.
Heart block
The patient's impulse conduction slows down, sometimes it stops completely. Blockades can also be persistent or transient. Their causes include heart disease, the use of certain medications, and high blood pressure. The blockade can even be congenital, but this is extremely rare (then the heart rate drops to 40 per minute).
The clinical picture is characterized by the absence of pulse and heart sounds. There is very slow blood circulation in the body, convulsions and fainting, oxygen starvation of internal organs occur. Heart block often ends in the death of the patient.
How to determine. On the ECG, the P wave is always deformed and exceeds the norm in width, height within 0.11 seconds. The PQ interval is extended.
The mechanism of occurrence of this disease
Failure of the contractile function of the heart muscle is usually caused by impaired excitability and conduction. In clinical practice, this includes atrial flutter and fibrillation, ventricular fibrillation or fibrillation. If a patient has chronic cardiac pathology, specialists are more often faced with atrial fibrillation.
It should be noted that atrial fibrillation is one of the most common and severe diseases of the cardiovascular system. This pathology was first diagnosed back in the 19th century, but the disease received its modern name at the beginning of the 20th century in the works of domestic scientists.
The main component of the development of the disease is considered to be a disturbance in the conduction of electrical and nerve impulses in the fibers of the atria. In this case, damage to the ventricles of the heart is secondary.
The entire nervous system of the heart is autonomous and depends little on the human central nervous system. The work of the heart muscle is regulated by several nodes. It is the malfunction and weakening of the conduction function in the sinus-atrial node that causes an increase in atrial excitability. The above node ceases to fulfill its main role as a pacemaker, which can be perfectly confirmed by various ECG signs of atrial fibrillation.
A large number of ectopic foci occur in the atria, which leads to a disruption in the rhythm of contractions of this part of the heart. Due to the fact that the myocardium is unable to respond to all incoming impulses, contractile movements occur in individual fibers of the atrial muscle, which resembles trembling or flickering.
Most often, such a pathology is observed only in the area of the atria; only individual impulses can leak to the ventricles, which causes inconsistency in the contractile work of the entire heart. However, most experts consider limiting the impact of excess nerve stimuli on the walls of the ventricles as a certain safety precaution.
The atria are responsible for only 25% of all pumped blood, which allows the body to compensate for such a disruption in hemodynamics with certain difficulties. Ventricular fibrillation most often causes the death of the patient, since the symptoms of circulatory failure in this case will be of a landslide nature.
Arrhythmia indicators on a tonometer
When it comes to arrhythmia, the tonometer may give incorrect values. Due to the lack of indication of heartbeat failures, the indicators may be greatly distorted. There are now good blood pressure monitors on the market that can perfectly recognize arrhythmia. Such devices immediately detect pulse irregularities and the sequence of contractions. As a rule, malfunctions in the heart are expressed by a heart at the bottom of the device monitor. Arrhythmia on the latest tonometers is displayed according to the following scheme:
Arrhythmia indicators on a tonometer
- first there are several measurements with pauses between them;
- if two of them passed without failures, then the process does not proceed further;
- the screen displays the pulse;
- The arrhythmia indicator lights up at the very bottom of the screen.
There is no need to worry that the device does not identify serious failures from minor irritations - all this is perfectly distinguished by a modern device. Such a device can be trusted, and if it reveals signs of arrhythmia, you should immediately consult a doctor. If the tonometer shows arrhythmia once, the result may be incorrect and you need to take another measurement.
How to choose a tonometer
For a person who periodically experiences interruptions in heart rhythm, it is very important to have a good blood pressure monitor on hand that can identify signs of arrhythmia. New generation devices produce results that are obtained on the basis of intelligent data analysis. They can work according to two principles:
- Some tonometers produce results by calculating the average value of the last three measurements;
- others carry out the required number of measurements themselves and, after processing their indicators, produce the final result.
Tonometers of this type are able to determine blood pressure even more accurately. This is an excellent opportunity to keep your blood pressure, heart rate and heart rate under control at the same time.
There is no need to worry if sometimes an arrhythmia icon appears during a normal blood pressure measurement. A constantly appearing indicator should cause alarm - this means that it is time to visit a doctor. If the sign of atrial fibrillation flashes on the screen, then you can no longer postpone the visit. When choosing a device, you need to focus on the following parameters:
- cuff size: it must strictly correspond to the circumference of the arm;
- The size of the screen must be sufficient for all indicators to be clearly visible;
- the arrhythmia indicator should be backlit, in some cases with sound;
- built-in memory can contain up to 90 records;
- function for calculating the average;
- a sound signal indicating the end of the measurement process;
- tonometers can be for the whole family - in this case, the indicators of each person are recorded separately;
- There are devices powered by both mains and batteries at the same time.
Modern blood pressure monitors are well suited for all people, they are easy to use and do not require any specific skills. They can even be used by patients who have hearing and vision problems. You just need to press a button, and the device does the rest without pain or discomfort in the form of strong tugging on the forearm.
The principle of dividing arrhythmia into types
There are several types of arrhythmia. The division into types is important because the patient’s further treatment, life prognosis, the likelihood of developing complications and much more depend on it. In addition, a person often exhibits several types of heart rhythm disturbances, which must be differentiated.
Arrhythmia is divided into types according to the principle of localization of the pathological focus, according to the frequency of heart contractions, and according to the nature of the failure. The Lown classification is also used.
Pulse counting for arrhythmia
People suffering from heart disease must be able to correctly count and evaluate their pulse. This is equally important for both fast and slow heartbeats. Sometimes this is what can prevent a heart attack in time.
To correctly determine the pulse, you need to locate the radial artery near the base of the hand, near the thumb. It is important to take into account the fact that the performance of the left and right hands may be slightly different. In order to detect the pulse, you need to lightly press your fingers on your wrist, clasping it from the back. It is the fingertips that will feel the pulse.
How to measure your pulse
The standard time is 15 seconds. Then the number of beats produced during this time must be multiplied by 4. The pulse counting time for arrhythmia is one minute, you need to count it by squeezing the artery with 3-4 fingers for the best detection of beats. Do not forget that there is also a pulsation in each finger, so it can be mistaken for a pulse. When measuring the pulse, the hand should be as relaxed as possible and placed with an open palm facing up. On a watch with a second hand, you need to wait for an even value and you can start counting. With different types of arrhythmia there will be completely different heart rate readings. For example, with tachycardia, more than 80 beats, with bradycardia - less than 60, paroxysms are characterized by a very rapid pulse - more than 200, with heart block it can reach 250-300.