Heart failure is a condition in which the heart muscle does not work well enough, causing blood to be retained in the systemic or pulmonary circulation and causing internal organs to lack oxygen.
Heart failure is not an independent pathology. It develops due to other diseases that affect the functioning of the heart.
To understand how heart failure is treated, it should be mentioned that it is divided into two types:
- Acute heart failure (AHF) is a condition in which the ability of the heart muscle to contract is sharply reduced, which leads to serious disruption of the blood supply and overload of the heart itself. It can occur suddenly, without any previous symptoms, or develop against the background of chronic heart failure. Treatment must be started immediately, otherwise this condition may result in the death of the patient.
- Chronic heart failure (CHF) develops gradually against the background of almost any disease of the cardiovascular system. The heart muscle cannot cope with the load and gradually weakens, symptoms of blood stagnation and oxygen starvation of internal organs appear. Treatment in this case should be aimed not only at eliminating these symptoms, but also at treating the disease that led to it.
Treatment of AHF
In the acute form, treatment of heart failure at home is unacceptable. Emergency medical care is required. Therapy should be aimed at improving the functioning of the myocardium, increasing its contractility, in order to improve blood circulation as quickly as possible and eliminate life-threatening symptoms: a strong increase in blood pressure, pulmonary edema and even cardiogenic shock.
Patients with AHF are hospitalized in a specialized department, where they are monitored for blood pressure, heart rate and respiration, body temperature, and an electrocardiogram is performed. With few exceptions, all medications are given intravenously because they need to start working as quickly as possible.
Treatment tactics for AHF:
- An important task is to provide the internal organs with oxygen to prevent the development of complications, so the patient is prescribed oxygen therapy. In the breathing mixture supplied to patients, the oxygen content is slightly increased compared to how much it is contained in ordinary air. This is necessary for better saturation of the blood.
- If there is no significant decrease in blood pressure, drugs that dilate blood vessels (vasodilators) are prescribed.
- If AHF is accompanied by a decrease in cardiac output, it is necessary to administer intravenous fluid in order to ensure vascular filling and maintain blood pressure at the proper level.
- Excess fluid is removed from the body by prescribing diuretics.
- It is necessary to eliminate the cause that led to the occurrence of this condition.
- Pain syndrome is relieved. For severe pain, the prescription of narcotic analgesics is justified.
- If necessary, cardiac catheterization may be performed.
- Medicines are prescribed to prevent recurrent attacks.
Cardiac glycosides
The group is represented by products of plant or synthetic origin. Preparations based on plant substances are obtained from foxglove, adonis, spring lily of the valley, oleander, strophanthus, etc.
The duration of the therapeutic effect, the accumulation effect in the body and the neurotoxicity of drugs depend entirely on their ability to form complexes with blood plasma proteins. The stronger the bond, the higher the effectiveness of the glycoside. Cardiotonic drugs of this group have an effect based on the following mechanisms:
- systole shortens with its simultaneous intensification;
- the rest period of the heart muscle is prolonged;
- heart rate decreases;
- the ability of the myocardial muscle to excite is enhanced;
- With an overdose of drugs, ventricular arrhythmia develops.
Drugs for the treatment of AHF
Morphine - it is usually prescribed in the early stages of severe AHF. It relieves pain well, has a calming effect, and also reduces the heart rate and dilates blood vessels.
Too large doses of morphine are not used, since it can cause a strong decrease in blood pressure, vomiting, and also depress breathing. Most often, complications from its use develop in older people.
- Vasodilators (Nitroglycerin, Nitroprusside, Nizeritide) - these drugs for the treatment of acute heart failure are used to reduce blood stasis without increasing the myocardial oxygen demand. They are used sublingually or intravenously, while monitoring blood pressure.
- ACE inhibitors - drugs in this group are usually not prescribed in the early stages of treatment, since their effect at this stage does not exceed the possible risks. They are more effective after the patient’s condition has been stabilized for further treatment.
- Inotropic drugs (Norepinephrine, Dopamine, Dobutamine) are used to improve myocardial contractility. However, their use results in the heart requiring more oxygen.
- Diuretics (Furosemide, Torasemide) are used in cases where excess fluid accumulates in the body during AHF. Their use allows you to remove excess fluid, reduce blood pressure and the load on the myocardium. It should be remembered that potassium and magnesium are removed from the body along with fluid, so it is necessary to monitor these indicators in the blood, and also, if necessary, ensure their additional intake. Using small doses of diuretics together with other groups of drugs is more effective than simply prescribing large doses of diuretics. Most patients tolerate the administration of these drugs well, but sometimes complications can develop, so it is necessary to monitor the patient's condition and monitor the body's response to the prescription of a particular drug.
- Cardiac glycosides - they are prescribed for certain indications, since they are able to increase cardiac output, thereby freeing the chambers of the heart from a large amount of blood.
- Beta-blockers (Propranolol, Metoprolol, Esmolol) are rarely used, since impaired myocardial contractility is a contraindication for their use. However, in certain cases their appointment may be justified.
Cardiotonic drugs: classification
The general effect of all drugs included in the group is based on the ability to increase the force of myocardial contractions, resulting in an increase in cardiac blood output and stroke volume. Cardiotonic agents reduce diastolic volume, pulmonary and systemic venous pressures, and ventricular filling pressures.
- Cardiac glycosides - Strophanthin, Korglykon, Digoxin.
- Adrenergic drugs – “Isadrin”, “Dobutamine”, “Dopamine”.
- Non-adrenergic synthetic drugs - Amrinon, Milrinone.
The choice of drugs used is related to the severity of the patient’s condition and the course of the disease.
Surgical treatment of AHF
In some cases, surgical methods are used to treat acute heart failure. The decision on this is made by a cardiologist, depending on what disease caused a sharp deterioration in the contractility of the heart. Typically, surgery is used in cases where drug treatment for circulatory failure does not bring results.
Surgical methods include:
- Myocardial revascularization
- Correction of certain defects both in the heart itself and in the valves
- Temporary maintenance of blood circulation using mechanical means
- In particularly severe cases, a heart transplant may be prescribed.
Adrenergic drugs
Non-glycoside cardiotonic drugs with a short-term effect. The group is used for acute heart failure to support important body functions.
"Isadrin" is a stimulator of adrenergic receptors in blood vessels, bronchi and the heart. The drug has a hypotensive effect and enhances the contractility of the heart muscle. It is used in cardiac surgery in case of a sharp decrease in contractility during surgical procedures, as well as in cardiogenic shock. Reviews from doctors warn: improper use or excess dosage can cause ventricular fibrillation of the heart.
"Dobutamine" is a cardiotonic drug with a non-glycoside structure that has a stimulating effect on the heart muscle and also normalizes coronary blood flow. The risk of developing arrhythmias when using this drug is quite low, since Dobutamine has virtually no effect on cardiac automatism.
Prescribed when there is a quick need to strengthen myocardial contractility. In some cases, it may cause side effects:
- nausea;
- headache;
- hypertension;
- increased heart rate;
- chest pain.
"Dopamine" is a catecholamine that stimulates adrenergic receptors. The drug increases blood pressure and increases coronary blood flow. Prescribed for acute myocardial failure, shock. Use with caution in case of myocardial infarction, pregnancy, thyroid diseases, arrhythmias.
Treatment of CHF
Chronic heart failure develops gradually against the background of any disease of the heart and blood vessels, so not only the symptoms of heart failure, but also the underlying disease must be treated. Diet and an appropriate lifestyle are important in treatment.
With CHF, the patient must follow a diet. It should be quite high in calories, but at the same time easily digestible, contain a lot of protein and vitamins. You should limit your salt and water intake as they contribute to edema and high blood pressure. Regular weighing will be a good habit for a patient with CHF, as this will allow timely detection of excess fluid accumulated in the body.
In addition, physical activity should not be underestimated. Physical inactivity has a bad effect on any person, and with CHF it is even more dangerous. Physical activity should be selected individually, depending on the underlying disease and general condition of the body. You should give preference to walking or light running, and take a lot of walks in the fresh air. Patients with CHF are not recommended to stay in a hot, humid climate for a long time.
With a mild course of the disease and under medical supervision, heart failure can be treated with folk remedies, however, if any deterioration in health occurs, you should immediately consult a doctor for timely diagnosis and adjustment of treatment.
For the treatment of acute and chronic heart failure
Clinical pharmacology of cardiotonic drugs
Heart failure is a complex of disorders caused mainly by a decrease in the contractility of the heart muscle.
HF occurs when the heart is overloaded and overworked (due to arterial hypertension, heart defects, etc.), disruption of its blood supply (myocardial infarction), myocarditis, toxic effects (for example, Graves' disease), etc. The consequence of HF is blood stagnation, since weakened heart muscle does not provide blood circulation.
Predominant failure of the left ventricle of the heart occurs with stagnation of blood in the lungs (which is accompanied by shortness of breath, cyanosis, hemoptysis, etc.), and of the right ventricle - with venous stagnation in the systemic circulation (edema, enlarged liver, etc.). As a result of CH.
Hypoxia of organs and tissues, acidosis and other metabolic disorders occur.
SN happens:
– acute (may manifest as an attack of cardiac asthma, pulmonary edema)
– chronic
Cardiac asthma (CA) – attacks of shortness of breath ( with difficulty inhaling
), sometimes reaching a degree of suffocation, caused by a pathological increase in pressure in the left atrium (a symptom of failure of the left heart).
The pathogenesis of an attack of SA is based on reflex excitation of the respiratory center due to excessive blood filling of the veins and capillaries of the pulmonary circulation, caused by difficulty in the outflow of blood from the pulmonary veins to the left atrium.
This occurs when there is an obstruction to blood flow in the left atrium (for example, with a large intra-atrial thrombus), but most often due to increased intra-atrial pressure due to insufficient contractile function of the left ventricular myocardium or due to mitral stenosis.
An important pathogenetic factor in the development of SA is an increase in the mass of circulating blood (for example, during pregnancy, fever) and an increase in venous return of blood to the heart, which leads to an increase in blood supply to the lungs if the outflow of blood from them to the left side of the heart is difficult.
Therefore, in patients with chronic heart failure, SA attacks are provoked by physical activity, horizontal body position, and the introduction of large volumes of fluid into the bloodstream. Attacks of SA most often occur at night during sleep. The patient wakes up from a feeling of suffocation, which is often combined with a feeling of fear of death.
Typically, shortness of breath has the character of polypnea (frequent and deep breathing), and may be accompanied by paroxysmal dry cough. The patient is forced to take a vertical position (orthopnea), often sits up in bed with his legs down; some patients get up and try to go to the open window.
Upon examination, pallor and cyanosis of the face, lips, and sometimes nail phalanges are revealed; the face is often covered with small drops of sweat.
Functional classes (according to the severity of the disease):
1. Patients with heart disease without restrictions on physical activity (very fast walking, climbing uphill is possible). Asymptomatic left ventricular dysfunction.
2. Patients with heart disease with slight limitation of physical activity (fast walking, climbing to the floor). Mild CH.
3. Patients with heart disease, with significant limitation of activity, in whom minor physical activity (walking on horizontal terrain) causes attacks of cardiac asthma. Moderate heart failure.
4. Patients with heart disease, in whom even minimal physical activity causes discomfort (even shortness of breath at rest). Severe HF.
Principles of treatment of heart failure
· Limitation of physical activity. In the 1st functional class - exercise therapy with a training regime of loads until the patient is tired.
· Limit the consumption of table salt to 5-6 g per day. and liquids up to 1000-1500 ml. per day Ensuring a sufficient supply of potassium and magnesium salts (for example, use multivitamin complexes containing these elements: sanasal, etc.
.).
· Drug therapy should be aimed at increasing tolerance to physical activity, reducing edema, shortness of breath, stress on the heart, enhancing myocardial contractility, and suppressing excess retention of salt and water in the body.
, 3 main groups of drugs are currently used
Cardiotonic drugs:
cardiac glycosides
Cardiotonic drugs of non-glycoside nature
Diuretics.
Peripheral vasodilators, including ACE inhibitors.
The main cardiotonic drugs for the treatment of heart failure are cardiac glycosides.
The implementation of the main property of cardiac glycosides - increasing the strength and speed of heart contractions - helps to increase cardiac output, reduce heart rate, reduce myocardial oxygen demand, improve gas exchange in the lungs, which leads to the elimination of shortness of breath, improvement of intracardiac and systemic hemodynamics (blood circulation), why the size of the heart decreases, diuresis improves (increases), swelling decreases; Cardiac glycosides also have an effect on the central nervous system, as a result of which they are often used together with bromides and valerian preparations as sedatives (adonis, lily of the valley preparations).
Application:
1. AHF, CHF
2. Pulmonary edema
3. To prevent heart failure before surgery
4. For the treatment of certain types of arrhythmias. Their arrhythmic action is based on the ability to slow down the conduction time of an impulse.
Side effects:
1. Arrhythmia, cumulation; result of cumulation => extrasystole, ventricular fibrillation until cardiac arrest in systole.
2. Large doses: nausea, vomiting, diarrhea
3. Loss of appetite
4. Central nervous system disorders: headache, blurred vision, anxiety, insomnia, depression.
Contraindications: angina pectoris, severe bradycardia, severe hypokalemia, hypercalcemia, intoxication with cardiac glycosides, thyrotoxicosis, tachycardia, arrhythmia; elderly people - with caution.
Poisoning:
1. Cardiac dysfunction (bradycardia, AV block, extrasystole, heart and coronary failure)
2. Gastrointestinal upset: (nausea, vomiting, diarrhea, abdominal pain, loss of appetite)
3. Central nervous system disorder: headache, aphasia (speech impairment), insomnia, dizziness, hallucinations, pressure in the eyes, blurred vision
4. Decrease in blood pressure
5. Cyanosis
6. Cramps
7. Coma
First aid:
Cancellation of cardiac glycosides, prescription of non-glycoside cardiotonics (dopamine, glucagon), IM - unithiol 5% solution 5-10 ml, Mg salts, antiemetic, antiarrhythmic drugs (lidocaine), for convulsions, hallucinations - aminazine.
Glycoside intoxication often occurs due to the ability of long-acting (digitoxin) and medium-acting glycosides (digoxin, celanide) to accumulate in the body.
The ability of SG to accumulate depends, on the one hand, on the strength of their connection with plasma proteins (digitoxin is 97% bound to proteins, has the highest degree of accumulation), on the other hand, on the ability of the drugs to dissolve in fats, which determines their good absorption in the intestine (this is digitoxin , digoxin, celanide), however, they are poorly excreted in the urine, due to insufficient solubility in water => the duration of their accumulation increases. On the contrary, drugs that are highly soluble in water and poorly absorbed from the housing and communal services should be administered parenterally (strophanthin, corglycon). They are well excreted by the kidneys. The duration of their action is not long, they do not accumulate.
Digitoxin is metabolized in the liver, however, most of it is excreted unchanged in the bile into the intestine, where it is reabsorbed. Enterohepatic recirculation continues until all non-protein-bound digitoxin is metabolized.
Didn't find what you were looking for? Use the search:
Source: //studopedia.ru/3_18420_dlya-lecheniya-ostroy-i-hronicheskoy-serdechnoy-nedostatochnosti.html
Principles of drug therapy for CHF
- It is necessary to detect the underlying disease, which led to a gradual deterioration in myocardial contractility and the development of heart failure. Correct treatment of the underlying disease will significantly improve the prognosis for the patient;
- If possible, it is necessary to eliminate those factors that may contribute to the occurrence of an attack of acute heart failure;
- Treatment of heart failure itself: reducing blood stasis and increasing cardiac output. Eliminating these two factors will improve blood supply to internal organs and eliminate symptoms of oxygen deficiency.
Certain groups of drugs are used to treat CHF. You can take them at home; if the course is uncomplicated, it is not necessary to go to the hospital, but you should still consult a doctor. He will conduct the necessary diagnostics, select the right medications and tell you how to treat heart failure at home.
All medications for the treatment of CHF are usually divided into three groups:
- Basic means - the effectiveness of these drugs has been proven and recommended in all countries of the world.
- Additional funds - they are prescribed according to indications.
- Auxiliary agents - their effectiveness is not 100% proven for CHF, but depending on the specific situation, the appointment of this group may be justified.
Let's take a closer look at each group.
Fixed assets:
- ACE inhibitors (Captopril, Enalapril) - these drugs should be prescribed to all patients with CHF, regardless of the stage, severity, etiology, form and other indicators. They slow down the course of the disease, protect internal organs, and lower blood pressure. When using them, undesirable effects may occur, such as a dry cough, a strong decrease in blood pressure, and deterioration of the kidneys. To avoid this, it is necessary to start treatment with small dosages, gradually increasing to the required numbers, not to take ACE inhibitors and vasodilators at the same time, and also not to take large doses of diuretics before the appointment.
- Angiotensin receptor antagonists - most often they are prescribed if the patient is intolerant of ACE inhibitors or has developed side effects.
- Beta blockers (Carvedilol, Bisoprolol, Metoprolol) - they are usually prescribed in addition to AFP inhibitors. They reduce heart rate and have an antiarrhythmic effect. They also start taking them with minimal doses, gradually increasing them. At the same time, it is advisable to increase the dose of diuretics, since the symptoms of heart failure may worsen due to a decrease in heart rate.
- Aldosterone receptor antagonists - these drugs have a slight diuretic effect and retain sodium in the body. They are usually prescribed for severe symptoms of heart failure, as well as after a myocardial infarction.
- Diuretics (diuretics) – are used when fluid accumulates in the body. Usually the weakest effective drug is prescribed to avoid the patient developing dependence.
- Cardiac glycosides (Digoxin) are herbal preparations produced from the foxglove plant. In large doses they are poisonous, but are indispensable in the treatment of heart failure caused by atrial fibrillation.
Additional tools:
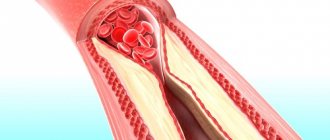
- Statins - they are used if chronic heart failure occurs against the background of coronary heart disease. Drugs in this group suppress the production of fats in the liver, which are deposited on the walls of blood vessels and cause narrowing or complete obstruction of their lumen, impeding the flow of blood through these vessels;
- Indirect anticoagulants - used when there is a risk of blood clots that can clog the vessel. These drugs interfere with the production of factors that promote blood clotting in the liver.
Auxiliary means:
- Nitrates - are prescribed mainly for angina pectoris to improve the nutrition of the heart itself and relieve pain, since they have a vasodilating effect and improve blood flow;
- Calcium antagonists - also used for angina pectoris, high blood pressure, heart valve insufficiency;
- If there are heart rhythm disturbances, antiarrhythmic drugs can be used;
- Disaggregants - these drugs are prescribed mainly to patients after myocardial infarction to prevent its recurrence. They impair the adhesion of platelets to each other, thereby thinning the blood and preventing the formation of blood clots.
Non-adrenergic synthetic cardiotonics
These are cardiotonic drugs used in cases of acute coronary insufficiency. The drugs act on the contractility of the heart muscle, strengthening it. They can provoke the development of arrhythmia and a decrease in blood pressure, and kidney problems.
Cardiotonic drugs of this group cannot be used for heart defects, as well as cardiomyopathy, heart rhythm disturbances, aortic aneurysm, kidney failure, heart attack and during pregnancy.
The drug "Amrinon" is used exclusively in intensive care units so that the patient is constantly under the control of special devices that indicate his condition. In addition to enhancing heart contractions, the drug dilates blood vessels, increases blood ejection during systole, and reduces pulmonary pressure.
Available in the form of a solution. For intravenous administration, it is diluted exclusively in physiological sodium chloride solution. Do not mix with other medications. When administered, a sharp decrease in blood pressure, increased heart rate, arrhythmia, headaches, and gastrointestinal disorders are possible.
"Milrinone" is more active than the first representative of the group, and, according to reviews, is better tolerated by patients. The use of the medication is contraindicated during pregnancy and the development of myocardial infarction. Belongs to group A drugs. The need to use the drug is determined exclusively by a doctor.
Surgical treatment of CHF
In some cases, when drug therapy does not have the desired effect, the patient's health deteriorates and life is threatened, surgical treatment may be prescribed. It is aimed at the underlying disease that caused heart failure.
Methods of surgical treatment:
- Aorto-coronary and mammary coronary bypass surgery - used in cases where the movement of blood through the coronary vessels is difficult due to narrowing of their lumen. Because of this, the myocardium does not receive enough oxygen for its work. With the help of shunting, bypass paths are created through which blood can go around the pathological focus;
- Correction of the heart valve apparatus;
- Heart transplantation from a donor;
- The use of artificial heart ventricles to create an auxiliary circulatory apparatus. This method is quite expensive and is dangerous due to complications: bacterial infection, blood clots.
Other drugs to support the heart
Digoxin helps restore a normal, steady heart rhythm and improve blood circulation by increasing the force of the heart's contractions. This drug is rarely used, but it is especially useful for patients who are often hospitalized due to fluid overload from heart failure. For those whose hearts are severely affected and have arrhythmia, digoxin can also be used to control the heart rhythm.
Many of digoxin's side effects are nonspecific, including nausea, vomiting, loss of appetite, and fatigue, making it difficult to determine whether they are related to the drug. If you experience problems with your vision, for example, difficulty seeing yellow and green colors, or the effect of flashes or flickering lights, you should consult a doctor.
Vasodilators, such as hydralazine and nitrates, are used to treat heart failure and control high blood pressure by relaxing blood vessels and improving heart function while taking pressure off the kidneys. Vasodilators are usually prescribed to patients who cannot take ACE inhibitors. Most patients tolerate the tablets well. But sometimes lupus symptoms occur, such as fever, joint or chest pain, sore throat, skin rash on the face, and swollen joints.
Common side effects of nitrates include headache, dizziness, or brain fog. If the patient feels dizzy or lightheaded, get out of bed or chair more slowly.
Treatment of CHF with folk remedies
Treatment of heart failure with folk remedies is possible only under the supervision of the attending physician as an addition to traditional medications. You should not prescribe treatment for yourself on your own, on the recommendation of a neighbor or a friend who has a “similar diagnosis,” and also ignore taking medications prescribed by your doctor, replacing them with folk remedies.
The following herbs are usually used to prepare folk remedies:
- Chopped blueberry shoots;
- Lily of the valley flowers;
- Foxglove leaves;
- St. John's wort herb;
- Parsley seeds;
- Dry ginseng root;
- Hawthorn flowers;
- Motherwort grass and many other plants.
It should be remembered that many of these plants are poisonous. Their incorrect use or failure to comply with the dosage can result in poisoning. Treatment with folk remedies only for symptoms of heart failure, without proper treatment of the underlying disease, will not bring the expected result and may worsen the patient’s condition.
Complex therapy
If shortness of breath occurs due to heart failure, complex treatment is indicated. If the syndrome is accompanied by cough and tachycardia, then the following treatment regimen is used:
- Diuretics, the action of which is aimed at removing excess fluid from the body and reducing the load on the circulatory system. Such medications include Indapamide.
- Drugs that dilate blood vessels (Losartan). They are taken only as prescribed by a doctor, as they have various contraindications.
What to take for heart pain?
Nitroglycerin and other nitrate derivatives are considered the most effective for chest pain. It can be taken 2 tablets under the tongue.
Some people experience severe headaches. Therefore, it is proposed to switch to prolonged (extended action) Sustak, Erinit. During an attack, you can use a spray of isosorbide dinitrate - Isoket. The main thing is to feel the quick effect of pain relief.
Validol is considered a mint tablet for freshening breath. It has no effect on the coronary vessels at all. Intramuscular or intravenous administration of solutions of antispasmodics Papaverine and No-shpa has very low effectiveness.
It is entirely justified for smokers to take Validol for fresher breath.
The effect of Corvalol and Valocordin on humans is based on the phenobarbital included in the composition. The pure drug is used for treatment in neurology and psychiatry, especially for seizures. It has been proven that its accumulation in cells leads to addiction, destroys mental abilities and reaction to others. Doesn't affect the heart. Banned everywhere except CIS countries.
General characteristics of drugs that improve heart function and vascular condition
An integrated approach to the treatment of cardiovascular pathologies is practiced. In the process of laboratory and instrumental diagnostics, the cause of the development of the disease is determined. First of all, it is necessary to eliminate provoking factors. For example, if the cause of a circulatory disorder is cholesterol blocks on the walls of blood vessels, then their dissolution and removal are required. Then drugs are used that restore the integrity of the coronary arteries, optimizing their permeability.
Only one remedy is rarely prescribed for treatment. Typically, cardiologists combine drugs from various clinical and pharmacological groups in therapeutic regimens. This allows you to simultaneously eliminate provoking factors and symptoms - pain in the heart, shortness of breath, high or low blood pressure. At the initial stage of treatment, cardiovascular drugs are used in the form of injection solutions, and then the result is secured by taking tablets.
Medicines that may worsen heart failure
The attending physician needs a complete list of medications that the patient is already taking. Some heart medications may make congestive heart failure worse or change the effect of the medications you are prescribed. Antiarrhythmic drugs, calcium channel blockers, and some beta blockers can be dangerous. Women are sometimes advised to avoid estrogens. Drugs like Viagra should not be used if nitrates are used in treatment.
It is important to always have a list of your medications with you. If the patient sees other doctors, including the dentist, it is important to make sure they are aware of all the pills, including vitamins, herbs and nutritional supplements.