When it comes to hemorrhages in newborns, many people associate them with severe traumatic births and medical errors. However, not all hemorrhages are associated with tissue trauma. We will talk about intraventricular hemorrhage (IVH) in newborns. They are typical for children born prematurely and are caused by the physiological characteristics of premature infants. IVH are a very serious problem, because the prognosis for the full life of premature babies largely depends on the nature of the pathological process and its proper treatment.
What is IVH of the brain?
IVH also occurs in adults and is a type of stroke that is almost 100.0% fatal. In this type of stroke, blood enters the cerebral ventricular chamber system from blood hematomas inside the brain.
During a stroke, intracerebral arteries rupture, which leads to hematomas.
Intraventricular hemorrhage (IVH) in newborns occurs in isolation. IVH is not associated with parenchymal hematomas, and therefore can be classified as an independent pathology.
Intraventricular hemorrhage (IVH) is one of the most common diseases in infancy in children born prematurely.
The cause of pathology in premature babies is an incompletely formed system of intracranial vessels.
Underformed vessels are at risk even with the slightest variability in the blood pressure index in the circulatory system.
The cause of rupture of the fragile walls of the arteries may be hypoxia of the brain, or head trauma when the child passes through the birth canal. When the arteries rupture, blood enters various chambers of the brain and IVH is formed.
Intraventricular hemorrhage in a newborn
The importance of the IVH problem
The importance of IVH pathology in newborn babies is due to a rather complex diagnostic study of the pathology, as well as its drug treatment. After all, many medications for the treatment of hemorrhage are not suitable for therapy in newborns.
Time also plays an important role in solving the problem, because the baby’s nerve centers are not yet sufficiently adapted to stress, so they simply may not be able to endure a negative situation.
In addition to children who were injured during the birth process, IVH pathology is quite often diagnosed in children born ahead of schedule.
And the shorter the period of intrauterine development of the baby, the higher the percentage of intraventricular hemorrhages.
In this situation, the complexity of brain hypoxia increases with a shorter period of intrauterine formation.
According to statistics:
- 50.0.0% of premature babies suffer from hemorrhage in the ventricles of the brain on the 1st day after birth;
- In 25.0% of infants, bleeding into the chambers of the cerebral ventricles occurs on the 2nd calendar day from the moment of birth.
If a child is born on time, then even with deviations from the normative course of the birth process, the probability of IVH ventricular hemorrhage does not exceed 5.0%.
Baby's head circumference
Premature babies have specific structure of the lateral ventricles and periventricular spheres: the arteries in them are in a germinal state and have a simple structure. These arteries are called the “subependymal germinal matrix.” They are very fragile and can easily be injured. Of no small importance is the complication of the decrease of venous blood from these areas, the pathology of the constancy of the internal environment of the body.
The impact of concomitant disorders in the blood coagulation system cannot be excluded. It can be both congenital and transient, in other words, temporary (usually due to the influence of certain medications). However, IVH does not occur in all babies born prematurely. For the most part, this also happens when the mother carried the baby. This factor negatively affects the baby's health. And therefore, you need to ensure that there is no post-term pregnancy.
Specific conditions have been identified that contribute to the appearance of IVH in children. Most of them are named below:
- The birth of a completely premature baby.
- Critical moments of hypoxia (lack of air to body tissues).
- High pressure in the venous bed (either during childbirth or during synthetic ventilation).
- Increased blood pressure, which increases brain bleeding.
- Changes in brain blood flow saturation.
- Difficulties of the blood coagulation system.
- Infectious and other inflammatory processes in the mother before childbirth or in children after them.
- Initial resuscitation assistance provided with defects or untimely.
- Regular attacks of respiratory arrest and respiratory pathologies, which are typical for premature and post-term infants.
- Injection into a vein of electrolytes, the concentration of elements in which exceeds their permissible values (this is called hyperosmolarity).
As you can see, there are many causes of IVH in newborns. The parents’ task is to eliminate them as much as possible.
In premature babies, it is important to monitor head circumference. When it grows in size by more than 10 millimeters per week, it is necessary to monitor the volume of the ventricles from time to time using the NSG method. As for the direct treatment of IVH, it largely depends on the level of hemorrhage and its complications. The same applies to a post-term, large baby with a suspicion of such a problem.
Etiology of IVH in newborn infants
The causes of hemorrhage in newborn babies are completely different from the causes that provoke stroke in adults.
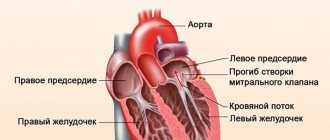
Causes of stroke in adults:
- Arterial hypertension (hypertensive crisis);
- Atherosclerosis of large diameter arteries;
- Cardiac ischemia;
- Coronary insufficiency;
- Arterial thrombosis;
- Stenosis of cerebral vessels.
In adults, during a stroke, a hematoma occurs inside the brain, and blood entering the chambers of the ventricles is a secondary manifestation of a stroke.
In infancy, a stroke (intracerebral hemorrhage) occurs immediately in the chambers of the ventricles.
The main reasons for what happens in the child’s brain are directly related to the course of pregnancy and labor:
- Premature baby;
- Hypoxia from a long period of the child being in the womb after the rupture of amniotic fluid;
- Hypoxia of the brain during the passage of the baby through the mother’s birth canal;
- Injury to the baby during obstetric care during childbirth;
- Low birth weight of a child - less than one kilogram;
- Pathologies of blood plasma coagulation, congenital genetic hereditary nature.
In children born prematurely, the main cause of IVH is considered to be the presence of a germinal matrix in such children.
This matrix disappears from parts of the brain during the maturation of the organ and the final formation of the intracranial vascular system.
The germinal matrix is a major risk factor for IVH.
Germinal matrix type
The germinal matrix is the cells of the organ tissue that are located around the ventricles. This matrix contains immature cells, which, when entering parts of the brain, are transformed upon further maturation into neurons, or into cells of neuroglial molecules.
In addition to these immature cells, the matrix also includes immature vessels that have a very weak membrane, which, at the slightest deviation from the norm of the blood pressure index, can burst and provoke blood to enter the newborn’s brain.
Hemorrhage into the cells of the germinal matrix is not yet a pathology of IVH, but this type of hemorrhage leads to blood entering the chambers of the ventricles of the brain.
A hematoma can form next to the ventricular wall and blood will begin to leak into the spatial ventricular lumen.
When a minimal volume of biological fluid enters the ventricles, a separate type of disease can be identified—IVH.
The stages of IVH pathology indicate the severity of the disease, and also determine the type of therapy and prognosis for the possibility of cure.
Possible complications and consequences
The peculiarity of the brain of a newborn child is the fact that it has excellent self-healing abilities. With a little treatment and proper treatment, it is possible to completely get rid of the pathology.
In addition, in the future the child will not experience negative consequences of hemorrhage, but full recovery may take from several months to 2 years.
Unfortunately, the prognosis is not always favorable and with serious brain damage the following complications may develop:
- hydrocephalus
- epilepsy
- developmental delay
In addition, death cannot be ruled out as a consequence of cerebral hemorrhage.
IVH grades according to CT method
Based on the results of deciphering the computed tomography technique, 4 degrees of development of IVH pathology were identified:
- Grade 1 - subependymal hematoma. Blood collects under the lining of the ventricle chambers of the brain. The liquid does not enter the ventricles and does not destroy the state of the brain space. The danger of a breakthrough of the subependymal membrane and intracerebral effusion of blood exists constantly;
- Grade 2 is a typical intraventricular hemorrhage without an expanded organ cavity. The filled subependymal space releases blood into the cavities of the ventricular chambers. The ventricles are filled with biological fluid to half their volume;
- 3rd degree - this is when blood enters the ventricles and fills them more than half, and in this situation the intraventricular chamber expands;
- Stage 4 premature babies are the most severe stage of the disease. At this degree, the ventricles are completely filled with blood, and biological fluid enters the tissue of the nerve endings. Parenchymal hemorrhage begins inside the brain.
Degrees of residential housing complex
Neurosonography
Neuroimaging is of primary importance in the early diagnosis of IVH and other intracranial defects. The obvious advantages of NSG are safety, speed, non-invasiveness, reliability, financial accessibility, absence of the need for sedation and radiation exposure, and the likelihood of repeated intra-vascular studies.
Transfontanel NSG is considered the main method for diagnosing IVH in newborns. In this case, recognition through the large fontanelle is mainly focused on assessing the state of supratentorial structures, including lateral structures and ventricles. More informative recognition is frontal, at the level of the foramina of Monroe;
and parasagittal, at the level of the thalamocaudal notch. In order to better visualize the structures of the posterior cranial fossa, additional study through the mastoid fontanel is necessary. With NSG, hyperechoic zones are formed in the matrix area, blood clots in the ventricles and ventriculomegaly can be detected.
Stages of IVH according to brain damage
According to the results of a tomographic study, changes in the structure of brain cells are visible, and based on these indicators, 3 stages of destruction of brain cells are distinguished:
- Stage 1 of organ damage . The ventricles are filled with biological fluid less than half, there is an option to stop the bleeding on their own, the chambers are not dilated. There is a possibility of normal functioning of the organ's liquorodynamics;
- Stage 2: The lateral ventricles are filled with blood and they expand. The lateral ventricles are filled with biological fluid by more than half and the blood proceeds to fill ventricles No. 3 and No. 4;
- Stage 3 of pathology is the most severe stage of damage to brain cells. Blood enters the protective membrane of the cerebellum, the medulla oblongata, and also into the cells of the spinal cord. More than 90.0% of cases of this pathology are fatal.
A disruption in the proper circulation of cerebrospinal fluid (CSF) and the development of hydrocephalus occurs due to blood entering the cerebral ventricle, where it mixes with the cerebrospinal fluid and does not immediately clot.
A partial volume of blood penetrates into other organs of the brain. The coagulation process begins in the blood, and blood clots close the pathways for the normal passage of cerebrospinal fluid (CSF).
Blockage of the cerebrospinal fluid passage leads to dilation of the cavities of the cerebral ventricles and the pathology of hydrocephalus with its characteristic pronounced symptoms.
Symptoms of IVH
Up to 90% of all blood effusions in the brain occur in the first 3 calendar days after birth. The likelihood of hemorrhage in premature babies directly depends on the weight of the child - the higher his weight, the lower the likelihood of developing IVH.
After 7 calendar days, the risk of IVH decreases, which is due to the adaptation of the arterial system of the brain to the external environment, and the maturation of the germ cell type matrix is also currently occurring.
After the first 3 days, premature babies should be under the close attention of neonatologists to avoid IVH.
First degree pathology occurs without visible symptoms. The second degree of pathology also quite often passes without visible symptoms.
The third and fourth degrees are a dangerous course of the disease, which can provoke the following complications:
- Dropsy of the brain;
- Hydrocephalus:
- Encephaly;
- Atrophy of brain cells.
Symptoms of IVH may not always have characteristic signs of intraventricular hemorrhage, and may also express other concomitant pathologies.
Symptoms that occur most often with IVH:
- The reflex to external stimuli disappears (reduced or completely absent Moro reflex);
- Muscle tone is significantly reduced;
- Drowsiness;
- Apnea attacks are attacks of respiratory arrest that immediately resume;
- Cyanosis of the skin;
- The skin is pale;
- The sucking reflex is very weak or completely absent;
- Refusal to eat;
- Visual function is impaired (the child practically does not move his eyes, but looks at one point);
- The cry is very weak;
- Muscle tissue spasms;
- Paresis;
- Acidosis (there is an imbalance between the acidic environment in the body and the alkaline environment);
- Impaired hematocrit;
- Blood transfusion develops;
- The fontanel is enlarged and constantly swells;
- Comatose state with hemorrhagic hemorrhages;
- A state of coma with greatly distended cerebral ventricles, even if biological fluid does not enter the cerebral cortex.
The mildest stage of the pathology does not cause a blockage to the passage of cerebrospinal fluid (CSF), the size of the chambers of the cerebral ventricles does not change, and the course of this type of hemorrhage can only be determined by the result of a clinical analysis of biochemistry - hematocrit.
In the transcript, hematocrit values are reduced.
When there is periventricular bleeding in the brain, the child exhibits the following symptoms in the body:
- Depressed emotional state (the child does not respond to external stimuli and bright light);
- Weakness of muscle tone;
- Paresis;
- Disturbances in the nerve endings of the eye organ - strabismus develops, as well as nystagmus;
- Disturbances in the respiratory system (signs of heavy breathing appear, as well as temporary apnea).
With the spasmodic type of the disease, symptoms appear for only a couple of days, and then the symptoms gradually subside. This is a consequence of the restoration of the functionality of the brain organs, or, on the contrary, a deviation in the performance of brain cells.
Deviations with this type of pathology are minor, which does not fundamentally affect the life prognosis.
Other types of hemorrhages in newborns
Cerebral hemorrhage in a newborn
Cerebral hemorrhage in a newborn, as described above, is divided into:
- Epidural;
- Subarachnoid;
- Hemorrhages in the substance of the brain and ventricles;
- Subdural.
In the first days of life, other types of bleeding may be detected in infants.
Hemorrhage in the adrenal gland in a newborn
It can develop due to incorrect obstetric management of labor and mechanical trauma to the fetus.
On the third day of the child’s life, the resulting hematoma disintegrates and a sharp deterioration in the baby’s condition is observed. The signs are:
- Severe muscle hypotension;
- Pressure drop;
- Vomit;
- Intestinal paresis.
For diagnostic purposes, urgent radiography and ultrasound of the abdominal cavity are prescribed.
Treatment may require surgery to remove the hematoma and hormonal therapy. The consequences of the disease can be chronic adrenal insufficiency.
Bleeding in the eye in newborns
It is observed in forty percent of cases during difficult labor with the use of stimulating medications and vacuum obstetrics. Typically, such bleeding disappears without a trace in the first couple of weeks and is in no way related to cerebral hemorrhages.
Diagnostics
The pathology of IVH cannot be independently diagnosed and diagnosed. There are many diseases that exhibit the same or similar symptoms. Therefore, an instrumental diagnostic examination of the cerebral arteries and their interpretation is prescribed by a neonatologist, as well as an ultrasound examination of all abdominal organs.
With timely diagnosis, it is possible to begin drug treatment for pathologies of organs that are not visible visually, but are identified during an instrumental examination of the body.
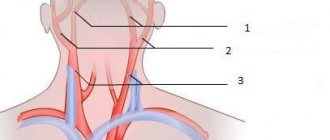
If the blood vessels in the brain are weak, an ultrasound scan must be done immediately after birth to avoid advanced stages of ventricular hemorrhage.
Also, in addition to the instrumental type of diagnosis, clinical testing of blood composition is added to determine the presence of anemia and inflammatory processes in the internal organs in the body.
Treatment
IVH is quite difficult to treat, because this pathology is not a disease, but IVH is a process in the brain that provokes quite serious complications and serious consequences.
In the first degree of hemorrhage and in the second degree of the disease - constant monitoring of the course of the pathology.
If the state of the brain is in a stable development of pathology, then drug therapy is used to eliminate the consequences of bleeding inside the cerebral ventricles.
When the first and second degrees of hemorrhage occur, there is no destruction of brain cells, abnormalities in the brain occur extremely rarely, and with 1st degree consequences, and with 2nd degree complications occur very rarely.
When treating such children, they are given all the conditions that are close to intrauterine interruption:
- Air circulation;
- The temperature regime is similar to the mother's womb;
- Required air humidity;
- Light indicators.
These conditions can be provided by a special pressure chamber, in which the baby is kept until the condition stabilizes after a cerebral hemorrhage.
The course of drug therapy with drugs includes:
- Preparations for stabilizing the blood pressure index in order to avoid the consequences of its sharp drop - hypoxia of brain cells, as well as hypoxia of nerve fibers;
- Oxygen therapy technique;
- Anticonvulsants;
- Drugs to normalize blood coagulation - coagulants, anticoagulants.
To reduce pressure in the arteries of the intracranial box, drugs are used intravenously orally, as well as intramuscularly:
Magnesia sulfate;- Medicine Diacarb;
- Diuretic drug Furosemide;
- Medicinal drug Veroshpiron.
Therapy with anticonvulsants:
- Medicinal drug Diazepam;
- Valproic acid.
An infusion is also carried out to cleanse the body of intoxication, and an intravenous injection of sodium bicarbonate is used to relieve the symptoms of acidosis.
To treat a more complex stage of IVH disease, the following surgical techniques are used:
- Ventricular puncture (via the fontanelle);
- Lumbar puncture (through the lumbar region);
- Liquor filtration technique;
- Liquor absorption method;
- A technique for washing the brain chambers of the ventricles using an artificial fluid, which is identical in properties to cerebrospinal fluid;
- Ventriculoperitoneal shunting. This technique is carried out when there is a blockage of the cerebrospinal fluid channel, or in case of hydrocephalic type syndrome. The treatment method involves inserting a drainage tube into the ventricles. This tube extends from the brain under the skin into the abdominal cavity, where cerebrospinal fluid (CSF) is absorbed. The drainage system must operate continuously and the drainage hose must be replaced as necessary.
Inserting a catheter for ventricular drainage
Is there a cure for hydrocephalus?
If the pathology of hydrocephalus has produced irreversible effects in the organ, and there is no positive result from drug therapy with fibrinolytics, then the only correct way out to save a life is surgical intervention in the body to install permanent drainage of cerebrospinal fluid:
- Installation of permanent drainage with a silicone tube. The tube is removed after the child’s condition has normalized and only after hydrocephalus has stopped progressing;
- Anastomosis using an endoscopic technique between the ventricles of the brain organ and the basal basin.
Preventive measures for pathology within the ventricular effusion of blood
There are no techniques that can 100.0% prevent IVH cerebral hemorrhage, but to reduce the number of risk factors, you can take some precautions:
- The first event is to determine the tactics of the birth process;
- If the woman in labor has a narrow pelvis and the baby’s head is large in diameter, the birth process should be a cesarean section;
- If there is poor blood coagulation in the fetus (genetic intrauterine pathologies), or in the woman in labor, a caesarean section is used.
Immediately after the birth of the child, drug therapy is prescribed to adjust blood plasma coagulation:
- Drugs of the corticosteroid group;
- Medicines of the immunoglobulin group;
- A platelet mass solution is administered by intra-arterial injection.
Drug therapy to adjust blood plasma coagulation
Who is at risk?
Brain hemorrhage in newborns can be associated both with damage to the skull itself and with a lack of oxygen.
Prerequisites for DRC:
- Post-maturity or, conversely, under-maturity. Premature babies are especially susceptible to intracranial hemorrhages, since their immature vessels do not yet have sufficient support in the tissues. In babies born late, the bones harden and the head is unable to adjust during birth. According to statistics, IVH occurs in every fifth premature baby and every tenth post-term baby.
- The size of the fetal head does not correspond to the size of the birth canal. In this case, natural delivery is contraindicated, because it is fraught with injury and hypoxia for the newborn baby.
- Difficult pregnancy (fetal hypoxia, intrauterine infection with various infections).
- Difficult (protracted or rapid) labor, breech presentation.
- Incorrect actions of obstetricians during childbirth.
Based on the above, several risk groups can be identified.
The risk of cerebral hemorrhage in a child increases with:
- prematurity;
- low birth weight (less than 1.5 kg);
- oxygen deficiency (hypoxia);
- child's head injury during childbirth;
- breathing complications during childbirth;
- infections leading to blood clotting disorders.
If the child belongs to at least one of these groups, it is necessary to find out whether he has symptoms of intracranial hemorrhage.
There are not always visible signs of hemorrhage. Also, if a child has any of the following symptoms, then it is not at all necessary that this is due to IVH; they can also be caused by other diseases.
The most common symptoms of intraventricular hemorrhage in infants:
- decrease or disappearance of the Moro reflex (to external stimuli);
- decreased muscle tone;
- drowsy state;
- episodes of apnea (stopping breathing);
- pale skin, cyanosis;
- refusal to eat, weak sucking reflexes;
- oculomotor disorders;
- weak and shrill cry;
- muscle twitching, convulsions;
- paresis;
- metabolic acidosis (disturbed acid-base balance);
- decrease in hematocrit or absence of its increase due to blood transfusion;
- a large fontanel is tense and bulging;
- coma (with severe hemorrhages, as well as concomitant hemorrhages in the cerebral cortex, significant stretching of the ventricles).
In premature infants, IVH manifests itself as a sharp and rapid deterioration of the condition on the second or third day after birth.
There are several classifications of hemorrhages, most of them include 4 stages. Below is the gradation most often used in modern medicine:
- IVH of 1st and 2nd degrees. Hemorrhage is observed in the projection of the germinal matrix and does not spread into the lumen of the lateral ventricles. In the second stage, the hemorrhage is slightly larger (1 cm) than in the first.
- At grade 3, hemorrhage from the germinal matrix enters the lumen of the lateral ventricles. As a result, posthemorrhagic ventriculomegaly or hydrocephalus develops. On the tomogram and section, expansion of the ventricles is observed, in which blood elements are clearly visible.
- Grade 4 is the most severe, IVH breaks through into the periventricular parenchyma. Hemorrhage is observed not only in the lateral ventricles, but also in the substance of the brain.
It is possible to establish one or another degree of hemorrhage only with the help of a special study.
For diagnosis in the presence of corresponding symptoms, as a rule, ultrasound of cerebral vessels is used (using sound waves, vascular ruptures and bleeding are determined). Blood tests are also taken to check for anemia, metabolic acidosis, and infections.
When diagnosing a pathology of any degree, the specialist selects individual treatment for the patient.
Basically, therapy for IVH is aimed at eliminating complications and consequences. If any diseases arise as a result of hemorrhage, appropriate treatment is prescribed.
Sometimes (if too much fluid accumulates in the brain), the following measures are applied:
- Ventricular (through the fontanel) or lumbar (through the lower back) puncture.
- Ventriculoperitoneal shunting, when a special drainage tube is inserted into the ventricles. It is pulled under the skin into the patient's abdomen, where excess cerebrospinal fluid is absorbed. The drainage system must remain in the body at all times, and the tube must be replaced if necessary.
It should be noted that for the majority of patients (with degrees 1 and 2 IVH) no therapy is required at all; one can count on a favorable outcome.
Be careful, video of the operation! Click to open
The consequences will depend on the degree of IVH and the adequacy of the actions of the medical staff:
- Grades 1 and 2 hemorrhage often do not require any treatment. Such infants need to be monitored; the likelihood that any neurological abnormalities will occur is low. Cases of the development of hydrocephalus and death with 1st and even 2nd degree disorders are extremely rare.
- 3rd degree. When hemorrhage breaks through into the ventricles, the likelihood of developing hydrocephalus increases; it can occur in approximately 55 percent of cases. Neurological abnormalities are observed in 35%. On average, death occurs in every fifth child. Patients are indicated for surgical intervention, and the outcome depends on the extent of brain damage and location (prognosis is more favorable if IVH is present within only one lobe, especially only in the frontal lobe).
- 4th degree. Unfortunately, the prognosis for such severe pathology is disappointing. Surgical intervention in this case is inevitable, but the risks of death remain high - approximately half of infants with stage 4 IVH die. In 80% of cases, hydrocephalus develops, in 90% - neurological abnormalities.
Preventive measures
It is impossible to prevent hemorrhage in the baby’s brain one hundred percent, but to reduce the risk, some measures can and should be taken.
Often perinatal intracranial hemorrhages occur due to birth injuries, so it is extremely important to carefully assess the relationship between the mother’s pelvis and the fetal head.
If there is a discrepancy, natural childbirth is contraindicated and a caesarean section is prescribed. This operation is also performed for diseases associated with a decrease in platelets in the blood of a pregnant woman or fetus (poor clotting).
In addition, in this case, special therapy is prescribed (corticosteroids, immunoglobulin, platelet mass). During childbirth, it is important to monitor the baby's blood pressure; it is necessary to avoid its fluctuations so that cerebral blood flow does not increase.
Although these studies are not mandatory for a pregnant woman, they should not be ignored.
In addition, you should know that intracranial hemorrhages are possible not only in newborns. They can occur as a result of injury at absolutely any age.
Preventive measures (IVH) for the expectant mother
Since this pathology cannot be prevented, then to facilitate the birth process, certain preventive measures can be taken:
- During the period of intrauterine formation of the baby, a pregnant woman should visit the attending doctor regularly;
- Systematically undergo clinical laboratory tests in order to determine deviations in the formation of the fetus and the development of intrauterine pathologies;
- Promptly treat infectious diseases in a pregnant woman, as well as treat pathologies in a baby in utero;
- Undergo instrumental examination;
- Consult your doctor about the risk of having a baby prematurely. If there is a provoking factor for premature birth, then the doctor will prescribe a course of medications to strengthen the fetal cerebral arteries, which will reduce the risk of intrapartum intrauterine congestion;
- A pregnant woman must maintain a healthy lifestyle: no nervous stress, give up nicotine addiction, do not drink alcoholic beverages;
- Constantly adjust the blood pressure index;
- Avoid sudden changes in temperature;
- Don't be in the heat.
Observation and treatment of children with IVH
Taking into account the fact that intraventricular hemorrhages are considered to be the lot of premature babies, they are monitored in the neonatal intensive care unit, and then in the nursing department for small children who were born prematurely. It is very important to observe the correct regime in the department. Doctors and nurses strive to schedule most of the manipulations at a constant time, so as not to unnecessarily disturb the children.
It should be taken into account that in addition to this pathology, the baby has many other associated problems: immaturity of the lungs and breathing problems, respiratory rate in newborns is disturbed, cardiovascular pathologies, difficulties in absorbing formula or breast milk, frequent layering of the infectious process, etc. .
Prognosis for life with IVH
The prognosis for life with IVH directly depends on the degree of cerebral hemorrhage.
- Grade 1 (mild) in which important centers of the brain are not affected - the prognosis is favorable.
- Grade 2 (moderate severity) , in which the ventricles are half filled, but do not have stretched membranes - the prognosis is favorable with the qualified help of the treating doctors.
- Grade 3 (severe) is aggravated by hemorrhage due to cerebral hydrocephalus.
Hydrocephalus occurs in 55.0% of newborns with hemorrhage.
35.0% receive significant deviations in the functioning of the brain of a neurological nature.
20.0% of IVH cases result in infant death.
With timely surgery to drain cerebrospinal fluid, the chances of life increase slightly and the prognosis is slightly favorable.
Stage 4 IVH is the most difficult stage to treat. Only surgical techniques are used, but even with timely therapy, 50.0% of babies die in the first day after the birth process.
80.0% of children suffer from the pathology of hydrocephalus, which also often leads to death - the prognosis is unfavorable.
90.0% of infants have neurological disorders that lead to a shortened life span.
Grade 3 and grade 4 IVH - the prognosis is unfavorable.
Consequences for children
The danger of the pathology lies in the fact that when a vessel ruptures, some areas of the brain stop receiving micronutrients and oxygen and are compressed by the accumulated fluid. The consequences depend on the speed of medical care and the degree of damage. Minor hemorrhage, if detected and treated in a timely manner, will not cause serious harm to the child. The course of treatment can range from 2 months to several years.
Consequences of a more severe form of pathology:
- coma;
- hydrocephalus (we recommend reading:);
- epilepsy;
- developmental disorder;
- cerebral edema;
- strabismus;
- speech disorders.