AB heart block is a particular variant of impaired contractility of the heart muscle. At its core, this is a weakening or complete cessation of the conduction of an electrical impulse through the atrioventricular node.
Treatment is not always required. In the early stages, recovery is not carried out at all; dynamic observation is indicated.
As it progresses, drug therapy is prescribed. The duration of the full development cycle of the deviation is approximately 3-10 years.
Symptoms appear much earlier than the terminal phase. They are quite pronounced. Therefore, there is time for diagnosis and treatment.
All activities are carried out under the supervision of a cardiologist and, as necessary, related specialists.
Classification of AV blocks
The division is carried out on three grounds.
Depending on the nature of the flow:
- Spicy. It is relatively rare and occurs as a result of severe external factors. Injuries, vomiting, sudden changes in body position, the course of somatic pathologies, all these are moments in the development of the process. The risks of cardiac arrest are maximum. Correction of the condition and stabilization of patients is carried out in a hospital setting, under the supervision of a group of doctors.
- Chronic form. Diagnosed in every second case of the total number of AV blocks. It is a lightweight option. Manifestations are minimal, and the likelihood of death is also not high. Restoration is carried out as planned. Treatment is medicinal or surgical, depending on the stage.
According to the degree of impairment of the functional activity of fibers:
- Complete AV block. There is no conduction of the electrical impulse from the sinus node to the atrioventricular node at all. The result is cardiac arrest and death. This is an emergency condition and can be treated in intensive care.
- Partial blockade of the atrioventricular node. It occurs more easily and accounts for the majority of clinical cases. But we must remember that progression may be abrupt, but this is relatively rare.
It is possible to subdivide the process according to the duration of the flow:
- Constant blockade. As the name suggests, it does not go away on its own.
- Transient (transient). The duration of the episode is from a couple of hours to several weeks and even months.
- Paroxysmal or paroxysmal. Duration about 2-3 hours.
Etiology
The causes of AV block are given in the table. The most common cause is isolated disease of the conduction system (Lenegre's disease). In addition, AV block can occur during myocardial infarction, usually in the first 24 hours. It occurs in patients with inferior myocardial infarction and in 2% of patients with anterior infarction.
| Causes of AV block |
Medicines
|
IHD
|
Isolated disease of the cardiac conduction system
|
Congenital heart defects
|
| Calcification of valve rings |
| Cardiomyopathies |
Infiltrative myocardial diseases
|
Inflammatory diseases
|
| Collagenoses (systemic scleroderma, rheumatoid arthritis, Reiter's syndrome, systemic lupus erythematosus, ankylosing spondylitis, polymyositis) |
Metabolic disorders
|
Endocrine diseases
|
AV node damage
|
Tumors
|
Neurogenic causes
|
Neuromuscular diseases
|
Four degrees of severity
The generally accepted clinical classification is based on severity. Accordingly, there are 4 stages in the development of the process.
1st degree (mild)
It occurs against the background of other cardiac and extracardiac pathologies. Manifestations of the subjective plan are minimal or completely absent. At the level of diagnostic techniques, there are minor deviations in the ECG picture.
Recovery is possible within 6-12 months, but is not always required. Dynamic observation is indicated, and the use of medications as needed.
2nd degree (medium)
It is further divided into 2 types, depending on electrocardiographic data.
- 2nd degree AV block Mobitz 1 is characterized by a gradual prolongation of the PQ interval. Symptoms are also uncharacteristic. Minimal manifestations occur that are practically unnoticeable if you do not overload the body. Provocative tests are quite informative, but can pose a danger to health and even life. Treatment is identical, with more emphasis on medication.
- 2nd degree AV block Mobitz 2 is determined by the loss of ventricular complexes, which indicates incomplete contraction of cardiac structures. Because the symptoms are much brighter, it’s difficult not to notice them.
3rd degree (severe)
It is determined by pronounced deviations in the functioning of a muscular organ. Changes on the ECG are easy to detect, the manifestations are intense - an arrhythmia occurs, such as a slowdown in contractions.
Such signs do not bode well. Against the background of complex organic defects, weakening of hemodynamics, tissue ischemia occurs, and multiple organ failure is possible in the initial phase.
4th degree (terminal)
Determined by complete blockade, heart rate 30-50. As a compensatory mechanism, the ventricles begin to contract at their own rhythm, and separate areas of excitation arise.
All chambers work in their own way, which leads to fibrillation and ventricular extrasystole. The death of the patient is the most likely scenario.
Clinical classifications are used to identify a specific type of disease, stage, determine treatment tactics and diagnosis.
Classification
By frequency and periodicity of development:
- persistent - is identified and persists in the future;
- transient (transitory) - was discovered once, but subsequently disappeared;
- intermittent - after detection it passed, but then reappeared.
Based on the location of the block, AV blockade is divided into:
- proximal (violation in the part of the node closest to the atria);
- distal (the part close to the ventricles is affected);
- There are combined blockades.
Causes of 1st degree AV block
These are mainly external factors. They can be eliminated by the patient himself, with rare exceptions.
- Intense physical activity, excessive activity. There is such a thing as a sports heart. Conduction disorders are the result of the development of cardiac structures. Such causes account for up to 10% of all clinical situations. But such a diagnosis can be made after long-term observation and exclusion of organic pathologies.
- Excess of medications. Cardiac glycosides, psychotropic drugs, calcium channel blockers, antispasmodics, muscle relaxants, narcotic analgesics, corticosteroids.
- Violation of the processes of inhibition of the nervous system. A relatively harmless factor. Usually it is part of a symptom complex of a disease.
Causes of AV block
The causes of the disease can be divided into organic and functional.
There are also a number of syndromes in which isolated degeneration of the AV node and His bundle is noted.
1) In the first case, partial anatomical (structural) damage to the conduction system is observed. This is observed, for example, when the node is involved in fibrosis after myocardial damage, with myocarditis, coronary heart disease, and Lyme disease. Congenital ab blockade is rare (children of mothers with CTD suffer). The AV node is often involved in inferior myocardial infarctions.
2) With a functional blockade, the morphology of the node is not impaired, only the function suffers, which, of course, is better amenable to correction.
This condition occurs when the tone of the parasympathetic nervous system predominates, antiarrhythmics are taken (beta-blockers - bisoprolol, atenolol; calcium channel blockers - verapamil, diltiazem; glycosides - corglikon, strophanthin), electrolyte disturbances (hyper-/hypokalemia).
It is also worth saying that 1st degree AV block can also normally occur, and no treatment is required. This happens, for example, among professional athletes and young people. 3) Degenerative changes in the AV node due to genetic pathology.
They develop due to mutations in the gene encoding the synthesis of sodium channel proteins in cardiomyocytes.
The following syndromes are specific: Leva, Lenegra, idiopathic calcification of the node.
Causes of 2-3 degree blockade
Much more serious. Possible factors include:
- Myocarditis. Inflammatory pathology of the muscular layers of an organ of infectious or autoimmune (less commonly) origin. Occurs as a consequence in most cases.
Treatment in a hospital, the clinical picture is clear. A terrible complication - destruction of the ventricles is determined in every tenth case.
Especially without special antibacterial and supportive effects.
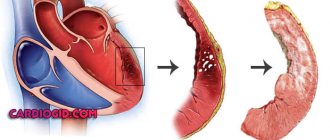
- Heart attack. Acute disturbance of trophism of cardiac structures. Occurs at any age, mainly in elderly patients. Also against the background of current ischemic heart disease, as a complication.
It ends with necrosis of cardiomyocytes (heart cells), replacement of active tissue with scar tissue. It is unable to contract and conduct a signal. Hence the AV block.
Depending on the extent, we can talk about the degree of severity. The more structures damaged, the more dangerous the consequences.
Complications of a major heart attack are described in this article, the symptoms of a pre-infarction condition are here, the causes and risk factors are here.
- Rheumatism. Autoimmune process affecting the myocardium. The treatment is long-term, lifelong maintenance therapy is the result.
It is possible to slow down the destruction and prevent relapses, but complete relief is unlikely.
The neglected phenomenon ends with damage to the His bundles and conduction disturbances.
- Ischemic disease. It is similar in nature to a heart attack, but the process does not reach a certain critical mass, since the blood supply still remains at an acceptable level. However, necrosis of the muscle layer will not take long to occur without treatment. This is the logical conclusion of IHD.
- Coronary insufficiency. As a result of atherosclerosis with narrowing or occlusion of the corresponding arteries supplying cardiac structures. Manifestations occur in later stages. Blockade is one of the organic disorders. Read more about coronary insufficiency here.
- Cardiomyopathy. The generic name of a group of processes. Arises as a consequence of severe somatic pathologies.
The essence lies in dystrophy of the muscular layer of the heart. Contractility decreases, the signal is transmitted through damaged tissues worse than in the normal position.
Weakened hemodynamics, ischemia, multiple organ failure as a consequence. Types of cardiomyopathy, causes and treatments are described in this article.
The presence of pathologies of the adrenal glands of the deficient type, the thyroid gland, and blood vessels, including the aorta, also affects.
The list goes on. There is an opinion about the participation of a hereditary factor in the process. Whether this is true or not is not entirely clear. In recent years, the role of the genetic component has been actively studied.
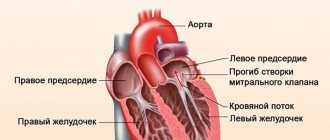
The essence of the disease
The heart muscle has nodes on its surface, presented in the form of clusters of nerve cells.
It is in these nodes that nerve impulses are formed, which are transmitted along nerve fibers through the myocardium to the cardiac atria and ventricles, causing their contraction. In the atrium there is one type of node - the sinus-atrial node, where an electrical impulse occurs and enters the atrioventricular node. As a result of this, the heart is able to contract.
Violation of the conduction process is heart block. If the impulses are not partially transmitted, we can talk about a partial blockade, and if the transmission stops completely, we can talk about a complete heart block. But regardless of the type of pathology, the patient’s heart contraction process is disrupted.
When the passage of the nerve impulse slows down, the patient lengthens the pause that occurs between the contraction of the ventricles and atria. When impulse transmission completely stops, contractions of the ventricles and atria do not occur. In this case, the patient develops ventricular or atrial asystole.
Violation of the transmission of electrical impulses can occur at different stages, which leads to the formation of blockades of various forms. If the transmission of NI is completely stopped, the blood does not pass through the blood vessels, which leads to a decrease in pressure and insufficient supply of oxygen to the internal organs of the human body.
Symptoms depending on the degree
The clinical picture depends on the stage of the pathological process.
Stage 1:
Manifestations are completely or mostly absent. The patient feels normal, there are no deviations in his vital functions.
Functional defects can be detected only by electrocardiography results. Often this is an accidental finding, discovered during a preventive examination of a person.
Mild shortness of breath is possible during intense physical activity (work, running, exhausting sporting events).
Attention:
First degree atrioventricular block is clinically favorable. If detected early, there is a chance of complete recovery without consequences.
Stage 2:
- Chest pain of unknown origin. Occurs in most cases. This is a non-specific sign. The duration of the episode is no more than a few minutes.
- Shortness of breath due to intense physical activity. She is not in a calm state.
- Weakness, drowsiness, lack of performance. Apathy and reluctance to do anything are possible.
- Bradycardia. Change in heart rate downwards. It is not yet threatening.
Stage 3:
- Shortness of breath with little physical activity. Even with simple walking.
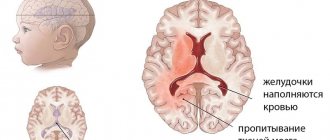
- Headache. Determined by ischemic disorders in cerebral structures. The duration varies from a few minutes to hours and even days. It is necessary to differentiate from migraine.
- Vertigo. Up to uncoordination of movements, inability to navigate in space.
- Arrhythmia of several types at once. The slowdown in cardiac activity is accompanied by a change in the time intervals between contractions.
- Fainting.
- Lowering blood pressure to critical levels.
- A sharp drop in heart rate.
All three symptoms presented above are part of the structure of the so-called Morgagni-Adams-Stokes syndrome. This is an emergency. It lasts a few minutes, but poses an enormous danger to life.
Injury, stroke, heart attack or cardiac arrest are possible. If this kind of manifestation occurs, surgical treatment is necessary, the essence of which is the implantation of a pacemaker.
Stage 4:
It is not always called. It is a variation of the previous one, but is characterized by even more severe symptoms. Massive organic disturbances are noted in all systems.
Death with 4th degree AV block becomes inevitable, it’s a matter of time. However, in order to trigger pathology in this way, you need to try and consciously ignore all the signals from your own body.
Symptoms
Dizziness and weakness
Atrioventricular block may be discovered incidentally during a medical examination, as some types are asymptomatic. An example is atrioventricular block of the first and second degrees (initial, single ventricular complexes are lost - degree 2, type 1).
In the second degree of type 2, as well as in advanced blockade, when 3 or 4 impulses in a row do not reach the ventricles, hemodynamics worsen. That is, for three or four contractions of the atria there was only one contraction of the ventricles, the remaining 3-4 impulses simply did not reach their destination. If the atria contracted 80 times in one minute, then the ventricles contracted only 20-30 times. Under such conditions, the nutrition of both the heart muscle and the brain deteriorates. Patients may complain of dizziness and weakness, fatigue, darkening of the eyes, and a feeling of cardiac arrest.
Distal atrioventricular block
The 3rd degree block is still complete in another way. The impulse from the atria does not travel to the ventricles at all. Therefore, the underlying nodes of the conduction system of the heart are triggered. This may be the atrioventricular node, if the block is located more proximally (higher) along the conduction system, or the His bundle (distal block). With complete AV block, 2 pacemakers work: the atria are excited from the sinus node, the ventricles from the AV node or from the His bundle. The AV node generates 40 impulses per minute, the His bundle - no more than 25 impulses per minute.
Patients complain of shortness of breath, dizziness, general weakness, episodes of loss of consciousness with convulsions (Morgagni-Adams-Stokes attacks). During an attack, involuntary urination and defecation may occur, breathing becomes shallow, the skin turns pale and acquires a bluish tint (cyanotic), the pulse is practically not detectable by palpation. After a few minutes, the patient’s consciousness is completely restored, most often they do not remember what happened.
Diagnostic methods
Management of persons with abnormalities in the conduction of cardiac structures is under the supervision of a cardiologist. If the process is complicated and dangerous, consult a specialized surgeon.
An approximate survey scheme includes the following elements:
- Questioning the patient about complaints, their age and duration. Objectification of symptoms and fixation.
- Anamnesis collection. Including family history, determination of lifestyle, presence of bad habits and others. Aimed at early identification of the source of the problem.
- Blood pressure measurement. Against the background of an advanced process, by the second stage, or even more so the third, jumps in blood pressure are likely. It is difficult to catch such a condition using routine techniques.
- 24-hour Holter monitoring. More informative way. Blood pressure and heart rate are assessed every half hour or more often, depending on the program. Can be performed repeatedly to improve accuracy.
- Electrocardiography. Allows you to identify functional disorders of the heart. Plays a key role in early diagnosis.
- EFI. Modified version of the previous survey. However, it is invasive. A special probe is inserted through the femoral artery. The activity of individual areas of cardiac structures is assessed. Quite a difficult study, but sometimes there are no alternatives to it.
- Echocardiography. In order to identify organic disorders. The classic variant resulting from a long course of blockade is cardiomyopathy of varying severity.
- Blood analysis. For hormones, general and biochemical. For a comprehensive assessment of the state of the body, in particular the endocrine system and metabolism in general.
As necessary, if previous methods do not provide answers to questions, CT, MRI, coronography, and radioisotope studies are used. The decision is made by a group of leading specialists.
Treatment options
Therapy can be carried out in the following ways:
- First degree atrioventricular block has no specific treatment; symptomatic treatment procedures are prescribed to normalize the patient’s condition.
- The blockade caused by intoxication of the body is eliminated with the help of neutralizing therapy.
- The occurrence of pathology against the background of myocardial diseases requires the prescription of adrenergic stimulants to resume the conduction of cardiac impulses.
- To eliminate the pathology, a procedure for implanting cardiac stimulators can be used. The technique is a radical solution to the problem and is indicated for diagnosing 3rd degree AV block.
- When edema develops, diuretics, vasodilators and cardiac glycosides are prescribed.
If symptoms of AV block are detected, you should consult a specialist to determine the exact cause and treatment of intra-atrial conduction disturbance. To relieve an attack, it is recommended to administer Atropine to the patient and give an Isoprenaline tablet. After stopping the dangerous condition, the patient should be urgently taken to the hospital.
Pathology of the 1st degree does not require special therapy, as a rule.
Variants of deviations on the ECG
Among the characteristic features:
- Prolongation of the QT interval by more than 0.2 s. At the first stage this is a typical finding.
- PQ extension. Changes in the frequency of occurrence of ventricular complexes. The so-called Mobitz 1.
- Complete loss of contractions of the lower chambers of the heart. Or alternately, in a symmetrical order.
- Decreased heart rate (bradycardia) of varying severity. Depends on the stage of the pathological process.
AV block is noted specifically on the ECG, and the more severe the phase, the easier it is to diagnose the problem.
Treatment
AV block is not a disease, but only one of the manifestations of any cardiac pathology. Therefore, therapy begins with treatment of the underlying disease (myocardial infarction, etc.).
First degree AV block and asymptomatic second degree block do not require treatment. You just need to stop using medications that impair AV conduction.
If atrioventricular block on the ECG is accompanied by signs of oxygen starvation of the brain, medical attention is needed.
A remedy for quickly accelerating heart rate is atropine, but it is not always effective. In these cases, temporary cardiac pacing is used.
Treatment of third degree atrioventricular block consists of installing a permanent pacemaker. Depending on the type of blockade, atrial-dependent ventricular pacing or on-demand ventricular pacing may be used.
In the first case, the device is adjusted in such a way that contraction of the atria is artificially carried out to the ventricles. In the second, the stimulator impulse is applied directly to the ventricular myocardium, causing them to contract rhythmically at the desired frequency.
Treatment depending on the degree
The therapy is complex.
1st degree.
Long-term follow-up is indicated. Such tactics can be repeated for more than one year. If there is no progression, gradually the frequency of consultations with a cardiologist becomes less frequent.
Against the background of deterioration, medications from several pharmaceutical groups are prescribed:
- Antihypertensive drugs. Different types.
- Antiarrhythmic.
If there is an inflammatory infectious pathology, antibiotics, NSAIDs and corticosteroids are used. Treatment is strictly in a hospital.
Transient 1st degree AV block (transient) is the only dangerous case requiring therapy, provided it is of viral or bacterial origin.
2nd degree
The same type of drugs are used. If the condition quickly worsens, there is no point in waiting. The installation of a pacemaker is shown.
Regardless of age. The only exception is older patients who may not be able to withstand surgery. The issue is resolved individually.
3-4 degrees
Implantation of an artificial pacemaker is mandatory. Once the terminal phase occurs, the chances of cure are minimal.
Throughout the entire period of therapy, lifestyle changes are indicated:
- Quitting bad habits.
- Diet (treatment table No. 3 and No. 10).
- Adequate sleep (8 hours).
- Walks, exercise therapy. The main thing is not to overwork. The duration is arbitrary.
- Avoiding stress.
Traditional recipes can be dangerous, so they are not used.
Forecast
Atrioventricular blocks can be relatively favorable and unfavorable. This division is made taking into account the progression or stability of the blockade. Relatively favorable blockades include:
- 1st degree atrioventricular block, as a complication of myocardial infarction, as well as complete AV block with lower infarction. Often such cardiac conduction disturbances resolve during treatment of the underlying disease.
- Functional blockades.
Unfavorable blockades include acute development of 2nd degree blockade of types 1 and 2, complete atrioventricular block.
Prognosis and possible complications
Typical consequences:
- Heart failure. Resuscitation in such a situation is minimally effective; as soon as it is restored, the rhythm will change again. A relapse is likely within a few days.
- Cardiogenic shock. Potentially fatal consequence. Moreover, death occurs in almost 100% of cases.
- Fainting and, as a result, injury may be incompatible with life.
- Heart attack or stroke. Acute malnutrition of cardiac structures and brain, respectively.
- Vascular dementia.
Forecasts depend on the stage of the pathological process:
| Stage 1. | Survival rate is close to 100%. There are risks only if there are infectious lesions. |
| Stage 2. | The probability of death is about 20-30% without therapy. With full treatment it is 2-4 times lower. |
| 3rd degree. | Mortality 40-60%. |
In the terminal phase, death is inevitable. Therapy is ineffective.
Radical surgery with the installation of a pacemaker significantly improves the prognosis.
Diagnostics
Heart disease can be diagnosed by visiting a doctor. At the first symptoms and suspicions, do not delay visiting a specialist. You should contact a cardiologist or arrhythmologist, who will prescribe procedures to check your heart rhythm and conduction. The doctor will ask about symptoms, check your medical history, and perform a physical examination of your child. After the doctor’s conclusion, the following types of examinations may be prescribed:
- ECG is the process of recording the activity of the heart, which records the work of the heart muscle; carried out using electric current;
- ECG with atropine tests - an ECG is recorded after the substance atropine is injected into a vein (it changes the heart rhythm);
- Echocardiography is a process in which the shape and size of the heart is analyzed using ultrasound waves, and an idea of its conductivity is formed;
- Holter monitoring is a method of continuous recording of an ECG in everyday life, which will allow one to analyze changes in cardiac conduction on the cardiogram at different times of the day. The method will allow you to create a diary of heart rhythm observations and most accurately characterize the disease.
Clinical manifestations of different degrees
AV block can be transient (quickly passing) or permanent. Transient blockades are quite difficult to diagnose. To detect them, Holter monitoring is required - recording a cardiogram throughout the day.
With first degree atrioventricular block there are no obvious clinical manifestations. The only symptom is bradycardia. Some patients may feel weak and fatigued.
A more pronounced clinical picture is observed in the second degree:
- palpation can detect periodic loss of the pulse wave;
- clinically, this will manifest itself as the patient’s feeling of interruptions in the functioning of the heart;
- patients also feel weak and tired.
The most dangerous is the third degree of blockade:
- periodic or constant dizziness;
- ringing in the ears, flickering of spots before the eyes;
- pain behind the sternum;
- a feeling of interruptions in the work of the heart;
- episodes of loss of consciousness.
When listening to the heart with a stethoscope, you can hear the correct rhythm, but with the appearance of long pauses, this is a loss of ventricular contraction. Bradycardia of varying severity is noted. A cannon heart sound, characteristic of blockades, appears, called Strazhesko's sound.
A complication of blockades can be ventricular tachycardia leading to asystole. With MAS syndrome, observed in conjunction with this blockade, attacks of ventricular asystole may also occur, threatening rhythm disruption and cessation of cardiac activity.
Atrioventricular blocks - systematization, diagnosis, emergency therapy
Atrioventricular block (AV block) is a manifestation of pathology at a certain level of the AV conduction system. The rationality of therapy and the prognosis of AV block depend on diagnostic verification of the level of AV conduction (distal lesions are prognostically less favorable).
I degree . Slowing of impulse conduction from the atria to the ventricles: prolongation of the PQ interval > 200 ms (0.2), the QRS complex is usually narrow, the ratio of P to QRS is 1:1.
II degree.
- Mobitz-1 type : progressive prolongation of the PQ interval followed by “loss” of the QRS complex (Samoilov-Wenckebach period), QRS complexes, P to QRS ratio > 1.
- Mobitz-2 type : “loss” of the QRS complex with a stable PQ interval, often narrow QRS complexes, P to QRS ratio > 1, maybe 2:1, 3:1, etc.
With AV blockade of the first degree and second degree of the first type, emergency measures are usually not required. For AV blockade of the second degree of the second type and complete AV blockade, the following measures are necessary:
- elimination and treatment of possible causes (myocardial infarction (MI), drug overdose, electrolyte disorders);
- intravenous administration of a 0.1 percent solution of atropine 1 ml per 10 ml of physiological solution, which can eliminate disturbances in AV conduction caused by hypertonicity of the vagus nerve, but does not affect conduction at the level of the His-Purkinje system; AV blockade with wide QRS complexes. The effect of atropine lasts about three hours;
- Temporary endocardial stimulation is indicated for patients with second-degree AV block of the second type and complete AV block at the level of the His-Purkinje system or accompanied by hemodynamic disturbances or syncope.
III degree . Complete AV block (atrial stimuli are not conducted to the ventricles), P and QRS waves are regular, there is a complete dissociation of excitation of the atria and ventricles. Not a single P wave is associated with the QRS complex; the P frequency is greater than the QRS frequency.
First degree AV block usually does not cause clinical symptoms. Second- and third-degree AV blocks are relatively rarely without clinical manifestations. They cause general weakness, shortness of breath, pre-fainting and fainting states.
Possible causes of AV block:
- increased tone n. vagus (these forms are characterized by a favorable prognosis, often asymptomatic, and registration of narrow QRS complexes on the ECG);
- primary diseases of the conduction system;
- myocardial lesions (MI, fibrosis, autoimmune inflammation, infiltration, storage diseases, etc.) with damage to the His-Purkinje system (frequent widening and deformation of QRS complexes, poor prognosis);
- congenital blockades;
- medicinal effects (combination of drugs that inhibit AV conduction, beta-blockers, AK, cardiac glycosides, etc.).
If there is a rhythm with narrow QRS complexes on the ECG, narrow QRS complexes are observed in proximal AV blockades, which have a favorable prognosis.
It is necessary to discontinue medications that worsen AV conduction (antiarrhythmics, NSAIDs, steroid hormones, cardiac glycosides, etc.).
With blockades at the level of the AV junction, the prognosis is relatively favorable (narrow QRS complexes, escape rhythm frequency more than 4 per minute).
The more distal the blockade, the worse the prognosis. Persistent type 2 second-degree AV block and complete distal AV block increase mortality and usually require permanent IVR implantation, regardless of the presence or absence of symptoms.
A PQ interval > 0.28 s is indicative of AV block at the level of the AV node, a PQ interval < 0.28 s is characteristic of AV block at the level of the inferior nodal AV conduction system. A QRS value > 0.12 s is characteristic of AV block at the level of the bundle branch system, < 0.12 s is indicative of localization of the block at the level of the AV node and the His bundle.
Tests with intravenous administration of atropine and physical exercise improve AV conduction when the block is localized at the level of the AV node and worsen when the block is localized at the level of the inferior nodal AV conduction system. Vagal tests worsen AV conduction when the pathology is localized at the level of the inferior nodal AV conduction system.
AV block of the second degree of the first type with Samoilov-Wenckebach periodicity . The cause is an increase in the tone of the vagus nerve, cardiosclerotic lesions of the conduction system of the heart and the toxic effects of drugs. In case of acutely developed second degree AV block of the first type, it is necessary to exclude ACS with occlusion of the right coronary artery, the acute stage of lower MI.
Second degree AV block of the second type is a distal, prognostically unfavorable conduction disorder. This blockade is usually localized in the area of the bundle branches, less often at the level of the trunk. QRS complexes are often wide, incomplete blockade of the right bundle branch. When conduction pathology is localized at the level of the His bundle, the QRS complexes are narrow (QRS <0.12 s), damage at the level of the His bundle branches leads to a widening of the QRS complex (> 0.12 s). The reasons for the development of second degree AV block type II are most often cardiosclerotic damage, occlusion of the left descending artery in the acute stage of MI.
Complete AV block (III degree AV block). The complete absence of impulse conduction from the atria to the ventricles compensates for this condition by slipping replacement rhythms.
- Wide QRS complexes are a sign of ventricular escape rhythm.
- The AV node is characterized by a frequency of 40-50 pulses per minute.
Lower IM. Complete AV block is usually transient; reperfusion therapy (thrombolytic administration, PCI) is necessary, which leads to conduction restoration. If conduction disturbances persist for more than seven days, the issue of implanting a permanent pacemaker should be considered.
Anterior MI is an unfavorable prognostic sign when complete AV block occurs as a result of damage to the conduction system. Temporary endocardial stimulation is indicated.
Urgent Care
Elimination and treatment of possible causes (MI, drug overdose, electrolyte disorders).
Administration of a 0.1 percent solution of atropine 1 ml per 10 ml of saline solution intravenously. Usually, disturbances in AV conduction caused by hypertonicity of the vagus nerve can be eliminated, but do not affect conduction at the level of the His-Purkinje system. The effect of atropine lasts about three hours.
Patients with Frederick's syndrome - a combination of AV block with atrial fibrillation - atrial flutter (block at the level of the AV junction with narrow or wide QRS complexes), accompanied by hemodynamic disturbances or syncope, are shown temporary endocardial stimulation.
Treatment of atrioventricular blockades
I degree AV block usually does not require special treatment until the possible causes are clarified; dynamic observation with repeated ECG and CM registration is necessary to exclude higher degree AV blocks and possible cardiovascular diseases (rheumatism, myocarditis, etc.). with a functional nature - correction of the vegetative status: anticholinergics (atropine, platyphylline), corinfar (10 mg 3-4 times a day), belloid (one tablet 3-4 times a day), teopek (1/4 tablet 2-3 times a day) day), isadrin (0.005 - under the tongue).
AV block of the second degree type Mobitz-1 . Observation, re-registration of ECG and HM, correction of vegetative status: atropine, platyphylline, clonazepam.
In the acute occurrence of AV block with clinical manifestations and frequent loss of QRS complexes:
- 0.5 ml of 0.1% solution of atropine sulfate intravenously slowly; then 0.5-1.0 mg at intervals of 3 minutes up to a total dose of 2 mg (under monitor control) or 0.5-1.0 ml of a 0.1 percent solution of atropine sulfate subcutaneously 4-6 times a day;
- if ineffective - be careful! - infusion of isoprenaline (Isadrina) at a rate of 0.5-5.0 mcg/min. under the control of a monitor (do not administer in case of acute MI!);
- if ineffective in acute anterior MI, temporary pacemaker is used.
2nd degree AV block type Mobitz-2, progressive AV block and 3rd degree AV block . In case of AV block with wide QRS complexes (> 0.12 s) of the main or replacement rhythms - temporary endocardial pacemaker, treatment of the underlying disease. The effect is possible when taking sympathomimetics (izadrin), Corinfar, Belloid.
For AV block with clinical manifestations, but with narrow QRS complexes (<0.12 s), heart rate 40-60 beats per minute or pauses less than 3 s, the following are indicated:
- 0.5 ml of 0.1% solution of atropine sulfate intravenously slowly; then 0.5-1 mg at 3-minute intervals to a total dose of 2 mg (under monitor control);
- if ineffective - be careful! - infusion of isoprenaline (Isadrina) at a rate of 0.5-5.0 mcg/min. under the control of a monitor (do not administer in case of acute MI!);
- if ineffective - temporary endocardial pacemaker.
In case of acute onset of AV block with periods of asystole > 3 s, Morgagni-Adams-Stokes attack and (or) heart rate < 40 beats per minute:
- indirect cardiac masses and temporary endocardial pacemaker;
- 0.5 ml of 0.1% solution of atropine sulfate intravenously and 0.5-1. ml of 0.1% solution of adrenaline intravenously or intracardially;
- if ineffective, implantation of a permanent pacemaker.
Indications for permanent pacemaker implantation:
- Morgagni-Adams-Stokes attacks (even one in history);
- Third degree AV block with heart rate < 40 beats per minute or pauses > 3 s;
- Second degree AV block of Mobitz type 2 without clinical manifestations;
- AV block of the second degree or third degree, two-bundle block, alternating with complete AV block with clinical manifestations caused by bradycardia (dizziness, angina or ACS, progressive CHF, systolic hypertension);
- AV blockade of the 2nd or 3rd degree with rhythm disturbances requiring the prescription of antiarrhythmics, which is impossible if AV conduction disturbances persist;
- 2nd degree or 3rd degree AV block with wide QRS complexes (> 0.12 s);
- First degree AV block with an increase in the PQ(R) interval > 0.3 s.
Contraindications to permanent pacemaker implantation:
- AV block of the first degree and second degree of the Mobitz-1 type without clinical manifestations;
- drug AV blockades, in which there is a high possibility of persistent regression of AV conduction disorders.
M.A. Gurevich
2018
Prognosis and prevention
First of all, prevention should be combined with emergency treatment of heart diseases, even if the blockade is partial and there is no direct threat to life. It is preferable to use medications than to use folk remedies.
The second mandatory point is monitoring the work of the heart and assessing the slightest changes for the worse. It is necessary to do an ECG regularly to prevent consequences. Use medications as recommended by doctors. If strong physical activity is prohibited, then under no circumstances should the child be allowed to overload.
If you have other diseases, you cannot stop visiting a cardiologist for preventive examinations and determining the current degree of the disease. Healthy children should be prescribed annual examinations for early diagnosis (using an ECG).
It is worth monitoring your diet: limit the consumption of strong tea, stop eating fried and too fatty foods, eat more vegetables and fruits. In terms of physical exercise, it is necessary to avoid overload, but at the same time continue to perform exercises according to a light program. Emotionally, a low-stress environment means a lot.
Symptoms and treatment
Symptoms of the pathology develop against the background of a rare heartbeat and circulatory disorders. Due to insufficient blood flow to the brain, dizziness occurs and the patient may lose consciousness for a while. The patient feels rare powerful tremors in the chest, and the pulse slows down.
When assessing the patient’s condition, the specialist finds out whether he has had previous heart attacks, cardiovascular diseases, and a list of medications taken. The main research method is electrocardiography, which allows you to capture and graphically reproduce the work of the cardiac system. Daily Holter monitoring allows you to assess the patient’s condition at rest and during light physical activity.
Additional studies are carried out using echocardiography, multispiral computed cardiography and magnetic resonance imaging.
If AV block (grade 2) occurs for the first time, the patient is prescribed a course of drug therapy. All medications that slow down impulse conduction are discontinued. Drugs are prescribed that increase the heart rate and block the influence of the nervous system on the sinus node. These drugs include: Atropine, Isadrine, Glucagon and Prednisolone. In cases of chronic disease, Belloid and Corinfar are additionally prescribed. Teopek is recommended for pregnant women and people suffering from epilepsy. The dosage is prescribed by the doctor depending on the patient’s condition.
Long-term heart failure contributes to the accumulation of fluid in the body. To eliminate congestion, take the diuretics Furosemide and Hydrochlorothiazide.
A severe form of the disease with 2nd degree AV block of the Mobitz type 2 requires radical treatment. For this purpose, an operation is performed to install a pacemaker - a device that controls the rhythm and frequency of the heart. Indications for surgery:
- clinical picture of the patient’s condition with frequent fainting;
- AV block (degree 2) Mobitz type 2;
- Morgagni-Adams-Stokes attack;
- heart rate less than 40 beats per minute;
- heart failures with a frequency of more than 3 seconds.
Modern medicine uses the latest devices that work on demand: electrodes release pulses only when the heart rate begins to fall. The operation causes minimal damage and is performed under local anesthesia. After installing the stimulator, patients' pulse normalizes, pain disappears and their well-being improves. Patients must follow all doctor's instructions and visit a cardiologist. The operating life of the device is 7-10 years.
Causes
Development factors are always cardiac.
On the one hand, this makes diagnosis easier. On the other hand, it initially worsens the prognosis. Poisoning with phosphorus compounds. Usually these are mineral fertilizers. Patients working in hazardous chemical plants are especially at risk. Once the dangerous factor is eliminated, the likelihood of restoring normal health is almost maximum.
Patients with acute intoxication should be immediately hospitalized for specific treatment measures. The prognosis in this case is relatively favorable.
Congenital and acquired heart defects. What kind doesn't play a big role. This may be stenosis, prolapse of the mitral, aortic valves, disturbances in the anatomical development of the septum and other conditions.
The problem is that it is extremely difficult to detect them if you do not contact a cardiologist every six months or a year for a routine examination.
Findings are mostly accidental, because pathological processes are detected already at irreversible stages. Some cases are even dealt with after the fact, when the person has died.
Sinoatrial blockade of this type is relieved as part of the main surgical treatment.
Drug overdose. It’s ironic, but drugs designed to lower blood pressure and eliminate arrhythmia, that is, medications aimed at improving the heart, can kill the patient in a matter of hours.
Amiodarone, Quinidine, Digoxin, glycosides in general, and beta blockers are especially dangerous. Third-party drugs include psychotropic drugs, including antipsychotics, antidepressants, and tranquilizers.
It is possible to provoke a similar effect due to the use of oral contraceptives. All drugs should be prescribed only by a specialist after a thorough diagnosis.
Myocarditis. Inflammation of the heart muscle. It is an infectious, less often autoimmune disease. Requires urgent medical care in a hospital.
Such a dangerous condition cannot be treated on an outpatient basis, since complications are possible, including a heart attack or cardiac arrest. Antibiotics are used in loading doses or immunosuppressants.
As a rule, the condition is secondary. Develops as a complication of colds, rheumatism and others. Sinoatrial blockade after severe myocarditis does not go away on its own.
Vegetovascular dystonia. Strictly speaking, it does not apply to cardiac problems. However, the normal innervation of the cardiovascular system is disrupted. Hence the deviations in the conductivity of the electrical impulse.
It is a complex symptomatic complex. It manifests itself in many ways: from tachycardia, to dizziness, fainting, shortness of breath and others.
It is not considered an independent diagnosis; you need to look for the cause of this condition. Usually we are talking about hormonal imbalance or pathologies of the cerebral structures themselves.
- Rheumatism. Autoimmune damage to cardiomyocyte cells. The body's protective forces, designed to cover the body, destroy its own tissues. The reasons for this deviation are not fully known. However, rheumatism quite quickly destructs cardiac cells, causing severe scarring and severe heart failure with sinoatrial block.
Heart attack and, as a consequence, scarring of the affected areas (cardiosclerosis). It ends with a significant decrease in the conductivity of the natural pathways of electrical impulses. Treatment is required urgently. There is always a risk of death.
In completely healthy people, sinoatrial blockade is also possible. Spontaneous, transient, and transient SA blockades are a consequence of increased activity of the vagus nerve.
Such conditions can be dangerous, but they last only a few minutes, half an hour at most. Patients with no cardiac history and no organic abnormalities in the objective picture are observed by neurologists.
Attention:
There is a chance that the first attack will be the only one, but it is not great. Most likely, we are talking about a disruption of the brain or endocrine system.
In the absence of data for pathologies and functional disorders, they generally speak of an idiopathic form of sinoatrial block. This is a relatively rare option. Typically, diagnostic problems do not arise due to the obviousness of the underlying process.