Hydropericardium: what is it, causes, symptoms, treatment
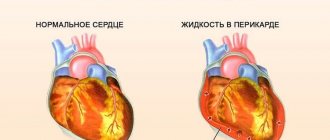
Hydropericardium is a pathology characterized by excessive accumulation of fluid in the atrial membrane. Another name for the disease is dropsy of the heart. This condition requires immediate medical examination and mandatory therapy. According to the international classification of various pathologies, the hydropericardium is assigned the following ICD-10 code: I30.
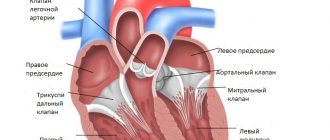
The structure of the pericardium resembles a sac, which looks like a truncated cone. Its smaller part is located on the diaphragm, and its wider apex abuts the ascending aorta. The described organ consists of two layers: visceral and pariental.
The latter is called the pericardium. Under normal healthy conditions, there is a special liquid between the two leaves - a natural lubricant. It fills the area between the epicardium and pericardium. Its task is to prevent friction during contraction of the heart muscle.
A healthy pericardium may contain 15-50 ml of fluid. This is quite enough to ensure proper functioning of the heart. With hydropericardium, its amount increases several times. A condition is considered dangerous when 200-1000 ml of liquid accumulates inside the cavity. Against this background, arterial permeability increases and nutrient absorption processes are disrupted.
Hydropericardium is classified according to several criteria. Depending on the amount of fluid localized between the sheets of the cardiac membrane, there are:
- Minor swelling. The volume of transudate is in the range of 50-100 ml.
- Small hydropericardium. The accumulated pathological fluid reaches half a liter in volume,
- Big. The amount of liquid is 500-1000 ml.
As pathological accumulations increase in the cavity, the petals of the cardiac sac diverge, and the distance between them increases. Normally, this indicator is 0.5 cm. Developing deviations are divided into three different stages:
- initial (0.6-1 cm),
- slight deviation (1-2 cm),
- pronounced pathology (2-3 cm).
Hydropericardium is also divided into 2 types depending on the nature of the accumulated fluid. Hemopericardium is diagnosed when blood accumulates between the petals, and chylopericardium is diagnosed when lymph accumulates inside the cavity.
Diagnostic measures
Laboratory Tests Dogs with hemangiosarcomonas have anemia, nucleated red blood cells, schizocytes or acanthocytes, or thrombocytonenia.
Cats with FIP may have neutrophilia and lymphocytopsnia. The serum biochemical profile is usually normal, but there may be a mild increase in liver enzymes due to chronic inactive congestion. Mild azotemia, usually pre-nasal, may also be noted.
Dogs with chronic pericardial effusions and ascites have hyponroteinemia, hyponatremia, gynochloremia, or hyperkalemia. Hynerglobulinemia is often seen in cats with FIP. Urinalysis is usually normal. In endemic areas, serology for coccidioidomycosis should be performed.
If coagulopathy is clinically suspected, several coagulation tests (eg, activated clotting time, activated partial trombonlastine time, and one-stage thrombone time) should be performed before nonricardiocentesis.
Causes of pathology
Cardiac edema can be caused by many different diseases and conditions. When diagnosing hydropericardium, the following causes of pathology are indicated:
- allergic phenomena,
- surgical interventions in the heart area,
- cardiac failure (CHF),
- chest injuries,
- anorexia,
- anemia,
- abnormalities in kidney function,
- ascites (edema of the peritoneum),
- various inflammatory processes,
- abnormalities in the structure of the pericardium,
- the presence of a diverticulum (protrusion) in the left ventricle,
- general exhaustion
- tumors in the mediastinum,
- hydrothorax (fluid accumulation in the pleural cavity of the lungs),
- myxedema,
- congestion in the cardiovascular system.
Hydropericarditis can also develop as a result of exposure to provoking factors. These include:
- elderly age,
- therapy with vasodilators,
- pregnancy (all trimesters),
- radiotherapy.
During pregnancy and in elderly patients, the disease can have an isolated form, that is, it can proceed independently.
Symptoms of ascites in a dog
Ascites is a very difficult period in the life of any animal. The condition occurs with severe symptoms and external signs. The following symptomatic picture is typical for abdominal dropsy in a dog:
- Severe bloating and protruding sides. In large dogs, this is difficult to notice in the initial stage, but ascites in a dachshund, for example, should be noticeable literally in the first day.
- Dyspnea. If dropsy develops slowly, then at first the dog will suffocate when running, and then it gets worse. Shortness of breath torments the dog even when it is just lying down.
- Due to breathing problems, your pet spends a lot of time sitting; this position allows him to breathe more easily.
- Change in color of mucous membranes. They usually turn blue, but if ascites is caused by liver problems, the color will be yellow.
- Swelling. May be a sign of ascites if the dog has other symptoms.
- Dropsy due to kidney failure may be characterized by high water consumption and frequent trips to the toilet.
- Slow, often painful movement. This condition causes the dog to reduce activity, and over time, general exhaustion is characterized by lethargy, drowsiness, and apathy.
- Decreased appetite.
Despite the lack of appetite, the animal's body weight continues to grow. This is associated with the progression of dropsy. Sometimes, due to ascites, the body is poisoned and the dog begins to vomit. The presence of such symptoms is a signal for an urgent visit to the veterinarian.
Features of the course of the disease in newborns and fetuses
Hydropericardium is diagnosed not only in elderly patients, but also in newborn babies. In premature babies, pathological fluid accumulates inside the cavity due to catheterization of the central veins.
Drugs injected into the umbilical artery often end up directly in the atrial lining. If the catheter is in place for more than 4-5 days, there is a risk of developing a hydropericardial complication such as cardiac tamponade.
The situation is especially dangerous when hydropericardium develops in the fetus. It occurs in rare cases against the background of intrauterine pathologies of the left ventricle.
Its wall protrudes in the area of the crown of the heart muscle, and transudate accumulates in the atrial membrane.
The listed pathological processes cause cardiac dysfunction and can lead to intrauterine fetal death.
To avoid the development of congenital heart defects in a child, a woman during pregnancy should be regularly observed by a doctor and undergo all prescribed ultrasounds and cardiotocography.
Sometimes situations were recorded when an excessive amount of pathological fluid in the pericardial membrane resolved on its own. However, in most cases, pericardiocentesis is required.
But this procedure is not considered safe, since there is a high risk of injury to the organs of the mother and the unborn child.
Source: https://cordiacardio.ru/diagnostika/umerennyj-gidroperikard.html
Classification
Various types of fluid can accumulate in the pericardial sac. This may be lymph, then the pathology is called chylopericardium. When blood accumulates, pilocarditis is diagnosed.
In addition to the nature of the liquid contents accumulated in the pericardium, its quantity also varies. Based on this feature, the following forms of hydropericardium are distinguished:
- small – up to 100 ml of transudate;
- moderate – 100-500 ml of liquid;
- large - over 500 ml of liquid content.
The degree of divergence of its leaves depends on the amount of fluid accumulated in the pericardium. If it does not exceed 5 ml, then this condition is considered normal. If this indicator is exceeded, hydropericardium is diagnosed as one of the following forms:
- initial – discrepancy within 6-10 mm;
- moderate – 10-20 mm;
- pronounced - over 20 mm.
Pericarditis in dogs: symptoms and treatment | how to treat
Pericarditis is an inflammatory disease of the lining of the heart. This sac-like protective membrane (pericardium) consists of two layers: the outer (fibrous) and the two-lobed inner (serous).
The narrow gap between the petals of the serous pericardium is filled with a transparent protein liquid. Inflammation of the cardiac membrane in most cases is a secondary disease. According to statistics, pericarditis is more common in dogs over 5 years of age, mainly in males.
Retrievers, Labradors, Great Danes, and German Shepherds are predisposed to this pathology.
Reasons for development
Pericarditis develops as a result of increased secretion of lubricating fluid by the cardiac membrane, which is a compensatory reaction of the pericardium to problems that have arisen.
The reasons may be:
- suffered a serious illness;
- sluggish chronic disease (tuberculosis, rheumatism, hepatitis);
- viral, bacterial, fungal, protozoal infections;
- direct or closed injuries of the pericardium (impact to the chest, fall from a great height);
- poor diet;
- frequent hypothermia;
- increased physical activity;
- oncology.
Types of pericarditis
Pericarditis in dogs can occur in acute or chronic form. There are several types of this disease.
Fibrinous
It develops when blood fibrin leaks from the serous membrane into the pericardial cavity. This form of pericarditis is called “dry” because it leads to impaired lubrication of the pericardium, which becomes rough, and deposits of calcium salts form between the layers of the serous membrane.
Exudative
The mechanism of development of this form is the opposite of the previous one: fluid accumulates in the heart sac in too large quantities. The origin of such an effusion may be associated with an inflammatory process or be caused by other reasons: heart failure, trauma, tumors. In the first case, the fibrous fluid is called exudate, in the second - transudate.
Stenotic
With this type of disease, scars and adhesions form on the lining of the heart, connecting it to neighboring tissues. This “adhesive” form of pericarditis usually develops as a result of the chronic course of exudative or fibrinous forms.
Fibrinous pericarditis is easier to treat, and complete recovery occurs in most cases. Exudative and stenotic pericarditis in dogs is much more severe, takes longer to treat, and more often leads to disability.
Symptoms
Clinical manifestations of inflammation of the cardiac sac depend on its type. Symptoms common to pericarditis of any origin include:
- increased heart rate;
- a sharp increase in temperature;
- pallor or cyanosis of the mucous membranes.
The dog becomes apathetic, lethargic, loses appetite, and sometimes has bloating.
Later, in later stages of the disease, other symptoms appear:
- swelling of the extremities develops;
- periodically causeless vomiting occurs;
- the dog refuses to eat, suddenly loses weight (this condition is called anorexia);
- due to exhaustion, the animal may lose consciousness.
Diagnosis of pericarditis
To diagnose a dog with pericarditis, determine the type of disease and the cause that caused its development, the following is carried out:
- Detailed blood test. Allows you to determine the level of hemoglobin, red blood cells, leukocytes, platelets and detect the presence of inflammation.
- Ultrasound. Using this method, you can detect the presence of fluid in the pericardial cavity.
- Chest X-ray. Indicated to determine the location and volume of effusion.
- Analysis of pericardial fluid. It is carried out to identify the cellular structure of the effusion. It can be serous (consisting of a protein fraction), hemorrhagic (admixed with blood), purulent or chylous (containing lymph).
- Electrocardiography, echocardiography. Using these diagnostic methods, you can get a clear picture of the distribution of fluid in the heart sac.
Treatment
Treatment for pericarditis depends on its type and degree of development. To reduce the formation of exudate, the animal is prescribed cold to the heart area.
For the same purpose, as well as to relieve edema, diuretics (diuretics) are prescribed: Mercuzal, Furosemide, Purina derivatives Eufillin or Temisal, herbal medicine Hexamethylenetetramine.
If the amount of fluid in the pericardium is large, it is removed using a special long needle. The procedure for draining exudate is carried out under general anesthesia and echocardiography control.
Mandatory points in the complex treatment of inflammation of the lining of the heart are antibiotic therapy, anti-inflammatory and cardiac medications. Among antibiotics, dogs are usually prescribed drugs from the penicillin group, aminoglycosides or cephalosporins.
Anti-inflammatory drugs (Prednisolone, Ibuprofen, Acetylsalicylic acid, Nefedipine, Reopirin, Indomethacin) are prescribed in a weekly course, gradually reducing the dose.
To relieve heart failure, potassium preparations (Asparkam, Potassium-magnesium asparaginate, Panangin), Pimobendan, Cardioprotector Divopride are used.
Additional activities during the treatment period:
- The amount of water consumed by the animal should be reduced (to avoid edema).
- Your pet's diet should include foods with high energy value, as well as vitamin and mineral supplements.
- The dog's physical activity is limited to a minimum.
- The animal is provided with complete rest.
With timely treatment of acute pericarditis, the dog’s chance of complete recovery is quite high. The chronic form of the disease takes longer and is more difficult to treat, and recurrent pericarditis may require surgical intervention - pericardiotomy (removal of part of the pericardium or the entire membrane).
Source: https://usatiki.ru/perikardit-u-sobak-simptomy-i-lechenie/
Clinical manifestations
As soon as excess fluid begins to accumulate in the pericardial sac, compression of the heart occurs and the person begins to show signs of illness:
- shortness of breath, feeling of lack of air;
- cardiopalmus;
- discomfort in the chest area;
- swelling of the face;
- increased sweating;
- dilated veins in the neck;
- swelling of the upper and lower extremities.
As the disease progresses, the following symptoms are observed:
- severe chest pain;
- tachycardia;
- decrease or increase in blood pressure;
- blue discoloration of the skin;
- dizziness, loss of consciousness;
- severe weakness;
- fear of death.
Important! If the amount of transudate is insignificant, there are no clinical manifestations.
Diagnosis and treatment of pericardial effusions
Pericardial diseases can be congenital (peritoneopericardial diaphragmatic hernia) or acquired (pericardial effusions, constrictive pericarditis and pericardial tumors). The most common of these are pericardial effusions, which most often impair the functioning of the heart.
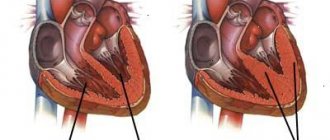
Pericardial effusions are an increase in the volume of fluid within the pericardial sac. The term cardiac tamponade describes the clinical situation in which pericardial effusions increase intracardiac pressure so much that hemodynamic equilibrium is disrupted.
At the Foster Veterinary Hospital at Tufts University School of Veterinary Medicine, pericardial effusions are diagnosed in 7% of cardiac cases (8% in dogs and 7% in cats).
It is possible that the overall incidence of pericardial effusions matches these figures, but symptomatic pericardial effusions are common in dogs and rare in cats.
Pathophysiology
As fluid accumulates in the pericardial sac, its ability to stretch is gradually exhausted.
Further accumulation of pericardial fluid creates high intracardiac pressure, which leads to collapse of the right atrium and/or ventricle and prevents the heart from filling (tamponade). Low cardiac preload results in decreased inflow and outflow.
With a further increase in intracardiac pressure, the filling of the left atrium and ventricle is disrupted by direct compression or due to displacement of the interventricular septum into the left ventricle.
Chronic pericardial effusion As a result of the compensatory mechanisms that are activated by any decrease in cardiac outflow, the neurohumoral system is activated, which creates fluid retention and, consequently, symptoms of congestive heart failure. High systemic venous pressure also contributes to heart failure. Its symptoms manifest as right-sided heart failure and include ascites, hepatomegaly, distension and pulsation of the jugular vein and in some cases lead to pericardial effusion.
Acute pericardial effusion With sudden bleeding into the pericardial sac (hemangiosarcoma of the right atrium with acute bleeding or rupture of the left atrium after chronic valve damage), intracardiac pressure sharply increases. In these situations, acute hemodynamic reactions dominate, and since the body takes time to accumulate sodium and water, fluid retention does not occur. Compression of the cardiac chambers
leads to a rapid drop in preload and a corresponding drop in cardiac output. The clinical picture is acute cardiovascular collapse due to a sharp fall in cardiac outflow with collapse, weakness, hypotension, pallor, and slowing of capillary refill rate. Fainting may occur.
Causes of pericardial effusion
90% of pericardial effusions are caused by neoplasia and idipathic causes, with neoplasia being the most common cause, especially in older dogs. The most common neoplasm associated with pericardial effusion is right atrial hemangiosarcoma.
There may be other tumors - mesothelioma, tumor of the aortic body (chemodectoma), ectopic thyroid carcinoma and metastases.
Other causes of pericardial effusions may include coagulopathies (vitamin K antagonist), infections (coccidioidomycosis, trypanosomiasis, bacterial pericarditis), congestive heart failure, hypoalbuminemia, uremia, pericardial cysts, left atrial rupture, and pericardial foreign bodies.
Some reports have reported that the most common cause of pericardial effusions in cats is feline infectious peritonitis (FIP).
Congestive heart failure is the second most common cause, especially in cats with pleural effusions and significant cardiac enlargement.
Other causes of pericardial effusions in cats include bacterial pericarditis, uremia, coagulopathies, lymphoma and metastases, left atrial rupture, and idiopathic pericarditis.
Clinical picture
Breed predisposition Pericardial effusion is most often diagnosed in large breed dogs over 5 years of age. In young dogs, the causes are more likely to be idiopathic. The cause of effusions in dogs over 7 years of age is most often neoplasms.
Golden retrievers, German shepherds, and Labrador retrievers are most predisposed to right atrial hemangiosarcoma. Golden Retriever and German Shepherd dogs, as well as male dogs of other breeds, are predisposed to idiopathic pericardial effusions.
Boxers, English bulldogs, and Boston terriers are predisposed to chemodectomas, but they represent a small percentage of dogs with pericardial effusions.
Clinical symptoms Chronic pericardial effusion Chronic pericardial effusion causes right-sided congestive heart failure.
Owners report lethargy, anorexia, weakness, collapse, bloating, tachypnea, restlessness at night and muscle wasting. Often, but in varying forms, ascites, muffled heart sounds, weak arterial pulse, paradoxical pulse, tachypnea, pleural fluid line are detected during general examination , tachycardia and dilatation of the jugular vein. Pulsus paradoxus causes an increased drop in blood pressure during inspiration. It is determined by palpation in the form of a strong pulse when inhaling and a very weak one when exhaling. Pallor of the mucous membranes and a slower rate of capillary refill may be noted. Fever is rare but may be present with septic pericarditis.
Acute pericardial effusion In acute pericardial effusion, all symptoms are associated with sudden collapse. There may be fainting. Before collapse, owners report a brief period of lethargy, anorexia, or weakness.
With the rapid development of collapse, most animals quickly weaken and cannot stand up. The arterial pulse is weak, and pulsus paradoxus may be present.
The mucous membranes are pale and the canillary filling rate is reduced. Tachycardia, tachypnea, and dilatation of the jugular vein are also present.
Percutaneous puncture of the pericardium
Surgery
Conclusion
Males with an average age of 5-12 years are more prone to pericarditis; The Labrador Retriever is a more susceptible breed. Echocardiography is the most sensitive means of diagnosing pericarditis, in particular, it allows differentiating various acquired heart diseases that cause cardiomegaly on the radiograph. Conservative therapy + pericardiocentesis are most effective in combating tamponade, but the main method of treatment, and sometimes the only way to make a final diagnosis, is pericardiotomy. In cats, pericarditis is usually associated with viral peritonitis or lymphoma, less often it is a consequence of heart failure, in which case the prognosis is poor, since the risk of developing pulmonary edema is extremely high.
Pericarditis in dogs: causes, symptoms and treatment
Pericarditis in dogs is a disease that is caused by inflammation of the pericardium (the outer lining of the heart).
This disease is a complication of other diseases (tuberculosis, bronchitis, pneumonia, hepatitis) and is secondary in nature.
Pericarditis makes up a small percentage of heart disease. Often dog owners do not pay attention to the clinical manifestations of the disease, as they are uncharacteristic or are mistaken for other cardiac disorders.
Causes
The main causes of pericardium in dogs are the following:
- Complications after an infectious disease.
- Overwork.
- Inadequate nutritional diet.
- Hypothermia.
- Pericardial injury.
- Oncology.
Predisposition to pericarditis
In large and medium-sized dog breeds, pericarditis is most often diagnosed. In addition, pericarditis occurs in older and middle-aged dogs (mainly in males over five years of age).
Breeds in which this disease is most often observed: Great Danes, Labradors, German Shepherds.
If the owner of the animal notices changes in the behavior or appearance of his pet, then you should not try to self-medicate, you should urgently consult a specialist. Only after a thorough examination can the disease be accurately diagnosed. In this case, the examination of the animal must be carried out carefully.
Quite often, a dog comes to see a veterinarian in serious condition, since symptoms can develop very quickly (often within 24 hours).
Diagnosis of the disease
Diagnosis of pericarditis includes the following measures:
- Clinical blood test.
- Ultrasound (helps detect fluid in the pericardial cavity).
- Chest X-ray (diagnoses changes in the contours of the heart and the boundaries of the pericardium).
- Electrocardiography (can reveal concomitant diseases, for example, tachycardia).
- Analysis of pericardial fluid (to make a final diagnosis).
It is very important to direct all efforts to eliminate and treat the disease that caused pericarditis. If treatment was started in a timely manner, then the animal’s chance of recovery is quite high.
Introduction
Etiology
An examination of an animal with suspected pericarditis should be carried out qualitatively, but with some caution. Often the patient comes to see a doctor in serious condition, with severe symptoms of right-sided heart failure due to cardiac tamponade; sometimes such symptoms can develop within 24 hours. In this case, weakness, shortness of breath are expressed, the cardiac impulse is reduced, the pulse is weak or not palpable at all, the jugular veins are dilated, the mucous membranes are pale, the SNK is more than 3-5 s. Abdominal enlargement due to ascites and wheezing due to developing pulmonary edema and chest effusion may also occur. Such patients should not be subjected to thorough diagnostics; it is enough to verify the presence of free fluid using ECHO and perform a percutaneous puncture of the pericardium. If the patient's condition is more stable, a thorough examination is necessary. X-ray examination reveals rounded contours of the heart. The method also allows you to determine metastasis of lung tissue.
The ECG diagnoses alteration of R waves, sometimes a decrease in voltage and depression of the ST segment (Fig. 5).
Treatment depends on the speed of development of the process and the cause of the disease and comes down mainly to three components:
– pericardial puncture and fluid removal; – antibiotic therapy and control of heart failure; – pericardiotomy.
Conservative treatment. If it is possible to identify the pathogen, treatment is selected individually; Routine antibiotics are recommended for all patients to prevent complications. Diuretics and ACE inhibitors are also indicated, but with caution so as not to provoke a decrease in blood pressure. It is important to monitor the functioning of the kidneys, since they are primarily affected by sudden changes in pressure. For severe anemia, iron and folic acid supplements are recommended, and in acute cases, blood transfusion. It is also possible to use drugs with antihypoxic and antioxidant properties. In cats, conservative treatment is more effective and almost always involves steroids. Surgical treatment is ineffective, since in severe cases, unlike in dogs, pulmonary edema often develops.
Diagnostic measures
To make an accurate diagnosis, instrumental and laboratory diagnostic methods are used. The patient is referred for the following studies:
- Echocardiography. Ultrasound examination is very informative if hydropericarditis is suspected. It allows you to see the degree of divergence of the heart leaves and determine the volume of fluid between them.
- Radiography. Necessary to assess the general condition of all chest organs. Carrying out this study is especially justified if chest injuries are suspected.
- Clinical and biochemical blood tests, urine analysis. They help assess the general condition of the patient’s body and identify inflammatory processes. Particular attention is paid to the level of hemoglobin, ESR, and red blood cells in the blood.
- Pericardial puncture. Prescribed when hydropericarditis is detected. The invasive procedure involves the collection of liquid contents (biological material) for microbiological and cytological examination.
Based on the diagnostic results, the doctor confirms or refutes the diagnosis. What is a hydropericardium, a cardiologist should tell you.